L O U
advertisement

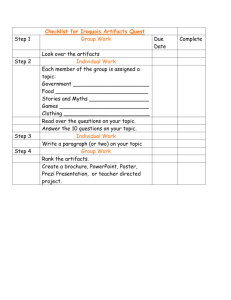
LIMITED OBSTETRIC ULTRASOUND JANUARY 14-16, 2016 Course Director: Oksana H. Baltarowich, MD THURSDAY, JANUARY 14, 2016 9:00 - 10:30 Introduction to Ultrasound Principles Mani Montazemi, RDMS 10:30 - 10:45 Break 10:45 - 12:00 Ultrasound Imaging of the Normal Female Pelvis 12:00 - 1:30 Lunch on Your Own 12:30 - 1:30 Principles of Ultrasound Physics Nathan Pinkney, BS, CDOS 1:30 - 2:15 Transvaginal Scanning Techniques Mani Montazemi, RDMS 2:15 - 3:15 Introduction to Ultrasound Evaluation of the Cervix Mani Montazemi, RDMS 3:15 - 3:30 Break 3:30 - 4:45 Demonstration of GYN Ultrasound Mani Montazemi, RDMS 4:45 - 5:00 Questions and Answers Mani Montazemi, RDMS Mani Montazemi, RDMS FRIDAY, JANUARY 15, 2016 9:00 - 10:30 1st Trimester Pregnancy 10:30 - 10:45 Break 10:45 - 12:00 Basic Fetal Anatomy 12:00 - 1:30 Lunch on Your Own 1:30 - 2:15 Measurements for Limited Obstetric Ultrasound G. William Shepherd, PhD, RDMS, RVT 2:15 - 2:45 Amniotic Fluid Assessment G. William Shepherd, PhD, RDMS, RVT 2:45 - 3:30 Biophysical Profile G. William Shepherd, PhD, RDMS, RVT 3:30 - 3:45 Break 3:45 - 5:00 Demonstration of Limited Obstetrical Ultrasound SATURDAY, JANUARY 16, 2016 9:00 - 12:00 Optional Hands-On Scanning G. William Shepherd, PhD, RDMS, RVT G. William Shepherd, PhD, RDMS, RVT G. William Shepherd, PhD, RDMS, RVT 1/6/2014 US Principles Image Orientation Introduction to Ultrasound Principles US Principles Image Orientation Artifacts Masses Instrumentation Basic Principles of Ultrasound • Ultrasound diagnostically is used in 2 ways Mani Montazemi, RDMS Baylor College of Medicine Division of Maternal-Fetal Medicine Department of Obstetrics and Gynecology Manager, Maternal Fetal Center Imaging Texas Children’s Hospital, Pavilion for Women Houston Texas & Clinical Instructor Thomas Jefferson University Hospital Philadelphia, Pennsylvania Artifacts B A D Masses Instrumentation US Principles Image Orientation Artifacts Masses Instrumentation Basic Principles of Ultrasound Basic Principles of Ultrasound • Ultrasound diagnostically is used in 2 ways • Ultrasound diagnostically is used in 2 ways – Anatomic information US Principles Image Orientation Artifacts Masses Instrumentation What is Ultrasound? – Anatomic information – Blood flow information US Principles Image Orientation Artifacts Masses Instrumentation What is Ultrasound? 1 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Artifacts Masses Instrumentation Basic Principles of Ultrasound Basic Principles of Ultrasound • What is “sound” • What is “sound” – Sound is a form of energy – Sound is a form of energy • What is “energy” – Energy is the capacity to do work • Moving an object, heating the room, lighting electricity US Principles Image Orientation Artifacts Masses Instrumentation Basic Principles of Ultrasound • Sound is mechanical energy transmitted by pressure waves in a material medium – Sound is not electromagnetic – Matter must be present for sound to travel US Principles Image Orientation Artifacts Masses Instrumentation Pulsed-echo Principle • The energy within a pulsed-echo system is electrical, but the energy in the patient’s body is sound, which is mechanical US Principles Image Orientation Artifacts Masses Instrumentation How Does an Ultrasound Instrument Work? US Principles Image Orientation Artifacts Masses Instrumentation What is a Transducer? • Converts one form of energy into another form 2 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Video Clip - Transducer Artifacts Masses Instrumentation Transducer Frequency 5.0 3.5 2.25 US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Transducer Configurations • Curved linear • Straight linear • Conventional sector • Microsector • Endocavity • Intraoperative US Principles Image Orientation Artifacts Masses Instrumentation Transducer Configurations • Mechanical • Phased array Artifacts – 2.25 MHz – 3.5 MHz – 5 - 6 MHz – 7.5 -10 MHz – 9.0 MHz – 12 -17 MHz Masses Instrumentation Image Configurations Linear Curved US Principles Image Orientation Artifacts Sector Masses Instrumentation Transducer Configurations • Mechanical – moving parts – – – – – – Wobbler or rotating Single or multi-element Mechanical beam steering & focusing Motor driven/fluid filled scan head FOV is sector Single or multi-frequency 3 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Transducer Configurations • Phased array – no moving parts – Flat linear – Curved linear – Sector Artifacts Masses Instrumentation Curved Linear Array Transducer • • • • • Multi-element Elements arranged in an arc and are sequentially pulsed FOV is trapezoidal-sector Produce larger FOV Benefits: – High quality imaging – Faster frame rate – Electronic focusing US Principles Image Orientation Artifacts Masses Instrumentation Video Clip - Transducer US Principles Image Orientation Artifacts Masses Instrumentation Categories of Sound Infra Sound below 20 Hz Audible Sound 20-20,000 Hz Ultrasound Above 20,000 Hz Sound is categorized according to the frequency of vibration per seconds US Principles Image Orientation Artifacts Masses Instrumentation Frequencies Used For Medical Diagnostic Ultrasound Are Normally Above 1 MHz One cycle / second = one Hertz (Hz) US Principles Image Orientation Artifacts Masses Instrumentation Resolution: What is it? • Clarity & sharpness of an ultrasound image • The capability of clearly distinguishing two points located close to each other on the sonogram One thousand cycles / second = one Kilohertz (kHz) One Million cycles / second = one Megahertz 4 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation Video Clip – Safety US Principles Image Orientation Artifacts Masses Instrumentation Safety - Prudent Use Minimize risk Minimize exposure Medical indication only Minimize exposure time Minimize exposure output US Principles Image Orientation Artifacts Masses Instrumentation Ultrasound Safety • Prudent use dictates that the principle of ALARA be observed and the ultrasound power levels be maintained As Low As Reasonably Achievable, in order to provide the maximum benefit / risk ratio US Principles Image Orientation Artifacts Masses Instrumentation Output Display Values • Power • Thermal Index – heat – Ratio of the in-situ power to the acoustic power required to raise tissue temprature by 1o C • Mechanical Index – cavitation – Acoustic output in terms of the likelihood of tissue cavitation 5 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation Image Orientation & Scanning Planes Caution US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Scanning Planes • Longitudinal • Transverse • Oblique US Principles Image Orientation Artifacts Artifacts Masses Instrumentation Sagittal Scan • Longitudinal, vertical planes • Divide the body into left & right Masses Instrumentation US Principles Image Orientation Sagittal Scan Artifacts Masses Instrumentation Sagittal Scan H A F P 6 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Sagittal Scan US Principles Image Orientation Artifacts Masses Instrumentation Artifacts Masses Instrumentation Sagittal Scan US Principles Image Orientation Sagittal Scan Artifacts Masses Instrumentation Sagittal Scan Anterior Maternal Head Maternal Feed Posterior US Principles Image Orientation Artifacts Masses Instrumentation Sagittal Scan US Principles Image Orientation Artifacts Masses Instrumentation Sagittal Scan 7 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Masses Instrumentation Sagittal Scan Anterior H Artifacts F Posterior US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Artifacts Masses Instrumentation Anterior H F Posterior US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Artifacts Masses Instrumentation Transverse Scan • Horizontal, transaxial planes • Divide the body into superior & inferior 8 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Transverse Scan Artifacts Masses Instrumentation Transverse Scan R A L P US Principles Image Orientation Artifacts Masses Instrumentation Transverse Scan US Principles Image Orientation Artifacts Masses Instrumentation Transverse Scan US Principles Image Orientation Artifacts Masses Instrumentation Transabdominal Transverse US Principles Image Orientation Artifacts Masses Instrumentation Transverse Scan Twin Pregnancy 9 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Oblique Scan Artifacts Masses Instrumentation Oblique Scan • Oblique planes • Inclined from the standard planes • In any direction US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Artifacts • • • • • Artifacts Masses Instrumentation Posterior Enhancement Posterior Enhancement Acoustical Shadowing Attenuation Reverberations Refraction US Principles Image Orientation Artifacts • Increased intensity in echoes from reflectors behind a structure that weakly attenuates sound • Classical feature of fluid Masses Instrumentation US Principles Image Orientation Posterior Enhancement Artifacts Masses Instrumentation Posterior Enhancement UT OV 10 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation Acoustical Shadowing US Principles Image Orientation Artifacts Masses Instrumentation Acoustical Shadowing • Marked decrease in intensity of echoes from reflectors that lie behind a structure that is strongly reflecting or attenuating sound • Complete lack of acoustical & anatomical information in the area of shadowing US Principles Image Orientation Artifacts Masses Instrumentation Acoustical Shadowing US Principles Image Orientation Artifacts Masses Instrumentation Acoustical Shadowing Head US Principles Image Orientation Artifacts Masses Instrumentation Acoustical Shadowing US Principles Image Orientation Artifacts Masses Instrumentation Acoustical Shadowing 11 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Acoustical Shadowing Artifacts Masses Instrumentation Attenuation • Reduction of the sound beam’s amplitude and intensity as it travels through a medium US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Attenuation Artifacts Masses Instrumentation Attenuation Normal US Principles Image Orientation Artifacts Masses Instrumentation Attenuation US Principles Image Orientation Artifacts Masses Instrumentation Reverberations • When 2 or more reflectors in the sound path cause multiple, repetitive artifactual echoes 12 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Reverberations US Principles Image Orientation Artifacts Masses Instrumentation Video Clip – Artifacts • • • • • Posterior Enhancement Acoustical Shadowing Attenuation Reverberations Refraction Masses Instrumentation Reverberations US Principles Image Orientation Artifacts Masses Instrumentation Cervix – US Appearance US Principles Image Orientation Artifacts Artifacts Artifacts Masses Instrumentation Echogenicity • Intensity of echoes reflected by tissues or structures from inside the body 13 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Artifacts Masses Instrumentation Echogenicity Liquids Solids Vessels & Ducts Soft Tissue Bone Gallbladder Urinary Bladder Fibrous Cysts Tumors Gall Stone Kidney Stone Cysts Polyps & Lesions Calcific Plaque US Principles Image Orientation Artifacts Masses Instrumentation • Echogenicity of a structure is described relative to surrounding or adjacent tissue US Principles Image Orientation Echogenicity • Anechoic • Hypoechoic • Hyperechoic US Principles Image Orientation Artifacts Artifacts Masses Instrumentation Anechoic • Sonolucent • No internal echoes Masses Instrumentation Anechoic US Principles Image Orientation Artifacts Masses Instrumentation Anechoic 14 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation Anechoic US Principles Image Orientation Artifacts Masses Instrumentation Hyperechoic Anechoic US Principles Image Orientation Artifacts Masses Instrumentation Hyperechoic • High intensity echoes • Increased echogenicity • Echogenic US Principles Image Orientation Artifacts Masses Instrumentation Hyperechoic Hyperechoic 15 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Hypoechoic Artifacts Masses Instrumentation Hypoechoic • Low intensity echoes • Decreased echogenicity US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Clotted Blood Hemoperitoneum Artifacts Masses Instrumentation Echotexture • Homogeneous • Heterogeneous US Principles Image Orientation Artifacts Masses Instrumentation Homogeneous US Principles Image Orientation Artifacts Masses Instrumentation Homogeneous • Uniform echoes • Fine, smooth texture 16 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Homogeneous Artifacts Masses Instrumentation Heterogeneous • Non-uniform echoes • Irregular texture US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Heterogeneous Normal Artifacts Masses Instrumentation Heterogeneous Normal US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Types of Masses • Cystic • Solid • Complex Artifacts Masses Instrumentation Cystic Masses • • • • Anechoic Fluid filled Smooth, well defined margins Posterior enhancement 17 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation Cystic Masses US Principles Image Orientation Artifacts Masses Instrumentation Cystic Masses Cephalocele US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Solid Masses • • • • • Artifacts Masses Instrumentation Solid Masses Contains varying amounts of internal echoes Regular or irregular margins Poorly defined back wall Posterior attenuation of sound Distal acoustic shadow US Principles Image Orientation Artifacts Masses Instrumentation Uterine Leiomyoma – US Findings • Discrete solid mass – single or multiple US Principles Image Orientation Artifacts Masses Instrumentation Uterine Leiomyoma – US Findings • Variable echogenecity – hypoechoic, hyperechoic 18 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Solid Masses Artifacts Masses Instrumentation Hemorrhagic Cyst Artifacts Masses Instrumentation Complex Masses • • • • • • US Principles Image Orientation Masses Instrumentation Diagnostic Challenge Uterine Leiomyoma – US Findings US Principles Image Orientation Artifacts Predominantly Cystic Mostly cystic Posterior enhancement Internal echoes Thin or thick septations Thin or thick walls US Principles Image Orientation Artifacts Masses Instrumentation Mural Nodule vs. Clot • Lace-like pattern of internal echoes 19 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Artifacts Masses Instrumentation Complex Masses Mural Nodule vs. Clot Normal Sacrococcygeal Teratoma US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Complex Masses Artifacts Masses Instrumentation Complex Masses Cervical Teratoma US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Complex Masses Artifacts Masses Instrumentation Complex Masses • • • • Predominantly Solid Mostly echogenic Internal cystic changes Posterior attenuation Cystic Lymphangioma 20 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Complex Masses Artifacts Masses Instrumentation Describing A Mass • • • • • Size Shape, borders, wall Acoustic properties (cystic, solid, complex) Posterior enhancement or attenuation Location Normal Hepatoblastoma US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation How Would You Describe This Mass? Artifacts Masses Instrumentation How Would You Describe This Mass? In the right adnexa TRV Pelvis US Principles Image Orientation Artifacts Masses Instrumentation How Would You Describe This Mass? In the right adnexa there is a round, well marginated thin walled mass with a sharply defined back wall, US Principles Image Orientation Artifacts Masses Instrumentation How Would You Describe This Mass? In the right adnexa there is a round, well marginated thin walled mass with a sharply defined back wall, thin internal septations, 21 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation How Would You Describe This Mass? In the right adnexa there is a round, well marginated thin walled mass with a sharply defined back wall, thin internal septations, low intensity echoes, US Principles Image Orientation Artifacts Masses Instrumentation How Would You Describe This Mass? Artifacts Masses Instrumentation How Would You Describe This Mass? In the right adnexa there is a round, well marginated thin walled mass with a sharply defined back wall, thin internal septations, low intensity echoes, and excellent posterior enhancement. US Principles Image Orientation Artifacts Masses Instrumentation Basic System Overview In the right adnexa there is a round, well marginated thin walled mass with a sharply defined back wall, thin internal septations, low intensity echoes, and excellent posterior enhancement. The features are those of a complex, predominantly cystic mass. US Principles Image Orientation Artifacts Masses Instrumentation Patient Data Entry US Principles Image Orientation Artifacts Masses Instrumentation Patient Data Entry 22 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation Transducer / Exam Selection US Principles Image Orientation Masses Instrumentation Transducer / Exam Selection US Principles Image Orientation Transducer Selection Artifacts Artifacts Masses Instrumentation Probe Handling Resolution vs. Penetration • Right frequency for penetration • Highest frequency for resolution US Principles Image Orientation Artifacts Masses Instrumentation ? US Principles Image Orientation Artifacts Masses Instrumentation Probe Handling – “Sagittal” Probe Handling – “Sagittal” Incorrect Incorrect 23 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation Probe Handling – “Sagittal” Artifacts Masses Instrumentation Probe Handling – “Sagittal” Correct Incorrect US Principles Image Orientation US Principles Image Orientation Artifacts Masses Instrumentation Probe Handling – “Sagittal” US Principles Image Orientation Artifacts Masses Instrumentation Probe Handling – “Transverse” Incorrect US Principles Image Orientation Artifacts Masses Instrumentation Probe Handling – “Transverse” Incorrect US Principles Image Orientation Artifacts Masses Instrumentation Probe Handling – “Transverse” Correct 24 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation Probe Handling – “Don’t” US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Artifacts Masses Instrumentation Probe Handling US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Artifacts Masses Instrumentation Basic Controls • • • • • Freeze Overall Gain TGC Depth Focus US Principles Image Orientation Artifacts Masses Instrumentation Overall Gain Overall Gain - Increase • An increase or decrease of the gain will change the brightness of the image • Affects entire field of view 25 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation Overall Gain - Increase US Principles Image Orientation Artifacts Masses Instrumentation Overall Gain - Decrease US Principles Image Orientation Artifacts Masses Instrumentation Overall Gain - Decrease US Principles Image Orientation Artifacts Masses Instrumentation Overall Gain - Increase US Principles Image Orientation Artifacts Masses Instrumentation Overall Gain - Decrease US Principles Image Orientation Artifacts Masses Instrumentation Overall Gain 26 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation Time Gain Compensation US Principles Image Orientation Artifacts Masses Instrumentation Time Gain Compensation • These slide pots controls amplification of returning echo signals at specific depths Near Field • The TGC compensates for loss in signal strength as the ultrasound beam passes through an organ Mid Field Far Field • Affects specific portions of the field of view US Principles Image Orientation Artifacts Masses Instrumentation Time Gain Compensation US Principles Image Orientation Artifacts Masses Instrumentation Time Gain Compensation Brighter Darker US Principles Image Orientation Artifacts Masses Instrumentation Time Gain Compensation US Principles Image Orientation Artifacts Masses Instrumentation Time Gain Compensation Brighter 27 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Time Gain Compensation Artifacts Masses Instrumentation Time Gain Compensation Darker US Principles Image Orientation Artifacts The diagnosis is only As good as the information your image provides Masses Instrumentation Time Gain Compensation US Principles Image Orientation Artifacts Masses Instrumentation What Constitute a Good Image? US Principles Image Orientation Artifacts Masses Instrumentation What Constitute a Good Image? 28 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Artifacts Depth Masses Instrumentation Depth • Controls the depth of field of view • When the image depth is changed, the field of view increases or decreases US Principles Image Orientation Artifacts Masses Instrumentation Too Small Depth Just Right Too Big US Principles Image Orientation Artifacts Masses Instrumentation Focus • Transmit Zone US Principles Image Orientation Artifacts Masses Instrumentation Focus Region of minimum beam width in a focused ultrasound beam – Highlights area of interest – Place at or slightly below area of interest 29 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation Artifacts Focus US Principles Image Orientation Artifacts Masses Instrumentation Focus Masses Instrumentation Don’t Get Fooled By Poor Technique Pay Attention to Focal Zone US Principles Image Orientation Artifacts Masses Instrumentation Cine Loop • Stores and displays images with no loss of quality Ancillary Functions US Principles Image Orientation Artifacts Masses Instrumentation M-Mode • Useful in evaluating motion and velocity of moving structures – Fetal Heart Motion 30 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation OB Calculations Sac Diameter • Highlight and Select OB Calc US Principles Image Orientation Artifacts Masses Instrumentation OB Calculations • Select [Single/A/B] soft key if needed US Principles Image Orientation Artifacts Masses Instrumentation Measurements • Calipers, Add Caliper • Individual measurements – Trace, Ellipse • Measures area and circumference US Principles Image Orientation Artifacts Masses Instrumentation OB Calculations • Highlight and select Biometry or AFI US Principles Image Orientation Artifacts Masses Instrumentation OB Worksheet • Edit or Delete Measurements • Enter Previous Exam Data • Enter Comments 31 1/6/2014 US Principles Image Orientation Artifacts Masses Instrumentation US Principles Image Orientation OB Worksheet US Principles Image Orientation Artifacts Masses Instrumentation Artifacts Masses Instrumentation OB Worksheet US Principles Image Orientation Artifacts Masses Instrumentation OB Worksheet Thank You 32 1/6/2014 Normal Anatomy of the Female Pelvis Sagittal Scan • Longitudinal, vertical planes • Divide the body into left & right Mani Montazemi, RDMS Mani Montazemi, RDMS Female Anatomy Clinical Instructor – Imaging Manager Baylor College of Medicine Division of Maternal-Fetal Medicine Department of Obstetrics and Gynecology Texas Children’s Hospital, Pavilion for Women Houston Texas Mani Montazemi, RDMS Female Anatomy Sagittal Scan Sagittal Scan H A F P Mani Montazemi, RDMS Female Anatomy Mani Montazemi, RDMS Female Anatomy Sagittal Scan Mani Montazemi, RDMS Female Anatomy Sagittal Scan Mani Montazemi, RDMS Female Anatomy 1 1/6/2014 Sagittal Scan Transverse Scan • Horizontal planes • Divide the body into superior & inferior Mani Montazemi, RDMS Female Anatomy Mani Montazemi, RDMS Female Anatomy Transverse Scan Transverse Scan R A L P Mani Montazemi, RDMS Female Anatomy Transverse Scan Mani Montazemi, RDMS Female Anatomy Mani Montazemi, RDMS Female Anatomy Transabdominal Transverse Mani Montazemi, RDMS Female Anatomy 2 1/6/2014 Uterus Located in Pelvis Between Bladder & Rectum Mani Montazemi, RDMS Female Anatomy Vagina • Lies between the urinary bladder & rectum • The vaginal canal is indicated by the bright line separating the anterior and posterior walls BL Mani Montazemi, RDMS Female Anatomy Vagina Vagina • The vaginal canal helps to identify the midline view of the uterus • Helps to distinguish lateral displacement of the uterus Mani Montazemi, RDMS Female Anatomy Mani Montazemi, RDMS Female Anatomy Vagina Vagina • If the hymen is imperforated at menarche the vagina will fill with blood, forming a hematocolpos Mani Montazemi, RDMS Female Anatomy Mani Montazemi, RDMS Female Anatomy 3 1/6/2014 Vagina Vagina Mani Montazemi, RDMS Female Anatomy Mani Montazemi, RDMS Female Anatomy Cervix Cervix • Lower cylindrical neck of the uterus which projects into vagina • Internal os – Junction of the uterine cavity and endocervical canal • External os – Junction of the endocervical canal and vagina Mani Montazemi, RDMS Female Anatomy Mani Montazemi, RDMS Female Anatomy Cervix Uterus * * * Mani Montazemi, RDMS Female Anatomy * * * * * * * * * * • Cervix • Body • Fundus * * * * * * * * * * Mani Montazemi, RDMS Female Anatomy 4 1/6/2014 Layers of Uterus Endometrium 1. Endometrium – Inner layer which varies in thickness & echo pattern with stage of the menstrual cycle 2. Myometrium – Thick, middle muscle layer 3. Serosa – Thin outer layer Mani Montazemi, RDMS Female Anatomy Mani Montazemi, RDMS Female Anatomy Myometrium inner muscular layer – low echogenicity Mani Montazemi, RDMS Female Anatomy Myometrium middle muscular layer – moderate echogenicity Mani Montazemi, RDMS Female Anatomy Myometrium Serosa arcuate arterial & venous plexus Mani Montazemi, RDMS Female Anatomy Mani Montazemi, RDMS Female Anatomy 5 1/6/2014 Endometrium central stripe Mani Montazemi, RDMS Female Anatomy Endometrium inner functional layer Mani Montazemi, RDMS Female Anatomy Endometrium outer basal layer Endometrial Thickness • Thickness and echotexture depend upon hormonal status Mani Montazemi, RDMS Female Anatomy Mani Montazemi, RDMS Female Anatomy Normal Endometrial Cycle Early Proliferative Phase Mani Montazemi, RDMS Female Anatomy Linear Echogenic Normal Endometrial Cycle Late Proliferative Phase Mani Montazemi, RDMS Female Anatomy Multilayered 6 1/6/2014 Normal Endometrial Cycle Secretory Phase Mani Montazemi, RDMS Female Anatomy Homogeneously Echogenic Endometrial Appearance • Under influence of estrogen & progestrone • The glandular epithelium secrets a glycogen rich fluid • Spiral arteries become tortuous Mani Montazemi, RDMS Female Anatomy Intermenstrual Bleeding When should the ultrasound examination be performed? Endometrial Appearance Mani Montazemi, RDMS Female Anatomy Premenopausal Endometrium Basal layer remains thin & hyperechoic throughout the menstrual cycle Mani Montazemi, RDMS Female Anatomy Intermenstrual Bleeding When should the ultrasound examination be performed? • Immediate Postmenstrual Phase • The endometrium is thin in this phase & small endometrial lesions are least likely to be obscured Mani Montazemi, RDMS Female Anatomy Mani Montazemi, RDMS Female Anatomy 7 1/6/2014 Endometrial Thickness 1-3 mm “Early Proliferation Phase” Endometrial Thickness 4-7 mm “Late Proliferation Phase” Mani Montazemi, RDMS Female Anatomy Endometrial Thickness Mani Montazemi, RDMS Female Anatomy Endometrial Thickness 8-15mm “Secretory Phase” Mani Montazemi, RDMS Female Anatomy Endometrial Appearance Mani Montazemi, RDMS Female Anatomy Mani Montazemi, RDMS Female Anatomy Endometrial Appearance Mani Montazemi, RDMS Female Anatomy 8 1/6/2014 Endometrial Thickness How to Measure? SAG TRV Postmenopausal < 5mm Mani Montazemi, RDMS Female Anatomy Mani Montazemi, RDMS Female Anatomy How to Measure? SAG TRV Mani Montazemi, RDMS Female Anatomy Endometrial Measurements Mani Montazemi, RDMS Female Anatomy Endometrial Measurements • Not included in measurement: – fluid/debris in canal – subendometrial halo Mani Montazemi, RDMS Female Anatomy Mani Montazemi, RDMS Female Anatomy 9 1/6/2014 Endometrial Measurements * * Endometrial Measurements * * Mani Montazemi, RDMS Female Anatomy Endometrial Appearance Mani Montazemi, RDMS Female Anatomy Endometrial Appearance * * * * Mani Montazemi, RDMS Female Anatomy Mani Montazemi, RDMS Female Anatomy Postmenopausal Endometrium Postmenopausal Endometrium • The endometrium becomes atrophic • Small amounts are common, especially in women receiving HRT • Appears as a thin echogenic line 4-5 mm thick Mani Montazemi, RDMS Female Anatomy • Aids in evaluating the appearance of the endometrium Mani Montazemi, RDMS Female Anatomy 10 1/6/2014 Uterine Positions Uterine Positions • Anteverted – Tilted forward • Anteflexed – Forward fold between the body & the cervix • Retroverted – Tilted backwards • Retroflexed – Flexed between body & cervix Mani Montazemi, RDMS Female Anatomy Tilted Forward Mani Montazemi, RDMS Female Anatomy Uterine Positions Uterine Positions Tilted backwards Mani Montazemi, RDMS Female Anatomy Mani Montazemi, RDMS Female Anatomy Uterine Size • Childhood – 2/3 cervix, 1/3 body & fundus • Puberty – 1 to 1 ratio between cervix body & fundus • Adult – 1/3 cervix, 2/3 body & fundus Mani Montazemi, RDMS Female Anatomy Uterine Shape • Childhood – Cylindrical shape – Corpus shrinks due to withdrawal of maternal hormones – Will not grow until ovaries produce hormones • Puberty – Assumes the pear shape • Menopausal – Shrinks & regress to prepubertal state Mani Montazemi, RDMS Female Anatomy 11 1/6/2014 Uterine Measurements Uterine Measurements SAG 8 Length TRV x 5Width x 3AP cm Length Mani Montazemi, RDMS Female Anatomy Uterine Measurements SAG TRV AP AP Mani Montazemi, RDMS Female Anatomy Uterine Measurements Mani Montazemi, RDMS Female Anatomy Width Mani Montazemi, RDMS Female Anatomy Uterine Measurements Mani Montazemi, RDMS Female Anatomy Uterine Measurements Mani Montazemi, RDMS Female Anatomy 12 1/6/2014 Uterine Measurements Uterine Measurements Don’t Mani Montazemi, RDMS Female Anatomy Mani Montazemi, RDMS Female Anatomy Ovary Ovary • Range in size according to the age 3 Mani Montazemi, RDMS Female Anatomy Length x 2 Width x 1 AP cm Mani Montazemi, RDMS Female Anatomy Ovary Ovarian Volume • Volume – – – – LxWxH/2 Adults – 9.8cm3 (+/-5.8) Girls until about 5 yrs of age – < 1cm3 Menarche – 4.2cm3 (+/-2.3) 3 x 2 x 2 / 2 = 6cm3 Mani Montazemi, RDMS Female Anatomy Mani Montazemi, RDMS Female Anatomy 13 1/6/2014 Follicular Cysts Mani Montazemi, RDMS Female Anatomy Follicular Cysts • • • • • Follicular Cysts Mani Montazemi, RDMS Female Anatomy Follicular Cysts < 2.5 cm in diameter Cysts are usually larger than a mature follicle (3-8cm) Thin walled and unilocular Usually unilateral Can be multiple and bilateral Mani Montazemi, RDMS Female Anatomy Follicular Cysts Mani Montazemi, RDMS Female Anatomy Normal Anatomy of the Female Pelvis Thank You Mani Montazemi, RDMS Female Anatomy Mani Montazemi, RDMS Female Anatomy 14 1/6/2014 Transvaginal Scanning Techniques Sagittal Scan Mani Montazemi, RDMS Clinical Instructor – Imaging Manager Baylor College of Medicine Division of Maternal-Fetal Medicine Department of Obstetrics and Gynecology Texas Children’s Hospital, Pavilion for Women Houston Texas Mani Montazemi, RDMS Endovaginal Sonography Mani Montazemi, RDMS Endovaginal Sonography Sagittal Scan H A Sagittal Scan F P Mani Montazemi, RDMS Endovaginal Sonography Mani Montazemi, RDMS Endovaginal Sonography Sagittal Scan Mani Montazemi, RDMS Endovaginal Sonography Sagittal Scan Mani Montazemi, RDMS Endovaginal Sonography 1 1/6/2014 Transverse Scan Transverse Scan A R L P Mani Montazemi, RDMS Endovaginal Sonography Mani Montazemi, RDMS Endovaginal Sonography Transverse Scan Mani Montazemi, RDMS Endovaginal Sonography Transvaginal – Image Orientation Transabdominal Transverse Mani Montazemi, RDMS Endovaginal Sonography Transvaginal – Sagittal Plane • Sagittal plane • Transverse plane F A F H P A P H Mani Montazemi, RDMS Endovaginal Sonography Mani Montazemi, RDMS Endovaginal Sonography 2 1/6/2014 Transvaginal – Sagittal Plane Transvaginal – Sagittal Plane Mani Montazemi, RDMS Endovaginal Sonography Mani Montazemi, RDMS Endovaginal Sonography Transvaginal – Sagittal Plane Transvaginal – Sagittal Plane • Transducer notch is on top • Thumb on notch • Urinary bladder is in left upper corner of sagittal image • make sure the image is not reversed Feet A H Anterior P Posterior F Head Mani Montazemi, RDMS Endovaginal Sonography Mani Montazemi, RDMS Endovaginal Sonography Transvaginal – Sagittal Plane Anteverted Uterus F A Anteverted Uterus Mani Montazemi, RDMS Endovaginal Sonography P H Uterine Fundus Mani Montazemi, RDMS Endovaginal Sonography 3 1/6/2014 Transvaginal – Sagittal Plane Retroverted Uterus F A P H Uterine Fundus Retroverted Uterus Mani Montazemi, RDMS Endovaginal Sonography Transvaginal – Sagittal Plane Mani Montazemi, RDMS Endovaginal Sonography Mani Montazemi, RDMS Endovaginal Sonography Transvaginal – Sagittal Plane Mani Montazemi, RDMS Endovaginal Sonography Transvaginal – Sagittal Plane A H F Transabdominal P Mani Montazemi, RDMS Endovaginal Sonography Mani Montazemi, RDMS Endovaginal Sonography 4 1/6/2014 Transverse Scan F A H A F P Transabdominal Transvaginal P H Mani Montazemi, RDMS Endovaginal Sonography Mani Montazemi, RDMS Endovaginal Sonography Transabdominal – Transverse Mani Montazemi, RDMS Endovaginal Sonography Transvaginal – Transverse Mani Montazemi, RDMS Endovaginal Sonography Transvaginal – Transverse Transvaginal – Transverse Feet Right Left Head Anteverted Mani Montazemi, RDMS Endovaginal Sonography Mani Montazemi, RDMS Endovaginal Sonography 5 1/6/2014 Transvaginal – Transverse Transvaginal – Transverse Plane Feet H L R Right Left F Head Retroverted Mani Montazemi, RDMS Endovaginal Sonography Mani Montazemi, RDMS Endovaginal Sonography Transvaginal – Transverse F A R Mani Montazemi, RDMS Endovaginal Sonography L R L Transabdominal Transvaginal P H Mani Montazemi, RDMS Endovaginal Sonography Transvaginal Scanning Motions • • • • Insert & withdraw Raise and lower Angulation Rotation Mani Montazemi, RDMS Endovaginal Sonography Transvaginal Sonography Thank You Mani Montazemi, RDMS Endovaginal Sonography 6 1/6/2014 Evaluation of the Cervix Predicting Preterm Delivery Ultrasound Evaluation Of the Cervix • Digital • Fetal Fibronectin • Ultrasound Mani Montazemi, RDMS Mani Montazemi, RDMS Ultrasound of the Cervix Clinical Instructor – Imaging Manager Baylor College of Medicine Division of Maternal-Fetal Medicine Department of Obstetrics and Gynecology Texas Children’s Hospital, Pavilion for Women Houston Texas Least accurate method to measure cervical length & to identify a cervical funnel Mani Montazemi, RDMS Ultrasound of the Cervix Lower Uterine Segment Mani Montazemi, RDMS Ultrasound of the Cervix Transabdominal Translabial Transvaginal Mani Montazemi, RDMS Ultrasound of the Cervix J Ultrasound Med 22:239-241, 2003 Filling of the Bladder For Pelvic Sonograms Beryl R. Benacerraf, MD Mani Montazemi, RDMS Ultrasound of the Cervix Lower Uterine Segment Mani Montazemi, RDMS Ultrasound of the Cervix 1 1/6/2014 Transabdominal Examination Pitfalls – – – – – – – Presenting fetal part Bladder distension Symphysis pubis cartilage External os not visible Critical angle artifact Large maternal body habitus Lower uterine contraction Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix Transabdominal Examination Pitfalls – – – – – – – Mani Montazemi, RDMS Ultrasound of the Cervix Placenta Previa: False Positives Over distended bladder can compress the lower uterine segment to give the appearance of an anterior previa Mani Montazemi, RDMS Ultrasound of the Cervix Presenting fetal part Bladder distension Symphysis pubis cartilage External os not visible Critical angle artifact Large maternal body habitus Lower uterine contraction Mani Montazemi, RDMS Ultrasound of the Cervix Transabdominal Examination Pitfalls – – – – – – – Presenting fetal part Bladder distension Symphysis pubis cartilage External os not visible Critical angle artifact Large maternal body habitus Lower uterine contraction Mani Montazemi, RDMS Ultrasound of the Cervix 2 1/6/2014 Transabdominal Examination Transabdominal Examination Pitfalls Pitfalls – – – – – – – – – – – – – – Presenting fetal part Bladder distension Symphysis pubis cartilage External os not visible Critical angle artifact Large maternal body habitus Lower uterine contraction Mani Montazemi, RDMS Ultrasound of the Cervix Transabdominal Examination Pitfalls – – – – – – – Presenting fetal part Bladder distension Symphysis pubis cartilage External os not visible Critical angle artifact Large maternal body habitus Lower uterine contraction Mani Montazemi, RDMS Ultrasound of the Cervix Placenta Previa: False Positives Presenting fetal part Bladder distension Symphysis pubis cartilage External os not visible Critical angle artifact Large maternal body habitus Lower uterine contraction Mani Montazemi, RDMS Ultrasound of the Cervix Lower Uterine Segment Contraction Post Void • Are common! • These contractions are very slow & long Mani Montazemi, RDMS Ultrasound of the Cervix “Contractions” Round myometrium Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix 3 1/6/2014 “Contractions” Thick & asymmetric LUS Mani Montazemi, RDMS Ultrasound of the Cervix “Contractions” “Contractions” Thick & asymmetric LUS Myometrial Thickness ≤ 1.5 cm Mani Montazemi, RDMS Ultrasound of the Cervix Thick & asymmetric LUS Myometrial Thickness ≤ 1.5 cm “Contractions” Cervical length > 5 – 5.5cm Thick & asymmetric LUS Myometrial Thickness ≤ 1.5 cm Cervical length > 5 – 5.5cm “S” shaped cervical canal Mani Montazemi, RDMS Ultrasound of the Cervix “Contractions” Mani Montazemi, RDMS Ultrasound of the Cervix Thick & asymmetric LUS Myometrial Thickness ≤ 1.5 cm “Contractions” Cervical length > 5 – 5.5cm Thick & asymmetric LUS Myometrial Thickness ≤ 1.5 cm Cervical length > 5 – 5.5cm “S” shaped cervical canal “S” shaped cervical canal Internal os cephalad to bladder reflection Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix 4 1/6/2014 Common Indications for TV Evaluation of Cervix If indicated, the cervical length should ALWAYS be measured with transvaginal approach Mani Montazemi, RDMS Ultrasound of the Cervix • Evaluating patients with vaginal bleeding to look for placenta previa • Fetal parts • Diagnosing cervical incompetence • Assessing cervical effacement and dilation in patients with preterm labor • Multiple Gestations • Post cerclage placement • History of preterm labor • Succenturiate lobed placentas • Velamentous cord insertion Mani Montazemi, RDMS Ultrasound of the Cervix Preterm Delivery Whether that‟s due to incompetent cervix or preterm labor leading to preterm birth is the single most common cause of poor neonatal outcome Mani Montazemi, RDMS Ultrasound of the Cervix Transvaginal Approach Mani Montazemi, RDMS Ultrasound of the Cervix Preterm Delivery • • • • Effects 8% of births Accounts for 15 – 20% of neonatal deaths 75% of non-anomaly deaths Treatment > $5 billion/yr USA Mani Montazemi, RDMS Ultrasound of the Cervix Transvaginal Approach Mani Montazemi, RDMS Ultrasound of the Cervix 5 1/6/2014 Transvaginal Approach Transvaginal Approach Feet Anterior Posterior Head Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix Anatomic Landmarks for Vaginal Sonography Bladder External Os Chorioamnion Membrane Mani Montazemi, RDMS Ultrasound of the Cervix Cervical Length Internal Os “Minimizing the effect of excess pressure” Good midline sagittal view of the cervix Transvaginal Approach Mani Montazemi, RDMS Ultrasound of the Cervix Transvaginal Approach Wall of the vagina * Be careful - Excess Pressure Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix 6 1/6/2014 Excessive Probe Pressure Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix Excessive Probe Pressure Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix Cervical Length • • • • Upper limit of normal Average Lower limit of normal Pathologically decreased Mani Montazemi, RDMS Ultrasound of the Cervix Cervical Length 5.0 cm 4.0 cm 3.0 cm 2.0 cm Mani Montazemi, RDMS Ultrasound of the Cervix 7 1/6/2014 “ One step” vs. “Two step” Technique “ One step” vs. “Two step” Technique Straight or Curved Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix Curved Cervix Cervical Changes • Essentially the same in – Term labor – Preterm labor – Cervical incompetence Mani Montazemi, RDMS Ultrasound of the Cervix If height ≥ 5 mm “two step” technique Mani Montazemi, RDMS Ultrasound of the Cervix Cervical Changes Cervical Changes •T •Y •V •U • Trust • Your • Vaginal • Ultrasound Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix 8 1/6/2014 Cervical Changes Cervical Changes • • • • • T Y V U Mani Montazemi, RDMS Ultrasound of the Cervix Dilation Effacement Funneling or Beaking Posterior – caudal Bulging membranes Mani Montazemi, RDMS Ultrasound of the Cervix Cervical Changes • Dilation – Widening of the endocervical canal from side to side Mani Montazemi, RDMS Ultrasound of the Cervix Cervical Changes • Effacement – Shortening of the cervix – Reduction of the cervical length from internal end to external end Mani Montazemi, RDMS Ultrasound of the Cervix Cervical Changes • Funneling or Beaking – Extension of amniotic fluid for some variable distance (≥ 5mm) into the endocervical canal from internal os toward external os – „V‟ shape • More common, triangular “notch” at the internal os – „U‟ shape • Uncommon, typically larger than V-shaped variety • Usually deeper than it is broad and may be dynamic Mani Montazemi, RDMS Ultrasound of the Cervix Cervical Changes • Funneling or Beaking – Extension of amniotic fluid for some variable distance (≥ 5mm) into the endocervical canal from internal os toward external os – „V‟ shape • More common, triangular “notch” at the internal os – „U‟ shape • Uncommon, typically larger than V-shaped variety • Usually deeper than it is broad and may be dynamic Mani Montazemi, RDMS Ultrasound of the Cervix 9 1/6/2014 Cervical Changes • Funneling or Beaking – Extension of amniotic fluid for some variable distance (≥ 5mm) into the endocervical canal from internal os toward external os – „V‟ shape • More common, triangular “notch” at the internal os – „U‟ shape • Uncommon, typically larger than V-shaped variety • Usually deeper than it is broad and may be dynamic Mani Montazemi, RDMS Ultrasound of the Cervix Cervical Changes • Funneling or Beaking – Extension of amniotic fluid for some variable distance (≥ 5mm) into the endocervical canal from internal os toward external os – „V‟ shape • More common, triangular “notch” at the internal os – „U‟ shape • Uncommon, typically larger than V-shaped variety • Usually deeper than it is broad and may be dynamic Mani Montazemi, RDMS Ultrasound of the Cervix Cervical Beaking – V Shape Mani Montazemi, RDMS Ultrasound of the Cervix Cervical Funneling – U Shape Mani Montazemi, RDMS Ultrasound of the Cervix Cervical Funneling Diagnostic Challenge Funnel Length > 1.6 cm Cervical Length < 2.0 cm Funnel Width >1.4 cm Sonographic Criteria Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix 10 1/6/2014 Diagnostic Challenge Mani Montazemi, RDMS Ultrasound of the Cervix Diagnostic Challenge Mani Montazemi, RDMS Ultrasound of the Cervix Diagnostic Challenge Mani Montazemi, RDMS Ultrasound of the Cervix Diagnostic Challenge Mani Montazemi, RDMS Ultrasound of the Cervix Cervical Changes to • Posterior Caudal – In the early to mid pregnancy the cervix points posteriorly toward the sacrum Mani Montazemi, RDMS Ultrasound of the Cervix Cervical Changes to • Posterior Caudal – In the early to mid pregnancy the cervix points posteriorly toward the sacrum – As the woman progresses towards labor the cervix starts to rotate to line up with vagina Mani Montazemi, RDMS Ultrasound of the Cervix Soft 11 1/6/2014 Cervical Changes Preterm Labor “to evaluate for cervical dilation” • Bulging of membranes – Fluid extends all the way to the external os – If into vagina, delivery likely unstoppable BLADDER AF Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix Preterm Labor “to evaluate for cervical dilation” Mani Montazemi, RDMS Ultrasound of the Cervix Diagnostic Challenge Mani Montazemi, RDMS Ultrasound of the Cervix Cervix – Dynamic Changes Remember Cervical Change is Dynamic! Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix 12 1/6/2014 Cervix – Dynamic Changes Mani Montazemi, RDMS Ultrasound of the Cervix Cervical Stress Test with Gentle Pressure Mani Montazemi, RDMS Ultrasound of the Cervix Cervix – Dynamic Changes Mani Montazemi, RDMS Ultrasound of the Cervix Cervical Stress Test with Gentle Pressure Mani Montazemi, RDMS Ultrasound of the Cervix Cervical Stress Test with Gentle Pressure Don’t… • Use cervical ultrasound as a screening test Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix 13 1/6/2014 Don’t… Don’t… • Rely upon transabdominal ultrasound to measure length to identify a funnel. It is not reproducible because of the variable pressure created by the maternal bladder • Measure cervical length before16 weeks, too much variation to be useful Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix Introduction to Ultrasound Evaluation of the Cervix Diagnostic Challenge Thank You Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix Diagnostic Challenge Vasa Previa • Partial or complete obstruction of the internal cervical os by blood vessels Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix 14 1/6/2014 Vasa Previa • • • • • Low lying placentas; Succenturiate lobed placentas; Velamentous cord insertion; Multiple pregnancies; Pregnancies resulting from IVF Risk Factors Most Common Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix Placenta Previa – Marginal Placenta Previa – Partial Inferior edge of placenta within 2cm of IO Often resolves with advancing pregnancy Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix Placenta Previa – Complete Mani Montazemi, RDMS Ultrasound of the Cervix Edge of placenta partially covers IO Difficult to differentiate from marginal previa Often resolves with advancing pregnancy Asymmetric complete previa Small part of placenta crosses IO May resolve with advancing pregnancy If > 1.5 cm crosses IO then less likely to resolve Placenta Previa – Complete Mani Montazemi, RDMS Ultrasound of the Cervix Symmetric complete previa Placenta centrally implanted on cervix Will not resolve with advancing pregnancy 15 1/6/2014 3 weeks later 27 weeks Hospitalized with bleeding Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix • It is recognized that apparent placental position early in pregnancy may not correlate well with its location at the time of delivery • It is recognized that apparent placental position early in pregnancy may not correlate well with its location at the time of delivery • “Trophotropism” • “Trophotropism” – The ability or the desire of the placenta to seek a blood supply – Proliferation of placental villi in areas of better blood supply (corpus , fundus) Kurt Benirschke, MD – The ability or the desire of the placenta to seek a blood supply – Proliferation of placental villi in areas of better blood supply (corpus , fundus) Kurt Benirschke, MD Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix 16 1/6/2014 Trophotropism Succenturiate lobe • May be low-lying or cross internal os Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix Trophotropism Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix 17 1/6/2014 Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix Mani Montazemi, RDMS Ultrasound of the Cervix Introduction to Ultrasound Evaluation of the Cervix Thank You Mani Montazemi, RDMS Ultrasound of the Cervix 18 12/22/2015 Sonography in the First Trimester Basic Embryology 1mm Sac G. William Shepherd PhD, RDMS, RVT 1 Embryonic Timeline Ovulation: Day 14-16 Fertilization: Day 14-16 Zygote to Morula: Day 16-18 Morula to Blastocyst: Day 18-19 Implantation: Day 19-20 2 Embryology Terms Gamete --------- Before fertilization Zygote ---------- After fertilization Morula --------- 16 -32 Cells (18 Days) Blastocyst ---------- 20 Days Embryonic Disc --- 28 Days Ultrasound Detection --- 31 Days Earliest Heart Beat ------ 36 Days Week 3 3 Yolk Sac Formation: 4w1d 4 Goals for a 1st Trimester Scan 5 Visualization and localization of the gestational sac Determination of viability Determination of the # of embryos & viability Estimation of gestational age Determination of any detectable anomalies 6 1 12/22/2015 Earliest Definite Ultrasound Visualization: 31days 4W6D 7 Is this an IUP? coronal Pre-embryonic (embryonic disc stage 4w4d or 32days) 8 “Double Sac” Sign 9 10 “Double Sac” Sign 11 12 2 12/22/2015 Pre-Embryonic Period: 3-5 weeks (by LMP) zygote, morula, blastocyst, implantation, embryonic disc, gastrulation (tubular embryo) Embryonic Period: 6-10 weeks heart beat, and organ formation Fetal Period: 11 weeks to term (all organs are present) 13 14 5 weeks by LMP Estimation of Gestational Age from the MSD (mean sac diameter) Age in Days (by LMP) = (L+W+H) + 30 3 15 16 5w0d by LMP Transabdominal scan with EV probe 1cm 4mm 6mm Width (from trv image) = 6 6+6+4 divided by 3 = 5.3, +30 = 35.3d or 5w 17 18 3 12/22/2015 EV Coronal (trans) 19 20 5 weeks 6 days by LMP Human Chorionic Gonadotropin + x x + xx 13mm ++ 11mm Width 15mm MSD 13 = 43d =6w1d 9.25 21 Beta Chorionic Gonadotropin Levels MSD 2mm 5mm 10mm 15mm 20mm Age (weeks) 5.0 5.4 6.0 6.6 CRL 7.3 Made by trophoblastic cells Detectable after implantation Doubling time every 2-3 days Correlates well with embryonic and sac size Level maximizes at about 8 weeks Max level is about 50,000 -100,000 IU/L Declines after 10-12 weeks HCG Level 1,164 1,932 4,478 10,379 24,060 22 4-5mm x x * Filly, in Ultrasonography in Obstetrics and Gynecology, ed Callen, W.B. Saunders, Philadelphia, 1994. 23 24 4 12/22/2015 “Diamond Ring” Sign Embryonic Timeline Week 6: Heartbeat will be detectable during this week. This is the neural tube stage Weeks 6-10: Essentially all of the tissues and organs of the embryo will form during this period. Week 11: All of the organs are present and all but a portion of the bowel and the external genitalia are in their final positions. Week 12: The bowel will reenter the fetal abdomen. 25 5w5d 6w1d 26 CRL and Gestational Age CRL 2mm 4 8 10 15 20 25 30 40 50 3 days development and growth Gest. Age 5.7 weeks 6.1 6.7 7.2 7.9 8.6 9.2 9.9 10.9 11.7 27 CRL 60mm 70 80 90 100 110 130 Gest. Age 12.5 weeks 13.2 14.0 14.9 15.9 16.9 17.9 Hadlock et al Radiology 18: 501, 1992 28 + + 5mm 6w1d “Double Bleb” Sign = Yolk sac and the Early Embryo 29 30 5 12/22/2015 6w1d 6w0d Day 43 Day 48 Day 55 10w0d Day 61 Day 66 Day 70 31 32 6w3d 2mm Early Embryo 5w6d 33 34 CRL = 18mm 8w3d Embryonic Period 7w3d Fluid? Oblique Scanning Plane Fluid? 35 36 6 12/22/2015 Don’t include the yolk sac in the CRL 13mm 7w2d 37 38 Be aware of fetal position 39 41 40 6w1d 7w4d 8w4d 10w3d 42 7 12/22/2015 Manipulation of Transducer for CRL After 13 weeks use BPD, HC, AC, and FL 43 Skeletal Development 8w2d 44 10w3d 9w3d 45 Questions? 46 Indications for a First Trimester Scan Is there a pregnancy? Where is it? Is it alive? How many embryos? Are they all alive? All IUPs? How far along is the pregnancy? Anything wrong with the fetus? Sac? Adnexa? 9.5 47 Vaginal bleeding Size and date discrepancy No heart tones Pelvic pain Accurate dating for future C-section History of an anomaly Trauma 48 8 12/22/2015 7 Week Embryo Significance of the Yolk Sac Earliest landmark in the early gestational sac Identifies an IUP Helps to locate the embryo and heart beat Should be round and “cystic” 3-6mm 1 yolk sac per embryo, can help identify monoamnionic twins Should disappear by 12 weeks 49 50 7 Week Embryo Yolk Sac Yolk Sac Amnion Chorionic Fluid Amniotic Fluid 51 Yolk Sac Too big 52 Irregular-Shaped Yolk Sac Amorphous Embryo 1 cm 1.5 cm Free Fluid 53 54 9 12/22/2015 Vaginal Bleeding (1st Trimester) Implantation Bleed Abortion Subchorionic Hemorrhage Placental Previa Ectopic Pregnancy Blighted Ovum Compressed Yolk Sac 55 56 The future Jen Shepherd Implantation Bleed Most common cause of 1st trimester vaginal bleeding Generally not significant Sonolucent area between the chorion and uterus (near the internal os) 57 58 Subchorionic Bleeds Vaginal Bleeding (1st Trimester) Implantation Bleed Subchorionic Hemorrhage Abortion Placental Previa Ectopic Pregnancy Blighted Ovum 59 Can be behind the placenta Can be behind the chorion lavae Can be behind the chorionic plate of the placenta Prognosis depends upon the cause and how much of the placenta is involved: >1/3 prognosis worsens 60 10 12/22/2015 61 62 63 64 1/4 of placenta is separated from uterus Vaginal Bleeding: 1st Trimester 8w2d 65 Implantation Bleed Subchorionic Hemorrhage Blighted Ovum Placental Previa Ectopic Pregnancy Abortion 66 11 12/22/2015 Blighted Ovum: Arrested or absent development of the embryonic pole (trophoblasts develop) No embryo or Yolk Sac 67 Growth will fall off HCG will level off Sac may move toward Cx 68 Trophoblastic ring may become irregular and thin < 2mm 69 70 71 72 Multiple Irregularities 12 12/22/2015 About 20% of all eggs are incapable of forming an embryo and will produce a blighted ovum or new term an anembryonic pregnancy. Some pregnancies will form an embryo and it will die early. This is early embryonic demise. There is an important, although often overlooked difference between anembryonic pregnancy and early embryonic demise. Anembryonic pregnancies do not increase the chances of future pregnancy failure. They are due to some inherently “bad” eggs found in all women. Early embryonic demise may herald a genetic defect and thus signify possible future pregnancy failures. Genetic testing may be desirable for Patients with multiple early demise pregnancies. These pregnancies may have a visible yolk sac but the embryo usually becomes necrotic. 73 Vaginal Bleeding: 1st Trimester 74 Placenta Previa Implantation Bleed Abortion Subchorionic Hemorrhage Placental Previa Ectopic Pregnancy Blighted Ovum The placenta covers the internal cervical os Unusual finding during the 1st trimester Placental “migration” may eliminate the previa Vaso previa may be present even though the placenta has “migrated”. Rule out vaso previa with color Doppler A partial mole can present with placenta previa 75 76 Vaginal Bleeding: 1st Trimester Placenta Previa 16w1d 77 Implantation Bleed Abortion Subchorionic Hemorrhage Placental Previa Ectopic Pregnancy Blighted Ovum 78 13 12/22/2015 Glossary of 1st Trimester Terms Inevitable Abortion Abortion: Premature expulsion of the gestation from the uterus Incomplete Abortion: The expulsion of only a portion of the gestational products from the uterus 79 80 Missed Abortion Fetal Parts Abortion in progress 81 82 Retained Products of Conception 83 84 14 12/22/2015 Findings for Embryonic Demise Old Criteria Findings for Embryonic Demise The Findings Below Depend upon Body Habitus and Type of Transducer, Endovag or transabd No Sac Growth on Serial Exams No Cardiac Pulsations in a 5mm Embryo No Embryo Seen in a Sac 25mm MSD No Yolk Sac Seen in a 20mm MSD Sac Trophoblastic Ring is not Intact No Sac Growth on Serial Exams A 7 -10 day interval between scans is recommended Give the embryo a chance EV scanning is always best Abdallah et al US Obstet & Gynecol 2011 85 The Gestational Sac Grows about 1mm/Day 1 Week Should Give a Statistically Significant Increase in MSD Jan 4 Jan 11 MSD = 3mm 86 Findings for Embryonic Demise MSD = 10mm 87 Reading an M-Mode 88 Findings for Embryonic Demise 1 second Heart rate only 60 bpm Slow Cardiac Pulsations in a 5 (now 7) mm Embryo in an endovaginal ultrasound examination No Cardiac Pulsations in a 9mm Embryo in a transabdominal ultrasound examination 1 second M-Mode No Heart-beat Heart rate 160 bpm 89 90 15 12/22/2015 91 92 93 94 95 96 16 12/22/2015 Findings for Embryonic Demise No Embryo Seen in a Sac 18 (now 25) mm MSD in an endovaginal ultrasound examination 97 Findings for Embryonic Demise 98 Findings for Embryonic Demise No Embryo Seen in a Sac 25mm MSD in an transabdominal or EV ultrasound examination Was 20mm No Yolk Sac Seen in a 10mm MSD Gestational Sac with endovaginal scanning 99 Findings for Embryonic Demise 100 New Criteria for Embryonic Demise No Yolk Sac Seen in a 20mm MSD Gestational Sac with transabdominal scanning MSD 25mm No Sac Growth on Serial Exams No Cardiac Pulsations in a 7 mm Embryo* No Cardiac Pulsations in a 9mm Embryo ** No Embryo Seen in a Sac 25 mm MSD* No Embryo Seen in a Sac 25mm MSD** No Yolk Sac Seen in a 10mm MSD Sac * No Yolk Sac Seen in a 20mm MSD Sac** * endovaginal scanning ** transabdominal scan 10.0 101 102 17 12/22/2015 Anembryonic Pregnancy Small for Dates Normal Pregnancy / Wrong Dates Anembryonic Pregnancy (blighted ovum) Ectopic Pregnancy Fetal Demise Oligohydramnios Intrauterine Growth Retardation (IUGR) Embryonic Demise Oligohydramnios S<D Ectopic Pregnancy 103 104 Pseudo-sac Ectopic Pregnancy 95% occur in the tube 5% are interstitial and are the most dangerous Cornual and cervical ectopics are increasing In vitro procedures increase the chance of ectopic pregnancy Heterotopic: IUP plus an ectopic Transabdominal scans 105 Pseudo-sac Endovaginal scans 106 Ruptured Ectopic 107 Live Ectopic Pregnancy in Right Fallopian Tube 108 18 12/22/2015 Ectopic Pregnancy in Right Cornu Cervical Ectopic Pregnancy 109 110 Right & Left Horns of Bicornuate Uterus Ectopic? Uterus? 111 112 Hemorrhagic Corpus Luteum Can Look Like an Ectopic 113 114 19 12/22/2015 Molar Pregnancy Large for Dates Vaginal Bleeding Very High HCG May be a live embryo 1 in 1200 pregnancies in the USA Risk is 20-40 fold higher if patient had a previous molar pregnancy (1 in 30-60) 115 116 Theca Lutein Cysts There may or may not be a sac. 117 The arrow heads point to the major portion of the mole. The white arrows point to echogenic invasive villi that extent almost to the serosal surface of the uterus (black arrows). 119 118 Partial Mole at 12 weeks -Top, 14 weeks - Bottom 120 20 12/22/2015 Large for Dates Normal Pregnancy / Wrong Dates Molar Pregnancy Gestation with Mass / Masses Multiple Gestation 10.25 121 Bicornuate Uterus 122 Bicornuate Uterus IUP 123 124 Early Pregnancy with a Mass Hydatidiform Mole Theca Lutien Cysts 125 126 21 12/22/2015 Multiple Gestation 127 128 Triplets Bleeds B A 3 C 1 E D 2 129 Anomalies: Detectable in the 1st Trimester (Endovaginal Scanning is Best) Anencephaly Acrania Cystic hygroma Hydrops Conjoined twins Large omphalocele Severe gastroschisis Thanatophoric dwarf 130 Normal Head at 12 Weeks Transverse Head at 12 Weeks Choriod Plexus Frontal Occipital 131 132 22 12/22/2015 Anencephaly at 12w3d 133 134 2mm Acrania at 10w2d Normal Nuchal Translucency 10w6d 135 136 Normal Herniation of the Gut into the Base of the Cord at 11w2d Bilateral Cystic Hygroma at 9w4d 137 138 23 12/22/2015 Omphalocele 12w4d Low Beta HCG Levels Blighted Ovum Wrong Dates Ectopic Pregnancy 139 140 141 142 High Beta HCG Levels Wrong Dates Multiple Gestation Molar Pregnancy Choriocarcinoma 24 12/22/2015 Obstetric Scanning: Normal Anatomy gshepherd@hvc.rr.com Bill Shepherd PhD, RDMS, RVT 1 Objectives 2nd and 3rd Trimester (1) 2 Objectives 2nd and 3rd Trimester (2) Evaluation of basic fetal anatomy 4 chamber Heart, Diaphragm Stomach Urinary Bladder & Kidneys Abdominal Cord & Insertions Skeleton Head, Face, Neck Documentation of fetal life, # & presentation Documentation of amniotic fluid volume Documentation of placental location Documentation of obstetric age Evaluation of uterus, fluid, cervix & placenta These are the minimum requirements of a 2nd trimester scan from the American Institute of Ultrasound in Medicine (1985) 3 Determine Fetal Presentation 4 Sag mll Show Fetal Position SAG ML Breech or transverse head right 5 6 1 12/22/2015 Drag inferior to superior Slide Inferior to Superior 7 8 Motion 11 weeks / 24 weeks Documentation of Life 1. Fetal motion 2. Fetal heart motion 3. Fetal circulation (Doppler) 9 M-Mode of the Fetal Heart 1 2 3 4 10 M-Mode 5 beats 2 seconds 150 beats /minute 11 12 2 12/22/2015 Number of Fetuses Amniotic Fluid 1. AFI 2. Largest pocket 3. “Eyeball” 13 14 Lower Uterine Segment Posterior Anterior ? Placental Location 15 16 Placenta Translabial or Transvaginal Sonography 17 Placental Position LUS - Rule out previa 18 3 12/22/2015 Placenta Previa? ? Incompetent Cervix 11.0 19 33 weeks 20 Tropho-tropism: Sag ml The preferential proliferation of trophoblastic villi into regions of better endometrial blood supply Atrophy of villi occurs where there is poorer endometrial blood supply 21 22 Placenta Previa: Risk Factors Tropho-tropism Explains: Advance maternal age High parity Prior cesarean section* Prior elective abortion Multiple fetuses Smoking IVF Resolution of placenta previa Succenturiate lobes of placentas Marginal & velamentous cord insertions Vasoprevia Prolapsed cord 23 24 4 12/22/2015 Placenta Previa: False Positives Risk of Placenta Previa After Caesarian Sections # of C-Sections 0 1 2 3 4 Overfilling of the bladder Risk of Previa .26% .65% 1.8% 3.0% 10% Pseudoprevia 25 26 False Positives Normal Pseudo-previa Previa Contraction 3cm 6cm 27 Placental Abruption 28 Placental Abruption Placental abruption is premature separation of the placenta from the uterus. Approximately 1% of pregnancies. 15-25% of all perinatal mortality. Usually pain & vaginal bleeding. A central abruption may present with pain but no bleeding. The recurrent risk is about 1 in 8 pregnancies. 29 30 5 12/22/2015 The 2 types of Placental Abruptions mass effect. Clinical Findings: Placental Abruption vaginal bleeding. Vaginal Bleeding Uterine tenderness Tetanic uterine contraction Rapid labor Fetal demise or distress Disseminated intravascular coagulation 31 Fresh Placental Abruption 32 Central Placental Abruption Hemorrhage Placenta 33 Placental Abruption: False Positives 34 Venous lake / gain increased Fibroids Marginal Veins Contractions Venous Lakes 35 36 6 12/22/2015 Marginal Veins 37 38 Scanning Planes of the Fetal Head Normal Fetal Anatomy & Measurements Sagittal Head, Neck Spine Abdominal/ Abdominal wall Urological, Genital Skeletal Cardio-thoracic 39 11.25 41 Coronal Axial 40 42 7 12/22/2015 Transventricular Choroid Plexus In lateral ventricle 43 44 Transcerebellar Transcerebellar Thalamus 3rd Vent Cerebellum Cisterna Magnum 45 46 Transcerebellar View Cavum Septum Pellucidi Transthalamic Cisterna Magna Cerebellar hemisphere 47 Head is ovoid in shape Symmetrical hemispheres Sharp edges ** 48 8 12/22/2015 Tilting transducer for head views Abdominal Views Abdominal section should be round Stomach bubble should be seen Umbilical portion of the PV should be seen and should be 1/3 of the distance to the center of the abdomen A cross-section of the fetal spine showing all three ossification centers should be seen 49 The Fetal Abdominal Circumference 50 The Fetal Abdominal 1 Stomach 2 Portal vein 3 Spine 4 Aorta 5 Abdominal muscles 6 Spleen 7 Liver 6 4 3 1 2 7 5 51 52 Normal or Abnormal? Why is the stomach so small? There is nothing to drink…oligohydramnios 53 54 9 12/22/2015 R 2 1 4 3 Subtle Tilting of the Transducer Abdomen 5 1. Umbilical vein 2. Liver 3. Stomach 4. Aorta / IVC 5. Spine L 55 56 Femur Epiphysis 57 58 Short Axis Long Axis 4 Chamber 4 Chamber Heart at 14 weeks 59 60 10 12/22/2015 Good view for Heart rate with M-Mode 11.5 61 62 Normal Position of the Fetal Heart Good 4 Chamber Views @ 27weeks 20 weeks 45 0 L Aorta LV RV LA RA R 63 64 What can be seen in this image? 65 66 11 12/22/2015 Rock, slide & drag to see kidneys free of shadow placenta umbilical cord aorta IVC stm amniotic fluid sp kidneys 67 68 69 70 Urinary Bladder - don’t confuse it with the stomach Fetal Spine Sagittal Plane Transverse Plane Coronal Plane Sagittal Coronal Umbilical Cord Insertion in Fetal Abdomen 71 Transverse 72 12 12/22/2015 Anterior This Sag view is of a fetus in Breech Position Posterior Ossification Center Caudal Cephalad Anterior Ossification Center 73 Sagittal image of fetal bladder, diaphragm & heart Fetus is in a vertex position. 74 What is the placental position? Diaphragm Biophysical Profile Image The “Take home Picture” Rule/ out: Bossing Macroglossia Micrognathia Nasal bridge Other 75 76 Cord Diaphragm 77 78 13 12/22/2015 ? 1 ? 2 3 Position? 4 Sag 79 80 ? Legs 81 Which one is normal? 83 Arm 82 Frontal Bossing 11.75 84 14 12/22/2015 Macroglossia? 85 86 Twins at 20 and 28 weeks ? ? Sag ML 28 weeks Normal? 87 Pseudo-previa 88 My Strangest Case: 8 years after delivery 89 90 15 12/22/2015 91 16 12/22/2015 Fetal Measurements Measurements Biparietal Diameter (BPD) Head Circumference (HC) Abdominal Circumference (AC) Femur Length (FL) G. W. Shepherd 1 2 Caliper Placement Markers for the BPD & HC + + + + 3 4 Finding the CSP 5 6 1 12/22/2015 Almost Coronal + 7 Head low in Pelvis 8 OFD 9 10 Dolichocephalic & Brachiocephalic Cephalic Index (CI) = BPD/OFD 11 Pair HC with BPD to compensate for shape 12 2 12/22/2015 Abdominal Circumference 13 14 15 16 Markers for AC Stomach Umbilical Vein Round 17 1.75 18 3 12/22/2015 19 20 21 22 Femur Length 23 24 4 12/22/2015 25 26 Curve is normal 27 28 Other Measurements Thoracic Circumference (TC/AC) Heart Circumference Renal Circumference & Diameter Foot Length Twins: Weight discordance Cord Doppler S/D 29 30 5 12/22/2015 Normal TC /AC 70% or Greater Cardiomegaly Short Rib Dysplasia HC/TC --- 1/3 -1/2 31 32 Renal Diameter Abdominal Diameter= 1/3 Foot = 0.9 – 1.1 Femur 33 Twins 34 Large for Dates 2.0 35 Normal Pregnancy / Wrong Dates Multiple Gestation Gestation with Mass / Masses Molar Pregnancy Polyhydramnios Gestational Diabetes 36 6 12/22/2015 Common Causes of Polyhydramnios High Beta HCG Levels Wrong Dates Multiple Gestation Molar Pregnancy Choriocarcinoma Gestational Diabetes Rh Incompatibility Anencephaly (50%) Esophageal Atresia (without TE Fistula) Duodenal/Small Bowel Atresia Non-immune Hydrops Neural Tube Defect (decreased swallowing) Multiple Gestation 37 38 Types of Twins Types of Twins Dichorionic/ Diamniotic (DC/DA) Divide before day 19 (morula divides) Monochorionic/ Diamniotic (MC/DA) Divide days 19-21 (early blastocyst divides) Monochorionic/ Monoamniotic (MC/MA) Divide days 21-28 (late blastocyst divides) Conjoined Twins: divides after day 28 (disc divides) Dizygotic: Fraternal Twins: Two ova were fertilized. This results in a dichorionic/ diamnionic pregnancy Monozygotic: Identical twins Result from the division of a single zygote. 39 40 Factors Influencing Frequency of Dizygotic Twins Frequency increases with age and parity Maternal history of twins increases frequency by 2-3X Termination of oral birth control pills increases frequency of twins Assisted reproduction: Increases frequency 41 42 7 12/22/2015 Chorionicity and Amnionicity: How do we tell the type of twins? Types of Twins: Distribution Determine the # of placentas: 2 placentas = DC/DA If there’s only one placenta: Is there a membrane? Thick membrane = DC/DA-fused placenta Thin membrane = MC/DA* No membrane = MC/MA* Look for “chorionic peak” Determine the sex, if different then it’s DC/DA Dizygotic (DZ): 70% of twins in USA (1% births Monozygotic (MZ): 30% of twins in the USA Monozygotic subtypes: DC/DA = 18-30% MZ DC/MA = 70% MZ MC/MA = 4% MZ twins 43 44 Twins: Two Placentas Amnion Chorion Monochorionic Placenta Dichorionic 45 46 Fused Placenta Di Di 47 48 8 12/22/2015 ? 49 50 Twins: One Placenta Di Di 51 52 Mono-Amniotic? Mono Di 2.25 53 54 9 12/22/2015 Mono Di 55 56 The difference in estimated fetal weights shouldn’t be more than 20% between Discordant Growth MC/DA Twins 57 Vanishing Twin 37mm 42mm 58 Monoamniotic Twins: Problems Cord Accidents Transfusions Conjoined Twins 59 Division after Disc is formed 60 10 12/22/2015 MC/MA Monoamniotic Twins A B = ACI’s Ability to change positions = cord entanglement 61 62 Monoamniotic Twins Monoamniotic Twins Single Yolk Sac Identify twins by placental cord insertions 63 Anomalies found in Monozygotic Twins Pre-membrane Fusion 64 Conjoined Twins (Disc divides) Conjoined Twins Neural tube defects Holoprosencephaly VACTERL association Heart defects Bladder extrophy Syrenomelia Gonadal dysgenesis 65 66 11 12/22/2015 Conjoined Twins Omphalopagus Twin to Twin Transfusion Thoracopagus 67 10 week Twins Discordant Growth 3D 69 68 Any Questions? 70 12 12/22/2015 Fluid Check Functions of Amniotic Fluid G. William Shepherd PhD, RDMS, RVT Cushion and protect embryo/fetus Allows symmetrical growth Allows motion for muscle & joint development Temperature stabilization 1 2 Production of AF: After 12 Weeks Functions of Amniotic Fluid Helps GI system development Helps the lungs to develop May play a role in the homeostasis of fetal electrolyte and fluid levels Fetal kidneys produce urine as early as 12 weeks. By 18 week > 50% of AF comes from fetal kidneys. At 25 weeks 100cc urine are produced each day. At term 600cc of urine are produced each day. 3 AF Consumption After 12 Weeks The fetus swallows AF. The swallowed AF is absorbed by the bowel. The fetal blood-stream transfers most of this fluid to the maternal blood-stream in the placenta. Metabolism produces fluid 5 4 Measurement of Amniotic Fluid Subjective method Deepest pocket method 4-quadrant AFI method 6 1 12/22/2015 Deepest Pocket Assessment of AF The entire uterus is examined and the deepest pocket located. The anterior to posterior measurement of the pocket is obtained. A value of < 2cm is considered to indicate a state of oligohydramnios. A value > 8cm is considered to indicate polyhydramnios. Advantages of the Deepest Pocket Method This method provides a quantitative result that can be used for comparisons to other scans. This is an easy technique to learn. This method can be used for assessing the AF volume in twin gestations. 7 Disadvantages of the Deepest Pocket Method A single measurement of a complex shape is not an accurate indicator of volume. The deepest pocket method fails to take gestational age into account. AF Volume 1st 2nd 3rd Gestational age 8 The 4-quadrant Amniotic Fluid Index This is the most widely used method for AF volume assessment. The deepest pocket in each quadrant of the uterus is measured in the AP dimension. The sum of these measurements is called the amniotic fluid index or AFI. The AFI values of thousands of normal gestations have been determined and have been correlated with gestational age. postdates 9 10 95th 50th RUQ LUQ RLQ LLQ 5th 16 20 11 24 28 32 Weeks Gestation 36 40 12 2 12/22/2015 Disadvantages of the 4-quadrant AFI Advantages of the 4-quadrant AFI The AFI is a reasonable assessment of AF volume. The AFI provides a basis for comparison to past or future exams. This is a relatively easy number to obtain. The AFI takes gestational age into consideration. There is a large body of data about this measurement and fetal well-being. 13 Pockets must be measured in an absolute AP direction, in a sagittal scanning plane The measurement must be made quickly before the position of the fetus changes. The AFI cannot be used for multiple gestations. Although the AFI is more accurate than the deepest pocket method, there is still some inaccuracy for this method. 14 A large curvolinear or linear transducer is a good choice 15 16 17 18 Small for Dates Normal pregnancy / wrong dates Blighted ovum Fetal demise Ectopic pregnancy IUGR Oligohydramnios 3 12/22/2015 19 20 21 22 Is this a good pocket? Large for Dates Normal pregnancy / wrong dates Multiple gestation Gestation with mass / masses Molar pregnancy Polyhydramnios Gestational diabetes 9.5cm 23 24 4 12/22/2015 Vernix in the fluid of 40 week gestation 25 Vernix 26 Vernix: Use of Gain 27 28 29 30 Vernix 5 12/22/2015 Hydrops ? 31 ? 32 Deepest Pocket Twins 33 34 Assessing Fetal Well-Being 3rd % 63-90mm 35 6 12/22/2015 Biophysical Profile (BPP) BPP: What is it? 30 minute test to evaluate fetal well-being There are 4 ultrasound parameters Amniotic fluid Gross fetal body motion (FM) Fetal tone Fetal breathing movement (FBM) A non-stress test (NST) is also included in a complete BPP The BPP is often used without the benefit of a NST 37 38 BPP: Why do we do it? BPP: Why do we do it? Hypertension Diabetes mellitus Multiple gestation Suspected IUGR or oligohydramnios Known placental or cord abnormality Failed NST Maternal heart or renal disease Previous unexplained fetal demise Hemoglobinopathy Postdated pregnancy Decrease in fetal motion Other…... 39 40 BPP: How do we score it? What Does the BPP Assess? The BPP assesses O2 delivery & adaptive behavior of the fetus If the fetus is functioning in a normal fashion, then systemic hypoxia is unlikely. The renal function is also assessed. Fluid changes occur over longer time periods (12-24 hours). 41 2 or 0 points are awarded for each parameter. If the fetus meets the criteria for the parameter, it is give 2 points. No partial scoring is done in the standard BPP Highest possible score is 10 42 7 12/22/2015 BPP: What are the parameters? NST Not Discussed Fluid Motion Breathing Tone 43 44 Older versions use 30 sec of resp & 2 episodes of gross motion Parameters: Fluid Causes of Oligohydramnios Fluid throughout the uterine cavity with the largest pocket of fluid equal or greater than 2 cm in AP Many hospitals will go beyond reporting a 2 or a 0 score for this parameter & additionally report the AFI along with the BPP score. Fluid is the most important parameter. It takes 12-24 hours for a significant change in fluid volume to take place Renal dysfunction (bilateral) Renal obstruction (bilateral) Renal agenesis (bilateral) Bladder outlet obstruction PROM Postdates pregnancy Hypoxia 45 46 Fetal Motion Parameters: Gross Fetal Motion 2 discrete (was 3) episodes of fetal motion Simultaneous motion of the trunk and a leg or the head and an arm etc. counts as one episode. Motions can include: twisting or flexion of the trunk or neck. Movement on the legs or arms and arching of the spine. This parameter tests neurological function. Is the cerebrum getting enough oxygen? 47 48 8 12/22/2015 Parameters: Fetal Breathing Parameters: Fetal Breathing Complex reflex, cerebellar and brainstem function 2 points are given if at least one episode of fetal breathing (duration of at least 20 sec.) occurs during the 30 minute exam. Fetal breathing is exhibited by diaphragm motion or motion of the kidneys, liver or expansion of rib spaces. Fetal breathing is rhythmic Fetal breathing is problematic it usually doesn’t occur during fetal sleep cycles. 49 50 Fetal Respiration 3.00 51 52 53 54 9 12/22/2015 Parameters: Fetal Tone Fetal tone is controlled by the cerebrum The opening of a hand and return to original position counts as one episode of tone Active flexion and extension of a limb. 55 Open 56 Closed The fetal hands are often near the face. Motion (clenching, arching) of the feet can be used for assessing tone 57 Fetal Tone 58 Duration of the BPP Manning has reported that in over 200,000 BPP tests, the average time was less than 8 minutes for normal results (8/8) Of course a score of <8 will take 30 min. 59 60 10 12/22/2015 55% 0/10 Value of the Biophysical Profile: Outcome Data 17% 11% 61 25% 2/10 4/10 62 Umbilical Artery Doppler as an Addition to Assessment of Fetal Well-Being 0/10 34w1d 8% 2/10 63 Umbilical Artery Doppler 64 S/D vs. Gestational Age 3.0@30w 2.5@35w 2.0@40w 11 12/22/2015 27w 31w Some nurse midwives find it useful to obtain a set of fetal measurements during the BPP for EFW Deteriorating Cord Doppler 1. S/D < 3.0 WNL for 27w 33w 35w 2. S/D > 4.5 Abn for 31w 3. No diastolic flow Abn 4. Rev diastolic Abn 68 Any Questions? 69 12