Document 14233617
advertisement

Journal of Medicine and Medical Sciences Vol. 2(3) pp. 722 –727 March 2011
Available online@http://www.interesjournals.org/JMMS
Copyright © 2011 International Research Journals
Full Length Research Paper
Symptomatic and Asymptomatic Neonatal Malaria in
Abuja
*Okechukwu AA, *Olateju K
*Department of Paediatrics, University of AbujaTeaching Hospital, Gwagwalada.
Accepted 14 March, 2011
Signs and symptoms of neonatal malaria does not differ much from those of neonatal sepsis, this has
resulted in non judicial use of anti malaria drugs in newborns suspected of having sepsis because of
the increasing reported cases of neonatal malaria in our environment. The study was aimed at
determining the prevalence of neonatal malaria among newborns admitted for suspected neonatal
sepsis, and to compare their malaria parasitic density with those of the apparently well neonate with a
view of ascertaining whether the symptoms from symptomatic newborn were truly as a result of malaria
parasitaemia. Blood culture and blood smear (thin and thick) were taken and made from neonates
suspected of having neonatal sepsis in the special care baby unit of the University of Abuja Teaching
Hospital from August 2007 to December 2009 (18 months study period). Thick and thin blood smear
were also taken from well neonates for comparative purposes. The smears were stained with Giemsa
and examined by light microscopy for asexual stages of plasmodium, specie identification, and
quantification. Of a total 266 neonates admitted for presumed sepsis, 150 were males and 116 females,
(m:f ratio of 1.3:1), and among the 272 well neonates recruited, 152 were male and 120 females, m:f ratio
of 1.3:1. Their mean age, body weight, and gestational age were 5.1±5.7 days, 2.5±0.87 kg, 36.1±3.5
weeks for neonatal sepsis babies, and 6.7±4.3 days, 3.1±0.35 kg, and 36.7±2.8 weeks for the well
neonates, p values >0.05. Malaria parasite was identified in 41.7% of babies with presumed sepsis, and
in 12.5% of well babies, p value <0.05. There was however no statistical significant difference in the
parasite density among the two groups, 84.7% Vs 88.2% for those with low parasite count, 12.6% Vs
11.8% for moderate parasite count, and 3.0% Vs 0.0% for high parasite count for babies admitted for
presume sepsis, and those from the well babies group, p values >0.05. Two deaths (1.8%) were
recorded among babies with malaria parasitaemia, one of whom had associated overwhelming sepsis,
and the other with high parasite count. Neonatal malaria is common in our environment. Greater
number however had low parasite count and had remained asymptomatic. Screening for malaria
parasite should be part of septic work up for babies suspected of having neonatal sepsis, but treatment
to be reserve to those with moderate to high malaria parasite count.
Keywords: Neonatal malaria, malaria parasite, malaria parasite count.
INTRODUCTION
Neonatal malaria (NM) defined as the presence of
malaria parasites (MP) in the peripheral blood smear of a
baby in the first month of life was taught to be rare
(Covell, 1950; Bruce-Chwatt, 1952). This was as a
resulted of the presence of feotal haemoglobin which
retards the growth of MP (Jellife, 1968), the role of
placenta in local antibody production (McGregor et al.,
1983), the protective effects of the transplacental
transferred maternal antibodies (McGregor, 1986), the
*Corresponding author Email: nebokest@yahoo.com
deficiency of para-aminobenzoic acid in breast milk
(McGregor et al., 1983; Mukhtar et al., 2006), the
immunological role of spleen (Marsh, 1993) and the
under reporting of the disease (Mukhtar, 2007).
However, there has been growing incidence of NM in
endemic areas with prevalence ranging from 0.3% to
46.7% (Orogade, 2004; Ekanem et al., 2008; Uneke,
2007; Obiajunwa et al., 2005). Reasons being due to:
possibility of increased resistance of plasmodium
falciparium (PF) to anti-malaria drugs resulting in
increase in maternal parasitaemia (Nahlen et al., 1998),
increased virulence from altered antigenic determinants
(White et al., 1998), antibody dependent cellular inhibition
Okechukwu and Olateju 723
of malaria parasite mediated via Fc gama RIIa (Kimberly
et al., 2004), mothers on regular malaria chemoprophylaxis having low malaria antibody titers and hence
transfer little protective antibody to their newborns (Ogala
et al., 1991), and most importantly increased reporting of
cases (Mukhtar, 2007).
Neonatal malaria has three types viz, congenital,
acquired, and transfusional. Congenital type is the
presence of MP in the peripheral blood smear of a new
born baby within the first seven days of life (McGregor et
al., 1983; Sodeinde et al., 1985), “acquired” results from
mosquito bite anytime after delivery when asexual
parasitaemia is detected within a minimum incubation
period of greater than one week, (Ibhanesebor, 1995),
and “transfusional” when malaria parasite is detected in
the peripheral blood of a neonate whose peripheral blood
film was negative prior to blood transfusion (Thapa et al.,
1987; Sodeinde et al., 1985). Congenital malaria (CM)
whose prevalence was put at 0–23% (Fischer, 1997; Uko
et al., 1999) results from MP crossing the placenta from
maternal blood to the fetal circulation. The exact
mechanism of this crossing is not known, but damage to
the syncytiotrophoblast occurring during active placental
infection has been suggested (Larkin et al., 1991;
Shulman et al., 2002). This type of malaria has been
shown to occur in children of clinically healthy mothers
who are delivered in malaria endemic areas (Larkin et al.,
1991). In babies of these women with high level of
immunity, CM is generally asymptomatic, majority of
parasite being rapidly cleared from the infant’s circulation
as a result of passive protection of the baby by maternal
antibody crossing the placenta, active immunity
developing from exposure to soluble malaria antigens in
uterus, and high proportion of fetal haemoglobin present
in the babies which retards the growth of the parasite
(Jellife, 1968), Shulman et al., 2002).
Neonatal sepsis (NS) defined as a clinical syndrome in
the presence of bacteraemia in a newborn in the first
month of life may be indistinguishable from NM
(Orogade, 2004; Ekanem et al., 2008; Ibhanesebor,
1995; Obiajunwa et al., 2005), and these has led to the
suggestion that screening for MP be included as part of
routine investigation in newborn infants with fever, as
(Nyirjesy et al., 1993) has reported increased risk of
perinatal deaths (RR=7.2), and low birth weight from CM.
Early workers have however found some primary attack
to be mild, in some instances being confined to a
transient asymptomatic parasitaemia (Thapa et al.,
1987). The mean incubation period of NM ranges from
1week to 8 weeks (Thapa et al., 1987), and the parasitic
density in babies with parasitaemia is generally low even
in those that develop clinical symptoms (Thapa et al.,
1987; Shulman et al., 2002). Plasmoduim falciparuim
(PF) is the predominant species causing malaria in
endemic area (White, 1998). It is responsible for over
90% of all cases of reported NM, however mixed infection
with plasmodium malaria has been reported (White,
1998), and plasmodium vivax is seen in most non
endemic areas. Ibhanesebor, 1995; Mukhtar et al., 2006;
Quinn et al.,1982). Over prescription of anti-malaria drugs
in neonatal period has been a common practice in some
centers in malaria endemic and mesoendemic areas
because of the increasing reported cases in the area.
This study is aimed at documenting the prevalence of NM
in neonates admitted into our neonatal ward for NS, and
compares their parasitic density with those of well
neonates from the child welfare, with a view of
ascertaining whether the symptoms from symptomatic
group were truly as a result of malaria parasitaemia. The
result from this finding, we believe will guide in
developing a definite policy on case management of NM
in our hospital, and other centers.
SUBJECTS AND METHODS
An 18 months prospective study was carried out at
University of Abuja Teaching Hospital (UATH) from
August 2007 to December 2009 for the above objectives.
All symptomatic neonates with features of NS and
admitted into the special care baby unit (SCBU) of the
hospital were part of the study. Also part of the study for
comparative purposes were well babies from the child
welfare clinic (CWC) of our health institution. Excluded
were neonates admitted into SCBU with other neonatal
conditions other than NS. Blood for culture, total white
blood cell count /differentials, and MP were collected
from all study patients. Blood for MP was also collected
from well neonates attending the CWC of the hospital.
Majority of the babies admitted into SCBU were referrals
from the neighbouring general, private, mission hospitals,
maternity homes, primary health centers and self
referrals from home. SCBU is a 32 bed capacity key
service ward in our health institution. It is an area where
newborns are promptly managed on 24 hour basis, and
represents a high volume, high stress service area of the
hospital. CWC is well baby’s clinic where infants and
young children receive their routine immunized according
to the national program on immunization, growth
monitoring and health talk on infant and young child
feeding is also carried out in the unit. It is opened to the
public on a daily basis from 8.00am to 4pm. UATH is a
350 bed capacity tertiary health institution located in the
Federal capital territory (FCT), Abuja in the north central
zone of the country. It is sub-serving many neighbouring
states including Nassarawa, Niger, Kogi, Benue, parts of
Kaduna state and FCT, Abuja.
The routine investigation done for neonates suspected
of having NS in the SCBU is a sepsis work-up, and total
full blood count (TFBC) with differentials. Blood for
culture was sent to the laboratory in 2 bottles, one
containing glucose broth and the other thio-glycolate
medium, and both incubated at 37°C for 48 hours.
Growth in either of the medium was sub-cultured on Mc-
724 J. Med. Med. Sci.
Conkey, blood or chocolate agar and further tested for
antibiotic sensitivity. However, if no growth was observed,
further incubation was done for another 48 hours. Other
culture investigations like cerebrospinal fluid, stool were
determined by clinical presentations of the patients.
Blood for MP was collected from recruited neonates
suspected of having NS in the SCBU, and those well
babies from the CWC. Thin and thick blood films were
prepared immediately upon collection of blood on
seperate slide. For thick films, 12 µl of blood was spread
over a diameter of 15 mm, while 2 µl of blood was used
for thin films. For the thick film, the smear was allowed to
air dry, dehaemoglobinized with buffered distilled water at
PH of 7.2. The thin film was fixed in absolute methanol
for 1-2 minute and air dried. Both thick and thin blood
films were stained after 24-48 hr with 3% Giemsa stain
solution at pH 7.2. For the thick film the dilution was in
the dilution of 1 volume of Giemsa to 9 volume of
buffered distilled water, while that of thin film is at 1:29 of
Giemsa and distilled water. The method adopted by
(Greenwood et al., 1991), and described by
(Cheesbrough, 2005) was used to determine MP density.
Between 10 and 15 fields were counted for each slide,
and results given per µl of blood. A definitive diagnosis of
malaria was made when a reddish chromatin dot with a
purple or blue cytoplasm of the MP are seen together. A
slide was pronounced negative when 100 high power
fields have been examined using ×100 oil immersion
objective lens without seeing either the reddish chromatin
dots or blue cytoplasm of MP. Malaria parasite density
was considered significant when MP count is greater than
1,000 parasites per µl of blood. Low parasite count was
when parasite count of 500 parasite/µ/ of blood and
below was obtained after the normal parasite count.
Moderate parasite count was parasite count of between
>500-<1,500 parasite/µl of blood, while high parasite
count was when parasite count was >1,500->3,000
parasite/µl. Other information collected from the patients
suspected of having NS included: age at onset of
symptoms (days), sex, birth weight (BW), presenting
problem and duration of such problem, gestational age
(GA), mother’s parity. Additional information obtained
from well babies in child welfare clinic includes age, sex,
gestational age at delivery, and body weight.
All
newborns admitted into SCBU for NS and found to have
moderate to high parasite count in their blood film were
treated for malaria with quinine syrup, while only those
found to have to moderate parasitaemia from the well
babies from CWC were treated with the same quinine
syrup. None had high parasite count. Those with low
parasite count among well babies, and had remained
asymptomatic were not treated.
Ethical approval was obtained from the Ethic
Committee of the hospital, as well as signed or thumb
printed informed written down consent from the mothers
of the subject after adequate explanation of the purpose
of the research in the language they understands best.
The research data was coded, privacy protected and
confidentiality maintained. Data analysis was conducted
using SPSS version 13.5. Tests for associations and
differences were done by chi-square analysis. Statistical
significance was set at p value < 0.05.
RESULTS
Of a total of 1,032 patients admitted into SCBU during the
study period, 266 (25.8%) were admitted for NS. There
were 150 were males and 116 females (ratio of 1.3:1).
The other 766 babies admitted were for other neonatal
conditions which includes: admission for observation,
HIV exposed babies for antiretroviral drugs prophylaxis,
low birth weight babies, small for gestational age, post
term deliveries, hypoglycemic babies, surgical conditions,
congenital abnormalities, birth asphyxia, neonatal
jaundice, etc. 272 well neonates were recruited from
CWC (152 males and 120 females, ratio of 1.3:1), table
1. The mean age, body weight (BW) and Gestational age
(GA) for babies suspected of having NS were 5.1±5.7
days, 2.5±0.87 kg, and 36.1±3.5 weeks, while those of
well babies from CWC were 6.7±4.3 days, 3.1±0.35 kg,
and 36.7±2.8 weeks, p values < 0.05.
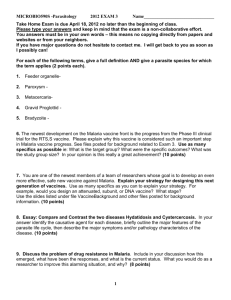
Table 2 shows MP density in the two groups.
Prevalence of NM among total admissions in SCBU was
10.8%. MP was positive in 41.7% of babies admitted for
NS, and 12.5% in the other group, p value <0.05. 58.3%
and 87.5% of on neonates in the two groups (NS and
those from CWC) had no MP in their blood stream, p
value also <0.05. While 68.8% of neonates with positive
MP among the NS group had CM, 45.2% of those from
the CWC also had CM. The mean MP count for babies
admitted for NS and those from the CWC did not differ
significantly, (682.79.±50.3 parasite/µl of blood with a
range of 500-3,000 parasite/µl) for NS group, and
(465.30±25.7 parasite/µl of blood and a range of 5001,500 parasite/µl) for the other group, p<0.05. The total
percentage among the two groups with low MP count did
not differ significantly, 84.9% Vs 88.2% for presume
sepsis babies and those from CWC, P>0.05, so also with
those with moderate parasitaemia, 15.3% Vs
11.8%,p>0.05.
DISCUSSION
This report from malaria mesoendemic area of north
central part of Nigeria documented prevalence on NM
among neonates admitted for suspected NS at 41.7%.
This was comparable to 35.0% reported by (Ekanem et
al., 2008) from Calabar on same group of babies
admitted for NS. The 10.8% prevalence of NM for overall
Okechukwu and Olateju 725
Table 1: Characteristics of Recruited Patients.
Neonatal Sepsis Babies
Total no
266 {150} [116]
Age (days)
5.1±5.7
Wt (kg)
2.5±0.87
Gestational age (wks) 36.1±3.5
Mother’s parity
2.3±1.5
SVD
190
C/S
76
Well Babies from CWC
272 {152} [120]
6.7±4.3
3.1±0.35
36.7±2.8
3.4±0.8
185
87
SVD: Spontaneous vertex delivery.
C/S: Caeserian section
CWC: Child welfare clinic
{}: Male
[]: Female
Table 2: Comparism of Malaria Parasite Density in Babies Admitted For Neonatal Sepsis and Well Babies
from Child Welfare Clinic.
Total
Total
Total
Total
Total
Total
NS Babies (%)
no of recruited patients
266
no with positive MP
111(41.7)
no with negative MP
155(58.3)
no with (500 parasites/ul) of MP
94(84.7)
no with (>500- <1,500 parasites/ul) of MP 14(12.6)
no with (>1,500- 3,000 parasites/ul) of MP 3(2.7)
CWC Babies(%)
272
34(12.5)
238(87.5)
30(88.2)
4(11.8)
0(0.0)
P value
>0.05
<0.05
<0.05
>0.05
>0.05
>0.05
MP:MP:Malaria
parasite.
Malaria parasite.
NS: Neonatal sepsis
CWC: Child welfare clinic
admissions in SCBU was also compared favourably to
the 5.1% by (Falade et al., 2007) in their multi centered in
Nigeria, and also similar to the 8.0% by (Ibhanesebor,
1995) from Benin, and 16.7% by (Kitua et al., 1990) from
Tanzania. Several reports have however reported high
prevalence of CM in malaria endemic area, ranging from
1.5% in Maputo Mozambique, by (Bergstrom et al., 1993)
to 28.2% from Jos by (Egwunyanga et al., 1995), and as
high as 46.7% from Ile-Ife by (Obiajunwa et al., 2005).
and 28.6% in the present study. All these support the
growing trend of neonatal/CM in hyperendemic malaria
area which was much earlier taught to be rare in the
region.
Congenital malaria may be symptomatic or
asymptomatic, and risk of symptomatic type is rare <1%
in babies born to women living in holoendemic conditions
(Shulman et al., 2002). In the majority of asymptomatic
cases, the parasites are rapidly cleared from the infant’s
blood from the reasons given previously (Shulman et al.,
2002). In the present study, 88.2% of well neonates from
the CWC with positive MP in their blood smear had low
MP count of 500 parasite/µ/l of blood, and had remained
asymptomatic. This supports the findings by (Falade et
al., 2007) who also noted that 62.1% of their smear
positive newborns in their multi center study had
remained asymptomatic. If we extrapolate this finding of
asymptomatic low parasitaemia of well babies from the
CWC to their counterpart in NS group who also recorded
84.9% of low malaria count among their smear positive
patients, one may suggest that only 15.1% of the NS
patients with significant malaria parasitaemia may have
had true symptoms of malaria, and 84.9% may be over
diagnosed. However because of high mortality and
morbidity associated with these two disease conditions
(NS and CM), and the great similarity in their clinical
presentation delayed treatment may worsen outcome,
and smear for MP should be part of septic work for
newborns with suspected NS so as to identify those with
significant malaria parasitaemia for anti malaria
treatment.
The clinical manifestation of congenital malaria
although occasionally seen within the first few hours of
birth are typically delayed until an infant is several weeks
of age (Marsh, 1993). The prolong interval between the
onset of clinical symptoms may be explained by the
present of protective transplacental acquired maternal
antimalaria antibody (Marsh, 1993; Mukhtar, 2007). It is
said that when such antibody is present in sufficient
concentration, as in infant born to an immune mother,
parasite replication may be prevented or attenuated
(Marsh, 1993). Preterm newborn babies who do not
benefit from such passive immunity may manifest clinical
726 J. Med. Med. Sci.
signs and symptoms earlier than the full term babies. In
the present study, 41.2% of babies with significant
malaria parasitaemia were preterm deliveries. Achidi et
al. (2005) made a similar observation in their study
population when they noted that neonates born with
malaria-positive placenta had a significantly higher
incidence of LBW. The higher malaria parasitaemia seen
in preterm deliveries may have been as a result of reason
stated above (inadequate transferred of passive
protective
maternal
transplcental
antimalaria
immunoglobulin). Similarly, primigravidae have also long
been noted to have increased susceptibility to malaria
than their multigravidae counterpart (Ekanem et al., 2008;
Uneke, 2007; Ibhanesebor, 1995; Obiajunwa et al., 2005;
Achidi et al., 2005). The apparent reason for this is poorly
understood, however, it has been found that when
compared with multigravidae, sera from multiparous
women have been found to inhibits the binding of MP to
chondroitin sulphate A, a ligandin present in a high
concentration on the surface of syncytiotrophoblast which
covers the placenta (Shulman et al., 2002), and possibly
explanation why multigravidae are less susceptible to
malaria infection than primigravidae.
CONCLUSION
Neonatal malaria is common in our environment. Greater
number however, had low parasite count and had
remained asymptomatic. Screening for MP should be part
of septic work up for babies suspected of having NS, but
treatment to be reserve to those with moderate to high
MP count.
REFERENCES
.Mukhtar MY, Lesi FEA, Iroha EU, Egri-okwaji MTC, Mafe AG (2006).
Congenital malaria among inborn babies at a tertiary centre in Lagos,
Nigeria. J. Trop. Paediatr. 52:19-23.
Achidi EA, Anchang JK, Jacob TM, Boyo MA, Mokube JA (2005). The
effect of maternal, umbilical cord and placental malaria parasitaemia
on the birthweight of newborns from South-western Cameroon. Acta
Pædiatrica. 94(7): 917–923.
Araoye MO (2004). Subject selection. In: Research methodology for
nd
health and social sciences. 2 eds Nathadex Publishers. 115-122.
Bergstrom S, Fernandes A, Schwaibach J, Perez O, Miyar R (1993) .
Materno-fetal transmission of pregnancy malaria: an immune
parasitologically study on 202 patients in Maputo. Gynecol. Obstet.
Invest. 35:103-107.
Bruce-Chwatt LJ (1952). Malaria in African infants and children in
southern Nigeria. Ann. Trop. Med. Parasitol. 46: 173-175.
Cheesbrough M (2005). District Laboratory Practice in Tropical
Countries.2nd Edition. Cambridge University Press,United Kingdom.
pp.244-251.
Covell G (1950). Congenital malaria. Trop. Dis. Bull. 47:1147-65.
Egwunyanga OA, Ajayi J, A.Oluyinka A, Popoola DD (1995).
Transplacental passage of Plasmodium faciparum and Sero
evaluation of Newborns in Northern Nigeria. J. Commun. Dis. 27:7783.
Ekanem AD, Anah MU, Udo JJ (2008). The prevalence of congenital
malaria among neonates with suspected sepsis in Calabar, Nigeria.
Trop. Doct. 38:73-76.
Falade C, Mokuolu O, Okafor H, Orogade A, Falade A, Adedoyin O
(2007). Epidemiology of congenital malaria in Nigeria: a multi-centre
study. Trop. Med. Int. Health. 12 (11): 1279 – 1287.
Fischer PR (1997). Congenital Malaria: an African survey. Clin. Pediatr.
(Phila), 36(7): 411-3.
Greenwood BM, Armstrong JRM (1991). Comparison of two single
methods for determining malaria parasite density. Transactions Royal
Society typical medicine and Hygiene. 85:186-188.
Ibhanesebor SE (1995). Clinical characteristics of neonatal malaria.
Trop. Paediatr. (16): 330-333.
Ibrahim M, Amuta SB, Ukokak S (1996). Incidence and causes of
neonatal mortality at UDUTH, Sokoto. Abstracts of Proceedings.
NJP.
Jellife EF (1968). Low birth weight and malaria infection of the placenta.
Bull World Health Org. 38:69-78.
Kimberly C, Brouwer A, Altaf A (2004). Plymorphism of Fc receptors IIa
for immunoglobulin G is associated with placental malaria in HIV-1positive women in western Kenya. J. Infect. Dis. 190:1192-8.
Kitua AY, Smith T, Aloko PL, Masanja KP (1990). Falciparum malaria in
the first year of life in an area of intense perennial transmission. Trop.
Med. Int. Health. 1: 475-484.
Larkin GL Thuma PE (1991). Congenital malaria in a hyperendemic
area. Am. J. Trop. Med. Hyg. 45 (5): 587-92.
Marsh K (1993). Immunogy of human malaria. In : Gilles HM and Warrel
th
DA (eds) 4 edition. Essentials malariology. London: Edward Arnold
(Publishers) Ltd. 60-77.
McGregor FA (1986). Congenitally acquired malaria. Postgrad Doctor
Afr. 8:52-54
McGregor FA, Wilson MME, Billewicz WZ (1983). Malaria infection of of
the placenta in the Gambia,West Africa. Its incidence and relationship
to still birth, birth weight and placental weight. Trans. R. Soc. Trop.
Med .Hyg. 77:232-44.
Mukhtar M (2007). The growing incidence of neonatal malaria- A
situational review in developing countries. Niger. J. Med. 16 (1): 2530.
Nahlen BI, Akintunde A, Alakija TI (1998). Lack of efficiency of
pyrimethamine prophlaxis in pregnant Nigerian women. Lancet. (ii):
830-834.
Nyirjesy P, Kasasiya T, Axelord P (1993). Malaria during pregnancy;
Neonatal morbidity and mortality and the efficacy of chloroquine
chemoprophylaxis. Clin. Infect. Dis.16 (1):127-32.
Obiajunwa PO, Owa JA, Adeodu O (2005). Prevalence of congenital
malaria in Ile-Ife, Nigeria. J. Trop. Paediatr. 51 (4):219-22.
Ogala WN, Azubuike JC, Nkangineme KEO (1991). Malaria. In
st
Paediatrics and child health in the tropical region 1 edition. Nigeria.
African Educational Services. 426-437.
Omokhodion SL, Adeyemo, AA, Akindele JA (1993). Neonatal
septicaemia in Ibadan: implications for neonatal care in developing
countries. Early Child Develop Care. 91:77-85.
Orogade AA (2004). Noenatal malaria in a mesoendemic malaria area
of Northern Nigeria. Ann. Afr. Med. 3(4):170-173.
Quinn TC, Richard FJ, Gregory JM(1982). Congenital malaria a report
of four cases and a review. J. Paediatr. 101 (2): 229-32.
Rienhardt MC, Ambroise–Thomas P, Cavallo–Serra R, Meylan C,
Gautier R (1978) Malaria at Delivery in Abidjan. Helvetica Paediatrica
Acta 33:65-84
Shulman C, Dorman E (2002). Clinical features of malaria in pregnancy.
th
In Warrell D.A, and Gilles H.M.(Ed), Essential Malariology, 4 ed.
London, BookPower formerly ELST, pg 223.
Sodeinde O, Dawodu AH (1985). Neaonatal transfusional malaria: A
growing clinical problem. Niger. J. Paediatr. 12:57-60.
Steketee RW, Wirima JJ, Bloland PB (1996a). Impairment of a
pregnant woman’s acquired ability to limit plasmodium falciparium by
infection with human immunodeficiency virus type-1. Am. J. Trop.
Med. Hyg. 55 (1):42-9.
Thapa BR, Narang A, Bhakoo ON (1987). Neonatal malaria: a clinical
study of neonatal and transfusional malaria. J. Trop. Paediatr. 33:
266-69.
Uko EK, Emeribe AO, Ejezie GC (1999). Maternal and Cord
Hemoglobin concentration in relation to malaria infection in Calabar.
Niger. J. Med. 8:27-29.
Uneke CJ (2007). Congenital Plasmodium falciparum malaria in sub-
Okechukwu and Olateju 727
Saharan Africa: a rarity or frequent occurrence? Parasitol. Res. 102(3):
333-342.
White NJ (1998). Malaria In : Cook GG (ed) Moanson’s Tropical
th
Diseases 20 edition. London. Edward Arnold. Pp. 1087-1164.