Developing a Rationale for Tolerance Values and Action Levels for the Performance of External Beam Planning and Delivery Systems
advertisement
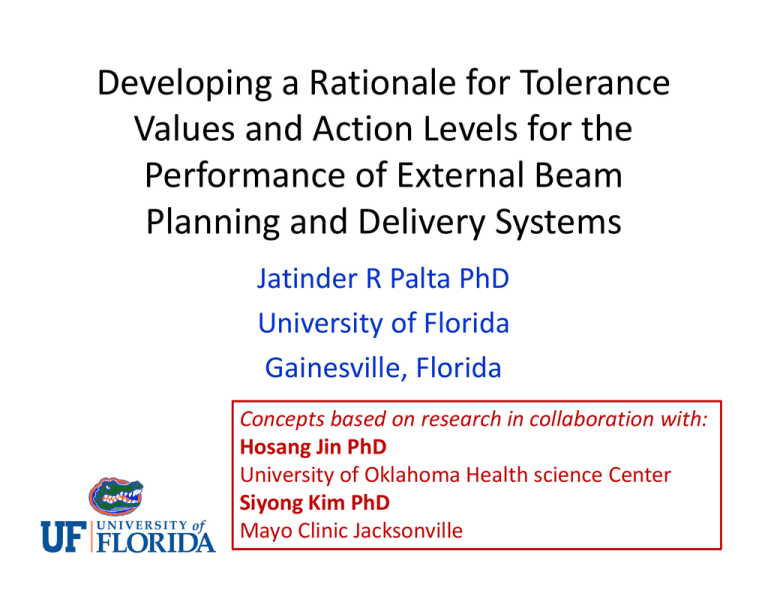
Developing a Rationale for Tolerance Values and Action Levels for the Performance of External Beam Planning and Delivery Systems Jatinder R Palta PhD University of Florida Gainesville, Florida Concepts based on research in collaboration with: Hosang Jin PhD University of Oklahoma Health science Center Siyong Kim PhD Mayo Clinic Jacksonville Disclosure • Co‐ Director of the 2011 AAPM summer school – Which gave me the prerogative of selecting the topic of talk • I have a strong bias towards the belief that “WYSINWYG®”, in the era of conformal radiotherapy (IMRT, IGRT, ART, etc…) ® Modified from the acronym WYSIWYG, used by R Mohan during 2007 AAPM Annual Meeting Objectives The objective of this and the presentation to follow is to suggest simple strategies that may potentially change “WYSINWYG” to “WYSWYG” AAPM REPORT No. 142 QUALITY ASSURANCE OF MEDICAL ACCELERATORS What is a “Baseline”? Klein et. al., Med. Phys.,(36) 2009 BASELINE (As defined by TG 142 Report) “Values of equipment parameters acquired at the time of acceptance testing and commissioning.” – Periodic test Tables (Daily, Monthly, and Annual) recommend these as tolerance values for each parameter. – Tolerance values are technique dependent (e.g. Non‐ IMRT, IMRT, SRS/SBRT) Limitations of this approach: •It does not say anything about the precision and accuracy of treatment planning and delivery •Because precision and accuracy is highly correlated to the complexity of planning and delivery Patient‐Specific IMRT QA Criteria of acceptability: 3%; 3mm DTA Lung (68) Prostate (155) Brain (55) Spine (65) H&N (437) Pelvis(24) Lower pass rate highly correlated to the complexity of the treatment plan Data from University of Florida QA Outliers 600 500 Number of meas. = 2679 Mean = 0,995 SD = 0,025 Fréquence 400 300 200 100 1, 13 1, 11 1, 09 1, 07 1, 05 1, 03 1, 01 0, 99 0, 97 0, 95 0, 93 0, 91 0, 89 0, 87 0 Dm/Dc 12 Centres‐ 118 patients Eleven patients are outside 4σ……….. M. Tomsej et al. Cancer/Radiothérapie, 8, 2004 RPC Credentialing: IMRT RPC criteria of acceptability: 7% for Planning Target Volume 4 mm DTA for the Organ‐at‐Risk Cord TLD Target 250 irradiations of H&N phantom 28% had failed … Anterior Posterior Profile Anterior Posterior 8 Dose (Gy) 6 4 2 Organ at Risk Primary PTV 0 -4 -3 -2 -1 0 1 Distance (cm) RPC Film Institution Values 2 3 4 What could be the reason??? It could be delivery error Mechanical Errors? MLC Leaf Positioning Fluence and Timing? Orchestration of MLC and Fluence It could be dosimetry artifacts Some measurement Problem? It could be algorithmic errors Source Model, Penumbra, MLC Modeling More than likely a conspiracy of effects, each with it own uncertainty……. SMLC IMRT Fields in the static MLC IMRT consists of a number of sub‐fields or beam segments. The overall uncertainty in an intensity‐modulated (IM) field arises from a complex interplay of uncertainties associated with each sub‐field. AAPM REPORT No. 13 PHSICAL ASPECTS OF QUALITY ASSURANCE IN RADIATION THERAPY “QA documents specify acceptable tolerance levels for individual parameters WITHOUT considering the cumulative effect on the uncertainty in the dose delivered to a specified volume in a patient.” – The reason is that uncertainty propagation is difficult and considered by some to be scientifically unsound because we are dealing with the combined effect of systematic (non‐random) and random uncertainties AAPM Publication, 1984 Dosimetric Uncertainties (95% confidence level) Combined incertainty in dose to a patient (5%) Cumulative uncertainty in dose delivered to a tissue‐phantom (2.5%) Effect on dose computation of tumor localization and contour delineation (2%; 5 mm accuracy) Uncertainty in the treatment planning compuation of dose a to a patient (4.2%) Computation of relative dose dose distribution (without heterogeneity) (3%) Central axis factors for beam modifiers (2%) AAPM Report #13 Spatial Uncertainties (95% confidence level) Spatial uncertainty from machine and patient motion (10 mm) Displacement due to mechanical inaccuracies (5 mm) Isocentric accuracy (2mm) Radiation field (2mm) Jaw accuracy (2mm) Radiation Isocenter (2mm) Positional errors due to patient or organ motion (8 mm) Setup error (6mm) Breathing motion (4mm) Organ motion (4mm) AAPM Report #13 “Calculation of the uncertainty in the dose delivered during radiation therapy” Michael Goitein, Med. Phys. 12(5), 608‐12, 1985 “There are inevitable uncertainties in the process of planning and delivering radiation therapy. They may stem from a variety of causes including patient motion, inexact placement of treatment fields: discrepancies between therapeutic situations and that in which treatment was planned;..... However it is essential to identify their sources and assess their magnitude in order to estimate the overall accuracy of therapy and ensure that it achieves the clinically appropriate level” “Calculation of the uncertainty in the dose delivered during radiation therapy” Michael Goitein, Med. Phys. 12(5), 608‐12, 1985 Uncertainty sources in radiotherapy Planning stage IU Delivery stage SOU NOU IU for planning accounts for dose uncertainty inherently existing in RTP system. It is mainly due to: grid size, dose calculation algorithm, and off‐axis behavior. SOU for delivery is caused by all spatial displacements such as the mechanical variation of treatment machine, inaccuracy of patient setup, and external/internal motion of patient. NOU for delivery is caused by quantum statistics of any irradiator through the beam line, mainly monitor chamber. A relative SD of NOU is simply assumed to be inversely proportional to monitor unit (MU). Dose uncertainty model Dactual ( r ) Dcal ( r ) II( r()r )ZZtotal total ( r ) Overall dose uncertainty Planning Inherent uncertainty (I(r)) Grid size effect (Igrid(r)) Algorithm effect (Ialgo(r)) Off‐axis effect (moa(r)) Delivery Statistical uncertainty (total(r)) Space‐oriented Uncertainty (SOU; SOU) Non‐space‐oriented Uncertainty (NOU; NOU) Planning Inherent dose uncertainty 1. A significant dose difference exists in high‐dose gradient regions. This phenomenon is assumed to be mainly caused by the finite size of the calculation grid, the finite size of the detector system during treatment planning commissioning, and a possible mismatch of reference field sizes between actual measurements and mathematical calculations. 2. A fair amount of dose discrepancy is observed near the field edge and it decreases along with the distance from the edge. This may be due mainly to an imperfection of the dose calculation algorithm itself and partly a typical normalization method used in relative dosimetry (i.e., normalization at the center). 3. A greater dose difference is observed at the off‐axis compared to the central axis. This is assumed to be mainly attributed to inaccurate modeling of off‐axis fluence (or spectrum) and a possible variation of beam symmetry (i.e., while a field from most radiation TPSs is symmetric, an actual beam is not). Igrid Ialgo moa Inherent dose uncertainty (IU) Planning IU illustration for a 5 X 5 cm2 open field Igrid + Ialgo × moa = Itotal I grid ( rp ) Dcal ( rp ) r Ialgo(rp) =(0.03·d(rp) + 1.9) × Dcen(rp) moa(rp)=0.015·|rp-rpo| + 1 SOU prediction (convolution) Delivery Patient Machine Gantry Collimator Couch (x, y, z, x, y, z, b) Patient Setup Internal Organ Motion (x, y, z, x, y, z) Planning Delivery Dcal PDFs Convolution ⓧ SOU (r ) For fractions (N) Lujan et al, Med Phys 26, 2397‐2402 1999 Degrees of freedom for sources of delivery uncertainties Delivery Patient Machine Quantified by Gantry [Rotation] (g) (1) Measurements (collimator Beam limiting devices angle) [Translation, Rotation] (x, y, z, b) (2) Annual QA data (collimator (x and y), SSD(z)) Couch [Rotation] ( c) (3) Peer‐reviewed publication (MLC) (Systematic , Random ) External Patient Setup Quantified by [Translation & Rotation] (1) Measurement using Brainlab (x, y, z, Exactrac (IR markers) x, y, z) (Systematic , Random ) (2) Cone‐beam CT Internal Organ Motion [Translation, Rotation] (x, y, z, x, y, z) (Systematic , Random ) PDF (Gaussian) for convolution (7 Degrees Of Freedom (DOF’s)) N DOF ( r ) 1 DOF ( r DOF ) 2 exp 2 2 2 DOF 3 DOF’s for translation: x, y, z 4 DOF’s for rotation: x, y, z, collimator NOU Prediction Relative SD is inversely proportional to the dose level NOU (r ) rel ,o MU o Dcal (r ) MU cal Meas. Theory SD for 15 meas. w/ ion chamber Delivery Dose uncertainty of IMRT delivery (Dose accumulation history) For a subfield, s Itotal(r)= Igrid(r) + Ialgo(r) × moa(r) total ( r ) SOU ( r ) 2 NOU ( r ) 2 For all subfields, S S I overall (r ) I total , s (r ) overall (r ) s S 2 ( r ) total , s s Uncertainty Model Validation Dose difference distribution between calculation and measurement Overall dose uncertainty of 95.4% confidence level (a) pyramid, (b) valley, (c) wedge, (d) checkerboard All dose difference points in the test patterns were contained within the overall dose uncertainty distribution of 95.4% confidence level. ( I overall ( r ) 2 overall ( r )) Jin et. al. Med. Phys. 35, 2008 Verification Dose Difference (Dose Difference vs. Predicted Uncertainty) Uncertainty Verification (Dose Difference vs. Predicted Uncertainty) For 32 IM fields Jin et al. Med Phys., 35(3), pp 982‐996, 2008 Verification (QA Failure Points versus Predicted Uncertainty) + QA Failure Point LOW UNCERTAINTY REGION + + + + + ++ + + + + + + + + + + + + + Uncertainty Map + Correlating uncertainty maps to failed regions in IMRT verification MapCHECK™ (455 diode array) Calculation 3% (ΔD) 3 mm (Δd) MapCHECK™ Measurement Failed points Measurement setup for IMRT QA Verification (Failure Points vs. Predicted Uncertainty) Correlating uncertainty maps to failed regions in IMRT verification Dose distribution Uncertainty map Failed points There is a strong correlation between high dose uncertainty regions and regions of high failure rate. Verification (Failure Points vs. Predicted Uncertainty) 1% & 1mm 2% & 2mm 3% & 3mm Tolerance Values and Sensitivity Analysis General assumptions: • The sensitivity analysis represents the worst case scenario for a single field, which was also the upper‐ bound of overall uncertainty for an IMRT field. • Tolerance values were set to achieve an overall dosimetric accuracy within ±5% and an overall spatial accuracy within ±5 mm. These values were applied to prescription dose level. • Tolerance values given in the TG reports have 95% confidence level (~2σ). • Spatial and dosimetric uncertainties involved in patient motion were excluded. Overall Treatment Planning Uncertainty (Percentage of the prescription dose) Computed Uncertainties (NOU and SOU) (For tolerance values given in TG142) Computed Spatial Uncertainty (computed with σ = 2.3 mm) 2.5 80 2 60 1.5 40 1 20 0.5 0 0 10 20 30 40 50 60 Field size (mm) 70 80 90 100 0 Uncertainty (%; 1 SD) Planned dose (%) 100 Overall Uncertainties (Based on tolerance values given in AAPM TG Report # 62 and 142) Summary Each step of the radiation therapy process has spatial and dosimetric uncertainties, which can be quantified for each treatment protocol and possibly for each patient. Uncertainties arise in 4 stages: 1) treatment planning, 2) patient setup (including inter‐fractional motion), 3) treatment delivery system, and 4) patient intra‐fractional motion (including deformation). uncertainties from patient intrafractional motion and deformation are temporally variant and are both patient and disease‐site specific. Summary The inability of almost one‐third of institutions to pass the IMRT benchmark experiment designed and distributed by the RPC clearly shows the need to have a complete understanding of the potential sources of dosimetric uncertainty in every step of the IMRT process and improve the accuracy of dose delivered to patients. A priori knowledge of potential uncertainties in the form of an uncertainty map in conjunction with the conventional dose distributions provide an opportunity to evaluate comparative plans and select one that satisfies all planning goals with the most accurate dose delivery to patients “Medicine is a science of uncertainty and an art of probability”. “He who studies medicine without books sails an uncharted sea, but he who studies medicine without patients does not go to sea at all”. “The best preparation for tomorrow is to do today's work superbly well”. Sir William Osler (1849‐1919) A Canadian Physician, The Father of Modern Medicine