Oncology Nurse Led Clinics
advertisement

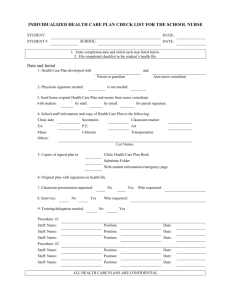
Oncology Nurse Led Clinics An economic assessment of Breast Open Access follow up and Uro-Oncology Clinical Nurse Specialist Clinics Understanding the service The Great Western Hospital Foundation Trust provides cancer services primarily to people living in Swindon and North Wiltshire. Predicted activity figures across all tumour sites demonstrates a steady rise in cancer diagnoses (Appendix 1 and 2). The number of people living with cancer is expected to increase from 2 million to 4 million by 2030 [National Cancer Survivorship Initiative (NCSI), 2013]. This means the number of people requiring specialist care and support will increase through the cancer pathway. The NHS Five Year Forward Report (2014) acknowledges, the healthcare system cannot remain in status quo but needs new models of care to support service delivery. The Cancer Clinical Nurse Specialist can help to improve the quality of life for people with cancer. They can also help empower patients to self-manage their conditions leading to reduced costs for health care providers through hospital appointments, emergency admissions and consultant time. The National Cancer Survivorship Initiative (NCSI) in collaboration with NHS England and Macmillan reviewed follow up practice and made recommendations on the stratified cancer pathway. The table below provides suggested pathways. 1 For the purpose of the economic assessment, the Breast and Uro-Oncology nurse led clinics were selected to undertake an economic assessment of the nurse-led clinics against traditional practice. Clinical Nurse Specialists (CNS) provide specialist advice and support for patients diagnosed with cancer acting as key worker in accordance with National Cancer Peer Review requirements. With an aging population and more people being diagnosed with cancer, the teams have developed their service to meet the needs of their patient population. CNSs are at the front-line of cancer care; they are the main point of contact for patients and as a result help to deliver personalised care for each patient according to need and patient choice, which contributes to wider cancer priorities. CNSs play an important role in enabling care to be delivered closer to home and in improving patients’ ability to self-manage symptoms and side-effects of treatment. The supportive care and information element of the Cancer Clinical Nurse Specialist role should not be underestimated in enhancing the patient experience. This includes providing support for the patient/carer at initial diagnosis, individualised information provision, assisting and supporting with treatment decision making, advice on management of symptoms and side effects, support and assistance with practical issues such as finance, providing emotional and basic (level 2) psychological support, signposting to specialised and support services providing continuity of care. Both during and at the end of treatment the CNS can provide holistic follow-up within a nurse-led clinic. The most recent national cancer strategy 2015-2020 “Achieving World Class Outcomes” emphasizes the importance of the role of the cancer clinical nurse specialist and is the single most important factor for ensuring a positive patient experience. To support the increasing activity and pressures on traditionally medically led clinics, the CNS team have introduced nurse-led clinics to enhance efficiency in the pathway and patient experience. The team have the appropriate skill and education to provide the nurse-led clinic providing a more holistic assessment and ensuring all questions are answered meeting the patient’s needs. This skill is acknowledged by the wider cancer multi-disciplinary teams (MDT) with the MDTs supportive of the clinical development. Whilst no additional CNS were recruited for the delivery of these clinics, the development of clinics would have been difficult if the team had not increased in size to support the increasing patient numbers. It is through improved efficiency in the clinical pathway that the team have been able to include this activity. The following are a summary of nurse led clinics held by the breast clinical nurse specialists. The clinic to be evaluated in the economic assessment is the breast open access follow-up (OAFU). Whilst the tariffs can be provided, it is evident following discussion with the finance team that the elements making up a tariff are not clearly known. With the OAFU clinic a specific tariff was negotiated with the local clinical commissioning group reflecting the time and activity provided in this clinic. 2 The nurse led clinics for Breast CNS: Clinic Frequency Activity Description Traditionally-led Breast Open Access follow-up clinic Weekly 5 patient slots 1hour each End of treatment summary, Holistic Needs Assessment Signposting to Living Well events Clinical Oncologist Surgeon annually for up to 5 years. Ad-hoc & virtual clinics As required Seroma drainage/surgical clinics Telephone clinics which stop a traditional outpatient appointment Surgeon Oncologist Breast Enhanced recovery clinicpre-operative assessment Weekly 45 minute slots 8 patients Clinic supporting enhanced recovery for breast surgery Surgeon The Uro-Oncology CNS nurse led clinics: The following are a summary of the range of nurse led clinics held by the urooncology clinical nurse specialists. For the focus of the economic evaluation, the prostate biopsy results clinic will be used. Clinic Radiotherapy Follow-up Clinic PSA/Support Clinic PSA Telephone Clinic E-HNA Clinic Andrology Clinic TURBT Clinic Prostate Biopsy result clinic Virtual Activity Description Men reviewed 6 weeks following radical/palliative radiotherapy to the prostate Monitoring PSA results in clinic Monitoring stable PSA results via telephone clinic Holistic Needs Assessment Clinic Erectile Dysfunction style clinic Provision of bladder histology results following surgery Provision of prostate biopsy results following MDT discussion Telephone and in person review ad hoc supporting patient need and reducing need for consultant review/admission Traditionally-led Clinical Oncologist Urologist Urologist Nurse-led Urologist Urologist Urologist Nurse-led 3 Breast OAFU Clinic: In 2012, in line with the NCSI recommendations, the breast MDT with patient involvement, reviewed standard follow up practice for patients following adjuvant breast cancer treatment. Metastatic breast patients are not included in this pathway. Adjuvant follow-up included annual review by the surgical and oncology teams for 5 years. Most patients were discharged at this time but for some psychologically they preferred on going annual review to ensure access to the system if required. With the breast open access follow up clinic (OAFU), following the completion of adjuvant treatment (surgery, chemotherapy & radiotherapy) the patient is referred for an end of treatment summary, holistic needs assessment and signposting to living well events and support groups. The patient is given written information listing treatment to date and advice on symptoms that require rapid access back into the healthcare system. A telephone number is provided to call if required for an urgent appointment in the breast clinic within 2 weeks. This stops the follow up of adjuvant breast cancer patients on an annual basis in both the breast surgical clinics and oncology clinics for up to 5 years. This type of follow up reduces the anxiety associated with routine follow up and empowers the patient to access at time of need with symptoms of concern. Anecdotally recurrence is often diagnosed between routine appointments and results in a person requiring an additional appointment or people waiting with symptoms until the next follow up appointment. Whilst 18 patients have re-accessed the service to date no one was diagnosed with a recurrence. This correlates with national work where the figures are presumed small. Financially the nurse led service is cost effective, meets national guidance and has met the patients’ needs demonstrated in a patient experience survey and Family & Friends testing. There have been no complaints received nor any incidents reported for this service. One Band 7 CNS conducts the OAFU clinic but two other CNS are also skilled to conduct the clinic to ensure it is not cancelled at times of leave. The nurses have completed the breast care module at the Royal Marsden Hospital. These clinics require suitably trained specialist staff. The nurses do not receive any health care assistant support to run the clinic nor prep the notes. The CNS spends approximately 2 hours per week prepping clinics. The patient pathway facilitator supports the maintenance of the OAFU database, approximately 2 hours/week. For a small cost, a health care assistant supporting the clinic and note preparation would reduce CNS time. It would also provide equality in service provision. Support of medical clinics is a given within the Trust but not supported for nurse clinics providing similar activity. 4 Traditional Medical Follow-up Early Breast Cancer- Surgery, Chemotherapy, Radiotherapy, Hormone treatment as required Traditional follow-up: Annual outpatient appointment with Breast Surgeon (4 OPA) Annual outpatient appointment with Oncologist (4OPA) CNS may also be in attendance at this appointment. Annually, 230 clinic slots released for both ← breast surgery and oncology allowing the consultant to see new patient/increasing activity. This will result in increased income for the Trust from new patient tariff. This is about efficiency in the pathway and the release of outpatient appointments for increasing predicted activity and the more complex patient pathway. This will increase service capacity allowing consultants to see more new patients and this comes with a higher tariff. Cost of a 3 hour consultant clinic (usual sessional clinic time- BMA reference cost) £891 Open Access Follow-Up CNS led Early Breast Cancer- Surgery, Chemotherapy, Radiotherapy, Hormone treatment as required Open Access Follow-Up (OAFU) 1 Nurse led appointment (1hour) to complete End of Treatment Summary, Holistic Needs Assessment and signpost to living well/support groups OAFU Tariff £164 5 appointments weekly £164 x5= £820 £820 x46 clinics/year=£37720 Annual number of patients: 230 230 patients x 8 OPA (1 patient f/u OPA over 4 years) = 1840 appointments released for new patients. It is acknowledged the Trust and nationally we are seeing increasing predicted activity & more complex patient pathways. From 1 year of activity, 920 Breast surgery appointments released over 4 years 920 Breast oncology appointments released over 4 years. A small percentage of patients will reaccess the service. Cost for Breast OAFU clinic £572 £654 with HCA support 5 Key benefits of this innovation For those using the service: Enhanced patient experience Patient pathway meeting NCSI guidance supporting Living Well & National cancer strategies. Fewer appointments at the hospital, possibly reduction of 4 years follow-up. Psychological benefit allowing patient to move forward, live well & selfmanage. Holistic patient assessment To the healthcare system: Efficiency in pathway Enhanced tariff Release consultant time to see new patients improving access to service & receiving enhanced activity Cost effective service- right band/right skill New patient tariff from increasing activity and OPAs released for Consultant activity Quality service To the wider health and social care system: Appropriate tariff for OAFU clinic Release of consultant time to new or more complex patients. Increasing activity figures- support clinical demand. Key costs of this innovation: The set up and running costs are listed in more detail in Appendix 3 and 4 Set up costs Direct £6043 Indirect Nil Total £6043 Weekly Running costs £572 £654 with HCA support Training costs Breast Marsden Module £970 Nurse-led clinics conference £175 It should be acknowledged that these costs are listed in the set-up costs but the CNS requires this training for the specialist role. 6 Demand for this clinic is outstripping supply. The clinic currently has a 6 month waitlist which does not meet national recommendations. A further clinic is required. Uro-Oncology Clinics: The uro-oncology clinical nurse specialists have established numerous nurse-led clinics to support patient need and increasing patient numbers. The clinics have ensured timeliness of access to treatment for patients with urological cancers within national treatment target times. The prostate cancer biopsy clinic improves efficiency in the patient pathway, particularly and will be the focus of this economic assessment. The CNS provides the diagnosis and treatment options following multi-disciplinary team (MDT) discussion and arranges onward referral to appropriate team (urology or oncology). This is releasing consultant Urologist capacity to see more complex and new patients which brings additional revenue at a higher tariff. The CNS supports the patient decisionmaking to determine which clinic the patient returns (surgical or oncology). On average this improves the patient pathway and experience reducing timed pathway by 14 days. Cancer patients will be on a timed pathway subject to 31 & 62 day targets. The CNS clinic will on average release 2 outpatient consultant appointments improving capacity with the consultant clinics for the increasing activity and the more complex patient. The three nurse specialists can support any of the clinics to ensure cover throughout the year and at times of leave. The nurses do not receive any health care assistant support to run the clinic nor prep the notes. The CNS spends approximately 4 hours per week prepping all clinics that could be undertaken by a band 2 health care assistant. The prostate biopsy clinic takes up to one hour to prep. The tariffs have not been included for the uro-oncology clinics but following discussion with the finance team the breakdown of the tariff is not known. No specific tariffs have been negotiated for these clinics. 7 Weekly Clinic Timetable Clinic Day Radiotherapy Follow-up Clinic Monday PM No of patients 4 Length of appointments 30 minutes Total: 120 mins PSA/Support Clinic Tuesday PM 5 10 minutes Total: 50 mins PSA Telephone Clinic Tuesday PM 12 10 minutes Total: 120 mins E-HNA Clinic Wednesday PM Weeks 1 & 3 3 45 minutes Total: 135 mins Andrology Clinic Thursday PM Weeks 2 & 4 4 45 minutes Total: 180 mins TURBT Clinic Prostate Biopsy result clinic Friday AM week 1 & 3 PM week 2 & 4 5th Friday if needed 5 Friday AM week 2 & 4 PM week 1 & 3 5th Friday if needed 5 20 minutes Total: 100 minutes 30 minutes Total: 150 minutes This does not include virtual activity. 8 Prostate Biopsy Results Clinic Traditional medical follow-up Uro-Oncology CNS follow-up Consultant first appointmentAssessment Consultant first appointmentAssessment TRUS Biopsy- Radiology TRUS Biopsy-Radiology MDT Discussion MDT discussion Results provided with Consultant and CNS MRI arranged as required MDT discussion following MRI Results provided by CNS MRI arranged as required Results OPA & treatment discussion by Consultant & CNS Results OPA & treatment discussion by CNS Surgical or Oncology OPA Cost for a 3 hour consultant clinic £891 (BMA reference costs) MDT discussion following MRI Surgical or Oncology OPA Cost for a CNS clinic £138 With HCA support £158 & release of 2 consultant appointments 9 Suspected Prostate Cancer Patient Pathway- Timed pathway comparison Appointment Previous Schedule Pathway Number New of days Pathway Doctor CNS Assessment OPA 11.8.15 TRUS Bx 20.8.15 Results OPA 11.9.15 Consultant 22 & CNS 13.11.15 MRI 21.9.15 10 25.11.15 Results OPA & Treatment discussion 9.10.15 Consultant 18 & CNS Consultant 20.10.15 9 Total Days 16.11.15 Consultant 38 & CNS Doctor 97 days Consultant 27.10.15 7 CNS 17 12 4.12.15 CNS 8 (some consultants 45 days may continue with this element of the pathway) 11/1/16 Oncology OPA 38 CNS 83 days 59 days Oncology OPA Number of days Not only did the CNS pathway save 14 days from time of referral to appointment with an oncologist, it also released two consultant appointments on the pathway. This is significant when considering patient numbers expected in the future. This would improve consultant clinic capacity and allow the doctor to see more complex or new patients. New patient appointments receive a higher tariff to follow up. To provide the clinics two of the CNS have completed the Royal Marsden Hospital UroOncology module and attended the nurse-led clinic study day. Both staff are undertaking Master’s programme. These clinics need suitably trained specialist staff. Key benefits of this innovation For those using the service: Enhanced patient experience Expedite patient pathway- reducing cancer diagnostic pathway for prostate cancer by 14 days & stopping 2 Urologist appointments. Holistic patient assessment 10 To the healthcare system: Two consultant appointments released Efficiency in pathway and possible reduction in cancer breaches. Patient pathway subject to 31 and 62 days cancer target. Release consultant time to see new or more complex patients improving access to service Cost effective service- right band/right skill New patient tariff from increasing activity and OPAs released for Consultant activity Quality of service To the wider health and social care system: Appropriate tariff Release of consultant time to new or more complex patients. Increasing activity figures - support clinical demand. Key costs of this innovation: The set-up and running costs for this clinic are listed in more detail in Appendix 3 and 4. Set-up Costs Direct £1106 Indirect Nil Total £1106 Weekly running costs £138 With HCA support £158 There is a potential for further savings by a health care assistant supporting the clinic and prepping notes. This would release 2 hours of a band 7 CNS time for clinical activity. Training costs GU Marsden module £970 Nurse-led clinics conference £175 This training is required as part of the specialist role and not specifically just for this clinic. 11 Conclusion: The running for each of the clinics incurs similar costs except for the difference in staffing costs and HCA support to the clinic. The weekly running costs have been compared with only the differences listed as per the running templates in Appendix 4. Where costs have been the same, they have not been included. Summary of clinic set-up and running costs Clinic type Traditional Medically led Consultant clinic Prostate Biopsy Clinic- UroOncology CNS Breast OAFU clinic Breast CNS £1106 £6043 £138 £572 £158 £654 Saving: £24.69 & release 2 hours CNS time for clinical activity This would potentially release 1 hour of CNS time to see an additional patient. Release 2 consultant appointments for new activity at a higher tariff. Reduction in follow-up appointments for possibly 4 years. Cost for 3 hour clinic Set up costs Weekly running costs With HCA support: £891 Not supported currently Additional benefits Annual appointment with surgeon and oncologist cease. This releases consultant appointments for new activity at a higher tariff. Enhanced tariff for nurse-led clinic 12 The biggest impact from the nurse-led clinics is to the patient having a reduced timed pathway to treatment and also to the Consultants who will see the release of sessions each week for new & more complex patients. The Trust also benefits from additional revenue from the consultants seeing more new patients at a higher tariff. Feedback from patient survey’s and from family & friends testing for nurse-led clinics has been very positive with all comments positively acknowledging the holistic and comprehensive assessment supporting shared decision-making. Whilst comparison of outcomes demonstrates more patients are reviewed in the medical clinic, the medical clinic will see a wider variety of specialty patients including non-cancer and cancer patients. For patients with a cancer diagnosis, the feedback to date suggests, that the outcomes from a nurse-led clinic experience is equivalent with having health care needs met but with more quality time having concerns listened to and supported. The patients in nurse-led clinics are reviewed earlier in the pathway in comparison to a medical pathway. No complaints or incidents have been noted in these clinics suggesting outcomes for both types of clinics are similar and worthy of comparison. The economic assessment has demonstrated the value of nurse-led clinics providing a service positively evaluated by patients that is value for money. Clinical teams also value the support of nurse led clinics and the time this releases for more complex patients and new patients. Clinical Nurse Specialist clinics improve quality of the service, release capacity in medical clinics and generate income via tariff. Recommendations: Where additional clinics are required; Trusts to recognise value of nurse led clinic and not default to further medical services. For this economic assessment to be repeated across all oncology clinical nurse specialist clinics An additional OAFU clinic be resourced to meet patient demand allowing appropriate capacity Health care assistant support provided for all nurse led clinics to improve efficiency and ensure right staff with right skill doing the job. 13 References 1. National Cancer Survivorship Initiative (2013) “Living with and beyond cancer: Taking action to improve outcomes”, London. 2. Royal College of Nursing (2010) Clinical nurse specialists: adding value to care. An executive summary. London. 3. http://alisonleary.co.uk/docs/RCN%20Study%20Adding%20Value%20to%20 Care%20the%20work%20of%20the%20CNS..pdf (Accessed 25November 2015) 4. https://www.rcn.org.uk/employment-and-pay/nhs-pay-scales-2015-16 (Accessed 13 December 2015) 5. http://bma.org.uk/support-at-work/pay-fees-allowances/payscales/consultants-pay-england (Accessed 13 December 2015) 6. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file /300549/Annex_4A_Additional_info_on_currencies_with_national_prices.pdf (Accessed 13 December 2015) 7. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file /214902/PbR-Guidance-2013-14.pdf (Accessed 13 December 2015) 8. https://www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf (Accessed 28 January 2016) 9. http://www.cancerresearchuk.org/sites/default/files/achieving_worldclass_cancer_outcomes_-_a_strategy_for_england_2015-2020.pdf (Accessed 30th January 2016) 10. http://www.bma.org.uk/support-at-work/pay-fees-allowances/fees/feefinder/fee-finder-government-agreed-fees-consultants (Accessed 30th January 2016) 11. https://www.rcn.org.uk/employment-and-pay/nhs-pay-scales-2015-16 (Accessed 30th January 2016) January 2016 This case study was completed by Lyndel Moore, Cancer Nurse Consultant, Trust End of Life Lead Nurse at The Great Western Hospital Foundation Trust in January 2016. Lyndel successfully completed a collaborative learning programme designed to empower nurses to understand, generate and use economic evidence to continuously transform care. The programme was delivered by the Royal College of Nursing and the Office for Public Management, funded by the Burdett Trust for Nursing and endorsed by the Institute of Leadership and Management. You can contact Lyndel by email lyndel.moore@gwh.nhs.uk. 14 Appendix 1 The following table provides indicative figures for cancer diagnoses locally for the next twenty years. This is then broken into predictive figures for the two main Clinical Commissioning Groups (CCGs)- Swindon and Wiltshire, however patients may also attend from Berkshire, Oxfordshire, Gloucestershire and Avon. Table 1 : Forecast increase in cancer diagnosis for GWH 15 Appendix 2: Table 2 : Swindon CCG – forecast new diagnoses at GWH NUMBER OF PATIENTS DIAGNOSED BLADDER BREAST CERVIX CNS COLON ENDOMETRIUM HEAD AND NECK HODGKIN LYMPHOMA KIDNEY LEUKAEMIA LUNG MELANOMA MYELOMA NHL OESOPHAGUS OTHER TUMOURS OVARY PANCREAS PROSTATE RECTUM SARCOMA STOMACH TESTIS TOTAL 2015 30 167 7 15 92 27 29 6 28 25 114 41 13 33 29 110 23 25 116 27 6 23 8 995 2016 31 169 7 15 94 27 29 6 29 26 116 42 14 33 29 112 23 26 119 28 6 23 8 1010 2017 31 171 7 15 96 28 30 6 30 26 117 43 14 34 30 114 23 26 122 28 6 23 8 1026 2018 31 172 7 15 98 28 30 6 30 26 119 44 14 34 30 115 23 27 125 29 6 23 8 1042 2019 32 174 7 15 100 29 31 6 31 26 121 46 14 35 31 117 23 27 128 29 6 24 8 1058 2020 32 176 7 16 101 29 31 6 32 27 123 47 14 35 31 119 23 28 131 30 6 24 8 1075 2026 35 186 7 16 113 32 35 6 37 28 136 57 15 39 34 130 23 31 150 33 6 25 8 1182 Table 3 : Wiltshire CCG – forecast new diagnoses at GWH NUMBER OF PATIENTS DIAGNOSED BLADDER BREAST CERVIX CNS COLON ENDOMETRIUM HEAD AND NECK HODGKIN LYMPHOMA KIDNEY LEUKAEMIA LUNG MELANOMA MYELOMA NHL OESOPHAGUS OTHER TUMOURS OVARY PANCREAS PROSTATE RECTUM SARCOMA STOMACH TESTIS TOTAL 2013 30 162 9 13 83 21 23 5 24 24 90 45 16 36 20 47 17 21 131 33 6 15 5 878 2014 30 163 9 13 85 22 24 5 25 25 92 47 16 36 20 48 17 22 134 34 6 15 5 892 2015 31 165 9 13 86 22 24 5 25 25 93 48 16 37 21 48 17 22 137 34 6 16 5 906 2016 31 167 9 13 88 22 25 5 26 25 95 50 17 37 21 49 17 23 140 35 6 16 5 921 2017 32 168 9 13 89 23 25 5 26 25 96 51 17 38 21 50 17 23 144 35 6 16 5 936 2018 32 170 9 14 91 23 26 5 27 25 98 53 17 38 22 51 17 23 147 36 6 16 5 951 2019 33 172 9 14 93 24 26 5 28 26 100 54 17 39 22 51 17 24 150 37 6 16 5 966 2020 33 173 9 14 94 24 27 5 29 26 101 56 17 40 22 52 17 24 154 37 6 16 5 982 16 2026 36 184 9 14 106 26 30 6 33 27 112 68 19 43 24 57 17 27 176 41 6 17 5 1,083 Appendix 3 Set Up Costs: Uro-Oncology CNS clinic Identify Additionality Set Up costs-Direct costs 2015 Apportion Full costs Real terms 1CNS Band yes Yes- 8hrs 8hours £18.36 Yes 2.5% 7- time to set of CNS x 8= £146.88 inflation up clinics & time + 22.5%on (1 year) writing costs protocol, =£169.38 £173 (2015) discussing Agenda for with MDT change- mid point payscales (2014) 2 Band 6 Yes Yes- 4 hours each= Yes 2.5% CNS (PCUK apportion 8 8hours total inflation funded x 1)- hours £15.37 (1 year) time to set up x8=£122.96 + clinics, oncosts reading 22.5% = policy, £149.89 discussing £153.63 (2015) Agenda for with MDT change- mid point payscales (2014) Training staff No- required No within role Each CNS: No £970 Royal Marsden Module £175 Nurseled clinic conference MDT approval of protocols for follow-up yes yes £760 1 hour £207 BMA Consultant Yes 2.5% inflation (1 year) £779 hourly rate: + on costs 17 22.5%= £253.57 Urologist, Medical Oncologist, clinical oncologist Indirect costs Telephone From existing resource Patient From existing information resource Premises In kind from Estates IT support/ In kind from computer corporate Secretarial From existing support resource Total: £1106 18 Breast OAFU clinic Identify Additionality Set Up costs-Direct costs Apportion Full costs Real terms 2012 OAFU Working yes 8 hours Group- Medical 8hours 1 hour £207 Oncologist, BMA Consultant Surgeon, hourly rate x 2 Cancer Consultants = Manager, CNS, £3312 +22.5%= patient £4057 representative, Lead Cancer CNS8hours Nurse £18.36 x 8= £146.88 + Yes 2.5% inflatio n (4 year) £4372 2012 £187 22.5%on costs =£169.38 Band 8 NHS AFC mid-point manager & Lead nurse £25.55 x 2= £51.10 x8= £408.80 +22.5% £553 oncosts= £500.78 Patient Representativevoluntary 1 Band 7 CNS 1 week 37.5 Yes time to set up hours total 2.5% clinics, writing £18.36 inflatio policy, writing x37.5hrs=£688.5 n (4 patient 0+ oncosts year) information, 22.5% = £843.41 setting up new process discussing with Yes 37.5hrs £931 Agenda for change- mid point payscales MDT 19 Training staff No required No for role Each CNS: No Royal Marsden module £970 Indirect costs Premises In kind from Estates IT support/ In kind from computer corporate Telephone In kind from corporate Secretarial From existing support resource Total: £6043 20 Appendix 4 Running Costs per week: Uro-Oncology CNS Running costs-Direct costs Identify Additionality Apportion Full costs Real terms Uro- 5 hours yes 5hours 2.5% Oncology £18.36 x5= inflation- CNS Band 7 £91.80 + 1 year 22.5%on £115 costs =£112.45 (2015) Agenda for changemid point payscales CNS 1hours 1hours 2.5% Prepping £18.36 + inflation- and 22.5%on 1 year supporting costs clinic =£22.49 £23 (2015) Agenda for changemid point payscales £8.29 x 2= HCA Band 2 2 hours £16.58 supporting +22.5%= clinic & £20.31 prepping notes (not provided nor funded currently) Potentia l saving if HCA support s clinic : £24.69 & release 2 hours CNS time 21 Indirect costs (Add rows as required, and indicate year) Premises In kind Computer/te In kind lephone Patient charity information Secretarial In kind Support Total £138 Weekly running cost: £158 With HCA support Potential £24.69 saving if & HCA release supports 2 hours clinic : CNS time for clinical activity 22 Breast OAFU Running Costs-Direct costs Identify Breast CNS (Band Additionality 10 hours/week Apportion yes 7) Full costs Real terms 10hours (4 years £18.36 x10= inflation £183.60 + 2.5%) 22.5%on £248.25 costs =£224.91 Agenda for change- mid point payscales Breast MDT Co- 1 hours/week yes ordinator (Band 4) £10.66 £14.41 +22.5%= £13.05 OAFU MDT Agenda for change- mid point payscales Patient Pathway co- 2 hours/week yes ordinator (Band 4) £10.66 x2= £28.82 £21.32 +22.5%= Updating OAFU £26.11 database Agenda for change- mid point payscales Breast Medical 1hours/week yes 1 hour £207 Oncologist (for BMA OAFU MDT) Consultant £279.90 hourly rate +22.5%= £253.57 HCA Band 2 8 hours £8.29 x 8= supporting clinic & £66.32 prepping notes (not +22.5%= provided nor funded £81.24 currently) 23 Indirect costs (Add rows as required, and indicate year) Premises In kind Computer/telephone In kind database In kind Patient information charity Total weekly running costs= £571.38 24 Urology Consultant Clinic Running costs-Direct costs 2015 Identify Additionality Apportion Full costs Real terms Oncology CNS 3 hours yes Band 7 3 hours 2.5% £18.36 inflation- x3= £55 + 1 year 22.5%on £69 costs =£67.50 2015 Agenda for changemid point payscales Urologist 3 hours yes 3 hour £780 £207 BMA Consultant hourly rate +22.5%= £760 HCA Band 2 4 hours £8.29 x 4= supporting clinic & £33.16 prepping notes +22.5%= £41.63 £40.62 Indirect costs (Add rows as required, and indicate year) Premises In kind Computer/telephone In kind Patient information Charity Secretarial Support In kind Total Weekly running cost: £891 25 Appendix 5 Pathways to Outcomes: Input Direct costs• Skilled Breast Care Clinical Nurse Specialist to provide Breast OAFU clinic • Breast MDT discussion • Service provided in outpatient setting 1 day/ week • Clinic room • Telephone service for assessment and rapid re-access of service if required • Telephone line • Computer to record Holistic Needs Assessment (HNA)and End of treatment summary • Patient information on service and Living well information • IT to access PAS and cancer services system • Admin staff to upload to IT system & send to GP • No direct funding of service Indirect Costs • Hospital accommodation/ overheads for clinic room • Outpatient team • IT support Input Direct costs• Skilled Uro-oncology Clinical Nurse Specialist to provide variety of follow-up • Uro-oncology MDT discussion • Service provided in outpatient setting • Clinic room • Telephone service for PSA clinic • Telephone line • Computer to record Holistic Needs Assessment (HNA)and clinic assessment and letter • Patient information on service and Living well information • IT to access PAS and cancer services system • Secretarial support to send to GP • PCUK funding for 1 WTE Band 6 • Macmillan 1WTE Band 7 funding (historicalpicked up by Trust) • 1WTE funded by Trust Indirect Costs • Hospital accommodation/ overheads for clinic room • Outpatient team • IT support Breast Open Access Follow-up (OAFU): Pathways to Outcomes model Activities & outputs • Number of patients seen in OAFU clinic •Number of patients awaiting an appointment •Number of calls •One hour clinic appointment with CNS to complete end of treatment summary (ETS) reviewing history, long term side-effects of treatment, possible signs of recurrence, ongoing care e.g. mammograms & Dexa scan. Hormone treatment. •Holistic Needs Assessment (HNA) •Advice on self management •Referral to Living well day •Patient support groups •Information on reaccessing service •ETS & HNA to GP •Patient information •1 Nurse led clinic (1hr clinic review/patient) completing above. Follow-up practice for next 4 years no longer required releasing consultant colleagues to see more complex and rising activity of new patients Outcomes Groups targeted Staff outcomes For intervention • Adjuvant/early diagnosis breast cancer patients. •Breast surgeons •Breast MDT •Medical & Clinical Oncologists •Administrative support •Outpatients department For training •All Breast CNS •Patient Pathway facilitator For partnership • Swindon and Wiltshire Clinical Commissioning groups • GP For delivery • As for intervention •Ability to deliver high quality care & streamline follow-up practice for breast cancer patients •Improves quality of patient/nurse experience. Satisfaction of delivering a quality service meeting individual patient needs •Nurse-led clinic activity •Medical teams release capacity to see more complex and increasing new patient activity. Patient outcomes •Patient access to specialist advice supporting Living well and beyond cancer initiative •Improved patient experience; less anxious about follow up appointment •Psychologically patients able to move forward and live well Organisational outcomes •Prevention of inappropriate followup •Meet National Cancer survivorship initiative •Evidence of economic impact of change •In house skills – economic evaluation •Trust Presentations at external events •Potential publications V1 21 June 2015 1 Uro-Oncology Clinical Nurse Specialist clinics: Pathways to Outcomes model Activities & outputs • Number of patients seen in each clinic •PSA clinic •Post Radiotherapy clinic •Prostate histology clinic •Bladder histology clinic •HNA clinic •Andrology clinic •Holistic Needs Assessment (HNA) •Advice on self management •Referral to Living well day •Patient support groups •Patient information Outcomes Groups targeted Staff outcomes For intervention • Uro-oncology patients. •Urologists •Urology MDT •Medical & Clinical Oncologists •Administrative support •Outpatients department For training •All Uro-oncology CNS For partnership • Swindon and Wiltshire Clinical Commissioning groups • GP For delivery • As for intervention •Ability to deliver high quality care & streamline follow-up practice for urology cancer patients •Improves quality of patient/nurse experience. Satisfaction of delivering a quality service meeting individual patient needs •Nurse-led clinic activity •Medical teams release capacity to see more complex and increasing new patient activity. Patient outcomes •Efficiency in patient pathway. Time to treatment more efficient •Improved patient experience •Consultant OPA x2 released allowing review of more complex and increasing patient numbers. Organisational outcomes •Efficiency in service with consultants time released to cope with increasing demand and more complex patients. •Evidence of economic impact of change •In house skills – economic evaluation •Trust Presentations at external events •Potential publications January 2016 1 26