Document 14240008
advertisement

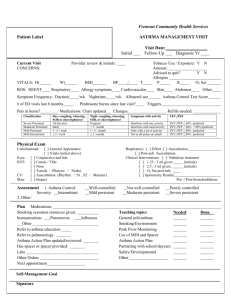
Journal of Medicine and Medical Science Vol. 3(4) pp. 232-236, April 2012 Available online http://www.interesjournals.org/JMMS Copyright © 2012 International Research Journals Full Length Research Paper Use of peak expiratory flow measurement for the assessment of asthma in adults in the emergency department Rhys H. Clark1,2, Zoe V. Wake1,3, Hannah Forward1,2 1 Sir Charles Gairdner Hospital, Hospital Avenue, Nedlands, Western Australia, 6009. University of Notre Dame Australia, 13-19 Mouat St, Fremantle, Western Australia, 6160. 3 Princess Margaret Hospital, Roberts Rd, Subiaco, Western Australia, 6008. 2 Abstract Asthma is a major cause of morbidity and mortality in emergency departments worldwide. New guidelines recommend the measurement of Peak Expiratory Flow or Spirometry to assess severity and monitor response to treatment. This is a retrospective review of asthma presentations to an emergency department. The objective of this study is to determine the proportion of adult patients (aged over 16 years) with mild to moderate asthma who have an evaluation of Peak Expiratory flow measured and documented at their initial assessment in the emergency department. 63 patients were included in this study with a median age of 50 years. Peak expiratory flow was documented for 68.3% (43) of the 63 patients during their initial assessment, and 86.0% (37) of these 43 patients had a follow-up PEF measurement subsequent to the commencement of treatment. There was no difference in the proportion of patients who had PEF documented when compared by severity of asthma. Emergency Departments should take measures to increase access to spirometry and peak flow meters for clinicians and nursing staff to more accurately assess patients and monitor response to treatment. Keywords: Asthma, Asthma Severity, Peak Expiratory Flow, Spirometry, Emergency department triage. INTRODUCTION Asthma is a major cause of morbidity and mortality in Australia, affecting approximately 2 million people (Australian Centre for Asthma Monitoring [ACAM], 2007). Acute asthma exacerbations account for 105,000 emergency department(ED) visits, 40,000 hospital admissions, and over 300 deaths every year in Australia (Australian Centre for Asthma Monitoring [ACAM], 2005). Unfortunately, despite national initiatives to improve asthma care and more effective medications, the mortality rate from asthma is on the rise and a recent national health survey showed that the management of asthma remains suboptimal (ACAM, 2007). The Peak Expiratory Flow (PEF) rate provides a simple, quantitative, and reproducible measure of the *Corresponding Author E-mail: rhc306@me.com degree of airflow limitation that is used with the patients clinical symptoms to risk stratify asthmatic presentations. Several studies (Beasley et al., 1989; Ignacio-Garciaand Gonzalez Santos, 1995) have found that PEF monitoring used as a component of asthma management optimises patient outcomes. The National Asthma Council has published guidelines that recommend PEF for determining severity and guiding treatment decisions in the ED (National Asthma Council [NAC], 2006). There are no studies published that investigate the outcomes of performing lung function tests in patients with asthma in the emergency setting. However, a study of emergency physicians’ ability to use clinical signs to risk stratify asthmatics demonstrated that they frequently underestimated the degree of airway obstruction and that subsequent knowledge of lung function results altered management in 20.4% of patients (Emermanand and Cydulka, 1995). Objective measurements of lung function are useful as there are Clark et al. 233 Figure 1. Summary of national asthma council steps in management of acute asthma Table 1. Initial assessment of acute asthma in adults, National Asthma Council Australia [NAC] (2006) Asthma Management Handbook 2006, Melbourne, p39 Findings Physical exhaustion Moderate No Talks in Pulse rate Pulsus paradoxus Central cyanosis Wheeze intensity PEF Sentences < 100/min Not palpable Absent Variable More than 75% predicted (or best if known) Phrases 100-120/min May be palpable May be present Moderate to loud 50-75% predicted (or best if known) FEV1 More predicted - 50-75% predicted Oximetry on presentation Arterial blood gases (assay) Other investigations # Mild No than 75% Not necessary Not required Necessary if initial response poor May be required Severe and life-threatening* Yes Paradoxical chest wall movement may be present Words More than 120/min† Palpable‡ Likely to be present Often quiet Less than 50% predicted (or best if known) or less than 100 L per min# Less than 50% predicted or less than 1 L Less than 90% Cyanosis may be present** Necessary†† Check for hypokalaemia Chest Xray to exclude other pathology (e.g. infection, pneumothorax) Patient may be incapable of performing test. often large disparities between symptoms and degree of obstruction. This is particularly useful in patients who are poor perceivers of their symptoms (NAC, 2006). Once patients present to an ED with acute asthma, the management algorithm relies solely on assessment of the severity of their asthma as mild, moderate or severe. These steps recommended by the NAC are summarised here in Figure 1. Assessment is based on clinical signs as well as Spirometry or PEF. Although spirometry is the lung function test of choice for assessing asthma severity it is more time consuming and is not always available in the emergency department. PEF meters are small, portable and more widely used in initial asthma assessment. This study was designed to audit the compliance with national guidelines that recommend the documentation of PEF to risk stratify patients. The objective is to determine the proportion of adult patients (aged over 16 years) with mild to moderate asthma who have an evaluation of Peak Expiratory flow measured and documented at their initial assessment in the emergency department. This was completed with the aim of expanding the use of PEF as a tool to assess severity and improve patient outcomes in the treatment of asthma. MATERIALS AND METHODS The current Australia standard of care is the National Asthma Council – Asthma Management Handbook which has been endorsed by The Thoracic Society of Australia and New Zealand, the Australasian College for Emergency Medicine and the Royal Australian College of General Practitioners (NAC, 2006). The guidelines require health professionals to perform spirometry and/or PEF measurement to gain an objective measure of airflow limitation (NAC, 2006). All patients with clinically diagnosed mild or moderate asthma should have a documented PEF level in their medical record within the time of their initial assessment in ED. National Health and Medical Research Council (NHMRC) level of evidence for this standard is recommenced best practice based on clinical experience and expert opinion. 234 J. Med. Med. Sci. Figure 2. Severity of asthma presentation by age of participants Study participants Adult patients, aged over 16 years, who presented to the emergency department of an outer metropolitan hospital from 1 January 2008 – 30 April 2008 with the diagnosis of mild to moderate asthma were included in this study. Patients with severe asthmas were excluded as they may not be able to perform PEF if lung function was severely restricted. the initial clinical assessment of the severity of asthma as mild, moderate or severe. The notes were also searched for documentation of findings that confirmed this level of severity such as pulse rate, physical exhaustion, cyanosis and wheeze. The findings required to classify the severity of the presentation by the NAC are included in full in Table 2. The level documented (mild/mod/severe) was checked for consistency with the findings recorded. Where no level of severity was documented, the investigators used the clinical findings to classify the presentation. Data collection Data was collected using the database Emergency Department Information Systems (EDIS, version 10.0) by searching for patients entered with a principal diagnosis of asthma (ICD-10 code J46) for the period 01/01/2008 to 20/04/2008. Medical records were searched by the investigators and data was entered in to a Microsoft Office Excel 2007 spreadsheet for storage and collation. Investigators cross-checked 20% of medical records to ensure data was entered correctly. The data collected included demographic details of patient age at presentation and gender and clinical details of assessment of severity as mild, moderate, severe, and whether or not PEF was documented pre and/or post-treatment and the percentage of the predicted or best PEF if documented. This data was collected as it allowed the investigators to not only audit the proportion of patients who had their PEF documented in total but to also look for some possible correlation between the asthma severity (mild or moderate) and the proportion of patients with PEF documented. The emergency department notes written by the assessing clinician were searched for documentation of RESULTS A total of 63 of the 70 patients initially identified met the selection criteria for inclusion. Patients were excluded if they were assessed has having severe asthma or had inadequate documentation to determine severity. Ages ranged from 18 to 67 years old with a median age of 50 years. Of the 63 patients, 42.9% (27) were male and 57.1% (36) were female. The clinical assessment of asthma severity by the attending ED doctor was mild in 65.1% (41) of cases and moderate in 34.9% (22) cases. Figure 2 represents the severity of asthma presentations by age group. Peak expiratory flow was documented for 68.3% (43) of the 63 patients during their initial assessment, and 86.0% (37) of these 43 patients had a follow-up PEF measurement subsequent to the commencement of treatment. Figure 3 represents the number of patients who had PEF documented by asthma severity group Of the patients who had an initial PEF documented, 90% (39) of patients had a response to treatment PEF documented. The values of PEF documented ranged from 130-530L/min and did not appear to have any Clark et al. 235 Figure 3. Percentage of patients with mild and moderate asthma who had initial Peak Expiratory Flow (PEF) documented in the Emergency Department correlation with clinical assessment of asthma severity. DISCUSSION The key finding of this audit is that 68.3% of patients had PEF documented during their initial assessment and 86.0% of these patients had a post-treatment PEF documented. There were very similar percentages across the different severity groups indicating that asthma severity did not change documentation of PEF. Reasons hypothesised that PEF was not documented in 31.7% of cases included uncertainty about whose role it was in the ED, lack of access to the PEF meter, uncertainty about the new guidelines. Doctors within the department also expressed doubt about the validity of PEF and therefore routinely did not use it as a measurement when spirometry was not available. The measurement of PEF has significant limitations in that it is dependent on patient effort and technique and it not ideal as a one off reading but as a series of readings (NAC, 2006; Miller et al., 1992; Sawyer et al., 1998). As this is a retrospective review of medical records, this study relies heavily on medical documentation which is often inadequate and may have resulted in patients who refused PEF not being recorded appropriately. Finally, several of the ED presentations coded as asthma may not have been attributable to acute attacks of asthma. Several papers discuss the use of the ED for routine primary care by asthmatics (Ford et al., 2001; Hanania et al., 1997). In these patients, documentation of PEF is not appropriate as they may not be experiencing acute asthma but requiring refills of prescription or medical certificates and this may underestimate the actual proportion who were managed according to the guidelines. To increase measurement of PEF in the emergency department education sessions were held with medical and nursing staff and training was provided with the PEF equipment. Posters were displayed in the assessment and triage area for early measurement of PEF and equipment was stored in a more accessible location. Instructions were taped to PEF storage containers for ease of use. The broader context of this study is that this data is relevant to other emergency where the measurement of PEF in asthma is inconsistent with the relatively new clinical guidelines. There have been no other clinical audits published on the use of PEF in the ED internationally however both the United Kingdom and United States have recently published new acute asthma management guidelines that make the same recommendation for early PEF measurement (British Thoracic Society, 2008; US National institute of Health, 2007). Therefore the results of this study may be useful for health professionals internationally to appreciate that there has not been 100% realization of asthma the guidelines. REFERENCES Australian Centre for Asthma Monitoring [ACAM], Asthma in Australia (2007): findings from the 2004–05 National Health Survey, Canberra: Australian Institute of Health and Welfare, Retrieved 8 June 2008, from http://www.aihw.gov.au/publications/index.cfm/title/10416 Australian Centre for Asthma Monitoring Asthma in Australia 2005, AIHW Asthma Series 2 (2005) Canberra: Australian Institute of Health and Welfare, Retrieved 8 June 2008, from www.aihw.gov.au/publications/index.cfm/title/10158 Beasley R, Cushley M, Holgate ST (1989). A self-management plan in the treatment of adult asthma. [Electronic version]. Thorax 44: 200204 British Thoracic Society (2008). British Guidelines on the Management of Asthma, British Intercollegiate Guidelines Network, Retrieved , from www.brit-thoracic.org.uk Emerman C, Cydulka R (1995). Effect of pulmonary function testing of acute asthma. [Electronic version]. Archives of Internal Medicine 155(20):2225-28 236 J. Med. Med. Sci. Ford JG, Meyer IH, Sternfels P, Findley SE, McLean DE, Fagan JK (2001). Patterns and predictors of asthma-related emergency department use in Harlem.[Electronic version]. Chest 120(4):1129– 35. Hanania NA, David-Wang A, Kesten S, Chapman KR (1997). Factors associated with emergency department dependence of patients with asthma. [Electronic version]. Chest 111(2):290–5. Ignacio-Garcia JM, Gonzalez-Santos P (1995). Asthma selfmanagement education program by home monitoring of peak expiratory flow. [Electronic version].Ame. J. Respir. Crit. Care Med.151:353-359 Miller MR, Dickinson SA, Hitchings DJ (1992). The accuracy of portable peak flow meters. [Electronic Version] Thorax. 47: 904-9. National Asthma Council Australia (2006) Asthma Management Handbook 2006, Melbourne, Retrieved 21 March 2008 from http://www.nationalasthma.org.au/cms/index.php National Health and Medical Research Council (NHMRC) (2003). When does quality assurance in health care require independent ethical review? Retrieved 20 March 2008 from http://www.nhmrc.gov.au National Institutes of Health (2007). Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma, [Electronic Version] J. Allergy and Clin. Immunol. (Suppl, 10) Sawyer G, Miles J, Lewis S, Fitzharris P, Pearce N, Beasley R (1998) Classification of asthma severity: should the international guidelines be changed. [Electronic Version] Clin. Exp. Allergy 28: 1565-1570.