Objectives: TSWBAT differentiate between types of insurance
advertisement

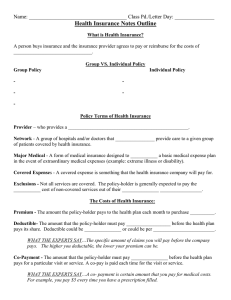
Objectives: -TSWBAT differentiate between types of insurance programs and terms by taking notes. -TSWBAT understand the different types of insurance by analyzing which health insurance plan available would best fit the students’ needs. • A person buys insurance and the insurance provider agrees to pay or reimburse for the costs of medical care • “Gambling analogy” • In 2006, 47 million people in the U.S. (16% of the population) who were without health insurance for at least part of that year https://www.youtube.com/watch?v=dTuIr_zrHkQ Can name some carriers/companies??? http://www.healthinsurancesort.com/carrier-list.htm • What’s the #1 reason young adults end up in bankruptcy? • Large, unexpected medical bills from • an accident • an illness Combined with… • NO health insurance • YES! • How much does a broken leg cost? • $5,000 - $20,000 • How much does a serious car accident cost? • $50,000 Group Policies – • provided by employer • you employer pays for all or most of you insurance plans cost • All employees at work have the same health insurance options as you do • Commonly called “benefits” Individual Policies – • you buy the policy yourself • Very similar to the way you get car insurance • About 9% of the population gets their health insurance this way • Provider – • provides a health care service • Network – • group of hospitals and/or doctors that jointly provide care to a given group of patients covered by health insurance • Major Medical – • form of medical insurance designed to supplement a basic medical expense plan in the event of extraordinary medical expenses • Example - extreme illness or disability • Covered Expense – •something that the insurance plan will pay for • Exclusions – •Not all services are covered. The policyholder is generally expected to pay the full cost of non-covered services out of their own pocket. • Premium – • The amount the policy-holder pays to the health plan each month to purchase health coverage • Deductible – • The amount that the policy-holder must pay out-ofpocket before the health plan pays its share • Deductible could be yearly or could be per injury / illness • Read italic paragraph in notes… • Example: Your yearly deductible is $500.00 and your medical Bill is $2,500.00. Your Insurance company pays $2,000.00 and you pay the deductible of $500.00. • Copayment –The amount that the policy-holder must pay out of pocket before the health plan pays for a particular visit or service. –Example • a policy-holder might pay a $45 copayment for a doctor's visit, or to obtain a prescription. –A copayment must be paid each time a particular service is obtained –Read italic paragraph in notes… - Organized system of health care services designed to control health care costs - Use of a panel or network of health care providers to provide care to enrollees - Managed care usually involves: 1. Standards for selecting providers 2. An emphasis on preventive care 3. Financial incentives to encourage enrollees to use care efficiently • HMO – Health Maintenance Organization • PPO – Preferred Provider Organization • Co-Insurance • Other kinds of plans (we will not go in depth with these plans): • EPO = Exclusive Provider Organization • POS = Point of Service Plan • HDHP = High Deductible Health Plan • Catastrophic Health Insurance Plan • HMO = Health Maintenance Organization • Manage patients' health care by reducing unnecessary services • Most HMOs require members to select a primary care physician (PCP) •Physician acts a gatekeeper to medical services • PCP authorizes referrals to specialists or other doctors if deemed necessary. This is called a “referral.” • Emergency medical care does not require prior authorization from a PCP • Most HMO’s will only pay for medical bills for services your PCP approves through referral • HMOs typically provide no coverage for care received from non-network physicians • exceptions for emergency care while traveling, etc. • Organization of medical doctors, hospitals and other health care providers • “network” or “preferred provider” • Network is contracted with an insurer to provide health care coverage at a reduced rate (substantial discount) • Some surgeries or procedures may need to require pre-approval by the insurance company • PPO’s will reimburse some of your costs if you go out of network: • PPO may reimburse 90% of costs for care received within the network, but only 70% of costs for non-network care CAN YOU NAME THREE DIFFERENCES BETWEEN A PPO AND A HMO? • Instead of paying a fixed amount up front (a copayment), the policy-holder must pay a percentage of the total cost. • Because there is no upper limit on coinsurance, the policy-holder can end up owing very little, or a significant amount, depending on the actual costs of the services they obtain. – Example• member might have to pay 20% of the cost of a surgery, while the health plan pays the other 80%. • Dental Insurance – required to have if age 18 or younger / helps totally or partially cover dental cleanings and other procedures needed (fillings, root canals, crowns, etc.) • Vision Insurance – not required to have / helps partially cover eye check-ups, contacts or glasses • Hospitalization Insurance- Specifically pays for hospitalization • Surgical Insurance – Specifically pays for fees associated with surgery • Disability Insurance – Pays for loss of income due to accident or illness; Usually only a percentage of your salary • Medicaid – • health insurance for people with lower incomes • Funded by state and federal government • Eligibility rule vary state to state • Example of Medicaid requirements • You're a pregnant woman who meets income requirements. For example, a family of four making $23,225 a year or less qualifies. • Your family's assets are less than $2,000 • Medicare – • Government health coverage for people 65 years or older • In many cases Medicare pays a portion of the person’s health care cost. • The rest is paid by the person or supplemental insurance plan • Women Infants and Children • Program that helps mothers and children with medical bills • • • • Prenatal care Preventive screenings Immunizations Pay for “proper” food and medicines You do not need to copy this acronym onto your t-chart… • Children’s Health Insurance Program • Uninsured Pennsylvania children and teens that are not eligible for Medicaid have access to affordable, comprehensive health-care coverage. • Once enrolled, children are guaranteed 12 months of CHIP coverage unless they no longer meet the basic eligibility requirements. • Families must renew their coverage every year in order for the coverage to continue. • There is no waiting list to enroll in CHIP. You do not need to copy this acronym onto your t-chart… • COBRA • Consolidated Omnibus Budget Reconciliation Act (1985) • Lose your job - may continue to pay your insurance premium & maintain coverage • This also applies to children on insured employees • If a child somehow loses full-time student status that child may make a COBRA payment to maintain coverage You do not need to copy this acronym onto your t-chart… • Beginning Oct 1 2013, the Health Insurance Marketplace will make it easy for Pennsylvanians to: • compare qualified health plans • get answers to questions • find out if they are eligible for lower costs for private insurance or health programs like Medicaid and the Children’s Health Insurance Program (CHIP), and enroll in health coverage. • Uninsured Pennsylvanians who are eligible for coverage through the Marketplace. • • • • • • • • 1,242,350 (12%) are uninsured and eligible 928,243 (75%) have a full-time worker in the family 491,258 (40%) are 19-34 years old 864,180 (70%) are White 201,028 (16%) are African American 114,374 (9%) are Latino/Hispanic 33,494 (3%) are Asian American or Pacific Islander 707,872 (57%) are male • 1,141,720 (92%) of Pennsylvania’s uninsured and eligible population may qualify for either tax credits to purchase coverage in the Marketplace or for Medicaid if Pennsylvania takes advantage of the new opportunity to expand Medicaid coverage under the Affordable Care Act. • Pennsylvania has received $34,832,212 in grants for research, planning, information technology development, and implementation of its Health Insurance Marketplace. Let’s see some plans available on www.healthcare.gov! • Single Payer = • Single-payer health care is a system in which the government, rather than private insurers, pays for all health care costs • Universal Health Care = • It is organized around providing a specified package of benefits to all members of a society with the end goal of providing financial risk protection, improved access to health services, and improved health outcomes. Universal health care is not a one-size-fits-all concept Centrally controlled heath care system (government) – pay higher taxes Sometime requires supplemental health insurance http://chartsbin.com/view/z1a Please write your answer on your notes outline. Be prepared to share your thoughts shortly… Do you know what coverage you will have when you graduate from NP? • On the post-it note, please write a response to one of the following: – A question you have about today’s notes – A reaction about health insurance in the USA or to your health insurance policy – Something you learned that was new regarding health insurance DO NOT WRITE YOUR NAME ON THE NOTE DO WRITE YOUR CLASS PERIOD/LETTER DAY PLEASE BE HONEST AND RESPECTFUL WITH YOUR RESPONSE