W ’ : A M
advertisement

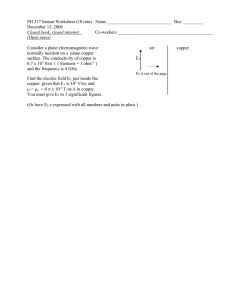
WILSON’S DISEASE: A MOLECULAR FOCUS PAUL TRUCHE CABM 010 April 7, 2010 WHAT IS WILSON’S DISEASE? Wilson’s disease is a neurodegenerative disease caused by a buildup of copper in the body’s tissues Effects 1 in 30,000 according to the Oxford Textbook of Medicine 1 in 100,000 posses a single copy of the mutated gene CAUSE OF WILSON’S DISEASE Mutation of the gene ATP7B is responsible for Wilson’s disease It is due to an abnormal gene located on chromosome 13: an autosomal recessive inheritable trait GENETIC BACKGROUND This gene is expressed predominantly in the liver, kidney and placenta. It is also expressed in the brain, heart, lungs and pancreas (Warrell) The ATP7B gene codes for the protein ATPase, Cu++ transporting, beta polypeptide, also known as ATPase 2 or ATP7B. Over 70 mutations have been found that are linked to Wilson’s disease. Gene deletions, and mutations that cause the allele to be completely unexpressed cause the worst forms of Wilson’s disease. WHY DO WE NEED COPPER? Copper is an essential mediates various cellular processes: mitochondrial energy generation (cytochrome c oxidase) iron uptake regulation (ceruloplasmin), melanin formation (tyrosinase) oxygen-radical scavenging (superoxide dismutase) collagen and elastin cross-linking (lysyl oxidase) WHEN WE HAVE TOO MUCH COPPER Excess copper can do many harmful things: generates reactive oxygen species, superoxide radicals and hydroxy radicals, which can damage cellular components. Copper can bind to histidine, cysteine, and methionine residues of various proteins, which results in the inactivation of the proteins COPPER TRANSPORT THROUGH THE BODY Ingested copper is first absorbed in the stomach, duodenum and small intestine. Copper first binds to albumin, transcuprien or histidine in the blood. Copper in the blood moving through the liver is removed by high affinity copper transport protein (hCTR1 and hCTR2). Once inside the liver cells, copper interacts with various other proteins including HAH1, ATOX1, and CCS Within liver cells, ATP7B brings copper across different membranes and prepares it for transport back out of the cell when copper needs to be removed COPPER IN THE BLOOD STREAM The protein ATP7A is responsible with the transport of ingested copper to cells within the body. The ATP7A protein carries copper through the membrane of intestinal enterocytes and then into the portal blood stream. Once in the blood stream, copper is transported throughout the body. MOVEMENT OF EXTRACELLULAR COPPER INTO CELLS Outside the cell, the protein called high affinity copper transport protein (Ctr1) first interacts with the copper cation. Once inside the cell, ATP7B the vesicular compartments when the cell needs to excrete excess copper Another protein, Atox1 delivers copper to the secretory pathway and docks with either copper-transporting ATPase. PROTEINS INVOLVED IN COPPER HOMEOSTASIS ATP7A ATP7B Ctr1 Atox1 Cox17 Other less understood proteins are hypothesized to play a role in copper homeostasis, but both their structure and functional role are still unknown ATP7A ATPase, Cu++ transporting, alpha polypeptide found in most tissues, but absent from the liver In the small intestine, the ATP7A protein helps control the absorption of copper from food. In other organs and tissues, the ATP7A protein has a dual role and shuttles between two locations within the cell. STRUCTURE OF ATP7A Figure above: Proposed mechanistic structure of the ATP7A protein embedded in the cell membrane. Note the six copper binding sites that extend into the cytosol. ATP interacts with the N domain to actively transport copper through the membrane. Image from Mutagenetix Database of Mutations and Phenotypes Figure below: Fourth Copper Binding Domain of the ATP7A protein. Not ever domain has been structurally determined and mutation at different domains shows different structural and functional changes in the protein suggesting that different structures exist between different binding sites ATP7B: THE WILSON DISEASE PROTEIN ATPase, Cu++ transporting, beta polypeptide The full structure of ATP7B has never been completely rendered six metal-binding subdomains (MBDs), each coordinating one copper between 2 Cys residues in an invariant CxxC motif. The large cytosolic N-terminal domain of ATP7B binds copper and plays a key role in regulation of ATP7B. STRUCTURE OF ATP7B Figure above: proposed structure of the ATP7B protein complex. (below): 3D structure of metal binding sites 3 and 4 on the ATP7B protein. These are the actual sites of metal binding within the protein structure. Figure above: N domain of the ATP7B protein. Helices are highlighted in red. The uppermost loop is the area responsible for the majority of mutation within the protein. This domain interacts with ATP. METAL BINDING DOMAINS Figure: The metal binding domains of the ATP7B molecule provide the major mechanistic location involved in Wilson’s disease. Mutation in the protein can often cause an inability for these sites to bind properly to copper. The 3D structure of the flexible loops that link the metal binding sites is shown in orange. Copper Binding Domain 3 Copper Binding Domain 4 Figure: Copper Binding site between two cystiene residues on the metal binding domain of ATP7B. Mutations around these binding sites cause inability of the protein to transport copper. Cystiene residues responsible for copper binding are located in two regions. Each of these regions is capable of binding copper within each copper binding domain. Why copper may bind to one over the other is not understood. N DOMAIN ATP Interacting Sites N-DOMAIN Figure: Residues E1064, H1069, G1099, and G1101 have been implicated as ATP binding sites within the N-domain. Figure: The region between ALA 1114 and THR 1143 has been attributed to many of the sequence mutations responsible for Wilson’s disease. This region corresponds exactly to the sequence insert, which is found in mammalian copper-ATPases, but absent in bacteria or lower eukaryotes. CTR1 Copper Transport Protein (Ctr1) Ctr1 is a homotrimeric protein, conserved from yeast to humans, that transports Cu across the plasma membrane with high affinity and specificity. ATOX1 Copper transport protein (ATOX1) plays a role in copper homeostasis by binding and transporting cytosolic copper to ATPase proteins in the trans-Golgi network for later incorporation to the ceruloplasmin. STRUCTURE OF ATOX1 ATOX1 copper binding site. Copper binding occurs between four cysteines: CYS 12.A, CYS 15.A, CYS 15.B and CYS 12.B. Two of each cysteine come from adjacent chains that make up the biological assemboly COX17 Cytochrome c oxidase copper chaperone An enzyme that may be involved in the recruitment of copper to the mitochondria for incorporation into the COX apoenzyme MUTATIONS OF THE ATP7B PROTEIN Numerous mutations in the ATP7B gene have been implicated in Wilson’s disease. The exact number of different mutations that can cause the disease is still unknown, but certain mutations account for a majority of those seen in clinical cases. Mutation of any of the six metal binding domains within the protein are the primary cause for inactive ATP7B proteins. Mutations in different metal binding domains cause different mutations in the overall protein structure and show that each binding domain may have specific mechanisms. This finding may explain the need for multiple copper binding sites, but this is still not understood . MUTATIONS OF THE ATP7B PROTEIN Mutations in the copper binding sites can lead to an increase in oxidation with subsequent decrease in copper binding. While the need for multiple copper binding sites is not completely understood, the interdomain communication between the metal binding sites is necessary for maintenance of reduced cysteines and proper copper acquisition. The metal binding domain interactions may involve a hydrogen-bonding network that allows copper binding to be translated into larger structural rearrangements via the loops between the metal binding sites. These rearrangements are likely to play a major role in regulating ATPase activity as well as mediating interactions with cellular trafficking of copper. MUTATIONS IN THE N DOMAIN The first group of mutations includes 16 residues in the following regions: 1,061–1,069 1,099–1,106 1,146–1,153 all located in the immediate vicinity of the ATPbinding site. Mutations in these locations most likely interfere with ATP binding in the protein. MUTATIONS NEAR THE ATP BINDING SITE Figure: Mutations near the ATP binding site account for the most common inactive forms of the ATP7B protein. Mutations for any residue in these locations seems to effect the ability for the protein to interact with ATP. Specific regions where mutations occur include: 1,061–1,069 (Red) 1,099–1,106 (Blue) 1,146–1,153 (Green) MUTATIONS (CONTINUED) The second group of mutations affects the following residues 1,033–1,038 ,which is a part of the hinge region connecting the N- and P-domains 1,168–1,176, which in the structure of the fulllength protein would face the P-domain. These mutations most likely alter the interactions between the N domain and other domains in the protein. There are other mutations that occur in other parts of the N domain and usually result in disruption of protein folding and other overall protein structure differences OTHER MUTATIONS Figure: Mutation sites not near the ATP binding site include: 1,033–1,038 (Red) 1,168–1,176 (Blue) Mutations in these areas most likely disturb the interactions between the N terminus and the rest of the protein PHYSIOLOGICAL EFFECTS OF MUTANT ATP7B The physiological effects of most mutations to the ATP7B protein lead to the clinical presentation of Wilson’s disease. Without proper function of the ATP7B protein, copper is unable to be removed by the hepatocytes in the liver. OUTLINE OF THE DISEASE PATHOLOGY 1) Failure of ATP7B to release copper from liver cells 2) Increase is copper levels in the liver 3) Inability for liver cells to further store copper 4) This excess copper in the blood stream is deposited in brain tissue 5) Neurologic and Hepatic symptoms begin to arise due to this build up of copper. SYMPTOMS OF WILSON’S DISEASE The earliest neurological symptoms include: difficulty speaking Drooling clumsiness of the hands change in personality. Acute abdominal symptoms include: Acute crises of acute hepatic necrosis, Coombes negative hemolytic anemia acute renal tubular damage may occur These crises are believed to be related to a massive release of copper from damaged or dead hepatocytes TREATMENT OF WILSON’S DISEASE Treatment for those diagnosed with Wilson’s disease focuses on the removal of copper from the body. In cases where liver damage has progressed to the point of complete failure, a liver transplant is necessary to replace dead and non functioning liver cells. Those who have had a liver transplant have not shown signs of Wilson’s disease after liver transplantation. For those who do not have full liver failure, pharmacological treatment is available. Pharmacological treatment of Wilson’s disease includes several drugs. Penicillamine binds copper and releases it through the urine. Trientine binds the copper and also releases it through the urine. Zinc acetate blocks further copper from being absorbed into the intestinal tract. Along with drug therapy, treatment involves avoiding ingestion of further copper. Common foods that contain copper are chocolate, dried fruit, liver, mushrooms, nuts, shellfish. CONCLUSION Many of the mechanisms involved in the transport of copper and those involved in Wilson’s disease are not well understood. Understanding the genetics and mechanisms behind copper transport will allow a better understanding of the pathology of the disease and allow more effective treatment options. Although current treatments for the disease are fairly effective, there is no way to reverse neurologic damage or completely cure the disease. Finding out how to reverse the neurologic damage will be an important step towards healing damage to the brain. DISCUSSION/QUESTIONS REFERENCES Banci, Lucia, Ivano Bertini, Francesca Cantini, Manuele Migliardi, Giovanni Natile, Fiorentin Nushi, and Antonio Rosato. "Solution Structures of the Actuator Domain of ATP7A and ATP7B, the Menkes and Wilson Disease Proteins." Biochemistry 48 (2009): 7849-855. Print. Bertini, Ivano, Lucia Banci, Francesca Cantini, and Simone Ciofi-Baffoni. "Cellular Copper Distribution: a Mechanistic Systems Biology Approach." Cellular and Molecular Life Sciences. Department of Chemistry, Magnetic Resonance Center CERM, University of Florence, 22 Feb. 2010. Web. <http://www.springerlink.com/content/n1t706677413127x/fulltext.pdf>. Dmitriev, Oleg, Ruslan Tsivkovskii, Frits Abildgaard, Clinton T. Morgan, John L. Markley, and Svetlana Lutsenko. "Solution Structure of the N-domain of Wilson Disease Protein: Distinct Nucleotide-binding Environment and Effects of Disease Mutations." PNAS 103.14 (2006): 5302-307. Print. Harada, Masaru. "Wilson's Disease." Medical Electron Microscopy 35 (2002): 61-66. Print. LeShane, Eric L., Ujwal Shinde, Joel M. Walker, Amanda N. Barry, Ninian J. Blackburn, Martina Ralle, and Svetlana Lutsenko. "Nteractions between Copper-binding Sites Determine the Redox Status and Conformation of the Regulatory N-terminal Domain of ATP7B." Journal of Biological Chemistry 285 (2006): 6327-336. Jbc.org. Web. 6 Apr. 2010. Prohaska, Joseph R., and Anna A. Gybina. "Intracellular Copper Transport in Mammals." American Society for Nutritional Sciences. J. Nutr. 134 (2004): 1003-006. Print. Swanson, Jerry W. "Wilson's Disease: Treatment and Drugs." Mayoclinic.com. Mayo Foundation for Medical Education and Research. Web. 1 Apr. 2010. <http://www.mayoclinic.com/health/wilsons-disease/DS00411/DSECTION=treatments-anddrugs>. Warrell, D. A. Oxford Textbook of Medicine. Oxford: Oxford UP, 2003. Print.