Clinical implementation and application of Monte Carlo methods calculation
advertisement

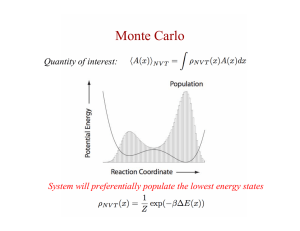
Clinical implementation and application of Monte Carlo methods in photon and electron dose calculation John DeMarco1 and Joanna E. Cygler2,3,4 1UCLA Radiation Oncology, David Geffen School of Medicine 2The Ottawa Hospital Cancer Centre, Ottawa, Canada 3Carleton University Dept. of Physics, Ottawa, Canada 4University of Ottawa, Dept. of Radiology. Ottawa, Canada The Ottawa L’Hopital Hospital d’Ottawa Regional Cancer Centre Part I: Photon beams John DeMarco, Ph.D. UCLA Department of Radiation Oncology David Geffen School of Medicine Los Angeles, CA Outline 1. Educational review of the physics of the MC method. 2. Factors associated with vendor implementation of the MC dose calculation, such as statistical uncertainties, spatial resolution, variance reduction, CT-number to material density assignments, and reporting of dose-to-medium versus dose-to-water. 3. Review the vendor transport codes currently used for clinical treatment planning. 4. Experimental verification of Photon based MC algorithms. 5. Potential clinical implications of Photon based MC calculated dose distributions. General Purpose Monte Carlo Codes Monte Carlo Codes Optimized for Treatment Planning Peregrine (Hartmann-Siantar et. al. 2002) DPM (Sempau et. al. 2000) MCDose (Ma et. al. 2002) VMC/XVMC (Kawrakov and Fippel) Commercial implementations CMS Monaco Brainlab iPlan I. Kawrakow, M. Fippel, and K. Friedrich, ‘‘3D electron dose calculation using a Voxel based Monte Carlo algorithm (VMC),’’ Med. Phys. 23, 445–457 (1996). M. Fippel, “Fast Monte Carlo dose calculation for photon beams based on the VMC electron algorithm”, Med. Phys., 26, 1466-1475 (1999). Accuray Multiplan C-M Ma, J S Li, T Pawlicki, S B Jiang, J Deng, M C Lee,T Koumrian, M Luxton and S Brain, “A Monte Carlo dose calculation tool for radiotherapy treatment planning” Phys. Med. Biol. 47 (2002) 1671–1689. Ma C-M, Li JS, Deng J, Fan J. “Implementation of Monte Carlo dose calculation for CyberKnife treatment planning. J Phys Conf Ser 2008;102 Spatial resolution Statistical uncertainty Material Conversion MLC Modeling iPlan/Brainlab Linear Accelerator Source Modeling Phase-space Virtual source Virtual Energy Fluence Model Complete Simulation (target to patient) Chetty et. al. “Report of the AAPM Task Group No. 105: Issues associated with clinical implementation of Monte Carlo-based photon and electron external beam treatment planning”, Med. Phys. 34, 4818-4853 (2007). Virtual Energy Fluence Model • Primary photon source and multiple scatter photon sources defined as two-dimensional Gaussian shapes • Electron contamination source • Photon energy spectrum derived based upon measured depth dose curves in water M. Fippel, F. Haryanto, O. Dohm, F. Nusslin, and S. Kriesen, “A virtual photon energy fluence model for Monte Carlo dose calculation”, Med. Phys. 30, 301-311, (2003). Photon Transport Collide or Cross? Region 1 • Energy (E) v • Direction u = (u, v, w) = (cos θ x , cos θ y , cos θ z ) • Position L v x = (xo , yo , zo ) x= − ln (ξ ) μ Region 2 Sampling for the photon collision type 0.000 Coherent 0.107 Incoherent Random Number = 0.532 0.788 1.000 PhotoElectric Update Photon Direction φ θ (u,v,w) u = cosθx = sinθ cosφ y = cosθ y = sinθ sinφ z = cosθz = cosθ (0,0,1) Particle start CT Voxel Array The transport process is repeated across each voxel of a 3D rectilinear array (based upon the simulation CT scan). Appropriate routines for scoring the energy deposition from secondary electrons. Particle end Appropriate routines to convert from HU to mass density and material composition on a voxel by voxel basis. Accuracy vs. Precision 1 x = ∑xi n i=1 N sx sr = x ⎡ ∑ xi2 1 ⎤ − ⎥ sr ≈ ⎢ 2 ⎢⎣ (∑ xi ) n ⎥⎦ Reproduced from the MCNP users manual Simulation Efficiency and Variance Reduction 1 ε= 2 sT I. Kawrakow and M. Fippel, “Investigation of variance reduction techniques for Monte Carlo photon dose calculation using XVMC”. Phys. Med. Biol. 45 (2000) 2163–2183. • “Variance reduction” techniques seek to increase the efficiency of the simulation by • ray-tracing • photon splitting • electron history repetition • electron and photon cut-off energies Particle start Primary photon collision points Initial ray-tracing can be used to pre-calculate the collision number within a voxel for incoming primary photons. Particle end Spatial resolution Statistical uncertainty Material Conversion MLC Modeling iPlan/Brainlab Monte Carlo calculation time as a function of the axial plane voxel size (iPlan/Brainlab Monte Carlo implementation) 7-Field IMRT plan RPC Lung & Spine phantom Mean variance = 2% Dose-to-medium Monte Carlo calculation time as a function of the variance setting (iPlan/Brainlab Monte Carlo implementation) 7-Field IMRT plan RPC Lung & Spine phantom Voxel resolution = 3 mm Dose-to-medium Variance Setting and the Qualitative Assessment of the Absorbed Dose Distribution 5% 2% 7-Field IMRT plan RPC Lung & Spine phantom Voxel resolution = 3 mm Dose-to-medium 1% Mean Variance = 5% Mean Variance = 1% 7-Field IMRT plan RPC Lung & Spine phantom Voxel resolution = 3 mm Dose-to-medium Mean Variance = 5% Mean Variance = 1% 7-Field IMRT plan RPC Lung & Spine phantom Voxel resolution = 3 mm Dose-to-medium Dosew vs. Dosemed J. V. Siebers, P. J. Keall, A. E. Nahum, and R. Mohan, “Converting absorbed dose to medium to absorbed dose to water for Monte Carlo based photon beam dose calculations,” Phys. Med. Biol. 45, 983–995 2000. 7-Field IMRT plan RPC Lung & Spine phantom Dmed Dw Clinical Planning Comparison medium vs. water (γ-setting 3%/3mm) Dosimetric Validation Chetty et. al. “Report of the AAPM Task Group No. 105: Issues associated with clinical implementation of Monte Carlo-based photon and electron external beam treatment planning”, Med. Phys. 34, 4818-4853 (2007). “Experimental verification of a MC algorithm should include testing to assess the accuracy of: (a) the beam model be it measurement-driven or based on treatment head simulation and (b) the radiation transport algorithm in homogeneous and heterogeneous phantoms. The former is part of routine commissioning of dose calculation algorithms, whereas the latter is likely to have significantly more involvement from developers and vendors.” • Beam Model • Multileaf collimator and other beam modifying devices • Output factors and the normalization condition for conversion to absolute dose B. Fraass, K. Doppke, M. Hunt, G. Kutcher, G. Starkschall, R. Stern, and J. Van Dyke, “American Association of Physicists in Medicine Radiation Therapy Committee Task Group 53: Quality assurance for clinical radiotherapy treatment planning,” Med. Phys. 25, 1773–1829 1998. IAEA-Technical Report Series No. 430: Commissioning and quality assurance of computerized planning systems for radiation treatment of cancer,” in International Atomic Energy Agency, Vienna, 2004 Dosimetric Validation CMS Monaco Grofsmid et al. “Dosimetric validation of a commercial Monte Carlo based IMRT planning system”, Med. Phys. 37, 540-549, (2010). Dosimetric Validation CMS Monaco Grofsmid et al. “Dosimetric validation of a commercial Monte Carlo based IMRT planning system”, Med. Phys. 37, 540-549, (2010). Dosimetric Validation CMS Monaco Grofsmid et al. “Dosimetric validation of a commercial Monte Carlo based IMRT planning system”, Med. Phys. 37, 540-549, (2010). Retrospective Comparison Accuray Multiplan 2.1.0 Sharma et al. “Clinical implications of adopting Monte Carlo treatment planning for Cyberknife”, JACMP, 11, (170-175), 2010. 8-Field IMRT plan 3 x 18 = 54 Gy Clinical Planning Comparison Pencil beam algorithm versus Monte Carlo 2.5x2.5x1.5 mm3 Monte Carlo Variance setting = 1% Dose to Medium The Monte Carlo recalculated plan predicts a lower dose (3%-8%) across the axial slice of the PTV Monte Carlo Pencil beam Clinical Implications for Monte Carlo based Photon Treatment Planning N. van der Voort et al., “Clinical introduction of Monte Carlo treatment planning: A different prescription dose for non-small cell lung cancer according to tumor location and size”, Radiotherapy and Oncology 96 (2010) 55–60. • Comparison of conventional treatment planning algorithms vs. Monte Carlo • Modification of prescription dose based upon Monte Carlo recalculation Clinical Implications for Monte Carlo based Photon Treatment Planning A. Fogliata, E. Vanetti, D. Albers, C. Brink, A. Clivio, T. Knoos, G. Nicolini, and L. Cozzi, “On the dosimetric behaviour of photon dose calculation algorithms in the presence of simple geometric heterogeneities: comparison with Monte Carlo calculations” Phys. Med. Biol. 52 (2007) 1363–1385. Photon energy, field size, and the heterogeneous nature of the treatment area will determine the dosimetric impact of a Monte Carlo treatment planning algorithm. Part II: Electron beams Joanna E. Cygler, Ph.D., FCCPM, FAAPM The Ottawa Hospital Cancer Centre, Ottawa, Canada Carleton University Dept. of Physics, Ottawa, Canada University of Ottawa, Dept. of Radiology, Ottawa, Canada Outline • Rationale for MC dose calculations for electron beams • Commercially available Monte Carlo based electron treatment planning systems • Clinical implementation of MC-based TPS • Issues to pay attention to when using MC based system • Timing comparisons of major vendor MC codes in the clinical setting. Rationale for Monte Carlo dose calculation for electron beams • Difficulties of commercial pencil beam based algorithms – Monitor unit calculations for arbitrary SSD values – large errors* – Dose distribution in inhomogeneous media has large errors for complex geometries * can be circumvented by entering separate virtual machines for each SSD – labour consuming Rationale for Monte Carlo dose calculation for electron beams 6.2 cm 15 Relative Dose 9 MeV 10 Measured Pencil beam Monte Carlo depth = 6.2 cm depth = 7 cm 5 0 -10 /tex/E TP /abs/X TS K 09S .OR G -5 0 Horizontal Position /cm 5 10 98-10-21 Ding, G. X., et al, Int. J. Rad. Onc. Biol Phys. (2005) 63:622-633 Commercial implementations • MDS Nordion (now Nucletron) 2001 - First commercial Monte Carlo treatment planning for electron beams – Kawrakow’s VMC++ Monte Carlo dose calculation algorithm (2000) – Handles electron beams from all clinical linacs • Varian Eclipse eMC 2004 – Neuenschwander’s MMC dose calculation algorithm (1992) – Handles electron beams from Varian linacs only (23EX) – work in progress to include linacs from other vendors • CMS XiO eMC for electron beams 2010 – Based on XVMC (Kawrakow, Fippel, Friedrich, 1996) – Handles electron beams from all clinical linacs Nucletron Electron Monte Carlo Dose Calculation Module •Originally released as part of Theraplan Plus •Currently sold as part of Oncentra Master Plan •Fixed applicator with optional, arbitrary inserts, or variable size fields defined by the applicator like DEVA •Calculates absolute dose per monitor unit (Gy/MU) •User can change the number of particle histories used in calculation (in terms of particle #/cm2) •Data base of 22 materials 510(k) clearance (June 2002) •Dose-to-water is calculated in Oncentra •Dose-to-water or dose-to-medium can be calculated in Theraplan Plus MC DCM •Nucletron performs beam modeling Varian Macro Monte Carlo transport model in Eclipse • An implementation of Local-to-Global (LTG) Monte Carlo: – Local: Conventional MC simulations of electron transport performed in well defined local geometries (“kugels” or spheres). • Monte Carlo with EGSnrc Code System - PDF for “kugels” • 5 sphere sizes (0.5-3.0 mm) • 5 materials (air, lung, water, Lucite and solid bone) • 30 incident energy values (0.2-25 MeV) • PDF table look-up for “kugels” This step is performed off-line. – Global: Particle transport through patient modeled as a series of macroscopic steps, each consisting of one local geometry (“kugel”) C. Zankowski et al “Fast Electron Monte Carlo for Eclipse” Varian Macro Monte Carlo transport model in Eclipse • Global geometry calculations – CT images are pre-processed to user defined calculation grid – HU in CT image are converted to mass density – The maximum sphere radius and material at the center of each voxel is determined • Homogenous areas → large spheres • In/near heterogeneous areas → small spheres C. Zankowski et al “Fast Electron Monte Carlo for Eclipse” Varian Eclipse Monte Carlo • User can control – Total number of particles per simulation – Required statistical uncertainty – Random number generator seed – Calculation voxel size – Isodose smoothing on / off • Methods: 2-D Median, 3-D Gaussian • Levels: Low, Medium, Strong • Dose-to-medium is calculated CMS XiO Monte Carlo system • XiO eMC module is based on VMC* – simulates electron (or photon) transport through voxelized media • The beam model and electron air scatter functions were developed by CMS • The user can specify – – – – – – the number of histories voxel size dose-to-medium or dose-to-water random seed the total number of particle histories or the goal Mean Relative Statistical Uncertainty (MRSU) • CMS performs the beam modeling *Kawrakow, Fippel, Friedrich, Med. Phys. 23 (1996) 445-457 *Fippel, Med. Phys. 26 (1999) 1466–1475 User input data for MC based TPS Treatment unit specifications: • Position and thickness of jaw collimators and MLC • For each applicator scraper layer: Thickness Position Shape (perimeter and edge) Composition • For inserts: Thickness Shape Composition No head geometry details required for Eclipse, since at this time it only works for Varian linac configuration User input data for MC TPS cont Dosimetric data for beam characterization, as specified in User Manual • Beam profiles without applicators: -in-air profiles for various field sizes –in-water profiles –central axis depth dose for various field sizes –some lateral profiles • Beam profiles with applicators: – Central axis depth dose and profiles in water – Absolute dose at the calibration point Dosimetric data for verification – Central axis depth doses and profiles for various field sizes Clinical implementation of MC treatment planning software • Beam data acquisition and fitting • Software commissioning tests* • Clinical implementation – procedures for clinical use – possible restrictions – staff training *should include tests specific to Monte Carlo A physicist responsible for TPS implementation should have a thorough understanding of how the system works. Software commissioning tests: goals • Setting user control parameters in the TPS to achieve optimum results (acceptable statistical noise, accuracy vs. speed of calculations) – Number of histories – Voxel size – Smoothing • Understand differences between water tank and real patient anatomy based monitor unit values Software commissioning tests • Criteria for acceptability – Van Dyk et al, Int. J. Rad. Oncol. Biol. Phys., 26, 261-273,1993; – Fraass, et al, AAPM TG 53: Quality assurance for clinical radiotherapy treatment planning,” Med. Phys. 25, 1773–1829 1998 • Homogeneous water phantom • Inhomogeneous phantoms (1D, 2D, 3D, complex) – Cygler et al, Phys. Med. Biol., 32, 1073, 1987 – Ding G.X.et al, Med. Phys., 26, 2571-2580, 1999 – Shiu et al, Med.Phys. 19, 623—36, 1992; – Boyd et al, Med. Phys., 28, 950-8, 2001 • Measurements, especially in heterogeneous phantoms, should done with a high (1 mm) resolution Lateral profiles at various depths, SSD=100cm, Nucletron TPS 20 MeV, 10x10cm2 applicator, SSD=100cm. Homogeneous water phantom. Cross-plane profiles at various depths. MC with 10k and 50k/cm2. 110 110 100 100 90 90 80 80 70 meas.@2cm 60 calc.@2cm 50 meas.@3.0cm calc.@3.0cm 40 meas.@d=3cm calc.@d=3cm calc.@d=3cm,50k meas.@d=7.8cm calc.@d=7.8cm 70 Dose / cGy Dose / cGy 9 MeV, 10x10cm2 applicator, SSD=100cm. Homogeneous water phantom,cross-plane profiles at various depths. MC with 10k/cm2. 60 50 calc.@d=7.8cm,50k meas.@d=9cm calc.@d=9cm calc.@d=9cm,50k 40 meas.@4.0cm 30 30 calc.@4.0cm 20 20 10 10 0 0 -10 -5 0 Off - axis / cm 5 10 -10 -5 0 Off - axis / cm 5 10 CMS: Cut-out factors Cutout Output Factors: 17 MeV Cutout Output Factors: 9 MeV 1.050 1.050 O u tp u t F a c to r (c G y /M U ) SSD=100 cm O u tp u t F a c to r (c G y /M U ) 1.000 0.950 0.950 0.850 SSD=100 cm 0.900 0.750 0.850 0.800 0.650 SSD=115 cm 0.750 0.550 0.700 Experimental XiO Calculated 0.450 SSD=115 cm 0.650 Experimental XiO Calculated 0.600 0.350 1 2 3 4 5 6 Square Cutout Length (cm) 7 8 9 1 2 3 4 5 6 7 8 Square Cutout Length (cm) Vandervoort and Cygler, COMP 56th Annual Scientific Meeting, Ottawa June 2010 9 Eclipse eMC no smoothing Voxel size = 2 mm Air Air Bone Bone 120 110 120 depth = 4.7 cm 18 MeV 110 100 90 90 Relative Dose 100 Relative Dose 4.7 cm 80 depth = 6.7 cm 70 60 50 depth = 7.7 cm 40 18 MeV depth = 4.7 cm 80 70 60 50 40 30 20 Measured eMC 30 Measured eMC 20 10 10 0 0 -6 -4 -2 0 2 Off-axis X position /cm 4 6 -6 -4 -2 0 2 Off-axis Y position /cm Ding, G X., et al (2006). Phys. Med. Biol. 51 (2006) 2781-2799. 4 6 Eclipse eMC Effect of voxel size and smoothing Air Air Bone Bone 110 2 mmand no smoothing 18 MeV 110 Relative Dose 100 90 80 70 2 mmand with 3D smoothing 60 5 mm and with 3D smoothing 50 120 Relative Dose 120 4.7 cm 90 80 70 60 50 40 30 30 depth = 4.9 cm 5 mm and with 3D smoothing 100 40 20 2 mm and with 3D smoothing 20 10 depth = 4.9 cm 10 0 2 mmand no smoothing 18 MeV 0 -6 -4 -2 0 Off-axis X position /cm 2 4 6 -6 -4 -2 0 2 Off-axis Y position /cm Ding, G X., et al (2006). Phys. Med. Biol. 51 (2006) 2781-2799. 4 6 CMS: 9 MeV - Trachea and spine Air Bone Bone Air Bone Bone Film Film Vandervoort and Cygler, COMP 56th Annual Scientific Meeting, Ottawa June 2010 Dose-to-water vs. dose-to-medium Hard bone cylinder 2cm 1 cm diameter and 1 cm length 1100 Small volume of water Bone cylinder is replaced by water-like medium but with bone density 100 90 BEAM/dosxyz simulation 80 70 Dose Dm - energy absorbed in a medium voxel divided by the mass of the medium element. 60 50 Bone cylinder location 40 30 20 10 Voxel of medium Dw - energy absorbed in a small cavity of water divided by the mass of that cavity. 0 0 3 4 5 1.14 9 MeV SPR ⎛S⎞ Dw = Dm ⎜ ⎟ ⎝ ρ ⎠m 2 Central Axis Depth /cm 1.13 w 1 1.12 Water/Bone stopping-power ratios 1.11 1.10 0 Ding, G X., et al Phys. Med. Biol. 51 (2006) 2781-2799. 1 2 3 depth in water /cm 4 5 Good clinical practice • Murphy’s Law of computer software (including Monte Carlo) “All software contains at least one bug” • Independent checks MU MC vs. hand calculations Monte Carlo Hand Calculations Real physical dose calculated on a patient anatomy Rectangular water tank Inhomogeneity correction included No inhomogeneity correction Arbitrary beam angle Perpendicular beam incidence only 9 MeV, full scatter phantom (water tank) RDR=1 cGy/MU Lateral scatter missing Real contour / Water tank = =234MU / 200MU=1.17 MU real patient vs.water tank MC / Water tank= 292 / 256=1.14 MU-real patient vs. water tank Impact on DVH 120 PTV-MU-MC 100 PTV-MU-WT %volume 80 LT eye-MU-MC LT eye-MU-WT 60 RT eye-MU-MC 40 RT eye-MU-WT 20 0 0.0 10.0 20.0 30.0 dose / Gy 40.0 50.0 60.0 Posterior cervical lymph node irradiation - impact on DVH 45.0 customized 40.0 35.0 30.0 PTV / cm 3 conventional 25.0 20.0 15.0 10.0 Jankowska et al, Radiotherapy & Oncology, 2007 5.0 0.0 0.0 5.0 10.0 15.0 dose / Gy 20.0 25.0 30.0 Internal mammary nodes MC / Water tank= 210 / 206=1.019 Timing – Pinnacle3 dual processor 1.6 GHz Sun workstation, 16 GB RAM. Overall uncertainty 2% 1% 0.5% Patient # histories CPU time (min) # histories CPU time (min) # histories CPU time (h) 1(cheek) 3.4x106 4.8 1.4x107 20 1.6x108 3.9 2 (ear) 1.7x106 2.1 6.5x106 8.1 7.1x107 1.5 3 (breast) 3.3x106 7.1 1.4x107 29.9 1.5x108 5.4 4 (face) 1.1x107 32.1 4.7x108 134.5 5.2x108 24.5 Fragoso et al.: Med. Phys. 35, 1028-1038, 2008 Timing – Nucletron TPS Oncentra 4.0 Anatomy - 201 CT slices Voxels 3 mm3 10x10 cm2 applicator 50k histories/cm2 4 MeV Timer Results: Init = 0.321443 seconds Calc = 42.188 seconds Fini = 0.00158201 seconds Sum = 42.5111 seconds 20 MeV Timer Results: Init = 0.311014 seconds Calc = 110.492 seconds Fini = 0.00122603 seconds Sum = 110.805 seconds Faster than pencil beam! Timing – Varian Eclipse Eclipse MMC, Varian single CPU Pentium IV XEON, 2.4 GHz 10x10 cm2, applicator, water phantom, cubic voxels of 5.0 mm sides 6, 12, 18 MeV electrons, 3, 4, 4 minutes, respectively Chetty et al.: AAPM Task Group Report No. 105: Monte Carlobased treatment planning, Med. Phys. 34, 4818-4853, 2007 Conclusions • Commercial MC based TP system are available – fairly easy to implement and use – MC specific testing required • Fast and accurate 3-D dose calculations • Single virtual machine for all SSDs • Large impact on clinical practice – Accuracy improved – More attention to technical issues needed – Dose-to-medium calculated – MU based on real patient anatomy (including contour irregularities and tissue heterogeneities) • Requirement for well educated physics staff Acknowledgements George X. Ding George Daskalov Gordon Chan Robert Zohr Ekaterina Tchistiakova Indrin Chetty Margarida Fragoso Charlie Ma Eric Vandervoort David W.O. Rogers In the past I have received research support from Nucletron and Varian TOHCC has a research agreement with Elekta Thank You