Purpose of QUANTEC Summarizing our knowledge of normal tissue tolerances:
advertisement

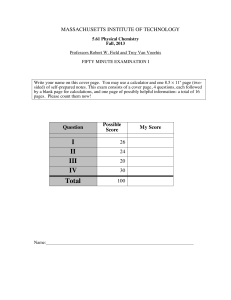
Summarizing our knowledge of normal tissue tolerances: the progress and future directions of QUANTEC*. Purpose of QUANTEC • Both AAPM and ASTRO recognized ($$): • Need for a systematic overhaul of our understanding of normal tissue tolerances ANDREW JACKSON Memorial Sloan-Kettering Cancer Center • For use in clinical treatment planning and optimization *QUAntitative Normal TissuE models in the Clinic History of QUANTEC • 2006 AAPM Science Council – Ellen Yorke and Rock Mackie – Steering Committee: Deasy, Bentzen, Yorke, Ten-Haken, Jackson, Marks, Eisbruch, Constein • 2007 1st QUANTEC meeting in Madison Wisconsin – Initial review of tolerances of involving physicists, biostatisticians and physicians. • 2008 Special Issue of Red Journal – in preparation, to be published in the fall. Organ specific QUANTEC articles • Significance of injury • Clinically relevant endpoints – Time course – Ambiguities • Anatomic definitions – Variations in contouring practice • Review of literature on dose-volume dependence of endpoints – Level of evidence 1 Organ specific QUANTEC articles • Patient related risk factors • Models of the data – Limitations • Caveats concerning models • Dose-volume and model dependent limits for clinical use • Future studies – • Additional knowledge required to improve toxicity prediction • Endpoint scoring and data capture in future studies Overview of Results for Specific Organs • Great variety in quality and quantity of data • Consistency issues: – Endpoints studied – Physical issues (organ motion, contouring issues, dosimetry) – Models/D-V constraints reported • Some organs are more equal than others – Lung: ~70 studies – Ear: ~4 studies of dose response of late hearing loss Organs Included • Brain, Brainstem, Cord, Optic Structures, Ear • Salivary Glands, Larynx & Pharynx • Lung, Heart, Esophagus • Liver, Kidney, Small Bowel, • Rectum, Bladder, Penile Bulb Mean dose response of pneumonitis (A. Jackson with L. Marks/S. Kong/J.Deasy/J.Bradley/M. Martel/S. Bentzen) • Patients treated for NSCLC – Data from 9 institutions, 10 separate studies • 1,167 patients with 222 cases of pneumonitis • Grade 3 RTOG ~ Grade 2 SWOG – (requiring steroids) – accepted grade 1 definition if few grade 1 cases 2 Pneumonitis, mean dose response - whole lung Mean dose response of pneumonitis – Numbers of pts w./w.o. pneumonitis – Bin locations on quartile plots • Fit of logistic function: – D50 = 30.75 [29.9 – 31.7] Gy – 50 = 0.907 [0.836 – 0.987] Probability of pneumonitis • Reporting rate (and S.D.) of pneumonitis as function of mean dose to total lung 1.0 MSKCC (10/78) Duke (39/201) Michigan (17/109) MD Anderson (~49?/223) NKI (17/106) WU (52/219) Martel et al. (9/42) Oeztel et al. (10/66) Rancati et al. (7/55) Kim et al. (12/68) logistic fit 0.9 0.8 0.7 0.6 0.5 0.4 0.3 0.2 0.1 0.0 0 10 20 30 Mean dose (Gy) Probability of aspiration as function of mean dose to Glottic and Supra-Glottic Larynx Rectal dose volume limits Jackson/Deasy/Gay/Michalski/Tucker/Zelefsky – Published limits having sig. correlation with grade 2 rectal bleeding – Color coded to indicate prescription dose • Blue = 66-70 Gy • Red = 83 Gy (LQ equivalent dose in 2 Gy fr) – Thickness of line indicates overall complication rate in study (T. Rancati, M. Schwartz, A. Allen, F. Feng, A. Popovtzer, B. Mittal, and A. Eisbruch) 3 Dose-volume limits with LQ corrected doses (a/b = 3 Gy) Jackson 70.2 Jackson 75.6 Akimoto Wachter Koper Cozarrino Zapatero 70-75.6 Gy: 7% Huang Hartford 75.6 Gy: 34% Grade 1 Fiorino Boersma 100 66 Gy: 33% 80 66 Gy: 14% 75.6 Gy: 19% 60 70-76 Gy: 9% 69 Gy: 25% 3 Gy/fr 40 – 4 published studies fitting LKB model to rectal complication data • Forrest plot of “n” values (n=1/a) • 1 S.D. indicated • Average value of “n” for all studies indicated – One further study* of RTOG 94-06 included • n=0.08 (95% conf: 0.04-0.26) 20 74-78 Gy: 23% 70.2 Gy: 6% 70-78 Gy: 3%Grade 3 0 10 20 30 40 50 60 70 80 LQ equivalent dose in 2 Gy fractions (Gy) estimates of LKB volume effect parameter n for rectal complications 90 * Tucker ASTRO 2007, IJROBP Kidney (L. Dawson, A. Paulino, B. Kavanagh, C. Pan, S. K. Das, M. Miften, X. A. Li, R. K. Ten Haken, T. E. Schultheiss) RTOG 94-06 Tucker Study % volume 66.2-70.2Gy: 11% Rectal lyman model fits Rancati Peeters Sohn 0.01 0.1 volume effect parameter, n 1 From: Cassady JR. Clinical radiation nephropathy. IJROBP 1995;31:1249-1256. 4 Bilateral Whole Kidney RT - TBI 0.5 Bilateral Partial Kidney RT minimal risk C he ng e t a l . Fi g ur e 2 low risk moderate-high risk high risk undefined Model 3 peptic ulcer gastric cancer seminoma lymphoma Model 4 0.4 Adults + Mixed Adults + Mixed: no NT drugs estimated threshold for injury Percent Volume Incidence of Late Renal Toxicity (% x 100) Data from 916 patients 0.3 0.2 0.1 gastric cancer lymphoma 0 4 6 8 10 12 14 gynecological cancer 16 Equivalent Total Dose (Gy) Cheng J, Schultheiss T, Wong J. Impact of Drug Therapy, Radiation Dose and Dose Rate on Renal Toxicity following Bone Marrow Transplantation. International Journal of Radiation Biology 2008; In press. Dose, Gy, over 5 weeks Mean dose response for SNHL at 4 kHz Late Hearing Loss 1.0 (A. Jackson, N. Bandare, W. Mendenhall) Chen et al. Oh et al. Honore et al. Pan et al. Kwong et al. – (post-treatment vs pre-treatment) • Differences in way endpoint is defined – Ispi- relative to contra-lateral hearing loss vs hearing loss • Dose reconstruction – 1 study, doses reconstructed with surrogate CT scans – 1 study, ipsi- doses relative to contra-lateral Incidence of SNHL at 4 kHz 0.9 • Hearing loss tests from 3 studies as function of mean cochlea dose 0.8 0.7 0.6 0.5 0.4 0.3 0.2 0.1 0.0 0 20 40 60 80 Mean cochlea dose (Gy) 5 Necessity of combining data sets • Number of complications in any given treatment series is usually low – False negatives – No statistical power to determine model parameters • Dose-volume exposures correlated in individual series – Introduces phony correlations with complications (False positives) – Insufficient range of dose-volume combinations to determine model parameters Problems in synthesizing data Problems in synthesizing data • Endpoint definitions: – Need to be clinically relevant – Need to be specific • Rectal bleeding or incontinence vs grade 2 RTOG toxicity – Different comps. have different dose-volume effects – Need to be standardized Problems in synthesizing data • Standard of reporting is POOR • Variety of dose volume limits proposed – These cannot be combined • Variety of models may be fit – Responses cannot be combined • gEUD responses with different “a” values cannot be combined – Lack of basic statistics (numbers not stated!) • Schultheiss 1994: “The information in this report would be of greater clinical use if some indication had been provided of the total number of patients from which the myelopathy cases were drawn” – Locations of bins in e.g. quartile plots not given – Model parameters (and errors) not be stated 6 Example: EUD Atlas of Pneumonitis In other words: • Report the numbers of patients with complications and the number treated • Report the number of NSCLC patients whose gEUD exceeds a given level – Elementary statistics increase clinical utility • Be comprehensive – Both with and without complication – Report as much about the data as possible • Be comprehensive: • How far can we take this? – Do this for each gEUD value – Vary the n=1/a parameter EUD Atla s o f severe p ne umoni ti s a t 6 mo nths 0 1 0 0 .8 0 Lower 68% confidence limit on complication probability 1 0/78 10 /60 7/31 4/14 3/6 1 /2 1 /1 0 /0 0 /0 0 /0 0 /0 0 /0 0 /0 0 /0 0/0 0/0 0/0 1 0/78 10 /62 7/33 4/17 3/7 1 /2 1 /1 0 /0 0 /0 0 /0 0 /0 0 /0 0 /0 0 /0 0/0 0/0 0/0 1 0/78 10 /62 7/39 4/17 3/7 1 /2 1 /1 0 /0 0 /0 0 /0 0 /0 0 /0 0 /0 0 /0 0/0 0/0 0/0 1 0/78 10 /64 9/43 5/21 3/9 1 /3 1 /1 1 /1 0 /0 0 /0 0 /0 0 /0 0 /0 0 /0 0/0 0/0 0/0 1 0/78 10 /68 9/49 6/26 3/11 2 /4 1 /2 1 /1 0 /0 0 /0 0 /0 0 /0 0 /0 0 /0 0/0 0/0 0/0 1 0/78 10 /69 10 /5 5 6/31 4/15 3 /7 1 /2 1 /1 1 /1 0 /0 0 /0 0 /0 0 /0 0 /0 0/0 0/0 0/0 1 0/78 10 /74 10 /5 9 9/42 5/22 3 /9 1 /3 1 /1 1 /1 0 /0 0 /0 0 /0 0 /0 0 /0 0/0 0/0 0/0 0.7 1 0/78 10 /76 10 /6 2 9/50 6/36 4 /16 2 /5 1 /1 1 /1 1 /1 0 /0 0 /0 0 /0 0 /0 0/0 0/0 0/0 0.6 1 0/78 10 /76 10 /7 0 10 /5 9 9/45 6 /33 3 /1 5 1 /4 1 /1 1 /1 1 /1 0 /0 0 /0 0 /0 0/0 0/0 0/0 0.5 1 0/78 10 /76 10 /6 8 9/57 9/47 7 /35 4 /1 8 1 /3 1 /1 1 /1 1 /1 0 /0 0 /0 0 /0 0/0 0/0 0/0 0.4 1 0/78 10 /76 10 /7 6 10 /7 1 9/59 9 /49 9 /4 0 5 /2 6 1 /6 1 /2 1 /1 1 /1 0 /0 0 /0 0/0 0/0 0/0 0.3 1 0/78 10 /77 10 /7 6 10 /7 4 10/6 7 9 /57 9 /4 8 7 /3 6 3 /2 1 1 /5 1 /3 1 /2 1 /1 0 /0 0/0 0/0 0/0 0.2 1 0/78 10 /76 10 /7 5 10 /7 4 9/68 9 /59 9 /4 8 7 /3 5 3 /2 1 1 /8 1 /5 1 /2 1 /2 0 /0 0/0 0/0 0/0 1 0/78 10 /77 10 /7 6 10 /7 5 9/70 9 /63 9 /5 0 7 /4 0 4 /2 5 3 /15 1 /6 1 /5 1 /2 0 /1 0/0 0/0 0/0 1 0/78 10 /77 10 /7 6 10 /7 5 9/74 9 /68 9 /5 8 7 /4 4 5 /3 1 3 /23 2 /1 4 1 /7 1 /5 0 /1 0/1 0/0 0/0 1 0/78 10 /77 10 /7 7 10 /7 6 9/73 9 /71 9 /6 6 7 /5 2 6 /3 9 3 /28 3 /2 4 2 /14 1 /7 0 /4 0/2 0/1 0/0 1 0/78 10 /77 10 /7 7 10 /7 4 9/71 9 /70 7 /6 1 6 /5 0 5 /3 7 3 /28 2 /2 4 1 /14 0 /8 0 /4 0/2 0/1 0/0 1 0/78 10 /76 10 /7 5 9/73 9/71 7 /64 6 /5 6 5 /4 1 3 /3 4 2 /30 2 /2 4 0 /16 0 /8 0 /4 0/2 0/0 0/0 1 0/78 10 /77 10 /7 5 9/73 9/73 8 /67 7 /5 9 5 /4 8 5 /3 9 2 /32 1 /2 8 1 /21 0 /1 3 0 /8 0/2 0/2 0/0 1 0/78 10 /77 10 /7 7 10 /7 4 9/73 9 /72 8 /6 7 7 /6 0 5 /4 9 5 /43 2 /3 4 1 /30 1 /2 6 0 /1 9 0/1 2 0/4 0/2 -0.5 1 0/78 10 /77 10 /7 6 10 /7 5 9/72 9 /72 8 /6 8 7 /5 9 5 /4 9 3 /41 2 /3 7 1 /30 1 /2 7 0 /2 2 0/1 6 0/8 0/1 -0.6 Lower 68% confidence limit on complication probability 1.0 0 0 .6 0 0 0 .4 0 0 2 4 log10(n) 2 0 .2 8 0 -0 .2 12 16 -0 .4 20 26 -0 .6 32 36 -0 .8 38 42 -1 0.9 0.8 log10 n 0 0.00 0.05 0.10 0.15 0.20 0.25 0.30 0.35 0.40 0.1 0.0 -0.1 -0.2 -0.3 -0.4 -0.7 dEUD (Gy) 0 4 8 12 16 E UD - dEUD (Gy) 20 24 30 -0.8 -0.9 -1.0 0 10 20 30 40 50 60 70 80 EUD (Gy) 7 Comparison of results from atlases with 2-0.5 Gy grid spacings with those from exact EUD For range of significant p-value, 2 Gy grid spacing in EUD is adequate p value vs n, 2 Gy binning and no binning in EUD Conclusions • QUANTEC is: For lower 95% and 68% conf. int. on n 2 and 1 Gy spacing resp. are adequate – Updating our clinical understanding of normal tissue tolerances – Providing clinical guidelines where possible Residual Deviance for EUD from Atlas (comparing various spacings) 1 p value anti-correlation 0.01 p value vs n (eud bins-2Gy) p=0.05 p value vs n (exact EUD per patient) 0.001 -1.0-0.9-0.8-0.7-0.6-0.5-0.4-0.3-0.2-0.1 0.0 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1.0 log10 n 60 EUD in 0.5 Gy bins Exact EUD EUD in 2 Gy Bins EUD in 1 Gy bins 59 • With appropriate caveats 58 – Defining areas of our ignorance 57 56 • recommend studies to remedy this 55 54 – Investigating future directions: 53 • Reporting standards • Clinically relevant but specific endpoint definitions • Inter-institutional data synthesis (atlases or pooling) 52 51 -1.0-0.9-0.8-0.7-0.6-0.5-0.4-0.3-0.2-0.1 0.0 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1.0 log 10 n Best fit value of n sensitive to grid noise - likelihood function is flat for n > 0.1 EUD atlas for severe pneumonitis at 6 months 1 0.8 0.6 0.4 0.2 log10 (n) correlation 0.1 residual deviance (=-2*ln(likelihood)) 61 0 -0.2 -0.4 -0.6 -0.8 -1 10/78 10/60 7/31 4/14 3/6 1/2 1/1 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 10/78 10/62 7/33 4/17 3/7 1/2 1/1 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 10/78 10/62 7/39 4/17 3/7 1/2 1/1 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 10/78 10/64 9/43 5/21 3/9 1/3 1/1 1/1 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 10/78 10/68 9/49 6/26 3/11 2/4 1/2 1/1 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 10/78 10/69 10/55 6/31 4/15 3/7 1/2 1/1 1/1 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 10/78 10/74 10/59 9/42 5/22 3/9 1/3 1/1 1/1 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 10/78 10/76 10/62 9/50 6/36 4/16 2/5 1/1 1/1 1/1 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 10/78 10/76 10/70 10/59 9/45 6/33 3/15 1/4 1/1 1/1 1/1 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 10/78 10/78 10/76 10/68 9/57 9/47 7/35 4/18 1/3 1/1 1/1 1/1 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 10/78 10/78 10/76 10/76 10/71 9/59 9/49 9/40 5/26 1/6 1/2 1/1 1/1 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 10/78 10/78 10/78 10/77 10/76 10/74 10/67 9/57 9/48 7/36 3/21 1/5 1/3 1/2 1/1 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 10/78 10/78 10/78 10/78 10/78 10/76 10/75 10/74 9/68 9/59 9/48 7/35 3/21 1/8 1/5 1/2 1/2 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/77 10/76 10/75 9/70 9/63 9/50 7/40 4/25 3/15 1/6 1/5 1/2 0/1 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/77 10/76 10/75 9/74 9/68 9/58 7/44 5/31 3/23 2/14 1/7 1/5 0/1 0/1 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/77 10/77 10/76 9/73 9/71 9/66 7/52 6/39 3/28 3/24 2/14 1/7 0/4 0/2 0/1 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/77 10/77 10/74 9/71 9/70 7/61 6/50 5/37 3/28 2/24 1/14 0/8 0/4 0/2 0/1 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 0/0 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/76 10/75 9/73 9/71 7/64 6/56 5/41 3/34 2/30 2/24 0/16 0/8 0/4 0/2 0/0 0/0 0/0 0/0 0/0 0/0 0/0 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/77 10/75 9/73 9/73 8/67 7/59 5/48 5/39 2/32 1/28 1/21 0/13 0/8 0/2 0/2 0/0 0/0 0/0 0/0 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/77 10/77 10/74 9/73 9/72 8/67 7/60 5/49 5/43 2/34 1/30 1/26 0/19 0/12 0/4 0/2 0/0 0/0 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/78 10/77 10/76 10/75 9/72 9/72 8/68 7/59 5/49 3/41 2/37 1/30 1/27 0/22 0/16 0/8 0/1 0 10 20 30 40 50 60 70 EUD (Gy) 8 EUD AND DOSE-VOLUME BASED ATLASES OF COMPLICATION INCIDENCE - A PROPOSAL FOR NEW STANDARDS IN 1) MSKCC, Yorke et al. IJROBP 63 2005: 672-682, from Fig 4a) ( RTOG grade 3, 6 months) 2) Duke, Hernando et al. IJROBP 51 2001: 650-659, from Table 4 ( CTC grade 1, 6 months) 3) Michigan, Kong et al. IJROBP 65 2006: 1075-1086, from Table 4 and Fig 2a) ( SWOG grade 2, 6 months) – bin location and time from authors. 4) MD Anderson, Wang et al. IJROBP 66 2006: 1399-1407, from Fig 2 ( CTC grade 3, 1 year actuarial – includes concurrent chemo patients) 5) NKI, Seppenwoolde et al. IJROBP 60 2004: 748-78, from Fig 3a) ( SWOG grade 2, 6 months) 6) WU, Hope et al. IJROBP 65 2006: 112-124, from Fig 9c) ( SWOG grade 2 – no time limit) with bin locations from authors, increased by 11% to ~account for inhomogeneity corrections. 7) Michigan, Martel et al. IJROBP 28 1994: 575-581, from Table 1 ( SWOG grade 1) with mean doses calculated from relationship between EUD (n=0.87) and mean dose from Kwa et al., Radiotherapy and Oncology 48 1998: 61-69 Fig 2a). 8) Heidelberg, Oeztel et al. IJROBP 33 1995: 455-460, from Fig 2 and text ( RTOG acute grade 1). 9) Milan, Rancati et al. Radiother. and Oncol. 67 2003: 275-283, from Fig 3 ( SWOG Grade 2 – no time limit, patients without COPD – includes induction chemo patients). 10) Gyeonggi, Kim et al. Radiology 235 2005: 208-215, from Table 5 ( RTOG grade 3, 6 months – includes concurrent chemo patients) – median values of mean dose in each bin provided by the authors. 11) Logistic fit: data fit to the form (f/(1+f)), where f=exp(b0+b1*dmean). Best fit values [95% confidence intervals] are b0 = -3.63 [-3.53--3.74], b1 = 0.118 [0.109-0.128], corresponding to D50 = 30.75 [29.9 – 31.7] Gy and 50 = 0.907 [0.836 – 0.987]. REPORTING RESULTS OF TREAMENT PROTOCOLS. Andrew Jackson, Ellen D. Yorke, Kenneth E. Rosenzweig, Ennapadam Venkatraman, and C. Clifton Ling Memorial Sloan-Kettering Cancer Center Dose-volume limits with LQ corrected doses (a/b = 3 Gy) estimates of LKB volume effect parameter n 100 66 Gy: 33% 66 Gy: 14% 80 % volume 66.2-70.2Gy: 11% 75.6 Gy: 19% 60 70-76 Gy: 9% 69 Gy: 25% 3 Gy/fr 40 RTOG 94-06 Tucker Study Jackson 70.2 Jackson 75.6 Akimoto Wachter Koper Cozarrino Zapatero 70-75.6 Gy: 7% Huang Hartford 75.6 Gy: 34% Grade 1 Fiorino Boersma Rancati Peeters Sohn 20 74-78 Gy: 23% 70.2 Gy: 6% 70-78 Gy: 3%Grade 3 1 0 10 20 30 40 50 60 70 80 90 2 3 4 5 volume effect parameter, n LQ equivalent dose in 2 Gy fractions (Gy) 9 Data Set Dose-Volume and EUD Atlases • 78 patients from a Phase I dose escalation study of 3D-CRT of non-small cell lung cancer* – Treated doses 57.6-90 Gy • Endpoint: RTOG Grade 3 radiation pneumonitis (G3RP) – G3RP = steroids and/or oxygen – Pts either developed G3RP within 6 months following treatment or survived that time without it – There were 10 instances of G3RP * Rosenzweig et al, Cancer 103:2118-27, 2005; Yorke et al, IJROBP 63:672-682, 2005 Calculation of EUD • EUD values were generated for total lung – Doses biologically corrected to l.q. equivalent doses delivered in 2 Gy fractions using / =3Gy – EUD calculated for each of a grid of n values (log10(n) varying from -1 to + 1 steps of 0.1) EUD(n j ) = v k (d k ) k 1 • We previously introduced the dose-volume atlas of complication incidence* – analyzed data from the lung protocol – does not account for overall shape of DVH • Here we introduce the EUD atlas – Accounts for overall shape of the DVH – Atlases can be based on other models * Jackson et al, Sem in Rad Onc 16:260-268, 2006 Additive property of the atlas • Provided dosimetric and endpoint information is compatible – Doses defined in same way – Endpoint defined in same way • Data from different atlases (A and B) can be added, grid point by grid point: nj nj Nc(A,B) / Np(A,B) = [Nc(A) + Nc(B)] / [Np(A) + Np(B)] 10 Additive property of the atlas • Facilitates meta-analysis of data from different institutions – Low numbers of complications from individual protocols can be combined – Potentially synergistic effect if adopted as a standard of reporting Calculations based on Atlas data • At each grid point, can calculate e.g.: Inefficient use of space • Many repeated numbers where no patient treatments occur • Solution: – Shift the range to eliminate this dead space – Record to shift so that correct position can be reconstructed Calculations based on Atlas data • For each value of n, can calculate e.g.: – Logistic regression of EUD with endpoint – Confidence limits on complication probability for patients with EUD > grid value – Probability that complication rate in patients with EUD > grid value is greater than tolerance • p-value for correlation of EUD with endpoint • range of n values for significant correlation with endpoint • Likelihood of fit of EUD response • Find max likelihood value and confidence intervals for n 11 Probability that G3PR rate is > 20% Probability that observed complications arise from true rate > 20% 1.0 • Need to determine effect of grid spacing noise on 0.9 0.8 0.7 0.0 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1.0 0.6 0.5 log10 n 0.4 0.3 0.2 0.1 0.0 Atlas grid spacing introduces statistical noise – Range of significant correlation -0.1 -0.2 – Best fit value of n parameter -0.3 -0.4 -0.5 -0.6 – confidence interval on fitted value of n -0.7 -0.8 -0.9 -1.0 0 10 20 30 40 50 60 70 80 EUD (Gy) Conclusions • Demonstrated utility of EUD and dose volume atlases using our lung data • Fitting n values from EUD atlas data – – – – At n 1 use 0.5 Gy grid At n < 1 use 2 Gy grid Noise should decrease as # pts and comps increase Reformatting atlas (shifting range) for each value of n: • better use of atlas space • better grid resolution Conclusions • Publication of atlases facilitates in depth meta-analysis of dependence of outcome data on atlas variables • Atlases allow for useful publication of treatment series with few to no comps • Atlases facilitate the quantitative assessment of potential risks and benefits of future treatments 12 P value, correlation with severe pneumonitis – exact vs atlas (2Gy bins) p value vs n, 2 Gy binning and no binning in EUD Residual deviance - exact and atlas values (2-0.5 Gy Bins) Residual Deviance for EUD from Atlas (comparing various spacings) 61 correlation 0.1 p value anti-correlation 0.01 p value vs n (eud bins-2Gy) p=0.05 p value vs n (exact EUD per patient) 0.001 -1.0-0.9-0.8-0.7-0.6-0.5-0.4-0.3-0.2-0.1 0.0 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1.0 log10 n residual deviance (=-2*ln(likelihood)) 1 60 EUD in 0.5 Gy bins Exact EUD EUD in 2 Gy Bins EUD in 1 Gy bins 59 58 57 56 55 54 53 52 51 -1.0-0.9-0.8-0.7-0.6-0.5-0.4-0.3-0.2-0.1 0.0 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1.0 log10 n Determining grid spacing • Noise increases at n>1 Basic Atlas Data • 2 dimensional grid in EUD and log10(n) – Range of EUD values , grid size gets cruder • For p value range, and 95% confidence interval on best fit value of n, – 2 Gy grid spacing in EUD is adequate • For lower limit of 68% confidence interval on n, – 1 Gy grid spacing in EUD is adequate • At each grid point (EUDi, log10(nj)), record – # patients with G3RP, (Nci,j), with EUD(nj) > EUDi – total # patients, (Npi,j), with EUD(nj) > EUDi. • Best fit value of n sensitive to grid noise – likelihood is a flat function of n – low statistics • Display as explicit ratio: Ncij/Npij 13 Residual deviance - exact values Best fit EUD response Best fit EUD response (n = 2), for >= grade 3 pneumonitis Residual deviance for exact EUD per patient 1.0 60 exact EUD per patient max likelihood, n = 2.0 lower 68.3% conf limit: n = 1.16 lower 95.4% conf limit: n = 0.710 59 58 57 56 55 54 53 52 51 -1.0-0.9-0.8-0.7-0.6-0.5-0.4-0.3-0.2-0.1 0.0 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1.0 log10 n Probability of >= grade 3 pneumonitis residual deviance (=-2*ln(likelihood)) 61 best fit (n=2), EUD50 = 15.3 Gy γ50 = 1.08 0.9 >= grade 3 pneumonitis data (quartiles) 0.8 0.7 0.6 0.5 0.4 0.3 0.2 0.1 0.0 0 5 10 15 20 25 30 EUD (Gy), n=2 Upper 68% confidence limit on complication probability Data Set Upper 68% confidence limit on complication probability 1.0 0.9 0.8 0.7 0.5 0.4 0.3 log10 n • treatments based on a single CT data set • treatment plans restorable from electronic archive 0.0 0.1 0.2 0.3 0.4 0.5 0.6 0.2 0.6 0.1 0.7 0.8 0.9 1.0 0.0 -0.1 -0.2 -0.3 -0.4 -0.5 -0.6 -0.7 -0.8 -0.9 -1.0 0 10 20 30 40 50 60 70 80 EUD (Gy) 14 Liver • Charlie Pan, Brian D Kavanagh, Laura A. Dawson, X. Allen Li, Shiva K Das, Moyed Miften, Randall K Ten Haken 15