Outline Monte Carlo - II: Clinical impact Monte Carlo for
advertisement

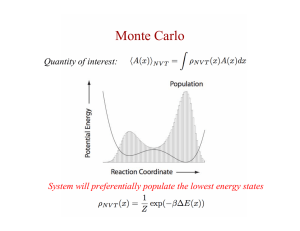
Monte Carlo - II: Clinical impact Monte Carlo for Electron Beam Treatment Planning C-M Charlie Ma, Ph.D. Dept. of Radiation Oncology Fox Chase Cancer Center Philadelphia, PA 19111 Why Use Monte Carlo for Radiotherapy Treatment Planning An accuracy of about 5% in dose delivery is required to effectively treat certain types of cancers and to reduce complications. ICRU Reports 24 (1976) and 42 (1988) Outline • Current status of electron Monte Carlo • Implementation of Monte Carlo for electron beam treatment planning dose calculations • Application of Monte Carlo in conventional and modulated electron beam therapy • Monte Carlo for other beam modalities The Accuracy Requirement for Treatment Planning Dose Calculation σ2=σ2calib+σ2dose+σ2setup+σ2motion +… and σ ≥ 2σdose=5% then σdose=2.5% Uncertainties in Electron Beam Dosimetry Limitations of dose calculation algorithms source models Fluence Profiles from an eMLC A B A B Beam modifier effect heterogeneous patient anatomy Limitations of dose measurement systems non-calibration conditions complex beam modifier geometry Jin et al (AAPM 2007) Pencil Beam Pinnacle3 Monte Carlo (BEAM) Achterberg et al (ESTRO 1999) Pencil Beam Pinnacle3 Monte Carlo (BEAM) Achterberg et al (ESTRO 1999) 20 MeV Beamlet Distributions Monte Carlo (MCDOSE) Pencil Beam (FOCUS) Monte Carlo Codes for Electron Beam Dose Calculations • The BEAMnrc/DOSXYZnrc system • Voxel Monte Carlo (VMC) • Macro Monte Carlo (MMC) • Superposition Monte Carlo • Other programs (ITS, MCNP, PENELOPE) • EGS4/MCRTP/MCDOSE/MCSIM Ma et al (PMB 2000) Commercial Implementation • Nucletron Oncentra MasterPlan (2001) – Implementation of Kawrakow’s VMC++ Monte Carlo dose calculation algorithm (2000) • Varian Eclipse eMC (2004) – Based on Neuenschwander’s MMC dose Timing – Nucletron Oncentra MasterPlan • • • • • 10x10 cm2 applicator 50k histories/cm2 Anatomy - 41 CT slices Pentium 4 Xenon 2.2 GHz Calculation time – 1.5 minutes for 6 MeV beam – 8.5 minutes for 20 MeV beam calculation algorithm (1992) Faster than pencil beam! Courtesy of Joanna Cygler Eclipse eMC no smoothing Implementation procedures Voxel size = 2 mm Air • Modeling of clinical electron beams Air 120 110 100 90 80 depth = 6.7 cm 70 60 50 depth = 7.7 cm 40 18 MeV depth = 4.7 cm 80 70 60 50 40 30 • Dose calculation, data processing and display 110 90 RelativeDose • CT data and beam setup conversion 120 depth= 4.7cm 18 MeV 100 Relative Dose • Commissioning of clinical electron beams 4.7 cm Bone Bone 20 Measured eMC 30 Measured eMC 20 10 10 0 0 -6 -4 -2 0 2 4 6 -6 Off-axisX position /cm -4 -2 0 2 4 Off-axisY position /cm Ding et al (PMB 2006) Effect of voxel size and smoothing MU real patient vs.water tank (MC / Water tank= 292 / 256=1.14) Air Air 2mmandnosmoothing 18 MeV 110 Relative Dose 100 90 80 70 2mmandwith3Dsmoothing 60 5 mm and with 3D smoothing 50 120 Relative Dose 120 110 4.7 cm Bone Bone 40 5 mm and with 3D smoothing 90 80 70 60 50 2 mm and with 3D smoothing 40 30 2mmandnosmoothing 18 MeV 100 30 depth = 4.9 cm 20 20 10 depth = 4.9 cm 10 0 0 -6 -4 -2 0 2 4 6 Off-axisX position /cm -6 -4 -2 0 2 4 6 Off-axisY position /cm Ding et al (PMB 2006) Courtesy of Joanna Cygler 6 MU real patient vs.water tank Internal mammary nodes (MC / Water tank= 210 / 206=1.019) Target 1,2 MC based MU Target 1,2 water tank based MU Lt eye water tank based Lt eye MC MU based MU Rt eye water tank based MU Rt eye MC based MU Courtesy of Joanna Cygler Monte Carlo for Mixed Beam Treatment for Breast Combined Photon/Electron Plan Based on MC • Conventional (46 Gy, 14 Gy boost) Photon beams to whole breast: 23 fractions, 2 Gy/fraction Electron boost to tumor bed: 7 fractions, 2 Gy/fraction • Hypofractionated (45 Gy, 56 Gy) IMRT to whole breast: 2.25 Gy x 20 fractions IMRT/MERT to tumor bed: 2.8 Gy x 20 fractions Courtesy of Jinsheng Li 58.0Gy 56.0Gy 47.3Gy 45.0Gy 42.8Gy 40.5Gy 36.0Gy 31.5Gy 22.5Gy 13.5Gy 4.5Gy Courtesy of Jinsheng Li Conclusions • Monte Carlo is a useful tool for radiotherapy treatment planning & dose verification • Monte Carlo has a more important role in electron dose calculation • High accuracy, high efficiency, low cost • More work is needed to make it clinically available