Overview The Principles of Quantitative MRI
advertisement

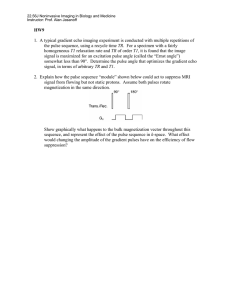
Overview • Sources of Error in qMRI The Principles of Quantitative MRI • Volume Measurements with MRI Perspectives for Imaging Cancers • Relaxation Time Measurements • • • Geoffrey D. Clarke, Ph.D. San Antonio, TX T1 Measurements T2 Measurements Magnetization Transfer Contrast • Motion Measurements with MRI • Diffusion • Tissue Perfusion MR Images are Produced Using ⊥ Gradient Fields Spin-Echo Sequence rf1 TX RX Gsl Gro Gpe rf2 Spin Echo y time time time x z time Symbolizes gradient increment from excitation to excitation Courtesy C. Keener • Image must be defined in 3 dimensions • z - slice selection • x - frequencyfrequency-encoded • y - phasephase-encoded 1 Gradient Coils are Typically Wound on Cylindrical Former MRI Gradient Fields Gradient Nonlinearities are often tolerated as part of trade-offs with gradient field strength or coil size Manufacturers often apply gradient distortion corrections in order to make images appear to be distortion free Influences image quality parameters (SNR, spatial resolution, etc.) http://www.nbirn.net Eddy Currents • Accelerating current in gradient coils (gradient pulse) causes induced currents in nearby metallic structures. • These currents produce magnetic fields which, in turn, oppose the magnetic fields of the gradient coils Eddy Currents • The magnetic field produced by Eddy Currents have two timetimedependent components: • An offset of the Bo field • An additional gradient field r r Bec (r , t ) = ∆g (r , t ) + ∆Bo (t ) 2 Eddy Current Pre-emphasis Gradient Current Eddy Current Actual Gradient Field Actively Screened Gradients •Reduce gradient field strength outside of gradient coil former - Current in shield is opposite polarity •Reduces gradient field in imaging volume also - Improves magnet homogeneity Gradient Current with PrePre-Emphasis Actual Gradient Field For details see: Morich et al, IEEE Trans Med Imag 1988; 7:247-254. Eddy Current Effects on Slice b a Ideal – no eddy currents •Each gradient coil is associated with a screen coil - Twice as many amplifiers required Tumor Volume Measurement c worst case prepre-gradient train RF pulse profiles used for T2T2-relaxometry a) Ideal profile calculated from Bloch equations b) profile showing the influence of eddy currents; c) prepregradient pulse train establishes steadysteady-state which regularizes the RF pulse profile De Deene Y et a. Phys Med Biol 2000; 45:1807-1823 Invasive ductal carcinoma Grade III in a 59 y.o. y.o. woman, studied while undergoing neoadjuvant chemotherapy. MRI was 3D fast GRE sequence. Partridge S et al. AJR 2005; 184: 1774-1781 3 Kaplan-Meier Curves Patients divided based on initial MRI volume of their tumors showed significant differences in recurrencerecurrencefree survival (p (p = 0.042, Wilcoxon’ Wilcoxon’s test). 1. A source of error in the prescribed gradient fields used in MRI include: 0% 1. B1 magnetic field inhomogeneities. inhomogeneities. 0% 2. Eddy currents. 0% 3. RF pulse timing instabilities 0% 4. Stimulated echoes 0% 5. Gradient coils coupling with the RF coils 10 Partridge S et al. AJR 2005; 184: 1774-1781 1. A source of error in the prescribed gradient fields used in MRI include: 1. B1 magnetic field inhomogeneities. inhomogeneities. Slice Selection rf1 TX RX Gsl rf2 Spin Echo time time time 2. Eddy currents. currents. 3. RF pulse timing instabilities 4. Stimulated echoes 5. Gradient coils coupling with the RF coils • If constant gradient field is on during the rf pulse: • Larmor frequency of spins varies with position • The flip angle depends on the local Larmor frequency and the frequency content of the RF field pulse • the RF pulse can be “crafted” crafted” to contain frequencies in only a specified range 4 FT Approximation B1 Transmission Field sin x • Proportional to current in TX coil A sinc function envelope on the r.f. x pulse produces a nearly square excitation profile of the phantom… phantom….. • Depends on Q of coil & coil loading • Depends on TX Coil Geometry • TX power autoauto-adjusted (pre(pre-scan) time FT • Values should be known to within 1% • 1% = 0.086 dB BW • TX nonlinearities • RF pulse droop frequency tp Resonant Frequency Offset RF Nonuniformities • Radio Frequency Field Nonuniformities are the Single Biggest Cause of Errors in qMRI • RF Nonuniformities Increase as the Bo-Field Increases M ∆Ω/γ X’ B= Bo+∆Ω/γ Y’ M Beff = B1x’y’+∆Ωz/γ Beff ∆Ω/γ X’ My’ = real Mx’ = imaginary Mz does not contribute to Y’ signal B1 90o, After Magnetization IS NOT on y’ axis Beff Mz Mx X’ X’ My Y’ Y’ 5 90o Sinc Pulse Profile 0 Mx -0.5 -1 -5 -2.5 0 2.5 5 1 0.5 Magnetization 0.5 Mz 0 -0.5 -1 -5 Frequency (kHz) -2.5 0 2.5 5 Frequency (kHz) 1 My Magnetization 1 My Magnetization Magnetization 1 180o Sinc Inversion Pulse 0.5 0 Mx -0.5 -1 -5 -2.5 0 2.5 Frequency (kHz) 5 0.5 0 Mz -0.5 -1 -5 -2.5 0 2.5 5 Frequency (kHz) 2 ms, 5-lobe, chemical shift refocused 2 ms, 5-lobe, chemical shift refocused Slice Profile Variations Poor RF Pulse Calibration • Flip Angle varies with location • Due to B1, B0 field nonuniformities • NonNon-linearity of Excitation (Bloch Eqns) Eqns) • FT approximation invalid for big flip angles • Bloch simulator software http://wwwhttp://www-mrsrl.stanford.edu/~brian/mritools.html * • T1T1-weighting of excitation profile *Brain Hargreaves Miscalibration of phase between 90o and 180o RF pulses in FSE (left image) is corrected (right image) 6 B1 Field Mapping - Purpose B1 Field Mapping - Methods a. Needed for accurate measurement of many NMR parameters, i.e. relaxation times a. OneOne-pulse read Mx,y b. Enables estimation of systematic errors in parameter measurement c. Enable correction of spatial sensitivity variation using reciprocity B1 Field Mapping • OneOne-pulse Mx,y method Venkatsen et al. Magn Reson Med 1998; 40:592 b. Spin Echo (both pulses altered) Barker et al. BJR 1998; 71: 5959-67 c. OneOne-pulse read Mz Vaughn et al. Magn Reson Med 2001; 46: 24 2. During the MRI excitation process, B1-field inhomoinhomogeneities will be manifest as: • Hard 1800o pulse preceding 2D field echo sequence 0% 1. an increase in MRI signal. 0% • Bright center is maximum B1 0% 2. distortion in the phasephase-encoding direction. 3. reduction of contrastcontrast-toto-noise ratio. ratio 4. spatial variation of the prescribed flip angle. 5. changes in the gyromagnetic ratio.10 • Ring pattern occurs at every 5% change in B1-field 0% 0% Deichmann R et al. Magn Reson Med 2002; 47: 398 7 2. During the MRI excitation process, B1-field inhomoinhomogeneities will be manifest as: 1. an increase in MRI signal. 2. distortion in the phasephase-encoding direction. 3. reduction of contrastcontrast-toto-noise ratio. ratio 4. spatial variation of the prescribed flip angle. 5. changes in the gyromagnetic ratio. Longitudinal Relaxation Relaxation Times • T1: longitudinal relaxation time defines recovery of potential for next signal (T1=1/R1) • T2: transverse relaxation time defines rate of dephasing of MRI signal due to microscopic processes (T2=1/R2) • T2*: transverse relaxation time with Bo inhomogeneity effects added; defines rate of dephasing of MRI signal due to macroscopic and microscopic processes (T2*=1/R2*) Applications for T1 Images M = Mo (1- exp(-TR/T1) • Tissue characterization Mo • Contrast agent uptake studies • Measurement of Tissue Perfusion τ T1 2T1 3T1 • Measurement of Blood Volume 4T1 8 Multi-Echo Acquisitions For Accurate & Precise T1 Mo exp(exp(-TE/T2) Mo exp ((-TE/T2*) • Varies over imaged slice due to slice profile • Flip angle must be calibrated across slice Signal Strength • Never Assume RF Flip Angle is Correct 90o • Be careful in assuming magnetization has reached steady state between acquisitions • Optimize sequence acquisition parameters to ensure maximal SNR • Always check that fitted data conforms to assumed model Gel Dosimeters • Used for 3D Radiation Dosimetry QC 180o TE 180o SE1 2*TE o SE2 180 SE3 time 3*TE Gslice Gread Gphase B1-Field Changes with Slice Position • Relies on direct relationship between relaxation rate, R2 (R2=1/T2) of gel following exposure and dose www.mgsresearch.com De Deene Y et a. Phys Med Biol 2000; 45:1825-1839 9 Effective Flip Angles R2 Calibration Average transverse magnetization within a slice as a fraction of Mo for various slice positions for flip angles ranging from 0o to 360o De Deene Y et a. Phys Med Biol 2000; 45:1825-1839 For Accurate & Precise T2 • Never Assume RF Flip Angle is Correct T2* Parametric Imaging • Varies over imaged slice due to slice profile • 180o flip angle must be calibrated across slice • Use multimulti-echo (vs. dual echo) approach and big TX coils whenever possible • Analyze and understand eddy current effects on T2 measurement M xy = M o e −t / T2 ' * • Similar to T2 measurements but use gradient echo imaging with varying TE • In tissues, beware of multimulti-exponential decay 10 Calculation of T2 Contrast Agent Maps M xy = M o e−t / T2 * ' ln M xy = −1/ T2*t + ln Mo ' ln(M xy / M o ) = slope= −1/ T2* ' T2* = −1/ slope T1-weighted image Parametric map of R2* http://www.research.philips.com/ Magnetization Transfer MTC in Liver Tumors PROTON SPECTRUM 0 Frequency (Hertz) Post-Contrast T1W SE Axial T2W SE Post-Contrast MTC Non-Contrast MTC “Free” Water Lipids “Bound” Water 217 Hz Frequency (Hertz) 1500 Hz Mahfouz M et al. J Egypt Nat’l Cancer Inst 2000;12(3):191–198 11 0 Magnetization Transfer Ratio MTR = Mo − Ms Mo Magnetization Transfer Ratio (MTR) • the difference of the saturated versus nonnonsaturate images relative to the signal in the normal (non(non-saturated images) MTR in Parotid Cancer • MR images obtained without (Left) and with (Right) magnetization transfer pulse. • Lesion toto-muscle MTR = 0.92. • Tumor diagnosed as malignant using combined criteria of poorly defined margins and lesionlesion-toto-muscle MTR > 0.71. Takashima et al. AJR 2001;176:1577–1584 3. Using magnetization transfer contrast effectively changes what? 3. Using magnetization transfer contrast effectively changes what? 0% 1. The T1 of tissue. tissue. 1. The T1 of tissue. tissue. 0% 2. The T2 of tissue. 2. The T2 of tissue. 0% 3. The T2* of tissue. 3. The T2* of tissue. 0% 4. The eddy currents. currents 4. The eddy currents. currents 0% 5. The rate of contrast uptake. 5. The rate of contrast uptake. 10 12 Physiological Measurements • Diffusion – random motion of spins in a homogeneous solution Diffusion Trajectory MRI exploits xploits phase losses in the signal due to diffusion of spins in a magnetic field gradient • Perfusion – amount of blood traveling through capillaries in ml/s/gm of tissue • Flow – bulk motion of blood and other fluids within body Hagmann, P. et al. Radiographics 2006;26:S205-S223 Crick Model Apparent Diffusion Coefficient ADC • Time must large enough so there is time for particles to interact with barriers • Do > ADC One dimensional model. • κ ≡ permeability of membrane barriers • a ≡ distance between barriers • ADC ≡ diffusion coefficient of molecules in presence of barriers • Do ≡ diffusion coefficient of bulk fluid Sotak C. Neurochem Internat’l 2004; 45(4): 569-582. The b-value • Controls amount of diffusion weighting in image • The greater the bb-value the greater the area under the diffusiondiffusionweighted gradient pulses • longer TE • stronger and faster ramping the gradients 13 Attenuation Due to Diffusion δ A(TE ) = A(0) exp[−γ 2G 2 Dappδ 2α 2 ( ∆ − )] 4 Where: α=π/2; G is amplitude of diffusion sensitive gradient pulse; δ is duration of diffusion sensitive gradient; ∆ is time between diffusion sensitive gradient pulses; Dapp is the apparent diffusion coefficient Diffusion Weighted Images Taylor WD et al. Biological Psychiatry. 55(3):20155(3):201-7, 2004 • Brighter regions indicate reduced diffusion values • Different effect for different directions of the diffusion sensitizing gradients • Splenium of the corpus callosum is aligned mainly with the x direction and has a large Deff • Splenium is dark when the gradients are in the x direction (upper left). DWI Basic Pulse Sequence 90o 180o time G G δ δ ∆ ( b = γ 2G 2δ 2 ∆ − δ 3 ) Stejskal EO & Tanner JE, J Chem Phys 1965. 42: 288-292 Changes in Tissue Cellularity are Related to Molecular Water Mobility Hall, D. E. et al. Clin Cancer Res 2004;10:7852-7859 Copyright ©2004 American Association for Cancer Research 14 MRI of Patients with Oligodendrogliomas DWDW-MRI of Glioblastoma Multiforme 7-week course of radiation therapy 7-week course of radiation therapy Moffat, Bradford A. et al. (2005) Proc. Natl. Acad. Sci. USA 102, 102, 55245524-5529 Hamstra, Daniel A. et al. (2005) Proc. Natl. Acad. Sci. USA 102, 1675916759-16764 DW MRI on Breast Tumor Parametric maps calculated from biomodal exponential decay model: ( ) ( I = P1' exp − bD1' + P2' exp − bD2' Io ) Paran Y et al. NMR Biomed 2004; 17:170-180 4. The degree of diffusiondiffusionweighting applied to a given pulse sequence is parameterized by the: 0% 1. b-value 0% 2. diffusion tensor 0% 3. ADC 0% 4. MTR 0% 5. effective RF flip angle 10 15 4. The degree of diffusiondiffusionweighting applied to a given pulse sequence is parameterized by the: Tissue Perfusion arteries Grey Matter 1. b-value vein 2. diffusion tensor 3. ADC White Matter 4. MTR 5. effective RF flip angle 500µ 500µm http://www.fmrib.ox.ac.uk/~patricia/web_talk/index.htm Compartmental Modeling Clinically available MRI contrast agents do not leak into the intracellular space. (Interstitial Space) Ktrans = volume transfer constant of contrast agent leakage into the interstitial spaces Jackson A et al. Clin. Cancer Res. 2007, 13(2): 3449 - 3459 Phases of Contrast Enhancement Uptake Phase: Phase: signal intensity rises above baseline and there is a net leakage of contrast from the blood vessels into the interstitial space. Zahra MA et al. Lancet Oncology 2007; 8: 6363-74. 16 Phases of Contrast Enhancement Phases of Contrast Enhancement Plateau Phase: Phase: maximum enhancement with an equilibrium in the movement of contrast between the plasma and extracellularextracellular-extravascular space. Washout Phase: Phase: contrast starts to leave tissue and goes back into blood vessels. Red part of graphs refer to phase in corresponding diagram showing movement of contrast. Zahra MA et al. Lancet Oncology 2007; 8: 6363-74. Zahra MA et al. Lancet Oncology 2007; 8: 6363-74. Dynamic Contrast Enhancement Angiogenesis • Angiogenesis is new blood vessel development, which can occur in the development of pathological states • Angiogenesis plays an important role in the growth and metastasis of tumors • Curves denote difference between uptake of normal glandular tissue (green (green)) & lesion (blue) blue) • High rate of uptake is linked to larger micromicrovessel size and density • Expanding tumors become hypoxic and express transcription factors, which induce the release of proangiogenic growth factors such as vascular endothelial growth factor Vlaardingerbroek & den Boer, 1999 17 DCEDCE-MRI In a Patient with Partial Response to Monoclonal Antibody Rx Angiogenesis Inflammatory Breast Cancer • A wide range of novel tumor therapies directed against angiogenesis have been developed Baseline Post Cycle 1 Bevacizumab (inhibits VEGFVEGF-A) + doxorubicin (chemo agent) Post Cycle 4 Post Cycle 7 • Perfusion MRI can assess hemodynamic parameters of tumors • Angiogenesis can be inferred from perfusion measurements from MRI s s DCE-MRI: tumor enhancement outlined in red; contrast kinetics (black line) Wedam, S. B. et al. J Clin Oncol; 24:769-777 2006 5. Dynamic Contrast Enhanced (DEC) MRI can be used to evaluate which physiological characteristic of tumors? 0% a. Diffusion 5. Dynamic Contrast Enhanced (DEC) MRI can be used to evaluate which physiological characteristic of tumors? a. b. c. d. e. 0% b. Apoptosis 0% c. Angiogenesis 0% d. Tumor growth 0% e. Tumor oxygenation Diffusion Apoptosis Angiogenesis Tumor growth Tumor oxygenation 10 18 Quantitative MRI Precautions Before undertaking qMRI: • • • • • Check gradient calibrations Understand gradient nonnon-linearities Evaluate eddy currents Measure RF pulse changes in space Determine RF receive nonuniformities References for SAMS 1. De Deene Y et al. Phys Med Biol. 45:1825– 45:1825–1839 (2000) 2. Jezzard P, Barnett AS & Pierpaoli C. Magn Reson Med. 39:80139:801-812 (1998) 3. Look DC, Locker DR. Rev Sci Instrum. Instrum. 41: 250250-251 (1970) 4. Le Bihan D et al. J Magn Reson Imag. Imag. 13: 534534-546 (2001) 5. Collins CM et al. J. Magn Reson Imag. Imag. 21:192– 21:192–196 (2005) Suggested Reading • Quantitative MRI of the Brain,Tofts Brain,Tofts,, P. ed. (2003, John Wiley & Sons, Southern Gate, Chichester, Chichester, UK) • Clarke GD, Lee Y. The Principles of Quantitative MRI. In Advances in Medical Physics 2008. 2008. AB Wolbarst, KL Mossman & WR Hendee, eds. (Medical Physics Publishing, Madison, WI) 2008. 19