History of IPE
advertisement
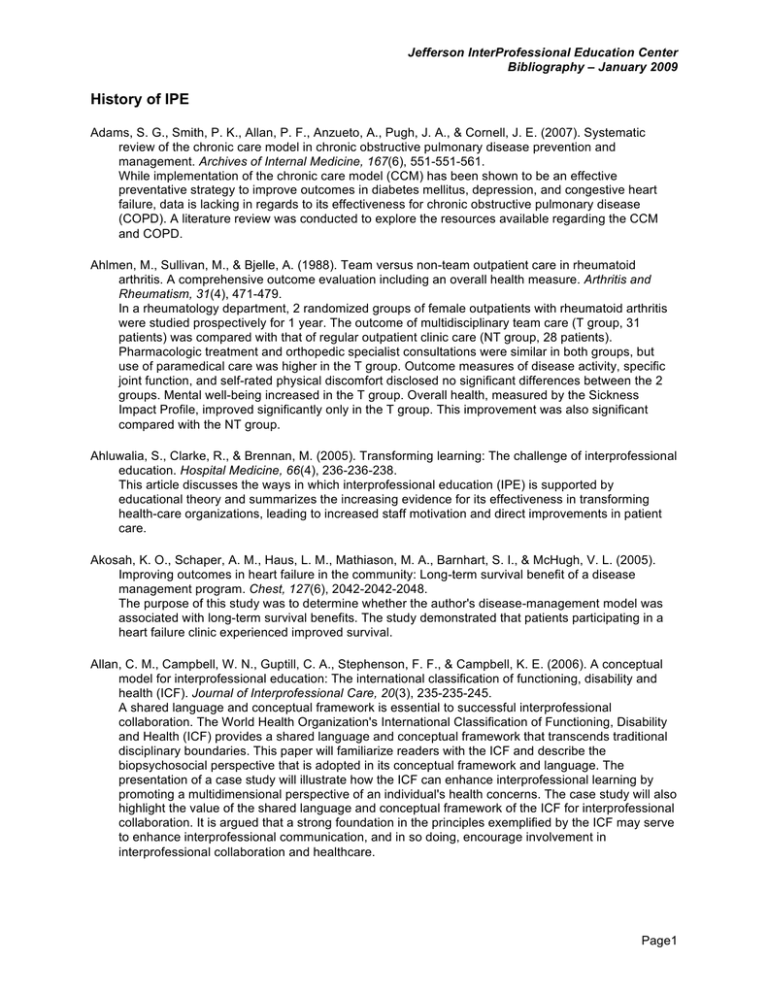
Jefferson InterProfessional Education Center Bibliography – January 2009 History of IPE Adams, S. G., Smith, P. K., Allan, P. F., Anzueto, A., Pugh, J. A., & Cornell, J. E. (2007). Systematic review of the chronic care model in chronic obstructive pulmonary disease prevention and management. Archives of Internal Medicine, 167(6), 551-551-561. While implementation of the chronic care model (CCM) has been shown to be an effective preventative strategy to improve outcomes in diabetes mellitus, depression, and congestive heart failure, data is lacking in regards to its effectiveness for chronic obstructive pulmonary disease (COPD). A literature review was conducted to explore the resources available regarding the CCM and COPD. Ahlmen, M., Sullivan, M., & Bjelle, A. (1988). Team versus non-team outpatient care in rheumatoid arthritis. A comprehensive outcome evaluation including an overall health measure. Arthritis and Rheumatism, 31(4), 471-479. In a rheumatology department, 2 randomized groups of female outpatients with rheumatoid arthritis were studied prospectively for 1 year. The outcome of multidisciplinary team care (T group, 31 patients) was compared with that of regular outpatient clinic care (NT group, 28 patients). Pharmacologic treatment and orthopedic specialist consultations were similar in both groups, but use of paramedical care was higher in the T group. Outcome measures of disease activity, specific joint function, and self-rated physical discomfort disclosed no significant differences between the 2 groups. Mental well-being increased in the T group. Overall health, measured by the Sickness Impact Profile, improved significantly only in the T group. This improvement was also significant compared with the NT group. Ahluwalia, S., Clarke, R., & Brennan, M. (2005). Transforming learning: The challenge of interprofessional education. Hospital Medicine, 66(4), 236-236-238. This article discusses the ways in which interprofessional education (IPE) is supported by educational theory and summarizes the increasing evidence for its effectiveness in transforming health-care organizations, leading to increased staff motivation and direct improvements in patient care. Akosah, K. O., Schaper, A. M., Haus, L. M., Mathiason, M. A., Barnhart, S. I., & McHugh, V. L. (2005). Improving outcomes in heart failure in the community: Long-term survival benefit of a disease management program. Chest, 127(6), 2042-2042-2048. The purpose of this study was to determine whether the author's disease-management model was associated with long-term survival benefits. The study demonstrated that patients participating in a heart failure clinic experienced improved survival. Allan, C. M., Campbell, W. N., Guptill, C. A., Stephenson, F. F., & Campbell, K. E. (2006). A conceptual model for interprofessional education: The international classification of functioning, disability and health (ICF). Journal of Interprofessional Care, 20(3), 235-235-245. A shared language and conceptual framework is essential to successful interprofessional collaboration. The World Health Organization's International Classification of Functioning, Disability and Health (ICF) provides a shared language and conceptual framework that transcends traditional disciplinary boundaries. This paper will familiarize readers with the ICF and describe the biopsychosocial perspective that is adopted in its conceptual framework and language. The presentation of a case study will illustrate how the ICF can enhance interprofessional learning by promoting a multidimensional perspective of an individual's health concerns. The case study will also highlight the value of the shared language and conceptual framework of the ICF for interprofessional collaboration. It is argued that a strong foundation in the principles exemplified by the ICF may serve to enhance interprofessional communication, and in so doing, encourage involvement in interprofessional collaboration and healthcare. Page1 Jefferson InterProfessional Education Center Bibliography – January 2009 American Medical Association. (2007). Initiative to transform medical education: Recommendations for change in the system of medical education Anderson, E., Manek, N., & Davidson, A. (2006). Evaluation of a model for maximizing interprofessional education in an acute hospital. Journal of Interprofessional Care, 20(2), 182-182-194. This article discusses bi-monthly interprofessional clinical teaching workshops which were derived from patient experiences in an acute care hospital after a one-year planning phase. Students utilized a problem-based methodology to analyze a ward case from an interprofessional perspective. The article supports that this half-day learning model can be easily supported by clinical staff. Anderson, G., & Horvath, J. (2004). The growing burden of chronic disease in america. Public Health Reports, 119(3), 263-263-270. This article explores the rise in chronic disease in the US and prevalence based on data from the Medical Expenditure Panel Survey. It recommends orienting medical care towards ongoing care and care management and a special focus on patients with multiple conditions. Anderson, G. F. (2005). Medicare and chronic conditions. New England Journal of Medicine, 353(3), 305305-309. The Medicare Modernization Act of 2003 was the first step in orienting Medicare toward care of patients with chronic illnesses. This article explores other changes that will be necessary to reform Medicare to make it truly responsive to the care of patients with chronic illnesses, including change to the delivery system, the research infrastructure, clinical education, and methods of financing medical care. Anderson, G. F., & Chalkidou, K. (2008). Spending on medical care: More is better? JAMA : The Journal of the American Medical Association, 299(20), 2444-2445. doi:10.1001/jama.299.20.2444 This article dicusses a number of studies which consistently have found that there is little correlation between healthcare spending and outcomes. Anderson, R. M., Donnelly, M. B., Gorenflo, D. W., Funnell, M. M., & Sheets, K. J. (1993). Influencing the attitudes of medical students toward diabetes. results of a controlled study. Diabetes Care, 16(2), 503-505. OBJECTIVE--To determine the effect of two educational interventions on the diabetes-related attitudes of medical students. RESEARCH DESIGN AND METHODS--We studied 67 junior and senior medical students who were participating in the University of Michigan Medical School's Family Practice elective clerkship. Students were assigned to one of two interventions. The first was a 1-wk living-with-diabetes behavioral simulation that involved injections, blood glucose monitoring, diet, exercise, and record keeping. The second intervention involved reading an autobiography about living with diabetes and viewing a videotape about the psychosocial impact of diabetes. RESULTS-No differential impact was found between the two interventions. However, both interventions were followed by a modest positive change in the attitudes of the medical students (which were very positive to begin with) toward the importance of patient autonomy and the value of the team approach to diabetes care. The attitude gains persisted at follow-up for patient autonomy but returned to baseline for team care. CONCLUSIONS--This study suggests that these two educational interventions resulted in modest increases in the already positive attitudes of medical students toward the importance of patient autonomy and team care in diabetes. However, because the study did not include a group that received no treatment, we cannot be certain on this point. The attitude gain related to team care did not persist at follow-up. These findings are consistent with classical attitude research, which suggests that attitudes are sensitive to influences such as these interventions, but that attitude changes may not persist when those influences are changed or withdrawn. We were not able to find a differential impact between the two interventions and suspect that the general nature of the DAS used as the dependent measure may not have been sensitive enough to capture such a differential impact. Page2 Jefferson InterProfessional Education Center Bibliography – January 2009 Anonymous. (2004). Five chronic conditions account for one-third of health care spending growth. Hospitals and Health Networks, 78(10), 90-92, 94. This article discusses the five chronic conditions that account for 1/3 of the growth in healthcare spending, heart disease, trauma, pulmonary disease, mental disorders and cancer and factors contributing to their growth. Anonymous. (2005). Current systems for handling chronic diseases is crippling primary care, study finds. Hospitals and Health Networks, 79(7), 127-127-128. Anonymous. (2006). Older people and the interprofessional agenda. Journal of Interprofessional Care, 20(4), 333-333-334. An introduction to a set of 4 papers that address international and interprofessional gerontology from the perspectives of policy and practice. APTR. (2006). Prevention education resource center: Advancing the teaching of clinical prevention and population health. Retrieved February 11, 2008, from http://www.teachprevention.org/interprofessional.php This website includes resources for clinicians and teachers to learn about the importance of interprofessional practice, interprofessional education in the news, and events taking place. In addition is includes opportunities for discussion forums, faculty exchange, and provides links to other key resources. Auerbach, A. D., Landefeld, C. S., & Shojania, K. G. (2007). The tension between needing to improve care and knowing how to do it. The New England Journal of Medicine, 357(6), 608-613. doi:10.1056/NEJMsb070738 This article, outlines the arguments in favor of rapid dissemination of novel quality and safety strategies and the counterpoints to each of the arguments. It concludes by proposing a framework for evaluating interventions to improve the safety and effectiveness of healthcare. Baker, D. P., Salas, E., King, H., Battles, J., & Barach, P. (2005). The role of teamwork in the professional education of physicians: Current status and assessment recommendations. Joint Commission Journal on Quality and Patient Safety / Joint Commission Resources, 31(4), 185-202. BACKGROUND: The Institute of Medicine (IOM) has recommended that organizations establish interdisciplinary team training programs that incorporate proven methods for team management. Teamwork can be assessed during physician medical education, board certification, licensure, and continuing practice. Team members must possess specific knowledge, skills, and attitudes (KSAs), such as the ability to exchange information, which enable individual team members to coordinate. ASSESSING PHYSICIAN TEAMWORK: KSAs might be elicited and assessed across a physician's career, starting in medical school and continuing through licensure and board certification. Professional bodies should be responsible for the development of specific team knowledge and skill competencies and for promoting specific team attitude competencies. Tools are available to assess medical student, resident, and physician competence in these critical team KSAs. CHALLENGES AND COMPLEXITIES IN TEAM PERFORMANCE MEASUREMENT: For teamwork skills to be assessed and have credibility, team performance measures must be grounded in team theory, account for individual and team-level performance, capture team process and outcomes, adhere to standards for reliability and validity, and address real or perceived barriers to measurement. Barker, K. K., Bosco, C., & Oandasan, I. F. (2005). Factors in implementing interprofessional education and collaborative practice initiatives: Findings from key informant interviews. Journal of Interprofessional Care, 19(Supplement 1), 166-166-176. Health Canada (the federal government department in Canada responsible for health issues) conducted an environmental scan and research report in order to understand interprofessional education and collaborative patient-centered practice. This initiative was implemented through semistructured telephone interviews utilizing grounded theory analysis. Several themes were generated and grouped according to interprofessional education and collaborative practice initiatives. Page3 Jefferson InterProfessional Education Center Bibliography – January 2009 Barker, K. K., & Oandasan, I. (2005). Interprofessional care review with medical residents: Lessons learned, tensions aired--a pilot study. Journal of Interprofessional Care, 19(3), 207-214. doi:10.1080/13561820500138693 Integrated interprofessional care teams are the focus of Canadian and American recommendations about the future of health care. Keeping with this, a family medicine teaching site developed an educational initiative to expose trainees to interprofessional care processes and learning (Interprofessional Care Review; IPC). A formative evaluation pilot study was completed using oneon-one interviews and a focus group (n = 6) with family medicine residents. A semi-structured guide was utilized regarding: knowledge, skills and attitudes related to interprofessional care; their experience of the processes utilized in IPC. Data were analyzed using content analysis. Residents' perspectives on their learning revolved around four themes: changes to understanding and practice of interprofessional care; personal impact of IPC; learning about other health professionals; tension and challenges of IPC learning and clinical implementation. Residents valued the educational experience, but identified that faculty supervisors provided "mixed messages" in the value of collaborating with other health professionals. Implications regarding future educational and research opportunities are discussed. Barlow, J., Wright, C., Turner, A., & Bancroft, G. (2005). A 12-month follow-up study of self-management training for people with chronic disease: Are changes maintained over time? British Journal of Health Psychology, 10(4), 589-589-599. OBJECTIVE: A previous study reported some improved outcomes at 4-month follow-up after attendance on a lay-led, chronic disease self-management course (CDSMC). The purpose of this study was to determine whether changes were maintained over time (i.e. at 12 months) and to describe participants' current use of self-management techniques. DESIGN: The study was a 12-month follow-up of a sample of 171 participants who attended a CDSMC in the UK. METHOD: Data were collected by self-administered questionnaires mailed to participants 12 months after they commenced a CDSMC and via telephone interviews with a sub-sample. RESULTS: The sample had a mean age of 54 years, mean disease duration of 16 years, 73% were women, and chronic diseases included endometriosis, depression, diabetes, myalgic encephalomyelitis, osteoporosis and polio. The significant improvements in outcomes identified at 4 months (i.e. cognitive symptom management, self-efficacy, communication with physician, fatigue, anxious and depressed moods and health distress) were sustained at 12 months. No significant changes between 4- and 12-month assessments were found on any study variables. Interview data confirmed that participants continued to use some of the self-management techniques learned on the course. CONCLUSION: Attendance on the CDSMC may lead to longer-term changes in key outcomes such as self-efficacy, use of some self-management behaviors and some aspects of health status (e.g. fatigue, depressed mood). Barr, H. (2005). Canada as a case study. Journal of Interprofessional Care, 19(Supplement 1), 5-5-7. Editorial: The Editor-in-Chief of the Journal of Interprofessional Care discusses the articles presented in this issue, stating that each article presents a unique perspective regarding the theme of interprofessional education and collaborative practice. Barr, H., Freeth, D., Hammick, M., Koppel, I., & Reeves, S. (2006). The evidence base and recommendations for interprofessional education in health and social care. Journal of Interprofessional Care, 20(1), 75-75-78. This is a summary of findings from a Systematic Review reported in: Barr, H., Koppel, I., Reeves, S., Hammick, M., & Freeth. D. (2005). Effective Interprofessional Page4 Jefferson InterProfessional Education Center Bibliography – January 2009 Education: Argument, Assumption and Evidence. Oxford: Blackwell. With recommendations based on analysis and arguments developed in that book and its companion volume: Freeth, D., Hammick, H., Reeves, S., Koppel, I., & Barr, H. (2005). Effective Interprofessional Education: Development, Delivery and Evaluation. Oxford: Blackwell. Barr, H., & Ross, F. (2006). Mainstreaming interprofessional education in the united kingdom: A position paper. Journal of Interprofessional Care, 20(2), 96-96-104. Interprofessional education (IPE) is being built into the mainstream of professional education for all health and social care professions throughout the United Kingdom driven by the Labor government elected in 1997. This paper suggests some ways to ease constraints and improve outcomes while improving interprofessional learning opportunities. It poses the question, can IPE be sustained within mainstream professional education once the initial enthusiasm ends? Barr, H., & Ross, F. (2006). Student voices. Journal of Interprofessional Care, 20(3), 221-221-222. Four winning essays in the JIC Student Competition, sponsored by Health Canada. Requirements for submission included student authorship, representing not less than two health or social care professions and contributing a perspective on interprofessional education and practice. Batalden, P., Ogrinc, G., & Batalden, M. (2006). From one to many. Journal of Interprofessional Care, 20(5), 549-549-551. This article discusses the shift from a ‘‘one professional: one patient’’ care model to a ‘‘many professionals: one patient’’ model. Baxter, H., Singh, S. P., Standen, P., & Duggan, C. (2001). The attitudes of 'tomorrow's doctors' towards mental illness and psychiatry: Changes during the final undergraduate year. Medical Education, 35(4), 381-383. AIMS: To compare the efficacy of two teaching styles, didactic teaching and problem based learning, in producing enduring change in final-year medical students' attitudes towards psychiatry and mental illness. METHOD: A 1-year follow-up questionnaire survey of two groups of medical students taught psychiatry in their fourth-year training by two different methods. One-year follow-up scores were compared with pre-attachment and post-attachment scores in the fourth year. RESULTS: 70 (68%) students completed both questionnaires at follow-up. The follow-up scores were significantly lower compared with both the fourth-year pre-attachment and post-attachment scores, suggesting that the positive change in attitudes following psychiatric training in the fourth year significantly decayed during the final year. The two teaching methods did not differ in the magnitude of this reduction. CONCLUSIONS: The positive change that occurs in medical students' attitude towards psychiatry, psychiatrists and mental illness after their fourth-year psychiatric training is transient and decays over the final year. Beal, A. C., Doty, M. M., Hernandez, S. E., Shea, K. K., & Davis, K. (2007). Closing the divide: How medical homes promote equity in health care (Results From the Commonwealth Fund: 2006 Health Care Quality SurveyThe Commonwealth Fund. The Commonwealth Fund 2006 Health Care Quality Survey finds that when adults have health insurance coverage and a medical home -- defined as a health care setting that provides patients with timely, well-organized care, and enhances access to providers -- racial and ethnic disparities in access and quality are reduced or even eliminated. When adults have a medical home, their access to needed care, receipt of routine preventative screenings, and management of chronic conditions improve substantially. The survey found that rates of cholesterol, breast cancer, and prostate screening are higher among adults who receive patient reminders, and that when minority patients have medical homes, they are just as likely as whites to receive these reminders. The results suggest that all providers should take steps to create medical homes for patients. Community health centers and other public clinics, in particular, should be supported in their efforts to build medical homes for all patients. Page5 Jefferson InterProfessional Education Center Bibliography – January 2009 Becker, G., Gates, R. J., & Newsom, E. (2004). Self-care among chronically ill african americans: Culture, health disparities, and health insurance status. American Journal of Public Health, 94(12), 20662066-2073. This article discusses the results from a qualitative interview study of African Americans with chronic illness. This article found that self-care activities were culturally based. Those who had some form of health insurance much more frequently reported the influence of physicians and health education programs on self-care regimens than did those who were uninsured. Becker, G., & Newsom, E. (2005). Resilience in the face of serious illness among chronically ill african americans in later life. Journals of Gerontology, 60(4), S214-S214-223. The purpose of this study was to examine older African Americans' philosophies about their chronic illnesses and how those philosophies have affected chronic illness management. In dept interviews were conducted over the course of several years with 38 respondents. This research attests to the importance of examining racism in the analysis of how older ethnic minorities live with chronic illness. Birbeck, G. L., Zingmond, D. S., Cui, X., & Vickrey, B. G. (2006). Multispecialty stroke services in california hospitals are associated with reduced mortality. Neurology, 66(10), 1527-1527-1532. This study sought to evaluate whether a multispecialty service, a distinct hospital ward, protocols, or a specialist are associated with reduced mortality among patients with stroke. The study concluded that multispecialty stroke services are underutilized despite their association with reduced stroke mortality. Biro, M. A., Waldenstrom, U., & Pannifex, J. H. (2000). Team midwifery care in a tertiary level obstetric service: A randomized controlled trial. Birth (Berkeley, Calif.), 27(3), 168-173. BACKGROUND: In 1996 a new model of maternity care characterized by continuity of midwifery care from early pregnancy through to the postpartum period was implemented for women attending Monash Medical Centre, a tertiary level obstetric service, in Melbourne, Australia. The objective of this study was to compare the new model of care with standard maternity care. METHODS: In a randomized controlled trial, 1000 women who booked at the antenatal clinic and met the eligibility criteria were randomly allocated to receive continuity of midwifery care (team care) from a group of seven midwives in collaboration with obstetric staff, or care from a variety of midwives and obstetric staff (standard care). The primary outcome measures were procedures in labor, maternal outcomes, neonatal outcomes, and length of hospital stay. RESULTS: Women assigned to the team care group experienced less augmentation of labor, less electronic fetal monitoring, less use of narcotic and epidural analgesia, and fewer episiotomies but more unsutured tears. Team care women stayed in hospital 7 hours less than women in standard care. More babies of standard care mothers were admitted to the special care nurseries for more than 5 days because of preterm birth, and more babies of team care mothers were admitted to the nurseries for more than 5 days with intrauterine growth retardation. No differences occurred in perinatal mortality between the two groups. CONCLUSIONS: Continuity of midwifery care was associated with a reduction in medical procedures in labor and a shorter length of stay without compromising maternal and perinatal safety. Continuity of midwifery care is realistically achievable in a tertiary obstetric referral service. Bjorke, G., & Haavie, N. (2006). Crossing boundaries: Implementing an interprofessional module into uniprofessional bachelor programmes. Journal of Interprofessional Care, 20(6), 641-641-653. This paper describes experience gained during the five-year implementation period of this study. Empirical data was collected through participatory observations, students' and tutors' evaluations, and group interviews with tutors and faculty leaders. Lessons learned can be summed up as: time, resources. staff consensus in dealing with and overcoming traditions and attitudes. Another lesson learned was that the students' learning is a socialization process which needs to be developed over time; intermittent interprofessional interventions during the three-year period was found to be inadequate, and the tutor role is essential in order to support the students' learning process. Page6 Jefferson InterProfessional Education Center Bibliography – January 2009 Blackburn, K. (2005). Dietetics professionals' role in the changing face of america's health care: The chronic care model. Journal of the American Dietetic Association, 105(3), 346-346-347. This article describes the Chronic Care Model and Chronic Care Improvement Programs how dietetics professionals can utilize these in their profession. As Congress has recognized medical nutrition therapy as a component of Chronic Care Improvement Programs, new opportunities are available to dietetics professionals. Bleakley, A. (2006). Broadening conceptions of learning in medical education: The message from team working. Medical Education, 40, 150-150-157. This paper addresses the limitations of the current dominant learning theories which inform medical education. It discusses how sociocultural learning theories may offer a best-fit exploration and explanation of learning. Finally, it is emphasized that it will be increasingly important to have a range of theories to draw from when considering medical education. Bleakley, A. (2006). A common body of care: The ethics and politics of teamwork in the operating theater are inseparable. Journal of Medicine and Philosophy, 31, 305-305-322. Interpersonal communication is a key element to patient safety, knowledge, and skills in the operating theater. As times change from an era of "professionalism" to one of "interprofessionalism", it will be important to consider a virtue ethics framework to inform practice. Bleakley, A., Boyden, J., Hobbs, A., Walsh, L., & Allard, J. (2006). Improving teamwork climate in operating theatres: The shift from multiprofessionalism to interprofessionalism. Journal of Interprofessional Care, 20(5), 461-461-470. This article discusses the importance of changing teamwork climates as a means to establish an interprofessional teamwork culture. This idea is explored through a longitudinal and prospective collaborative inquiry with one half of the cohort of operating theater personnel serving a rural population in 2002. The other half of the cohort was introduced to this inquiry in 2004. Blum, R. H., Raemer, D. B., Carroll, J. S., Dufresne, R. L., & Cooper, J. B. (2005). A method for measuring the effectiveness of simulation-based team training for improving communication skills. Anesthesia & Analgesia, 100(5), 1375-1375-1380. Team behavior and coordination, particularly communication or team information-sharing, are critical for optimizing team performance. This study developed a technique for placing clinical information with members of a team of trainees in a controlled simulator setting. Despite the low level of team information-sharing, the authors demonstrated construct validity of the probe methodology. Bodenheimer, T. (2005). Planned visits to help patients self-manage chronic conditions (comment). American Family Physician, 72(8), 1503-1503-1510. This article explains the benefit of planned visits on patient self-management. At mutiple-agenda visits, there is not enough time to provide information and engage in decision making, and this time is often trumped by acute problems. Planned visits offer a single agenda geared to patient selfmanagement and education. Bodenheimer, T., Lorig, K. H., H., & Grumbach, K. (2002). Patient self-management of chronic disease in primary care. Journal of American Medical Association, 288(19), 2469-2469-2475. A central concept in self-management is self-efficacy -confidence to carry out a behavior necessary to reach a desired goal. Self-efficacy is enhanced when patients succeed in solving patient-identified problems. Evidence from controlled clinical trials suggests that programs teaching self-management skills are more effective than information from solely patient education when considering improving clinical outcomes. In some circumstances, self-management education improves outcomes and can reduce costs for arthritis and probably for adult asthma patients. A self-management education program bringing together patients with a variety of chronic conditions may improve outcomes and reduce costs. Self-management education for chronic illness may soon become an integral part of high-quality primary care. Page7 Jefferson InterProfessional Education Center Bibliography – January 2009 Bodenheimer, T., MacGregor, K., & Stothart, N. (2005). Nurses as leaders in chronic care. British Medical Journal, 330(7492), 612-612-613. This article provides support for the pivotal role of nurses in interprofessional care. Bodenheimer, T. (2007). A 63-year-old man with multiple cardiovascular risk factors and poor adherence to treatment plans. JAMA : The Journal of the American Medical Association, 298(17), 2048-2055. doi:10.1001/jama.298.17.2048 Mr P has long-standing hypertension, obesity, and diabetes mellitus and has experienced lifethreatening cardiovascular events. Mr P is receiving evidence-based clinical care but has adhered to his medical regimen poorly and remains at considerable risk of future catastrophic cardiovascular events. Practicing evidence-based medicine should be a 5-step process: research uncovers the evidence, clinicians learn the evidence, clinicians use the evidence at every visit for every patient, clinicians make sure patients understand the evidence, and clinicians help patients incorporate the evidence into their lives. Research demonstrates, however, that clinicians do not use the evidence at every visit, patients may misunderstand what took place in the visit, and clinicians are not always effective in helping patients incorporate the evidence into their lives. These failures reflect the difficulty faced by clinicians attempting to address multiple issues while providing sufficient information and engaging in collaborative decision making during a brief clinical visit. Bodenheimer, T., Wagner, E. H., & Grumbach, K. (2002). Improving primary care for patients with chronic illness. JAMA : The Journal of the American Medical Association, 288(14), 1775-1779. The chronic care model is a guide to higher-quality chronic illness management within primary care. The model predicts that improvement in its 6 interrelated components-self-management support, clinical information systems, delivery system redesign, decision support, health care organization, and community resources-can produce system reform in which informed, activated patients interact with prepared, proactive practice teams. Case studies are provided describing how components of the chronic care model have been implemented in the primary care practices of 4 health care organizations. Bokhour, B. (2006). Communication in interdisciplinary team meetings: What are we talking about? Journal of Interprofessional Care, 20(4), 349-349-363. This study examines professional communication practices in interdisciplinary team meetings, a common forum for discussing patient care.Two teams at a long-term care facility specializing in patients with Alzheimer's participated in this qualitative, exploratory study. Through detailed discourse analysis of transcripts of the meetings, the authors identified three different communication practices in team meetings: giving report, writing report, and collaborative discussion. Only the latter practice met the goals indicated by the team members to coordinate and make joint decisions about patient care and allowed for team members to collaboratively solve problems. Bower, P., & Rowland, N. (2006). Effectiveness and cost effectiveness of counselling in primary care. Cochrane Database of Systematic Reviews (Online), 3, CD001025. doi:10.1002/14651858.CD001025.pub2 BACKGROUND: The prevalence of mental health and psychosocial problems in primary care is high. This review examines the clinical and cost-effectiveness of psychological therapies provided in primary care by counsellors. OBJECTIVES: To assess the effectiveness and cost effectiveness of counselling in primary care by reviewing cost and outcome data in randomised controlled trials for patients with psychological and psychosocial problems considered suitable for counselling. SEARCH STRATEGY: To update the review, the following electronic databases were searched on 25-102005: MEDLINE, EMBASE, PsycLIT, CINAHL, the Cochrane Controlled Trials register and the Cochrane Collaboration Depression, Anxiety and Neurosis (CCDAN) trials registers. SELECTION CRITERIA: All controlled trials comparing counselling in primary care with other treatments for patients with psychological and psychosocial problems considered suitable for counselling. Trials completed before the end of June 2005 were included in the review. DATA COLLECTION AND ANALYSIS: Data were extracted using a standardised data extraction sheet. Trials were rated for Page8 Jefferson InterProfessional Education Center Bibliography – January 2009 quality using CCDAN criteria, to assess the extent to which their design and conduct were likely to have prevented systematic error. Continuous measures of outcome were combined using standardised mean differences. An overall effect size was calculated for each outcome with 95% confidence intervals (CI). Continuous data from different measuring instruments were transformed into a standard effect size by dividing mean values by standard deviations. Sensitivity analyses were undertaken to test the robustness of the results. Economic analyses were summarised in narrative form. MAIN RESULTS: Eight trials were included in the review. The analysis found significantly greater clinical effectiveness in the counselling group compared with usual care in the short-term (standardised mean difference -0.28, 95% CI -0.43 to -0.13, n = 772, 6 trials) but not the long-term (standardised mean difference -0.09, 95% CI -0.27 to 0.10, n = 475, 4 trials). Levels of satisfaction with counselling were high. There was some evidence that the overall costs of counselling and usual care were similar. AUTHORS' CONCLUSIONS: Counselling is associated with modest improvement in short-term outcome compared to usual care, but provides no additional advantages in the longterm. Patients are satisfied with counselling. Although some types of health care utilisation may be reduced, counselling does not seem to reduce overall healthcare costs. Boyd, C. M., Darer, J., Boult, C., Fried, L. P., Boult, L., & Wu, A. W. (2005). Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: Implications for pay for performance. (see comment). Journal of the American Medical Association, 294(6), 741-741-743. This article discusses a study conducted to evaluate the applicability of Clinical Practice Guidelines (CPGs) to the care of older individuals with several comorbid diseases. This review suggests that adhering to current CPGs in caring for an older person with several comorbidities may have undesirable effects. Brehm, J. G. (2004). Medical education and chronic disease. (comment). Journal of the American Medical Association, 292(24), 2975-2975-2976. Dr. Brehm comments on a commentary by Dr. Holman in JAMA regarding a gap in the current training and practice of physicians. He raises a related problem, the role of the payment system and its subsequent impact on the problem. Brems, C., Johnson, M. E., Warner, T. D., & Roberts, L. W. (2006). Barriers to healthcare as reported by rural and urban interprofessional providers. Journal of Interprofessional Care, 20(2), 105-105-118. This article reviews a study conducted in Alaska and New Mexico on barriers to care in rural areas. Findings confirm that rural areas struggle with more barriers than urban or small urban areas, particularly related to resource limitations, confidentiality, overlapping roles, travel distance, access to services and training. Britto, M. T., DeVellis, R. F., Hornung, R. W., DeFriese, G. H., Atherton, H. D., & Slap, G. B. (2004). Health care preferences and priorities of adolescents with chronic illnesses. Pediatrics, 114(5), 1272-1272-1280. This study sought to develop a measure of health care preferences of adolescents with chronic illnesses and to determine demographic, developmental, and health factors associated with adolescents' preferences. A questionnaire and survey were administered. Participants rated aspects of interpersonal care as most important in their judgments of quality. In addition, technical aspects of care were also rated highly. Brooker, C., & Curran, J. (2006). The national continuous quality improvement tool for mental health education: Result of targeted and supported implementation in england. Journal of Interprofessional Care, 20(3), 276-276-289. The national continuous quality assurance tool for mental health education and training has recently been developed. This paper describes the planned implementation of the tool across NHS Workforce Development Confederations (WDCs) in England. Large stakeholder groups in 15 WDCS were convened. The groups rated 29 programmes across a range of provisions including prequalifying programmes (social work and mental health nursing), post-qualifying programmes, new graduate mental health worker programmes and programmes run within NHS Trusts. Overall, the Page9 Jefferson InterProfessional Education Center Bibliography – January 2009 results indicate that the majority of rated programmes are relevant to the policy agenda and involve service users in a meaningful way. However, courses are less likely to engage with carers and to assess the impact of the programmes. Key factors are identified that promote the implementation of the new quality assurance tool and key barriers to implementation are also elicited. The paper concludes that the tool can provide a useful framework to assess the quality of a broad range of mental health education, furthermore, that it should be incorporated into existing quality assurance systems. Browning, D. M., Solomon, M. Z., & for the Initiative for Pediatric Palliative Care (IPPC) Investigator Team. (2005). The initiative for pediatric palliative care: An interdisciplinary educational approach for healthcare professionals. Journal of Pediatric Nursing, 20(5), 326-334. doi:10.1016/j.pedn.2005.03.004 There is growing empirical evidence that the U.S. healthcare system fails to meet the needs of children with life-threatening conditions and their families. The confluence of several recent developments has created a critical window of opportunity for improving clinical practice and institutional effectiveness in pediatric palliative care. This article presents an innovative, comprehensive approach to pediatric palliative care education that was developed by the Initiative for Pediatric Palliative Care, a consortium of seven academic children's hospitals, Education Development Center, the National Association of Children's Hospitals and Related Institutions, the New York Academy of Medicine, the Society of Pediatric Nursing, and the Association of Medical School Pediatric Department Chairs. The approach is based on needs assessment research with clinicians and parents and reflects a commitment to culturally respectful, family-centered care of children with life-threatening conditions. The pedagogy combines principles of adult education, includes families as teachers, and integrates affective and cognitive dimensions to enhance learning. Calvin, J. E. (2007). Improving outpatient care in chronic cardiac disease: No easy solutions. (comment). American Heart Journal, 151(1), 1-1-3. This editorial discusses the focus of quality improvement methods in cardiology and the current aims of quality healthcare delivery systems. Carlisle, C., Cooper, H., & Watkins, C. (2004). "Do none of you talk to each other?": The challenges facing the implementations of interprofessional education. Medical Teacher, 26(6), 545-545-552. The aim of this study was to explore the feasibility of introducing interprofessional education (IPE) within undergraduate health professional programs. This paper discusses and reports findings from focus-group interviews. There was an overall consensus that IPE had potential to break down barriers to team working. Carpenter, J., Barnes, D., Dickinson, C., & Wooff, D. (2006). Outcomes of interprofessional education for community mental health services in england: The longitudinal evaluation of a postgraduate programme. it concludes that a well-designed IPE program can help students in obtaining knowledge and skills and implementing these in their workplace. Journal of Interprofessional Care, 20(2), 145-145-161. This article provides an evaluation of a two-year longitudinal post-graduate program designed to enable health and social care providers to work together to deliever community mental health services. Carty, A. E., & Day, S. S. (1993). Interdisciplinary care. effect in acute hospital setting. Journal of Gerontological Nursing, 19(3), 22-32. The Senior Care Unit was developed to meet the needs of hospitalized elderly patients. Nurses assumed leadership roles as members of an interdisciplinary care team that also included representatives from medical, social work, dietary, physical therapy, and pharmacy departments. This collaborative effort not only resulted in a more complete holistic plan of care for the patient, but also increased the nurses' and other team members' knowledge of each other's areas of expertise. This project demonstrated that it is feasible to introduce a comprehensive, interdisciplinary geriatric Page10 Jefferson InterProfessional Education Center Bibliography – January 2009 team coordinated by the nurses into an existing staff, resulting in quality care without increasing the length of stay or hospital costs. Casalino, L. P. (2005). Disease management and the organization of physician practice. The Journal of the American Medical Association, 293(4), 485-485-488. What physicians do for patients with chronic disease and what they should do vary greatly. Disease management and the chronic care model are two models used to address this "quality chasm" in outpatient care. The Center for Medicare and Medicaid Services (CMS) will begin an initiative to address this problem by bringing to light the two models to make an impact on physician practice and patient care. Catty, J., Burns, T., Knapp, M., Watt, H., Wright, C., Henderson, J., et al. (2002). Home treatment for mental health problems: A systematic review. Psychological Medicine, 32(3), 383-401. BACKGROUND: Concerns have been raised about the scope and generalizability of much community mental health research. In particular, both experimental and control services are poorly characterized. METHODS: To review the effectiveness of 'home treatment' for mental health problems in terms of hospitalization, we conducted a systematic review, using Cochrane methodology but with a wider remit. Non-randomized studies were included in response to concerns about RCTs' generalizability. All authors were followed up for data on service components. 'Home treatment' was defined broadly for the purposes of the literature search, but included studies were then assessed against service components specifically focused on delivering treatment at home. The study tested components and other features for associations with days in hospital, as well as conducting a conventional meta-analysis of data on days in hospital. RESULTS: We found 91 studies, 18 comparing home to in-patient treatment. Sixty per cent of authors responded to followup. The vast majority of the services studied had a 'home treatment function' and regularly visited patients at home. The heterogeneity of control services made meta-analysis problematical as did the limited availability of data. There was some evidence that 'regular' home visiting and combined responsibility for health and social care were associated with reduced hospitalization. The inclusion of non-randomized studies rarely affected the findings. CONCLUSIONS: Evidence concerning the effectiveness of home treatment remains inconclusive. A centrally coordinated research strategy is recommended, with attention to study design. Experimental and control service components should be prospectively recorded and reported to enable meaningful analysis. Catty, J. S., Bunstead, Z., Burns, T., & Comas, A. (2007). Day centres for severe mental illness. Cochrane Database of Systematic Reviews (Online), (1)(1), CD001710. doi:10.1002/14651858.CD001710.pub2 BACKGROUND: The number of people with severe mental illness who receive treatment whilst living at home has increased greatly over the last 30 years. Day centres and day hospitals frequently supplement this treatment. OBJECTIVES: To determine the effects of non-medical day centre care for people with severe mental illness. SEARCH STRATEGY: We updated our search in September 2005. All databases and searches are detailed in the body of the text. SELECTION CRITERIA: We would have included all randomised controlled trials where seriously mentally ill people were allocated to non-medical day centre care. DATA COLLECTION AND ANALYSIS: We reliably selected studies, quality rated them and extracted data. For dichotomous data, it had been hoped to estimate the fixed effects Relative Risk (OR) with 95% confidence intervals (CI) and the number needed to treat statistic (NNT). Analysis was to have been by intention-to-treat. Normal continuous data were to have been summated using the weighted mean difference (WMD) and scale data presented only for those tools that had attained pre-specified levels of quality. MAIN RESULTS: Electronic searches identified over 300 citations but none were relevant to this review. We found no trials of non-medical day centres. AUTHORS' CONCLUSIONS: We feel that the inclusion of any studies less rigorous than randomised trials would result in misleading findings and that it is not unreasonable to expect well designed, conducted and reported randomised controlled trials of day centre care. More precise nomenclature would greatly help identify relevant work. At present nonrandomised comparative studies give conflicting messages about the roles provided by day centres and the clinical and social needs they are able to meet. It is therefore probably best that people with Page11 Jefferson InterProfessional Education Center Bibliography – January 2009 serious mental illness and their carers, if given the choice, take a pragmatic decision on which type of unit best meets their needs. There is a clear need for randomised controlled trials of day centre care compared to other forms of day care, and when resources are limited, day centre care within the context of a pragmatic randomised trial may be the only way of ensuring equity of provision. Challis, D., Stewart, K., Donnelly, M., Weiner, K., & Hughes, J. (2006). Care management for older people: Does integration make a difference? Journal of Interprofessional Care, 20(4), 335-335-348. This paper examines whether integrated structures appear to impact upon the operation of care management, a key approach to providing coordinated care for vulnerable older people. It is concluded that further investigation is required as to the extent to which integrated structures have impacted upon patterns of professional working and underlying beliefs about roles. Chan, S., Siu, A., Poon, P., & Chan, C. (2005). Chronic disease self-management program for chinese patients: A preliminary multi-baseline study. International Journal of Rehabilitation Research, 28(4), 351-351-354. This study reports the preliminary findings on the effects of the Chronic Disease Self-management Program on a group of Chinese participants who suffered from chronic diseases. A total of 23 participants were recruited in a multi-baseline study protocol. Their self-management behaviors, selfefficacy and health status were captured over three baseline assessments and one post-test assessment. The results indicated significant increases in the performance of stretching exercises, the management of cognitive symptoms and communication with physicians. Their self-efficacy in terms of these aspects was found to be significantly increased. However, changes in other aspects of self-management which required more special skills and coordination with outside agencies were not significant. The changes in the physical and mental statuses of the participants were also not significant. It was observed that the positive effects of the program could be attributed to traditional Chinese beliefs of 'self-discipline' and a welcoming response towards self-efficacy strategies. Further studies should adhere to standards of a randomized clinical trial and further examine the mechanisms underpinning the changes in self-management behaviors among Chinese people with chronic diseases. Chang, E., Hancock, K., Harrison, K., Daly, J., Johnson, A., Easterbrook, S., et al. (2005). Palliative care for end-stage dementia: A discussion of the implications for education of health care professionals. Nurse Education Today, 25(4), 326-332. doi:10.1016/j.nedt.2005.02.003 The increasing burden of chronic disease demands that palliative care clinicians address the needs of patients with non-malignant disease. This discussion document seeks to address some of the challenges to providing palliative care for end-stage dementia (ESD) and the need for skill enhancement in key providers of care. In spite of the intent, there is an apparent lack of appropriate, co-ordinated and comprehensive palliative care available for these individuals and their families. There is an absence of well-articulated models to assist health care providers of ESD clients. It would appear that the development and evaluation of guidelines, implementation of education programs and collaborative associations between palliative and aged-care providers of care are key strategies to facilitate palliative care for ESD clients. Charles, G., Bainbridge, L., Copeman-Stewart, K., Art, S. T., & Kassam, R. (2006). The interprofessional rural program for british columbia (IRPbc). Journal of Interprofessional Care, 20(1), 40-40-50. The Interprofessional Rural Program of British Columbia IRPbc was established in 2003 as an important first step for the Province of British Columbia, Canada, in creating a collaborative interprofessional education initiative that engages numerous communities, health authorities and post-secondary institutions in working toward a common goal. Designed to foster interprofessional education and promote rural recruitment of health professionals, the program places teams of students from a number of health professional programs into rural and remote British Columbia communities. In addition to meeting their discipline specific learning objectives, the student teams are provided with the opportunity to experience the challenges of rural life and practice and advance their interprofessional competence. To date, 62 students have participated in the program from nursing, social work, medicine, physical therapy, occupational therapy, pharmaceutical sciences, Page12 Jefferson InterProfessional Education Center Bibliography – January 2009 speech language pathology, audiology, laboratory technology, and counseling psychology. While not without numerous struggles and challenges, IRPbc has been successful in meeting the program mandate. It has also had a number of positive outcomes not anticipated at the time the program was established. The chronic care model :: Improving chronic illness care. Retrieved 10/31/2008, 2008, from http://www.improvingchroniccare.org/index.php?p=The_Chronic_Care_Model&s=2 This website provides information on the Chronic Care Model, topics include the Health System, Delivery System Design, Decision Support, Clinical Information Systems, Self-Management Support, and The Community. Clar, C., Waugh, N., & Thomas, S. (2007). Routine hospital admission versus out-patient or home care in children at diagnosis of type 1 diabetes mellitus. Cochrane Database of Systematic Reviews (Online), (2)(2), CD004099. doi:10.1002/14651858.CD004099.pub2 BACKGROUND: In many places, children newly diagnosed with type 1 diabetes mellitus are admitted to hospital for metabolic stabilisation and training, even if they are not acutely ill. Outpatient or home based management of these children could avoid the stress associated with a hospital stay, could provide a more natural learning environment for the child and its family, and might reduce costs for both the health care system and the families. OBJECTIVES: To assess the effects of routine hospital admission compared to out-patient or home-based management in children newly diagnosed with type 1 diabetes mellitus. SEARCH STRATEGY: We searched The Cochrane Library, MEDLINE, EMBASE, CINAHL, and the British Nursing Index. Additionally, we searched reference lists of relevant studies identified and contacted one of the trialists about further studies. SELECTION CRITERIA: Comparative studies of initial hospitalisation compared to homebased and/or out-patient management in children with newly diagnosed type 1 diabetes. DATA COLLECTION AND ANALYSIS: Studies were independently selected by two reviewers. Data extraction and quality assessment of trials were done independently by two reviewers. Authors of included studies were contacted for missing information. Results were summarised descriptively, using tables and text. MAIN RESULTS: Seven studies were included in the review, including a total of 298 children in the out-patient/home group. The one high quality trial identified suggested that home-based management of children with newly diagnosed type 1 diabetes may lead to slightly improved long term metabolic control (at two and three years follow-up). No differences between comparison groups were found in any of the psychosocial and behavioural variables assessed or in rates of acute diabetic complications within two years. Parental costs were found to be decreased, while health system costs were increased, leaving total social costs virtually unchanged. None of the other studies assessing metabolic control found a difference between the comparison groups. There seemed to be no differences in hospitalisations or acute diabetic complications between the outpatient/home groups and the hospital groups. AUTHORS' CONCLUSIONS: Due to the generally low quality or limited applicability of the studies identified, the results of this review are inconclusive. On the whole, the data seem to suggest that where adequate out-patient/home management of type 1 diabetes in children at diagnosis can be provided, this does not lead to any disadvantages in terms of metabolic control, acute diabetic complications and hospitalisations, psychosocial variables and behaviour, or total costs. Clark, P. G. (2006). What would a theory of interprofessional education look like? some suggestions for developing a theoretical framework for teamwork training 1. Journal of Interprofessional Care, 20(6), 577-577-589. Currently, much of the literature available on interprofessional education (IPE) is descriptive and atheoretical. To advance practice and research in the field it will be important to develop theoretical frameworks. This article discusses the role that theory might play in advancing IPE and then discusses 5 different approaches for guidance in developing an IPE framework. Cole, M. G., McCusker, J., Elie, M., Dendukuri, N., Latimer, E., & Belzile, E. (2006). Systematic detection and multidisciplinary care of depression in older medical inpatients: A randomized trial. Canadian Medical Association Journal, 174(1), 38-38-44. Page13 Jefferson InterProfessional Education Center Bibliography – January 2009 This article discusses a study that was conducted to evaluate the effectiveness of a strategy of systemic detection and multidisciplinary treatment of depression in older medical inpatients. Coleman, M. T., & Newton, K. S. (2005). Supporting self-management in patients with chronic illness (see comment). (review). American Family Physician, 72(8), 1503-1503-1510. This article reviews literature which discusses the support of patient self-management of chronic illnesses. This support includes: processes that develop problem-solving skills, self-efficacy, and the application of knowledge in real life situations that matter to patients. Emerging evidence supports the implementation of practice strategies that are conducive to patient self-management and improved patient outcomes among chronically ill patients. Cook, D. A. (2005). Models of interprofessional learning in canada. Journal of Interprofessional Care, 19(Supplement 1), 107-107-115. This article provides an overview of interprofessional education in Canada and models that are currently being employed. It also discusses the idea that the lack of convincing evidence of the effectiveness of existing programs is the most serious problem for the expansion of interprofessional education. The most frequently utilized model involves a mandatory experience, which is casebased, and involves all the students registered in health faculties. Cooke, M., Irby, D. M., Sullivan, W., & Ludmerer, K. M. (2006). American medical education 100 years after the flexner report. The New England Journal of Medicine, 355(13), 1339-1344. doi:10.1056/NEJMra055445 In this article, which introduces a new series on medical education in the Journal, we summarize the changes in medical education over the past century and describe the current challenges, using as a framework the key goals of professional education: to transmit knowledge, to impart skills, and to inculcate the values of the profession. Cooper, H., & Spencer-Dawe, E. (2006). Involving service users in interprofessional education narrowing the gap between theory and practice. Journal of Interprofessional Care, 20(6), 603-603-617. his paper reports findings from an evaluation which focused on narrowing the gap between theory and practice. Findings showed that service users can make an important contribution to IPE for health and social care students in the early stages of their training. By exposure to a service user perspective, first year students can begin to learn and apply the principles of team work, to place the service user at the center of the care process, to make connections between theory and "real life" experiences, and to narrow the gap between theory and practice. Findings also revealed benefits for facilitators and service users. Copperman, J., & Newton, P. (2005). Scoping interprofessional education and training in north east london. Journal of Interprofessional Care, 19(5), 523-523-525. In investigating why uptake of interprofessional course offerings at City University was low among social work students, the authors discovered wider issues affecting interprofessional working. These issues related to funding, organization and practicality of interprofessional work. Cox, P. (2005). Managing chronic diseases: Palliative care spectrum starts early on. (comment). British Medical Journal, 330(7492), 611-611-612. This article describes palliative care as a spectrum which begins at the time of diagnosis, not just when the patient begins dying. Palliation becomes a partnership between patient and physician. The length of palliative treatment can vary and can be stopped by the physician or the patient. When death becomes close palliative care becomes terminal care, a relationship of understanding will have already been formed between doctor and patient Page14 Jefferson InterProfessional Education Center Bibliography – January 2009 Cullen, T. (2004). The chronicity of chronic disease [a piece of mind]. The Journal of the American Medical Association, 291(6), 671-671-672. This article is a narrative describing a mother and her son's struggles with severe, persistent asthma. Curran, V. R., Deacon, D. R., & Fleet, L. (2005). Academic administrators' attitudes towards interprofessional education in canadian schools of health professional education. Journal of Interprofessional Care, 19(Supplement 1), 76-76-86. The introduction and successful implementation of the interprofessional education approach is dependent on a variety of factors, including the attitudes of students, faculty, senior academic administrators and practitioners. The purpose of this study was to examine attitudes towards interprofessional teamwork and interprofessional education amongst academic administrators of post secondary health professional education programs in Canada. A web-based questionnaire was distributed via e-mail. Curran, V. R., Sharpe, D., & Forristall, J. (2007). Attitudes of health sciences faculty members towards interprofessional teamwork and education. Medical Education, 41(9), 892-896. doi:10.1111/j.13652923.2007.02823.x OBJECTIVES: Faculty attitudes are believed to be a barrier to successful implementation of interprofessional education (IPE) initiatives within academic health sciences settings. The purpose of this study was to examine specific attributes of faculty members, which might relate to attitudes towards IPE and interprofessional teamwork. METHODS: A survey was distributed to all faculty members in the medicine, nursing, pharmacy and social work programmes at our institution. Respondents were asked to rate their attitudes towards interprofessional health care teams, IPE and interprofessional learning in an academic setting using scales adopted from the peer-reviewed literature. Information on the characteristics of the respondents was also collected, including data on gender, prior experience with IPE, age and years of practice experience. RESULTS: A total response rate of 63.0% was achieved. Medicine faculty members reported significantly lower mean scores (P < 0.05) than nursing faculty on attitudes towards IPE, interprofessional teams and interprofessional learning in the academic setting. Female faculty and faculty who reported prior experience in IPE reported significantly higher mean scores (P < 0.05). Neither age, years of practice experience nor experience as a health professional educator appeared to be related to overall attitudinal responses towards IPE or interprofessional teamwork. CONCLUSIONS: The findings have implications for both the advancement of IPE within academic institutions and strategies to promote faculty development initiatives. In terms of IPE evaluation, the findings also highlight the importance of measuring baseline attitudinal constructs as part of systematic evaluative activities when introducing new IPE initiatives within academic settings. Daaleman, T. P. (2006). Reorganizing medicare for older adults with chronic illness. Journal of the American Board of Family Medicine : JABFM, 19(3), 303-309. A major challenge for the US health care system during coming years will be the financial viability and reorganization of Medicare--a program in which over 90% of family physicians participate. Although chronic illness constitutes a trajectory characterized by long-term patterns of health and functional states, fee-for-service Medicare is largely directed to the treatment of acute, episodic illness. Beyond the prescription drug benefit, there were several provisions in the Medicare Prescription Drug Improvement and Modernization Act of 2003 that were designed to improve the quality of care and reduce costs for chronically ill beneficiaries, an important first step in the reorientation of Medicare to chronic illness care. Quality is the foundation of Medicare's movement to a chronic care program and paying physicians for quality care is on the horizon. Family physicians will need to be actively engaged in Medicare's reorientation by articulating and promoting a quality of care that effectively integrates evidence-based medicine with a person-centered focus. D'Amour, D., Ferrada-Videla, M., Martin-Rodriguez, L. S., & Beaulieu, M. D. (2005). The conceptual basis for interprofessional collaboration: Core concepts and theoretical frameworks. Journal of Interprofessional Care, 19(Supplement 1), 116-116-131. The goal of this literature review was to identify conceptual frameworks that could increase an Page15 Jefferson InterProfessional Education Center Bibliography – January 2009 understanding of interprofessional collaboration and interprofessional relationships within health care organizations. Definitions and theoretical frameworks were explored in an effort to discover underlying concepts of collaboration and theoretical frameworks utilized. D'Amour, D., & Oandasan, I. (2005). Interprofessionality as the field of interprofessional practice and interprofessional education: An emerging concept. Journal of Interprofessional Care, 19(Supplement 1), 8-8-20. This paper introduces the concept of "interprofessionality" and contrasts this concept with the idea of "interdisciplinarity". "Interdisciplinarity" concerns the development of integrated knowledge in response to fragmented disciplinary knowledge. "Interprofessionality" concerns the processes and determinants that influence interprofessional education initiatives as well as determinants and processes inherent to interprofessional collaboration. Darer, J. D., Hwang, W., Pham, H. H., Bass, E. B., & Anderson, G. (2004). More training needed in chronic care: A survey of U.S. physicians. Journal of the Association of American Medical Colleges, 79(6), 541-541-548. Physicians' perceptions with respect to their chronic care training was evaluated through interviews. Most physicians reported inadequate training in chronic disease and believe that proper training has a positive effect on their attitudes towards people with chronic diseases. Darren, A., DeWalt, D., Pignone, M., Malone, R., Rawls, C., Kosnar, M. C., et al. (2004). Development and pilot testing of a disease management program for low-literacy patients with heart failure. Patient Education and Counseling, 55, 78-78-86. Randomized trials have shown that disease management programs can reduce hospitalizations and improve symptoms for patients with CHF. The authors sought to create and pilot test such a program for patients with low literacy skills. It was found that a heart failure disease management program designed specifically for patients with low literacy skills is acceptable and is associated with improvements in self-care behavior and heart failure related symptoms. Dartmouth Atlas Project. (2006). The care of patients with severe chronic illness: A report on the medicare program by the dartmouth atlas project (Executive Summary. Hanover NH: Center for the Evaluative Clinical Sciences. The reallocation of resources from the acute care sector to create a population-based communitywide integrated system from managing severe chronic illness is today only a thought experiment. It should become a national goal. the benchmarks from efficient practice indicate that Medicare already invests more than enough money to build and maintain such a system. The problem is that the resources are now largely locked in by Medicare's reimbursement policy. Davis, B. E., Nelson, D. B., Sahler, O. J., McCurdy, F. A., Goldberg, R., & Greenberg, L. W. (2001). Do clerkship experiences affect medical students' attitudes toward chronically ill patients? Academic Medicine : Journal of the Association of American Medical Colleges, 76(8), 815-820. PURPOSE: To measure changes in medical students' attitudes toward chronically ill patients, and to identify experiences, specifically during clerkships, that contributed to students' attitudes. METHOD: A cohort of students from five U.S. medical schools voluntarily participated in three surveys longitudinally administered before and after required clinical rotations. The first two questionnaires were identical and asked for demographic information and pre-matriculation experiences with chronically ill patients. The third was modified to include questions about clinical experiences with chronically ill patients. Responses from the first and third questionnaires were linked for analysis. RESULTS: A total of 502 of 695 students (69%) completed both the first and the third questionnaires. Many students (36%) had had pre-matriculation experiences with chronic illness. After clinical training, 25% of the respondents stated that they would seek another career specialty if the incidence of chronically ill patients increased in their chosen field, compared with the 9% who responded so before clinical training (p <.001). While 73% of the students had favorable perceptions toward chronically ill patients, and 91% felt involved in care, significantly fewer students (p <.01) had had positive patient care experiences when working with residents (57%) and attendings (59%). Page16 Jefferson InterProfessional Education Center Bibliography – January 2009 Gender, age, prior experiences, and school site were not associated with attitudinal changes. CONCLUSION: Students begin medical school with positive attitudes toward caring for chronically ill patients, but this perception depreciates with clinical experience, which may affect specialty decisions. Contributing factors may include adequate role modeling by residents and attendings and a perceived discrepancy in the quality of care patients receive. Davis, M. P., Albert, N. M., & Young, J. B. (2005). Palliation of heart failure. The American Journal of Hospice & Palliative Care, 22(3), 211-222. Heart failure is the major cause of morbidity and mortality in the United States. Stage D heart failure has a greater mortality rate than many cancers and has equivalent symptom burden and severity. There has been a paradigm shift in our understanding of the pathophysiology of heart failure. Progressive heart failure is associated with ventricular remodeling and a maladaptive neurohumoral response. Drug classes have evolved that curtail ventricular remodeling, and blunt neurohumoral responses reduce morbidity and mortality. Despite combination drug and device therapies, the management of Stage D heart failure includes palliation. Both cardiology and palliative specialists need to learn from one another in order to palliate these highly symptomatic patients. Such collaboration will enhance care and are the basis for well-conceived research trials. Davis, T. K., Montford, C. R., & Read, C. (2005). Interdisciplinary teamwork in a school-based health center. The Nursing Clinics of North America, 40(4), 699-709, x. doi:10.1016/j.cnur.2005.07.002 The goal of school-based health centers (SBHCs) is to provide culturally competent primary, preventive, and mental health care services for students who otherwise may not have access to care. Often, an SBHC is the primary health care provider for students because many adolescents are uninsured or lack access to other health care service providers. At other times, the SBHC works in collaboration with primary care providers and other health professionals to provide health care services for students and their families. Complex health and social problems and changes in professional practice make it impossible to serve clients effectively without collaborating with professionals from other disciplines. One process used in SBHCs to assure that students' needs and concerns are addressed is an interdisciplinary case review (ICR). The ICR is a method of evaluating complex cases with members of the health care team to ensure that the physical and mental health and social needs of students are meeting or exceeding the standard of care. Davoli, G. W., & Fine, L. J. (2004). Stacking the deck for success in interprofessional collaboration. Health Promotion Practice, 5(3), 266-266-270. This article discusses the importance of interprofessional collaboration as educators, health professionals, and social service providers focus more on health promotion and illness prevention. Key concepts associated with the early stages of collaboration are forming group identity and weathering conflicts associated with task and personnel issues. De Brantes, F., Gosfield, A. G., McGlynn, E., Rosenthal, M., & Levin-Scherz, J. (2005). Clinical practice guidelines for older patients with comorbid diseases (comment). Journal of the American Medical Association, 295(1), 34-34. The author argues that CPGs could be used to establish clinically-relevant payment systems. Payments under this system could be based on evidence-based, clinically appropriate resources and could help to eliminate both over- and under-use. Today's CPGs may not be appropriate for this type of system, but using them to establish changes for simple conditions could later pave the way toward helping those with more complex cases. D'Eon, M. (2005). A blueprint for interprofessional learning. Journal of Interprofessional Care, 19(Supplement 1), 49-49-59. This article examines several learning approaches that can help the Interprofessional Education initiative fulfill its expectations. The first approach involves the transfer of learning novel situations. The second approach emphasizes that the learning situation needs to be structured using the five elements of best-practice cooperative learning: positive interdependence, face-to-face-promotive interaction, individual accountability, interpersonal and small-group skills, and group processing. The Page17 Jefferson InterProfessional Education Center Bibliography – January 2009 third approach emphasizes that the learning process should come from an experiential learning framework. Dewitt, C., & Baldwin, J. R. (2007). Collected works on interdisciplinary and interprofessional education and practice (listed chronologically by category). Journal of Interprofessional Care, 21(Supplement 1), 108-108-112. Published papers compiled by Dewitt and Baldwin. Papers are organized by category and chronological order. Dewitt, C., & Baldwin, J. R. (2007). Some historical notes on interdisciplinary and interprofessional education and practice in health care in the USA. Journal of Interprofessional Care, 21(Supplement 1), 23-23-37. This paper describes the origins of interdisciplinary health care teams in the United States. During World War II President Johnson's vision of The Great Society helped to create multidisciplinary medical and surgical teams in community health care centers. Dickinson, A. (2006). Implementing the single assessment process: Opportunities and challenges. Journal of Interprofessional Care, 20(4), 365-365-379. The Single Assessment Process (SAP) has been introduced as part of the National Service Framework for Older People and has major implications for health and social care. The aim of this study was to evaluate a pilot introduction of the Single Assessment Process in the South-East of England. Overall the evaluation found three major themes that had an impact on the implementation of the Single Assessment Process, these were: the process of implementing policy and change, the health and social care boundary, and communication and sharing of assessments. Front-line practitioners (street-level bureaucrats) had a major impact on the SAP implementation, particularly through their reluctance to engage with the process, work together and share assessments. Dobscha, S. K., Corson, K., Hickam, D. H., Perrin, N. A., Kraemer, D. F., & Gerrity, M. S. (2006). Depression decision support in primary care: A cluster randomized trial. Annals of Internal Medicine, 145(7), 477-477-487. This article discusses a clinician-level, randomized controlled trial that analyzes the effect of a depression decision support team on individuals' depression scores and health-related quality of life. The depression decision support team consisted of a psychiatrist and a nurse. The decision support team did not improve the depression outcomes any greater than the control group. Dobson, R. T., Henry, C. J., Taylor, J. G., Zello, G. A., Lachaine, J., Forbes, D. A., et al. (2006). Interprofessional health care teams: Attitudes and environmental factors associated with participation by community pharmacists. Journal of Interprofessional Care, 20(2), 119-119-132. This study was conducted to determine if community pharmacists were prepared to assume more active roles in healthcare teams. Secondarily, it was used to collect information to develop multi-item scales for future studies involving pharmacists and other health professions. The study found that pharmacists on teams were more likely to agree that their skills and abilities prepared them for working on a team and that there was more opportunity to get to know other health disciplines. They also reported good relationships with physicians and were less likely to view other disciplines as being protective of their "turf." Dougherty, M. B., & Larson, E. (2005). A review of instruments measuring nurse-physician collaboration. The Journal of Nursing Administration, 35(5), 244-244-253. This article reviews instruments used to measure nurse-physician collaboration and compares the strengths and potential opportunities for each instrument. Dube, S. (2005). Medical education and chronic disease [letters]. Canadian Medical Association Journal, 172(7), 857-857-858. A letter in response to a commentary about the need to improve health care services for children Page18 Jefferson InterProfessional Education Center Bibliography – January 2009 with chronic health conditions. An interdisciplinary approach might help, but the medical curriculum will also need to be revised. The authors feels that faculty members are not prepared to serve as adequate role models in an interdisciplinary approach. Ducharme, A., Doyon, O., White, M., Rouleau, J. L., & Brophy, J. M. (2005). Impact of care at a multidisciplinary congestive heart failure clinic: A randomized trial. (see comment). Canadian Medical Association Journal, 173(1), 53-53-54. Multidisciplinary congestive heart failure clinics in the United States appear to be effective in reducing the number of hospital readmissions, however, it is unclear whether this is the case in countries such as Canada. This study sought to determine the impact of care at a multidisciplinary specialized outpatient congestive heart failure clinic compared with standard care. At the conclusion of the study, it was found that compared with standard care, care at a multidisciplinary specialized congestive heart failure outpatient clinic reduced the number of hospital readmissions and improved quality of life. Durbin, C. G. (2006). Team model: Advocating for the optimal method of care delivery in the intensive care unit. Critical Care Medicine, 34(3), S12-S12-S17. A review of the literature focused on published data on the team model of intensive care unit care delivery. The team model for delivery of ICU care reduces mortality, ICU length of stay, hospital length of stay, and cost of care. Current shortages of all ICU health care providers is a barrier to universal implementation of the team model. Dutton, R. P., Cooper, C., Jones, A., Leone, S., Kramer, M. E., & Scalea, T. M. (2003). Daily multidisciplinary rounds shorten length of stay for trauma patients. Journal of Trauma-Injury Infection and Critical Care, 55(5), 913-913-919. This study sought to determine whether daily multidisciplinary "discharge rounds" would improve patient flow and increase readiness. The study concluded that discharge rounds have streamlined the care of complex trauma patients. Dykes, P. C., Acevedo, K., Boldrighini, J., Boucher, C., Frumento, K., Gray, P., et al. (2005). Clinical practice guideline adherence before and after implementation of the HEARTFELT (HEART failure effectiveness & leadership team) intervention. The Journal of Cardiovascular Nursing, 20(5), 306314. HEART Failure Effectiveness & Leadership Team (HEARTFELT) is a multifaceted intervention designed to improve adherence with the American College of Cardiology/American Heart Association practice guidelines for heart failure (HF). The purpose of this study was to assess differences in clinician adherence with clinical practice guidelines before and after implementation of HEARTFELT. A quasi-experimental, untreated control group design with separate pretest/posttest samples was employed at a community hospital in Connecticut. The untreated historical control group included patients aged 65 years or older with HF and a nonequivalent comparison group of patients with stroke. The posttest samples included patients with the diagnosis of HF and stroke admitted after implementation of the HEARTFELT intervention. The HEARTFELT intervention included automated pathway in electronic medical record (order sets, interdisciplinary plan of care, self-management plan), access to evidence for clinicians and patients, HF self-management education tools, and ongoing discipline-specific feedback regarding adherence. Data were analyzed using parametric and nonparametric methods. The HEARTFELT intervention significantly improved clinician adherence with addressing all self-management categories in the electronic medical record (P = .000) and adherence with self-management education given to the patient in writing at discharge (P = .000). There were no significant differences in adherence with medical interventions (P = .39). While guideline adherence is associated with less practice variation and improved processes, methods of integration into practice in community hospital settings have been largely unexplored. The multifaceted HEARTFELT intervention is promising for its potential to integrate evidence at the point of care, to reduce unwarranted variation in practice, and ultimately to improve the outcomes of individuals with HF. Page19 Jefferson InterProfessional Education Center Bibliography – January 2009 Early Supported Discharge Trialists. (2005). Services for reducing duration of hospital care for acute stroke patients. Cochrane Database of Systematic Reviews (Online), (2)(2), CD000443. doi:10.1002/14651858.CD000443.pub2 BACKGROUND: Stroke patients conventionally receive a substantial part of their rehabilitation in hospital. Services have now been developed which offer patients in hospital an early discharge with rehabilitation at home (early supported discharge (ESD)). OBJECTIVES: To establish the effects and costs of ESD services compared with conventional services. SEARCH STRATEGY: We searched the Cochrane Stroke Group's trials register (last searched August 2004) and obtained further information from individual trialists. SELECTION CRITERIA: Randomised controlled trials recruiting stroke patients in hospital to receive either conventional care or any service intervention which has provided rehabilitation and support in a community setting with an aim of reducing the duration of hospital care. DATA COLLECTION AND ANALYSIS: Two reviewers scrutinised trials and categorised them on their eligibility. Standardised individual patient data was then sought from the primary trialists. Results were analysed for all trials and for subgroups of patients and services; in particular whether the intervention was provided by a co-ordinated multidisciplinary team (coordinated ESD team) or not. MAIN RESULTS: Outcome data are currently available for 11 trials (1597 patients). Patients tended to be a selected elderly group with moderate disability. The ESD group showed significant reductions (P < 0.0001) in the length of hospital stay equivalent to approximately 8 days. Overall, the odds ratios (OR) (95% confidence interval (CI)) for death, death or institutionalisation, death or dependency at the end of scheduled follow up were OR 0.90, 95% CI 0.64 to 1.27, P = 0.56, OR 0.74, 95% CI 0.56 to 0.96, P = 0.02 and OR 0.79, 95% CI 0.64 to 0.97, P = 0.02, respectively. The greatest benefits were seen in the trials evaluating a co-ordinated ESD team and in stroke patients with mild-moderate disability. Improvements were also seen in patients' extended activities of daily living scores (standardised mean difference 0.12, 95% CI 0.00 to 0.25, P = 0.05) and satisfaction with services (OR 1.60, 95% CI 1.08 to 2.38, P = 0.02) but no statistically significant differences were seen in carers' subjective health status, mood or satisfaction with services. AUTHORS' CONCLUSIONS: Appropriately resourced ESD services provided for a selected group of stroke patients can reduce long term dependency and admission to institutional care as well as reducing the length of hospital stay. No adverse impact was observed on the mood or subjective health status of patients or carers. Edgley, A., & Avis, M. (2006). Interprofessional collaboration: Sure start, uncertain futures. Journal of Interprofessional Care, 20(4), 433-433-435. This article reports on a study examining social barriers to successful interprofessional collaboration. The study investigated the perception of professionals about working with the Sure Start program in Nottinghamshire, UK. Sure Start is a government initiative to take on child poverty and social exclusion by providing extra provisions for families with pre-school children living in geographic areas identified as "deprived". The expectation of the program was to facilitate interprofessional collaboration through a shared agenda. Editorial.(2006). Learning in Health and Social Care, 5(4), 169-169-180. This editorial seeks to review the extent to which the journal, Learning in Health and Social Care, has contributed to issues relating to interprofessional learning. It also seeks to explore why the "forum" section of the journal, which was created for readers to make short contributions and comments, was so underutilized. Ehman, A. J. (2007). Saskatchewan successfully implementing best practices. Canadian Medical Association Journal, 176(8), 1072-1072. A quarter of family physicians in Saskatchewan volunteered to participate in an initiative to implement best practices in the treatment of diabetes and CAD. After one year, there was an increase in the number of patients receiving the recommended drugs, tests and services, and a decrease in wait time for physician appointments. The Saskatchewan Medical Association is working with the provincial government to increase physician payment for chronic disease management for those who follow best practice guidelines and report on results. Page20 Jefferson InterProfessional Education Center Bibliography – January 2009 El-Zubeir, M., Rizk, D., & Al-Khalil, R. (2006). Are senior UAE medical and nursing students ready for interprofessional learning? validating the RIPL scale in a middle eastern context. Journal of Interprofessional Care, 20(6), 619-619-632. Using a self-administered extended 29 item version of the Readiness for Interprofessional Learning Scale (RIPLS), this study examined attitudes and readiness for interprofessional education of senior medical and nursing students' from the United Arab Emirates University and Institute of Nursing. The researchers also tested the validity of the RIPLS in this Middle Eastern context. The extended RIPLS was validated for use in an undergraduate Middle Eastern community and thus provides program developers and evaluators with a useful tool to assess medical and nursing students' readiness for interprofessional learning in this context. Epping-Jordan, J. E., Galea, G., Tukuitonga, C., & Beaglehole, R. (2005). Preventing chronic disease: Taking stepwise action. (see comment). (review). Lancet, 366(9497), 1667-1667-1671. This paper presents a novel planning framework that can be used in the context of planning for the prevention of chronic disease, particularly in low-income and middle-income countries. Countries such as Indonesia, the Philippines, Tonga, and Vietnam have implemented this stepwise planning framework and their experiences helps to illustrate the applicability of the framework to solving chronic disease problems. Evans, A., Perez, I., Harraf, F., Melbourn, A., Steadman, J., Donaldson, N., et al. (2001). Can differences in management processes explain different outcomes between stroke unit and stroke-team care? Lancet, 358(9293), 1586-1592. doi:10.1016/S0140-6736(01)06652-1 BACKGROUND: Stroke units reduce mortality and dependence, but the reasons are unclear. We have compared differences in management and complications of patients with acute stroke who were admitted to a stroke unit or to a general ward as part of a previously reported randomised trial. METHODS: 304 patients had been randomly assigned to stroke units (n=152) or to general wards supported by a specialist stroke team (152). We used a structured format to gather prospective data on the frequency of prespecified interventions in each of the major aspects of stroke care. Observations were undertaken daily for the first week and every week for the next 3 months by independent observers. The effect of differences in management on outcome at 3 months was assessed with the modified Rankin score, dichotomised to good (0-3) and poor (4-6) outcome. FINDINGS: Patients in the stroke unit were monitored more frequently (odds ratio 2.1 [1.3-3.4]) and more patients received oxygen (2.0 [1.3-3.2]), antipyretics (6.4 [1.5-27.5]), measures to reduce aspiration (6.0 [2.3-15.5]), and early nutrition (14.4 [5.1-40.9]) than those in general wards. Complications were less frequent in patients in the stroke unit than those in general wards (0.6 [0.20.7]), with fewer patients having progression of stroke, chest infection, or dehydration. Measures to prevent aspiration, early feeding, stroke unit management, and frequency of complications independently affected outcome. INTERPRETATION: Differences in management and complications between the stroke unit and general wards differ substantially, even when specialist support is provided. Such differences could be responsible for the more favourable outcome seen in patients on stroke units than those on general wards. Fairbrother, P., & Mathers, N. J. (2004). Lecturer practitioners in six professions: Combining cultures. Journal of Clinical Nursing, 13(5), 539-539-546. This paper reports a study to investigate the commonalities and differences between lecturer practitioners across professions and to generate hypotheses about the role, which follows different models of practice in the different professions. An exploratory research design was utilized. All lecturer practitioners perceived a clear dichotomy between their professional practice role and their university role. Faresjo, T. (2006). Interprofessional education- to break boundaries and build bridges. Rural and Remote Health, 6(3), 602-602. Feifer, C., Mora, A., White, B., & Barnett, B. P. (2006). Challenges to improving chronic disease care and training in residencies [chronic care]. Journal of Medical Education, 81(8), 696-696-701. Page21 Jefferson InterProfessional Education Center Bibliography – January 2009 This study investigated residency-based experiences with changes in teaching and delivery of chronic disease care. Qualitative cross-sectional in-depth interviews were conducted with directors of grant-funded residency-based chronic care projects. The following challenges were identified: engaging faculty and residents who spend limited time in the practice center, institutional barriers related to authority, competing priorities, process, and resources. Successful innovations for chronic disease care and training are possible in residencies, but their implementation cannot be taken lightly. Feinberg, J. R., & Brandt, K. D. (1984). Allied health team management of rheumatoid arthritis patients. The American Journal of Occupational Therapy.: Official Publication of the American Occupational Therapy Association, 38(9), 613-620. The use of a coordinated team of allied health professionals (AHPs) to treat patients with rheumatoid arthritis assigned to experimental groups (EG) and comparison groups (CG) was assessed. The EG patients were evaluated regularly by each AHP team member, whereas CG patients were seen by AHPs only upon referral. Of the 10 EG and 13 CG patients who remained in the study for 2 years, the EG patients initially exhibited somewhat greater disease activity than CG (as reflected by erythrocyte sedimentation rate and duration of morning stiffness). After 2 years, EG patients demonstrated less disease activity than at the outset, whereas CG patients either showed little change in these parameters or deteriorated during the study. Grip strength, which was initially similar in the two groups, improved in EG patients but decreased in CG patients, so that after 2 years a significant difference was noted between the two groups (p less than .05). Tendency to lose hand range of motion was also greater in CG than in EG patients. Some EG patients showed improvement in finger flexion deformities during the study. Furthermore, EG patients showed a greater tendency to acquire positive attitudes regarding themselves and family relationships. These results suggest that ongoing "team care" may be more efficacious than episodic use of AHPs in management of patients with mild rheumatoid arthritis. Fiscella, K., & Holt, K. (2007). Impact of primary care patient visits on racial and ethnic disparities in preventive care in the united states. Journal of the American Board of Family Medicine : JABFM, 20(6), 587-597. doi:10.3122/jabfm.2007.06.070053 BACKGROUND: The causes of racial and ethnic disparities in preventive care are not fully understood. We examined the hypothesis that fewer primary care visits by minority patients contribute to these disparities. METHODS: We analyzed claims for Medicare beneficiaries 65 and older who participated in the Medicare Current Beneficiary Survey, 1998 to 2002. Five preventive services were included: colorectal cancer testing, influenza vaccination, lipid screening, mammography, and Papanicolaou smear screening. In separate multivariate analyses, we examined the effect of minority status (self-report of African American race or Hispanic ethnicity) on having a claim in the past 12 months for each preventive service after successive control for number of primary care visits and other patient characteristics. RESULTS: The final sample included 15,962 subjects. In age-adjusted analyses, minorities had statistically lower rates of claims for each of the 5 procedures. After controlling for number of primary care visits, the effect of minority status was slightly attenuated but remained statistically significant for receipt of each procedure. After adding low income, low educational level and supplementary insurance, health status, and year, minority status was significantly associated only with colorectal cancer screening (odds ratio [OR] 0.79; 95% confidence interval [CI] 0.67 to 0.94) and influenza vaccinations (OR 0.56; 95% CI 0.49 to 0.64). CONCLUSIONS: The frequency of primary care visits seems to contribute minimally to racial and ethnic disparities in preventive services. Other patient characteristics, particularly those associated with poverty, explain much of these disparities. Forster, A. J., Clark, H. D., Menard, A., Dupuis, N., Chernish, R., Chandok, N., et al. (2005). Effect of a nurse team coordinator on outcomes for hospitalized medicine patients. American Journal of Medicine, 118(10), 1148-1148-1153. Several randomized trials have found that discharge planning improves outcomes for hospitalized patients. This study seeks to explore whether adding a clinical nurse specialist (CNS) to physician teams in hospitals that already have discharge planning services makes a difference. At the Page22 Jefferson InterProfessional Education Center Bibliography – January 2009 conclusion of the study, the addition of a clinical nurse specialist to a medical team improved patient satisfaction but did not impact hospital efficiency or patient safety. Fortin, M., Soubhi, H., Hudon, C., Bayliss, E. A., & Akker, M. (2007). Multimorbidity's many challenges. British Medical Journal, 334(7602), 1016-1016-1017. This article discussed the need for investigation into multimorbidities. The author provides three categories into which research into multimorbidity should fall - defining and categorising the population; developing the tools needed to explore multimorbidity and its consequences; and using these tools to investigate promising processes of care. Fowler, F. J.,Jr, Gallagher, P. M., Anthony, D. L., Larsen, K., & Skinner, J. S. (2008). Relationship between regional per capita medicare expenditures and patient perceptions of quality of care. JAMA : The Journal of the American Medical Association, 299(20), 2406-2412. doi:10.1001/jama.299.20.2406 CONTEXT: Wide variations in Medicare expenditures exist across regions, but little is known about whether beneficiaries residing in low-expenditure regions perceive receiving lower-quality care than those in high-expenditure regions. OBJECTIVE: To evaluate how Medicare beneficiaries' perceptions of their health care are related to per capita expenditure in the areas where they live. DESIGN, SETTING, AND RESPONDENTS: A probability sample of Medicare beneficiaries living in households in the United States was surveyed by a combination of mail and telephone in 2005. Each respondent was allocated to 1 of 5 quintiles, depending on mean age-, sex-, and race-adjusted per capita Medicare expenditures based on Centers for Medicare & Medicaid Services claims data. MAIN OUTCOME MEASURES: The survey included 3 questions about perceived unmet need for care, 4 questions about the perceived quality of ambulatory care, and 3 questions rating the perceived quality of overall care. RESULTS: Of 4000 Medicare beneficiaries sampled, 160 (4%) were ascertained to have died or to be living in a long-term care facility. Of the remaining 3840 potentially eligible beneficiaries, 2515 (65%) responded. Per capita expenditures were highly related to receiving more medical care, such as mean number of ambulatory visits to physicians in the past year (range from lowest to highest expenditure quintile, 3.4-3.9; P < .001 for linear trend) and more cardiac tests (respondents reporting receiving tests in past year, 158/387 [40.1%] to 468/739 [63.5%]; P < .001 for linear trend). However, 7 of the 10 measures of perceived quality, including perceived unmet needs for tests and treatment (respondents reporting unmet needs, 15/387 [3.9%] to 37/739 [5.0%]; P = .25 for linear trend) and spending enough time with physicians (respondents reporting adequate time, 311/387 [88.7%] to 603/739 [87.0%]; P = .94 for linear trend), were unrelated to expenditures, while the overall rating of perceived quality of care was higher in the lower-expenditure areas (respondents reporting overall care rating of 9 or 10, 242/387 [63.3%] to 404/739 [55.4%]; P = .008 for linear trend). CONCLUSION: In this representative sample of Medicare beneficiaries, no consistent association was observed between the mean per capita expenditure in a geographic area and the perceptions of the quality of medical care of the people who live in those areas. Freeth, D., Ayida, G., Berridge, E., Sadler, C., & Strachan, A. (2006). MOSES: Multidisciplinary obstetric simulated emergency scenarios. Journal of Interprofessional Care, 20(5), 552-552-554. The MOSES program was developed to provide training in response to concerns about the quality of team care in maternity care. Its aim is to to improve teamwork skills and highlight the role that human behavior can play in crisis prevention and resolution. While course evaluations show that participants enjoyed and valued the program, no evaluation has been conducted to determine its effect on the delivery of maternity services. Freeth, D., & Reeves, S. (2004). Learning to work together: Using the presage, process, product (3P) model to highlight decisions and possibilities. Journal of Interprofessional Care, 18(1), 43-56. doi:10.1080/13561820310001608221 Collaborative practice is seen as a core aspect of professional practice and, therefore, a focus of professional education. Current interprofessional and quality assurance literature provides Page23 Jefferson InterProfessional Education Center Bibliography – January 2009 enumeration and discussion of a range of competencies required for effective collaborative practice. Case studies of education and training related to collaborative competences rarely discuss the nature of influences on development, delivery and learning. Barriers to development and delivery have been identified for interprofessional education, but we want to move beyond the mental picture of climbing over or moving around fixed hurdles. Learning opportunities are complex dynamic systems, seeking equilibrium. The creative tension of influences provides opportunities for insightful management. This paper uses the systems-form 3P (presage-process-product) model of learning and teaching (Biggs, 1993) to help examine the nature of educational opportunities designed to promote collaborative working. Presage, process and product factors are identified and discussed. We argue that untangling (or at least seeing) the web of influences on learning to work together promotes critical awareness and encourages more informed and timely decisions. Freudenstein, U., Jagger, C., Arthur, A., & Donner-Banzhoff, N. (2001). Treatments for late life depression in primary care--a systematic review. Family Practice, 18(3), 321-327. BACKGROUND: Depression is common among older people. It is associated with increased mortality and use of health services. We could identify no prior systematic review of treatment for depression in either primary care attenders or population samples of older people. OBJECTIVES: The aim of this study was to carry out a systematic review of trials of treatments for depression of patients over 60 years of age in primary care or population samples. CONCLUSION: There is little evidence of effectiveness for a variety of treatment approaches for depression in older people in primary care, particularly in those with less severe depression. As older people take more medication, making contra-indications to the use of antidepressant drugs more likely, there is a pressing need for studies of the efficacy of non-pharmacological interventions in primary care settings. Friedman, D. M., & Berger, D. L. (2004). Improving team structure and communication: A key to hospital efficiency. Archives of Surgery, 139(11), 1194-1194-1198. This study sought to determine whether improving team structure and heightening communication would provide cost-effective and high-quality patient care for general surgery patients. The study concluded that restructuring the patient care team yielded a decreased mean length of stay while maintaining a high level of patient satisfaction. Fu, D., Ding, Y., McGowan, P., & Fu, H. (2006). Qualitative evaluation of chronic disease selfmanagement program (CDSMP) in shanghai. Patient Education and Counseling, 61, 389-389-396. This study sought to explore the impact of a chronic disease self-management program on participants' perceptions of their behavior, health status, quality of life, and how the program achieves its benefits. In addition, the study explored how to collect suggestions for future improvement and dissemination of results. CDSMP was perceived to be effective to participants mainly through behavior change and self-efficacy development, though it had a few deficiencies. Fuentes, B., & Tejedor, E. D. (2002). Re: Randomized controlled study of stroke unit versus stroke team care in different stroke subtypes. Stroke; a Journal of Cerebral Circulation, 33(7), 1740-1; author reply 1740-1. This article is a response to the article "Randomized controlled study of stroke unit versus stroke team care in different stroke subtypes" by Evans et al. The authors, based on their own studies, agree with Evans' findings and believe that all stroke patients should be treated on stroke units. Gandhi, T. K. (2005). Fumbled handoffs: One dropped ball after another. (see comment). Annals of Internal Medicine, 143(7), 542-542-543. This article discusses the idea that missed follow-up of abnormal tests results and resultant days in diagnosis is a safety issue that is gaining increased attention. Current systems in health care do not reliably ensure that test results are received and acted upon by ordering physicians. This article examines a specific case of a patient who's diagnosis was delayed because of systems problems. Page24 Jefferson InterProfessional Education Center Bibliography – January 2009 Gannon-Leary, P., Baines, S., & Wilson, R. (2006). Collaboration and partnership: A review and reflection on a national project to join up local services in england. Journal of Interprofessional Care, 20(6), 665-665-674. The need to provide more joined services in health and social care is now recognized by governments as a major objective, and technology is increasingly seen as the key to achieving it. This paper is based upon the authors' experience as research partners in a national project in England known as FrAmework for Multi-agency Environments (FAME). In the first phase of FAME (April 2003 - October 2004) six local “strands” led by local authorities worked in partnership with service providers and IT suppliers. Each partnership aimed to support collaboration and interaction between professions in a particular set of services (for example, to vulnerable older people or disabled children) through effective and appropriate exchange of information. This paper examines the literature on partnership and collaboration in public services in order to contextualize and reflect upon IT-enabled multi-agency partnerships Gask, L. (2005). Role of specialists in common chronic diseases. (see comment). (review). British Medical Journal, 330(7492), 651-651-653. Most people with chronic conditions such as diabetes, congestive heart failure, asthma, and depression are managed in primary care. NHS consultants have traditionally confined their role to patients who are referred to outpatient clinics by their general practitioners. Such patients usually have the most severe and complex problems. Effective care teams for chronic illness must be able to 1 cross practice or organisational boundaries, but the current organisational structure of the NHS does not provide many incentives to develop such linkages. General practitioners refer patients they cannot manage and hospitals are funded on the basis of referrals. Time spent on joint work with primary care is not accounted for. To ensure that all patients get the best treatment, the role of consultants needs to change so that their specialist knowledge is more available to everyone dealing with chronic disease. Gaudet, J., Shekter-Wolfson, L., Seaberg, R., Stulla, D., Cohoon, C., Kapelus, G., et al. (2007). Implementing and evaluating interprofessional education for health sciences students: Early experiences from a canadian college. Journal of Interprofessional Care, 21(4), 459-461. doi:10.1080/13561820701273190 In 2004, leaders a the The Centre for Health Sciences at George Brown College (GBC) in Toronto, Canada, identified implementation of interprofessional education initiatives to be a priority. This report describes the components of the IPE initiative, details of its related evaluation project, and initial findings. Gebbie, K. M. (2004). The competency-to-curriculum toolkit. Retrieved April 9, 2008, from http://www.nursing.columbia.edu/chphsr/projects/complProj/cct.html The Competency-to-Curriculum Toolkit grew out of discussions held at the CDC-sponsored Public Health Workforce Meeting in 2001. This toolkit is presented to the public health workforce training and education community as an aid to assure that the workforce is truly competent to perform essential public health services in all areas of public health practice. Gilbert, J. H. V. (2005). Interprofessional learning and higher education structural barriers. Journal of Interprofessional Care, 19(Supplement 1), 87-87-106. This article discusses the barriers to implementing an interprofessional education approach for patient-centered collaborative practice within universities. The article also discusses structural changes that need to be made within universities in order for an interprofessional education approach to be successful. Gilkey, M. B., & Earp, J. A. (2006). Effective interdisciplinary training: Lessons from the university of north carolina's student health action coalition. Academic Medicine : Journal of the Association of American Medical Colleges, 81(8), 749-758. PURPOSE: To identify essential elements of effective interdisciplinary training through an evaluation Page25 Jefferson InterProfessional Education Center Bibliography – January 2009 of the University of North Carolina's Student Health Action Coalition (SHAC), an interdisciplinary service learning program for health science students. METHOD: In 2004, 516 SHAC volunteers were asked to complete a 52-item, online questionnaire. Responses were tallied by volunteer role, and four of the resulting "divisions" (counseling, medical care, interpretation, and community outreach) were analyzed using qualitative and quantitative rating schemas. The four divisions were compared on volunteers' perception of two concepts: (1) the level of interdisciplinary training achieved and (2) the potential for working together, or "community capacity." RESULTS: A total of 283 students accessed the online questionnaire, and 281 provided consent and filled out some portion of the questionnaire, an overall response rate of 54%. A total of 159 of the 281 respondents (57%) reported volunteering most often for one of the four divisions of interest. The respondents in each volunteer division reported a level of interdisciplinary training similar to that division's level of community capacity. The division responsible for counseling services indicated the least interdisciplinary training, earning 4 points on an 8-point rating schema. This group also reported low levels of participation, group skills, information sharing, shared values, sense of community, and social networks. The community outreach division reported the highest level of interdisciplinary training, receiving 8 out of 8 points. They also had high levels of participation, group skills, information sharing, networking, and sense of community. CONCLUSIONS: Effective interdisciplinary training goes hand in hand with five elements identified from the community capacity literature: participation, training in group skills, information sharing, networking, and critical reflection. Program planners and evaluators should pay particular attention to the social environment so as not to reinforce professional stereotypes that interdisciplinary programs are meant to dispel. Ginsburg, L., & Tregunno, D. (2005). New approaches to interprofessional education and collaborative practice: Lessons from the organizational change literature. Journal of Interprofessional Care, 19(Supplement 1), 177-177-187. This paper highlights a variety of issues from the organizational change literature that are especially relevant to the implementation initiatives in interprofessional education (IPE) for collaborative practice (CP). The paper discusses these issues at the level of the individual, organization, and system. The paper concludes with a set of key recommendations suggested for reducing the incidence of implementation failure. Gitlin, L. N., Lyons, K. J., & Kolodner, E. (1994). A model to build collaborative research or educational teams of health professionals in gerontology. Educational Gerontology, 20(1), 15-15-33. A five-stage model of collaboration is presented which utilizes key constructs from the social exchange theory and literature relating to team building. The model presented ensures that projects are based on gerontological knowledge, integration of theory, and reflect real-life health care needs of the elderly. Gitlin, L. N., Hauck, W. W., Winter, L., Dennis, M. P., & Schulz, R. (2006). Effect of an in-home occupational and physical therapy intervention on reducing mortality in functionally vulnerable older people: Preliminary findings. Journal of the American Geriatrics Society, 54(6), 950-955. doi:10.1111/j.1532-5415.2006.00733.x OBJECTIVES: To evaluate the effect of a multicomponent intervention on mortality and the role of control-oriented strategy use as the change mechanism. DESIGN: Two-group randomized design with survivorship followed for 14 months. Participants were randomized to intervention or a notreatment control group. SETTING: Urban, community-living older people. PARTICIPANTS: Three hundred nineteen people aged 70 and older with functional difficulties. INTERVENTION: Occupational therapy and physical therapy sessions involving home modifications, problem solving, and training in energy conservation, safe performance, balance, muscle strength, and fall recovery techniques. MEASUREMENTS: Survival time was number of days between baseline interview and date of death or final interview if date unknown. Control-oriented strategy use was measured using eight items. RESULTS: Intervention participants exhibited a 1% rate of mortality, compared with a 10% rate for no-treatment control participants (P=.003, 95% confidence interval=2.4-15.04%). At baseline, those who subsequently died had more days hospitalized and lower control-oriented strategy use 6 months before study enrollment than survivors. No intervention participants with Page26 Jefferson InterProfessional Education Center Bibliography – January 2009 previous days hospitalized (n=31) died, whereas 21% of control group counterparts did (n=35; P=.001). Although intervention participants with low and high baseline control strategy use had lower mortality risk than control participants, mortality risk was lower for intervention participants with low strategy use at baseline (P=.007). CONCLUSION: An occupational and physical therapy intervention to ameliorate functional difficulties may reduce mortality risk in community-dwelling older people overall and benefit those most compromised. Instruction in control-oriented strategies may account for the intervention's protective effects on survivorship. Gitlin, L. N., Winter, L., Dennis, M. P., Corcoran, M., Schinfeld, S., & Hauck, W. W. (2006). A randomized trial of a multicomponent home intervention to reduce functional difficulties in older adults. Journal of the American Geriatrics Society, 54(5), 809-816. doi:10.1111/j.1532-5415.2006.00703.x The objective of this study was to test the efficacy of a multicomponent intervention to reduce functional difficulties, fear of falling, and home hazards and enhance self-efficacy and adaptive coping in older adults with chronic conditions. The study was a prospective, 2-group randomized trial, where patients were assigned to a treatment or non-treatment group. The intervention consisted of occupational and physical therapy sessions involving home modifications and training, problem solving, energy conservation, safe performance and recovery techniques, and balance and muscle strengthening. After 6 months, intervention participants has less difficulty with ADLs than controls. The study conclusion is that a multicomponent intervention targeting modifiable environmental and behavioral factors can result in improvement in quiality of life for older adults with functional difficulties. Glasziou, P., Irwig, L., & Mant, D. (2005). Monitoring in chronic disease: A rational approach. British Medical Journal, 330(7492), 644-644-648. Monitoring chronic diseases for both benefit and harm is important, preferably with a single measurement. Monitoring is not always necessary or beneficial and can lead to inappropriate changes. Monitoring aims to establish the response to treatment, detect the need to adjust treatment, and detect adverse effects. Control charts help distinguish natural variability from true change and reduce unnecessary adjustment. Goldstein, J. (2008, 02-13-2008). Helping patients help selves: Pa. panel aims to transform chronic-care delivery. Philadelphia Inquirer. Govan, L., Weir, C. J., Langhorne, P., & for the Stroke Unit Trialists' Collaboration. (2008). Organized inpatient (stroke unit) care for stroke. Stroke; a Journal of Cerebral Circulation, doi:10.1161/STROKEAHA.108.515510 This study sought to review literature (Cochrane Review) to test whether the use of an inpatient stroke unit resulted in improved patient outcomes. The study found that stroke unit care reduced the odds of death at final follow-up, death or institutionalized care, and death or dependancy. Gow, P., Berg, S., Smith, D., & Ross, D. (1999). Care co-ordination improves quality-of-care at south auckland health. Journal of Quality in Clinical Practice, 19(2), 107-110. Inpatient discharge surveys at Middlemore hospital, a 600 bed hospital in South Auckland, New Zealand, consistently rate communication and co-ordination of care as parameters in need of improvement. A case management model of care was suggested as a means of achieving this. The objective of this study was to determine the effectiveness of care co-ordination in an acute general medical setting in a pilot study over a 4 week period. A care co-ordinator identified 18 patients with complex problems among 48 patients admitted to a single medical ward under the care of a single multidisciplinary team, with their care being co-ordinated over the entire episode of illness. A control group of 59 similarly complex patients admitted to other wards and teams without care co-ordination over the same period was also studied and the outcomes compared. Communication and coordination, discharge information, involvement in discharge planning and information on postdischarge services were rated by the study patients as good or very good by 77, 85, 69 and 77%, respectively, compared with 62, 30, 41 and 45% in the control group. The same parameters were rated as poor or very poor by 13, 30, 36 and 15% of the control patients, compared with 0% in all Page27 Jefferson InterProfessional Education Center Bibliography – January 2009 these measures in the study group. Twenty-one clinical staff involved in the study agreed that there was an improvement in care co-ordination with respect to efficiency, reduction of workload and better communication, with approval ratings being 71, 76 and 76%, respectively. There was no difference in Average Length of Stay between the control and study groups, but three of the patients in the control group may have had their preventable readmissions within 10 days avoided if their care had been co-ordinated during their initial admission. Gray, J. A. (2004). Self-management in chronic illness. (comment). Lancet, 364(9444), 1467-1467-1468. This author comments on methods of providing patient education about chronic diseases, emphasizing the varied needs of patients even when dealing with the same disease. He states that individualization is the task of the primary care physician and proposes that this is a three step process and believes that this outlined method will become standard in primary care, as patients continue to seek more involvement in their treatment. Green, S. (2004). Medical education and chronic disease. (comment). Journal of the American Medical Association, 292(9), 1057-1057-1059. This author comments on the lack of medical student education on the topic of chronic disease. Grey, M., Knafl, K., & McCorkle, R. (2006). A framework for the study of self-and family management of chronic conditions. Nursing Outlook, 54(5), 278-278-286. The Yale School of Nursing has developed a framework to guide research efforts in interventions to enhance self- and family-management of chronic illness. Grogan, E. L., Stiles, R. A., France, D. J., Speroff, T., Morris, J. A. J., Nixon, B., et al. (2004). The impact of aviation-based teamwork training on the attitudes of health-care professionals. Journal of the American College of Surgeons, 199(6), 843-843-848. The purpose of this study was to explore whether patient safety can be enhanced by implementing aviation Crew Resource Management (CRM) in health care. CRM emphasized six key areas: managing fatigue, creating and managing teams, recognizing adverse situations (red flags), crosschecking and communications, decision making, and performance feedback. CRM training was found to improve attitudes towards fatigue management, team building, communication, recognizing adverse events, team decision making, and performance feedback. Groves, T., & Wagner, E. H. (2005). High quality care for people with chronic diseases. British Medical Journal, 330(7492), 609-609-610. Editorial - an edition of the BMJ dedicated to management of chronic disease Gurses, A. P., & Xiao, Y. (2006). A systematic review of the literature on multidisciplinary rounds to design information technology. Journal of the American Medical Informatics Association : JAMIA, 13(3), 267-276. doi:10.1197/jamia.M1992 Multidisciplinary rounds (MDR) have become important mechanisms for communication and coordination of care. To guide design of tools supporting MDR, we reviewed the literature published from 1990 to 2005 about MDR on information tools used, information needs, impact of information tools, and evaluation measures. Fifty-one papers met inclusion criteria and were included. In addition to patient-centric information tools (e.g., medical chart) and decision-support tools (e.g., clinical pathway), process-oriented tools (e.g., rounding list) were reported to help with information organization and communication. Information tools were shown to improve situation awareness of multidisciplinary care providers, efficiency of MDR, and length of stay. Communication through MDR may be improved by process-oriented information tools that help information organization, communication, and work management, which could be achieved through automatic extraction from clinical information systems, displays and printouts in condensed forms, at-a-glance representations of the care unit, and storing work-process information temporarily. Page28 Jefferson InterProfessional Education Center Bibliography – January 2009 Gurwitz, J. H. (2004). Polypharmacy: A new paradigm for quality drug therapy in the elderly? (comment). (review). Archives of Internal Medicine, 164(18), 2031-2031-2037. This article looks at issues surrounding avoiding excessive use of medications in the elderly vs. providing access to therapies that may be more beneficial. Factors examined include lack of high quality evidence to guide prescribing, adoption of new systems of care, and costs as a barrier. Hagar, M. (2005). The convergence of neuroscience, behavioral science, neurology, and psychiatry. New York, NY: Josiah Macy, Jr. Foundation. Hager, M. H., & Michael, P. (2005). Clinical practice guidelines for older patients with comorbid diseases (comment). Journal of the American Medical Association, 295(1), 716-716-724. The authors provide comments on Boyd's article "Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance." They clarify the benefits of nutritional therapy by a registered nutritionist and that as of 2001 Medicare benefits include nutrition therapy for beneficiaries with diabetes and renal disease. Hall, P. (2005). Interprofessional teamwork: Professional cultures as barriers. Journal of Interprofessional Care, 19(Supplement 1), 188-188-196. Each health care profession has a different culture. As students progress throughout their education, common values from their respective professions are reinforced, which leads to increased specialization within each professional group. However, this specialization contributes to decreased interprofessional teamwork. Insight into the educational, systemic, and personal factors which contribute to the culture of the professions can help guide the development of innovative educational methodologies to improve interprofessional collaborative practice. Hall, P., Weaver, L., Fothergill-Bourbonnais, F., Amos, S., Whiting, N., Barnes, P., et al. (2006). Interprofessional education in palliative care: A pilot project using popular literature. Journal of Interprofessional Care, 20(1), 51-51-59. A seminar course was developed at the University of Ottowa in order to address the need for collaboration within the area of palliative care. This course utilized popular literature as a basis for learning. Evaluation findings suggest that meaningful interprofessional education can be introduced effectively to students prior to or while they are maturing in their professional roles. Hall, P., & Weaver, L. (2001). Interdisciplinary education and teamwork: A long and winding road. Medical Education, 35(9), 867-875. PURPOSE: This article examines literature on interdisciplinary education and teamwork in health care, to discover the major issues and best practices. MAIN FINDINGS: Two issues are emerging in health care as clinicians face the complexities of current patient care: the need for specialized health professionals, and the need for these professionals to collaborate. Interdisciplinary health care teams with members from many professions answer the call by working together, collaborating and communicating closely to optimize patient care. Education on how to function within a team is essential if the endeavour is to succeed. Two main categories of issues emerged: those related to the medical education system and those related to the content of the education. CONCLUSIONS: Much of the literature pertained to programme evaluations of academic activities, and did not compare interdisciplinary education with traditional methods. Many questions about when to educate, who to educate and how to educate remain unanswered and open to future research. Halsted, M. J., Perry, L. A., Cripe, T. P., Collins, M. H., Jakobovits, R., Benton, C., et al. (2004). Improving patient care: The use of a digital teaching file to enhance clinicians' access to the intellectual capital of interdepartmental conferences. (review). American Journal of Roentgenology, 182(2), 307-307309. This article describes a simple method for creating teaching cases from clinical data, radiologic images, surgical images, and images from pathologic slides that are presented at tumor board conferences. This system improves the efficiency and accuracy in gathering patient histories when care is transferred among clinics, the emergency department, and wards. Page29 Jefferson InterProfessional Education Center Bibliography – January 2009 Handley, M., MacGregor, K., Schillinger, D., Sharifi, C., Wong, S., & Bodenheimer, T. (2006). Using action plans to help primary care patients adopt healthy behaviors: A descriptive study. Journal of the American Board of Family Medicine : JABFM, 19(3), 224-231. PURPOSE: An action plan is an agreement between clinician and patient that the patient will make a specific behavior change. The goals of this study are to: determine whether it is feasible for patients to make action plans in the primary care visit; determine whether patients report carrying out their action plans; and describe the action plans patients choose. METHODS: Forty-three clinicians in 8 primary care sites were recruited to hold action-plan discussions with patients. Research assistants contacted patients by telephone 3 weeks later to assess whether patients had conducted their action plans. RESULTS: Eighty-three percent of enrolled patients (228) made an action plan during a primary care visit. Of the 79% who recalled making the action plan when interviewed by telephone 3 weeks later, 56% recalled the details of their action plan, and an additional 33% recalled the general nature of the action plan. At least 53% of patients making an action plan reported making a behavior change consistent with that action plan. CONCLUSIONS: Most patients reported making a behavior change based on an action plan, suggesting that action plans may be a useful strategy to encourage behavior change for patients seen in primary care. Harward, D. H., Tresolini, C. P., & Davis, W. A. (2006). Can participation in a health affairs interdisciplinary case conference improve medical students' knowledge and attitudes? Journal of Medical Education, 81(3), 257-257-261. A three-hour health affairs interdisciplinary case conference was conducted with 2,005 health professions students. Following participation in the conference, there were significant increases in students' knowledge about the training and skills of all ten professions, the advantages of working in an interdisciplinary team, and the importance of care provided by these professions. In general, there were significant improvements in students' attitudes toward the value of interdisciplinary team work and leadership by all health professionals. Healey, A., Undre, S., Sevdalis, N., Kutanji, M., & Vincent, C. (2006). The complexity of measuring interprofessional teamwork in the operating theatre. Journal of Interprofessional Care, 20(5), 585585-595. This paper addresses the complexity of measuring interprofessional teamwork in the operating theater. It focuses mainly on the design and properties of observational assessment tools. The report and analysis serves to inform the researcher or clinician of the issues to consider when designing or choosing from alternative measures of team performance for training or assessment. Hean, S., Clark, J. M., Adams, K., & Humphris, D. (2006). Will opposites attract? similarities and differences in students' perceptions of the stereotype profiles of other health and social care professional groups. Journal of Interprofessional Care, 20(2), 162-162-181. The extent to which health and social care (HSC) students hold stereotypical views of other HSC professional groups is of potential importance to team working in health care. This paper explores students' perceptions of different HSC professional groups at the beginning and end of their university programs. The implications of the similarities and differences discussed could potentially have an impact of interprofessional interactions, role boundaries, and team working. Hean, S., & Dickinson, C. (2005). The contact hypothesis: An exploration of its further potential in interprofessional education. Journal of Interprofessional Care, 19(5), 480-480-491. The Contact Hypothesis is a useful theoretical framework to address challenges that face researchers who wish to build the evidence base around interprofessional education (IPE). This article briefly describes the theory and closely-related theories of social identity and categorization. The application of the Contact Hypothesis to interprofessional education is also described. Heathfield, S. M. (2007). Twelve tips for team building: How to build successful work teams. Retrieved February 11, 2008, from http://humanresources.about.com/od/involvementteams/a/twelve_tip_team.htm?p=1 This brief article gives tips for team building which include: clear expectations, context, commitment, Page30 Jefferson InterProfessional Education Center Bibliography – January 2009 competence, charter, control, collaboration, communication, creative innovation, consequences, coordination, and cultural change. Hebert, K. A., Horswell, R. L., Dy, S., Key, I. J., Butler, M. K., Cerise, F. P., et al. (2006). Mortality benefit of a comprehensive heart failure disease management program in indigent patients. [The purpose of this study was to determine whether participation in a heart failure disease management (HFDM) program would reduce mortality in an indigent population from rural Louisiana. The study found that participation in an HFDM program was associated with decreased mortality compared with traditional follow-up care for this indigent population.] American Heart Journal, 151(2), 478-478-483. T Henrich, J. B., Chambers, J. T., & Steiner, J. L. (2003). Development of an interdisciplinary women's health training model. Journal of Medical Education, 78(9), 877-877-884. The Interdisciplinary Women's Health Clinic (IWHC) was established at Yale University School of Medicine to allow for an interdisciplinary women's health training and education model. The IWHC was developed as a consultation service that augmented the primary care provided to low-income, minority-group women in an established outpatient primary care setting. The article describes the structure, function, and evolution of that training model up to its closure in 2000, when the Yale Department of Health and Human Services contract ended. Herbert, C. P. (2005). Changing the culture: Interprofessional education for collaborative patient-centered practice in canada. Journal of Interprofessional Care, 19(Supplement 1), 1-1-4. Editorial: the author, Co-Chair of the Health Canada National Expert Committee on Interprofessional Education for Collaborative Patient-Centered Practice, discusses the importance of implementing interprofessional education in health care education programs being that increasingly more health care providers are expected to work as a team in practice. The author also discusses and defines collaborative patient-centered practice. Higashi, T., Wenger, N. S., Adams, J. L., Fung, C., Roland, M., McGlynn, E. A., et al. (June 14, 2007). Relationship between number of medical conditions and quality of care. The New England Journal of Medicine, 356, 2496-2496-2504. Hill, K. S. (2003). Development of leadership competencies as a team. Journal of Nursing Administration, 33(12), 639-639-642. The author of this article describes an organized approach to leadership competency development for nursing and non-nursing department directors and senior administrative staff members. Hodnett, E. D. (2000). Continuity of caregivers for care during pregnancy and childbirth. Cochrane Database of Systematic Reviews (Online), (2)(2), CD000062. doi:10.1002/14651858.CD000062 BACKGROUND: Care is often provided by multiple caregivers, many of whom work only in the antenatal clinic, labour ward or postnatal unit. However continuity of care is provided by the same caregiver or a small group from pregnancy through the postnatal period. OBJECTIVES: The objective of this review was to assess continuity of care during pregnancy and childbirth and the puerperium with usual care by multiple caregivers. SEARCH STRATEGY: The Cochrane Pregnancy and Childbirth Group trials register was searched. SELECTION CRITERIA: Controlled trials comparing continuity of care with usual care during pregnancy, childbirth and the postnatal period. DATA COLLECTION AND ANALYSIS: Trial quality was assessed. Study authors were contacted for additional information. MAIN RESULTS: Two studies involving 1815 women were included. Both trials compared continuity of care by midwives with non-continuity of care by a combination of physicians and midwives. The trials were of good quality. Compared to usual care, women who had continuity of care from a team of midwives were less likely to be admitted to hospital antenatally (odds ratio 0.79, 95% confidence interval 0.64 to 0.97) and more likely to attend antenatal education programs (odds ratio 0.58, 95% confidence interval 0.41 to 0.81). They were also less likely to have drugs for pain relief during labour (odds ratio 0.53, 95% confidence interval 0.44 to 0.64) and their newborns were less likely to require resuscitation (odds ratio 0.66, 95% confidence interval 0.52 to Page31 Jefferson InterProfessional Education Center Bibliography – January 2009 0.83). No differences were detected in Apgar scores, low birthweight and stillbirths or neonatal deaths. While they were less likely to have an episiotomy (odds ratio 0.75, 95% confidence interval 0.60 to 0.94), women receiving continuity of care were more likely to have either a vaginal or perineal tear (odds ratio 1.28, 95% confidence interval 1.05, 1.56). They were more likely to be pleased with their antenatal, intrapartum and postnatal care. REVIEWER'S CONCLUSIONS: Studies of continuity of care show beneficial effects. It is not clear whether these are due to greater continuity of care, or to midwifery care. Hojat, M., Fields, S. K., & Gonnella, J. S. (2003). Empathy: An NP/MD comparison. The Nurse Practitioner, 28(4), 45-45-47. This study compared the scores of empathy among nurse practitioners and physicians within the context of health care. Research has demonstrated that empathy plays a key role in patient outcomes. Results demonstrated that nurse practitioners and pediatricians obtained a significantly higher mean empathy score than hospital-based physicians. Holland, R., Battersby, J., Harvey, I., Lenaghan, E., Smith, J., & Hay, L. (2005). Systematic review of multidisciplinary interventions in heart failure. Heart, 91(7), 899-899-906. The purpose of this study was to determine the impact of multidisciplinary interventions on hospital admission and mortality in heart failure. The study concluded that multidisciplinary interventions for heart failure reduce both hospital admission and all cause mortality. Holman, H. (2004). Chronic disease -- the need for a new clinical education. The Journal of the American Medical Association, 292(9), 1057-1057-1059. Medical schools currently do not adequately prepare their students for care of chronically ill patients. The author of this article suggests creating a chronic care model which includes a practice team, information system, decision supports for practice, and patient self-management supports. It is suggested that students should be assigned to a supervised longitudinal case study upon enrollment in these programs. Providing these new learning experiences requires new understandings and new behaviors. Holman, H., & Lorig, K. (2004). Patient self-management: A key to effectiveness and efficacy in care of chronic disease. Public Health Reports, 119, 239-239-243. This article examines the role of the patient in their treatment of chronic disease. Hope, J. M., Lugassy, D., Meyer, R., Jeanty, F., Myers, S., Jones, S., et al. (2005). Bringing interdisciplinary and multicultural team building to health care education: The downstate teambuilding initiative. Journal of Medical Education, 80(1), 74-83. The purpose of the article was to evaluate the impact of the Downstate Team-Building Initiative (DTBI), a model multicultural and interdisciplinary health care team-building program for health professions students. DTBI successfully united students across health discipline, ethnicity, socioeconomic class, gender, and sexual orientation into functioning teams. The model represents an effective approach to teaching health care team building and demonstrates benefits in both preclinical and clinical years of training. Horsburgh, M., Merry, A., Seddon, M., Baker, H., Poole, P., Shaw, J., et al. (2006). Educating for health care quality improvement in an interprofessional learning environment: A new zealand initiative. Journal of Interprofessional Care, 20(5), 555-555-557. The University of Auckland's Faculty of Medical and Health Sciences have created an interdisciplinary learning initiative for their undergraduate medical, nursing and pharmacy students. The program brings the students together for two learning modules, one focused on Maori Health and the other on Patient Safety. Horsburgh, M., Perkins, R., Coyle, B., & Degeling, P. (2006). The professional subcultures of students entering medicine, nursing and pharmacy programmes. Journal of Interprofessional Care, 20(4) Page32 Jefferson InterProfessional Education Center Bibliography – January 2009 This study sought to determine the attitudes, beliefs and values towards clinical work organization of students entering undergraduate medicine, nursing and pharmacy programs in order to frame questions for a wider study. Horton, R. (2006). The neglected epidemic of chronic disease (see comment). Lancet, 367(9510), 563563-564. As reduction of chronic disease is not a Millennium Development Goal (MDG), the Lancet has issued a series of articles to stimulate global discussion of chronic disease. Howe, A. (2006). Can the patient be on our team? an operational approach to patient involvement in interprofessional approaches to safe care. Journal of Interprofessional Care, 20(5), 527-527-534. This paper describes a spectrum of practical approaches that can be implemented by teams and organizations, ranging from whole population prevention strategies to the learning that can be gained from avoidable deaths. It explores concrete examples of the ways in which individual patients might be included in a team approach to self protection, and addresses underpinning principles of effective interprofessional working which are needed to make such approaches effective. Hroscikoski, M. C., Solberg, L. I., Sperl-Hillen, J. M., Harper, P. G., McGrail, M. P., & Crabtree, B. F. (2006). Challenges of change: A qualitative study of chronic care model implementation. Annals of Family Medicine, 4, 317-317-326. The Chronic Care Model (CCM) works to improve health care for patients with chronic conditions. Small changes were seen with the implementation of the CCM with many identifiable barriers. It was found that there are many organizational challenges with the transformation of health care with the CCM because it is not a specific model. Hudson, B. (2007). Pessimism and optimism in inter-professional working: The sedgefield integrated team. Journal of Interprofessional Care, 21(1), 3-3-15. The literature on inter-professional working tends to be dominated by explanations for lack of progress rather than accounts of achievements. This paper develops two models, termed the optimistic and pessimistic models respectively, to understand the factors that may underpin different rates of interprofessional achievement. A case study is utilized to test the models. Hughes, M., Ventura, S., & Dando, M. (2004). On-line interprofessional learning: Introducing constructivism through enquiry-based learning and peer review. Journal of Interprofessional Care, 18(3), 263-263-268. This paper illustrates the issues in designing a large, on-line, inter-professional module for third year, undergraduate students drawn from nine professional health care courses and from four campus sites. This program utilized an inquiry-based learning approach. The learning theories of Piaget, Vygotsky, and Schon are integrated with the on-line frameworks of Salmon and Collis et al. Hui, E., Lum, C. M., Woo, J., Or, K. H., & Kay, R. L. (1995). Outcomes of elderly stroke patients. day hospital versus conventional medical management. Stroke; a Journal of Cerebral Circulation, 26(9), 1616-1619. BACKGROUND AND PURPOSE: Much controversy exists over the value of geriatric day hospitals in the rehabilitation of elderly patients, and cerebrovascular accident is a particularly common diagnosis among patients referred to these day hospitals. We carried out a prospective, randomized study to compare the outcomes of elderly stroke patients managed by a geriatric team using a day hospital facility versus conventional medical management. RESULTS: Functional improvement (Barthel Index score) was greater in the group managed by the geriatricians with a day hospital facility compared with the conventional group at 3 months (P = .03). There were also fewer outpatient visits among the day hospital patients at 6 months (P = .03). No significant difference was found in costs between the two treatment groups. CONCLUSIONS: Compared with conventional medical management, care in the geriatric day hospital hastened functional recovery and reduced outpatient visits in elderly stroke patients without additional cost. Page33 Jefferson InterProfessional Education Center Bibliography – January 2009 Hunt, M. (2006). Interdisciplinary journal club: An innovative tool for the transfer of knowledge and the promotion of a culture of interdisciplinarity. Journal of Interprofessional Care, 20(2), 196-196-198. In 2004 Schriners Hospital for Children implemented a new Journal Club to act as a forum for increased discussion and awareness of interdisciplinary issues within the hospital. Iezzoni, L. I. (2006). Going beyond disease to address disability. The New England Journal of Medicine, 355(10), 976-979. doi:10.1056/NEJMp068093 This article addresses the responsibility of the physician to go beyond treating disease to treating disability and how doctors should be taught to fulfill this role. Infante, C. (2006). Bridging the "system's" gap between interprofessional care and patient safety: Sociological insights. Journal of Interprofessional Care, 20(5), 517-517-525. Based on a medical sociology approach, this paper analyzes four forces that threaten a well sustained development of research and problem-solving strategic proposals that are to be derived from the intersection of patient safety and interprofessional care. The paper concludes with the proposal of developing theoretically grounded empirical interprofessional research that allows the crucial inclusion of social sciences in the systemic approach. Institute of Medicine. (2008). Retooling for an aging america: Building the health care workforce. Washington, D.C.: National Academies Press. Inventor, B. R., Henricks, J., Rodman, L., Imel, J., Holemon, L., & Hernandez, F. (2005). The impact of medical issues in inpatient geriatric psychiatry. Issues in Mental Health Nursing, 26(1), 23-46. At an advanced age, serious medical and psychiatric illnesses frequently coalesce. Often, the need for admission to inpatient geriatric psychiatric care arises from coexisting medical problems. While cognitive and behavioral interventions are important, the complexity of physical comorbidities usually becomes the focus of hospitalization and requires intensive medical treatments. This paper describes adaptations made in one metropolitan geriatric psychiatry unit in order to better treat complex patients who experience both medical and psychiatric illness. The need for all members of the interdisciplinary team to expand their practice and the importance of complementary approaches of psychiatry and medicine are emphasized. Irajpour, A. (2006). Interprofessional education: A facilitator to enhance pain management? Journal of Interprofessional Care, 20(6), 675-675-678. This review aimed to assess the efficiency of interprofessional education on the pain documentation of professionals and on the pain intensity reported by patients. Two studies demonstrated no significant changes in patient outcomes, while the other revealed significant improvements. Jaber, R., Braksmajer, A., & Trilling, J. S. (2006). Group visits: A qualitative review of current research. Journal of the American Board of Family Medicine : JABFM, 19(3), 276-290. PURPOSE: The group visit model has emerged as one possible solution to problems posed by the limitations of current structures of care and the demands of a growing chronic illness load. In this article, we summarize current group visit research and develop suggestions for furthering this care model. METHODS: An electronic review of all group visit articles published from the years 1974 to 2004 was conducted via the PubMed and MedLine databases. Reference sections of articles thus obtained were mined for additional citations. Articles were excluded if: (1) they were not research studies (ie, purely descriptive, with no evaluative component); or (2) the group visit intervention was subsumed under larger primary or hospital-based interventions. RESULTS: Although the heterogeneity of the studies presented renders the assessment of this care model problematic, there is sufficient data to support the effectiveness of group visits in improving patient and physician satisfaction, quality of care, quality of life, and in decreasing emergency department and specialist visits. CONCLUSION: Group visits are a promising approach to chronic care management for the motivated patient. Future research may benefit, however, from abandoning old nomenclatures and clearly defining the structure, processes of care, content of visits, and appropriate outcome measures. Page34 Jefferson InterProfessional Education Center Bibliography – January 2009 Johnson, A. W., Potthoff, S. J., Carranza, L., Swenson, H. M., Platt, C. R., & Rathbun, J. R. (2006). CLARION: A novel interprofessional approach to health care education. Academic Medicine, 81(3), 252-252-256. This article describes the development of CLARION, a student-run organization at the University of Minnesota which is dedicated to furthering interprofessional education for health professions students. Through engaging students, faculty, and health care professionals, CLARION creates extracurricular and interprofessional experiences for students. This organization has prompted faculty to reexamine traditional health professions curricula. Juntunen, A., & Heikkinen, E. (2004). Lessons from interprofessional e-learning: Piloting a care of the elderly module. Journal of Interprofessional Care, 18(3), 269-269-278. Four Finnish polytechnics providing education for nurses, social workers and physiotherapists wished to develop the content and methods of teaching the care of the elderly by collaboratively creating and implementing an interprofessional module of 15 European Credit Transfer units, using e-learning. This paper examines the planning and assessment of the impact of the pilot module. Karlsson, I., Nilsson, M., & Ekman, S. (2006). Physicians' expectations regarding registered nurses caring for older people living in sheltered housing, retirement homes and group dwellings. Journal of Interprofessional Care, 20(4), 381-381-390. Twelve physicians from two municipalities in Sweden were interviewed. When registered nurses have this skill, the physicians have a "we" feeling towards the nurse. The paper provides insights into the physician-nurse relationship, in the context of residential care in Sweden. Kirkegaard, M. (2004). Medical education and chronic disease. (comment). Journal of the American Medical Association, 292(9), 1057-1057-1059. Dr. Kirkegaard comments on Dr. Holman's article "Chronic disease—the need for a new clinical education" and the seven areas which Holman identifies as necessary for medical students to gain proficiency to manage patients with chronic disease. To this list, he adds two more proficiencies, inspiring students to become advocates for underserved patients and teaching students how to be culturally competent. Klesser, M., McFadden, J., & Bellard, J. C. (2006). An interdisciplinary view of medical pluralism among mexican-americans. Journal of Interprofessional Care, 20(3), 223-223-234. This article highlights the relationship between traditional, complementary, and alternative medicine (TCAM) and biomedicine, and the challenges this relationship poses to patients. Medical professionals tend to represent these systems dualistically - as mutually exclusive and in competition with one another. Patients, on the other hand, tend to make truly pluralistic health care decisions moving freely between TCAM and biomedicine based on what they can access, what they can relate to, and what they believe works. Using their experience with Mexican immigrant and MexicanAmerican populations in Southwestern United States, the authors discuss strengths and weaknesses in both healthcare systems, and how medical dualism can be a significant barrier to effective healthcare. Recent literature on medical pluralism is discussed from the public health (i.e., community) and medical (i.e., provider) perspectives. These two disciplines are brought together in an attempt to deconstruct the notion that TCAM and biomedicine are diametrically opposed healthcare systems. Biomedically trained health care providers must understand, appreciate, and integrate into their practice how their patients make use of other healing practices and beliefs. Such integration is particularly essential when serving immigrant or minority populations as these groups are more likely to use a pluralistic approach in meeting their health needs. Koffman, J., & Higginson, I. J. (2005). Assessing the effectiveness and acceptability of interprofessional palliative care education. Journal of Palliative Care, 21(4), 262-262-269. There is controversy about interprofessional education in health care in general and in palliative care. This evaluation aimed to explore (1) the career progression of former students who attended an interprofessional MSc in palliative care; (2) the activities former students were engaged in as a Page35 Jefferson InterProfessional Education Center Bibliography – January 2009 result of attending the course; and (3) the experience of attending an interprofessional postgraduate course in palliative care. Kripalani, S., Yao, X., & Haynes, R. B. (2007). Interventions to enhance medication adherence in chronic medical conditions: A systematic review. (review). Archives of Internal Medicine, 167(6), 540-540550. Approximately 20% to 50% of patients do not adhere to their medical therapies. A review of the literature was performed to summarize, categorize, and estimate the effect size of interventions to improve medication adherence in chronic medical conditions. The review concluded that several types of interventions are effective in improving medication adherence in chronic medical conditions, but few of them significantly affected clinical outcomes. Kucukarslan, S. N., Peters, M., Mlynarek, M., & Nafziger, D. A. (2003). Pharmacists on rounding teams reduce preventable adverse drug events in hospital general medicine units. Archives of Internal Medicine, 163(17), 2014-2014-2018. It is proposed that having a pharmacist available when patients are evaluated during the rounding process may reduce the likelihood of preventable adverse drug events. The authors evaluated the effectiveness of having a pharmacist participate during rounds in general medicine units and documented their interventions made during the rounding process. It was concluded that pharmacist participation with the medical rounding team on a general medicine unit contributes to a significant reduction in preventable adverse drugs events. Kwan, D., Barker, K., Austin, Z., Chatalalsingh, C., Grdisa, V., Langlois, S., et al. (2006). Effectiveness of a faculty development program on interprofessional education: A randomized controlled trial. Journal of Interprofessional Care, 20(3), 314-314-316. The goal of this study is to assess the effectiveness of education in IPE for clinical faculty who teach and practice in clinical settings. The primary objective is to measure the effectiveness of a Faculty Development Program on Interprofessional Education (FDP-IPE) on the faculty’s knowledge, skills, attitudes (KSA) related to teaching IPE for collaborative practice. Our secondary objective is to create interprofessional clinical placement opportunities for medical trainees and other health professional learners at the University of Toronto. Kyrkjebo, J., Brattebo, G., & Smith-Strom, H. (2006). Improving patient safety by using interprofessional simulation training in health professional education. Journal of Interprofessional Care, 20(5), 507507-516. This paper reports the findings from pilot testing a simulated training program in interprofessional student teams. The findings suggest that the students were satisfied with the program, but some of the videos and simulation exercises could be more realistic and more in accordance with each other. Involving students in interprofessional team training seem to be more likely to enhance their learning process. LaBresh, K. A., Ellrodt, A. G., Gliklich, R., Liljestrand, J., & Peto, R. (2004). Get with the guidelines for cardiovascular secondary prevention: Pilot results. Archives of Internal Medicine, 164(3), 203-203209. Data collection and outcome measures were completed by 24 hospitals on patients admitted to the hospital with coronary artery disease. The following outcome measures were completed at baseline and 10- to 12-month follow-up: aspirin use, beta-blockers, angiotensin-converting enzyme inhibitors, cholesterol management and treatment, smoking cessation counseling, blood pressure control, and cardiac rehabilitation referral. Prevention guideline adherence in hospitalized patients with coronary artery disease was improved with the web program utilization, interactive physician training, and initiation of collaborative quality improvement. Ladden, M. D., Bednash, G., Stevens, D. P., & Moore, G. T. (2006). Educating interprofessional learners for quality, safety, and systems improvement. Journal of Interprofessional Care, 20(5), 497-497-505. Page36 Jefferson InterProfessional Education Center Bibliography – January 2009 Until recently, knowledge and skills necessary for systems improvement in the health professions was not included in formal educational curricula. In addition, interprofessional collaboration was not taught as a means to improve systems. Achieving Competence Today (ACT) was designed as a new model for interprofessional education for quality, safety, and health systems improvement. This paper describes the ACT program and curriculum model and makes recommendations for the future. Lahey, W., & Currie, R. (2005). Regulatory and medico-legal barriers to interprofessional practice. Journal of Interprofessional Care, 19(Supplement 1), 197-197-223. This paper discusses potential legal ramifications of implementing interprofessional practice in Canadian health care. The two major legal issues likely to inhibit health care professionals from working together on an interprofessional basis are: laws under which health care professionals are regulated and the law of professional malpractice. The authors of this paper propose three strategies designed to minimize the risk of malpractice claims due to the legal constructs currently employed by the courts of Canada. Landers, S. H. (2006). Home care: A key to the future of family medicine? Annals of Family Medicine, 4(4), 366-368. doi:10.1370/afm.550 This essay is about my transition from family medicine residency into house call/home-based primary care practice. Though some aspects of making home visits have been difficult and uncomfortable, I have found a higher level of satisfaction and sense of purpose than I had as a resident in a traditional outpatient clinic. This enhanced satisfaction is, in part, due to my discovery that a lower-volume, time-intensive house call practice is a more appropriate way than the brief office visit to care for older patients who have multiple morbidities. In light of the aging population, advances in portable medical technology, and changes in Medicare reimbursement, home care could become a key to the future success and ongoing relevance of family medicine. Lawrence, D. M. (2005). Chronic disease care: Rearranging the deck chairs. (comment). Annals of Internal Medicine, 143(6), 427-427-438. Background: Although enthusiasm is growing for self-management programs for chronic conditions, there are conflicting data regarding their effectiveness and no agreement on their essential components. Purpose: To assess the effectiveness and essential components of self-management programs for hypertension, osteoarthritis, and diabetes mellitus. Conclusions: Self-management programs for diabetes mellitus and hypertension probably produce clinically important benefits. The elements of the programs most responsible for benefits cannot be determined from existing data, and this inhibits specification of optimally effective or cost-effective programs. Osteoarthritis self-management programs do not appear to have clinically beneficial effects on pain or function. Lenz, T., Monaghan, M., Ekeler, J., & Hayes, M. (2006). An interprofessional medication risk assessment program. Journal of Interprofessional Care, 20(5), 558-558-560. This article describes a collaboration between pharmacists and nurses to conduct medication risk assessments on patients viewed as potentially "high risk". Leveille, S. G., Wagner, E. H., Davis, C., Grothaus, L., Wallace, J., LoGerfo, M., et al. (1998). Preventing disability and managing chronic illness in frail older adults: A randomized trial of a community-based partnership with primary care. Journal of the American Geriatrics Society, 46(10), 1191-1198. This study was conducted to evaluate the impact of a 1-year, senior center-based chronic illness self-management and disability prevention program on health, functioning, and healthcare utilization in frail older adults. The trial was conducted at a large senior center in a Seattle suburb in collaboration with primary care providers of two large managed care organizations. A total of 201 chronically ill older adults, aged 70+, were recruited through medical practices. The intervention group recieved a targeted, multi-component disability prevention and disease self-management program led by a geriatric nurse practitioner (GNP). Results show that intervention participants showed less decline in function and lower scores on the Health Assessment Questionnaire. Other Page37 Jefferson InterProfessional Education Center Bibliography – January 2009 measures of function, such as the SF-36 and other physical performance tests, did not change with the intervention. In the intervention group, the number of hospitalizations decreased by 38%, while it rose by 69% among the controls. The intervention also led to significantly higher levels of physical activity and senior center participation and significant reductions in the use of psychoactive medications. The study concludes that "a community-based collaboration with primary care providers can improve function and reduce inpatient utilization in chronically ill older adults. Linking organized medical care with complementary community-based interventions may be a promising direction for research and practice." Lewis, L. (2005). The state of the science: Focus on chronic illness. American Journal of Nursing, 105(2), 27-27-28. Researchers from the University of Pittsburgh School of Nursing have been examining whether the existence of comorbidities influences treatment adherence. Their studies have focused on patients with different chronic conditions, including rheumatoid arthritis (RA), urinary incontinence, hypertension, and HIV. Lewis, R., & Dixon, J. (2004). Rethinking management of chronic diseases. (see comment). British Medical Journal, 328(7433), 220-220-222. Recent organisational changes to the NHS are bound to affect the care of patients with chronic diseases. But will they help or hinder? Chronic disease represents a huge burden of ill health in the United Kingdom and a large cost to the NHS. Yet for many years government policy has focused on improving access to elective care. Recently, attempts have been made to improve the management of selected chronic conditions through the introduction of national service frameworks together with the associated activity of the NHS Modernisation Agency and the national clinical directors. But the NHS still has no agreed model for managing all chronic diseases. We aim to stimulate debate by suggesting some basic ingredients of good management of chronic diseases and examining how recent policies might influence their development and implementation in the NHS in England. Lindqvist, S., Duncan, A., Rout, J., Watts, F., & Pearce, S. (2005). Interprofessional education for undergraduate health care students throughout their training. Journal of Interprofessional Care, 19(2), 175-175-176. Since 1992 The University of Hawaii, John A. Burns School of Medicine has offered communitybased interprofessional training, with the intention that physicians would choose primary care specialties, work in community care settings, and work well as interdisciplinary teams. This study was conducted to look at the effects of CBIT on the choice of career paths for participating students. Lindqvist, S., Duncan, A., Shepstone, L., Watts, F., & Pearce, S. (2005). Case-based learning in cross professional groups- the development of a pre-registration interprofessional learning program. Journal of Interprofessional Care, 19(5), 509-509-520. This paper describes the development and evaluation of an interprofessional learning (IPL) program at the pre-registration level. The aim of the study was to investigate whether case-based learning in cross-professional groups is a feasible and an effective way to conduct interprofessional education (IPE). The findings in this paper reported that the method used in this paper was a feasible and effective way to deliver IPE. Lingard, L., Whyte, S., Espin, S., Baker, G., Orser, B., & Doran, D. (2006). Towards safer interprofessional communication: Constructing a model of "utility" from preoperative team briefings. Journal of Interprofessional Care, 20(5), 471-471-483. This article sought to improve understanding by analyzing the discourse arising from structured preoperative team briefings among surgeons, nurses, and anesthesiologists prior to general surgery procedures. Modeling this pathway is a critical step in promoting change, as it renders visible both the latent dangers present in current team communication systems and the specific ways in which altered communication patterns can impact team awareness and behaviors. Page38 Jefferson InterProfessional Education Center Bibliography – January 2009 Lorente, M., Hogg, G., & Ker, J. (2006). The challenges of initiating a multi-professional clinical skills project. Journal of Interprofessional Care, 20(3), 290-290-301. This paper uses force field analysis to make explicit the challenges experienced by two National Health Service (NHS) organizations on the east coast of Scotland during the initiation phase of a multi-professional clinical skills project. An action research methodology is employed to highlight the strategies adopted by the project team. The authors suggest that gaining insight into the cultural, logistical and educational challenges inherent in such initiatives provides valuable data to plan appropriate strategies to aid project success. Lorenz, R. A., & Pichert, J. W. (1986). Impact of interprofessional training on medical students' willingness to accept clinical responsibility. Medical Education, 20(3), 195-200. Interprofessional training has been suggested as a means of preparing medical students for team health care, but the effects of such training have not been carefully studied. A multidisciplinary training programme in ambulatory diabetes care was developed to promote positive attitudes towards team care. Programme effects were assessed by a questionnaire which asked medical students to indicate their willingness to delegate or share 25 specific clinical tasks with a nurse. Following programme participation, students' willingness to share responsibility increased significantly for seven of the 25 tasks. To test the hypothesis that this effect resulted from the assignment of a teaching role to nurses, selected seminar content was taught by doctors or nurses on a random basis. No differences in willingness to share responsibility were related to which professional taught the seminar content. However, students were more willing to share responsibility with a nurse when they thought they had learned that topic from a nurse, suggesting that their experience in observing nurses at work may have been important in influencing attitudes towards team care. Lorig, K. (2003). Self-management education: More than a nice extra. Medical Care, 41(6), 699-699-701. Self-management education provides patients with the skills to live an active and meaningful life with their chronic conditions. This article looks at self-management interventions such as PRIDE. Lorig, K. (2006). Action planning: A call to action. JABFM, 19(3), 324-324-325. A commentary that examines the concept of action planning, or self-regulation. Lorig, K., Hurwicz, M. L., Sobel, D., Hobbs, M., & Ritter, P. L. (2005). A national dissemination of an evidence-based self -management program: A process evaluation study. Patient Education and Counseling, 59, 69-69-79. While evidence exists regarding the effectiveness of many health education interventions, few of these evidence-based programs have been systematically or widely disseminated. This paper reports on the dissemination of one such intervention, the 6-week-peer-led Chronic Disease SelfManagement Program, throughout a large health-care system, Kaiser Permanente. The authors describe the dissemination process and, using qualitative analysis of interviews and surveys, discuss the factors that aided and hindered this process and make recommendations for similar dissemination projects. Six years after the beginning of the dissemination process, the program is integrated in most of the Kaiser Permanente regions and is being offered to several thousand people a year. Lorig, K., Ritter, P. L., & Gonzalez, V. M. (2003). Hispanic chronic disease self-management. Nursing Research, 52(6), 361-361-369. This study aimed to evaluate the health and utilization outcomes of a 6-week community-based program for Spanish speakers with heart disease, lung disease or type 2 diabetes. At 4 months, the participants as compared with the usual-care control subjects, demonstrated improved health status, health behavior, and self-efficacy, as well as fewer emergency room visits. At one year, the improvements were maintained and remained significantly different from baseline condition. Lorig, K., Ritter, P. L., & Jacquez, A. (2005). Outcomes of border health Spanish/English chronic disease self-management programs. The Diabetes Educator, 31(3), 401-401-409. Page39 Jefferson InterProfessional Education Center Bibliography – January 2009 The purpose of this study was to evaluate the community based Chronic Disease Self-Management Program (CDSMP) and the Spanish-language version (Tomando control de su salud) programs as delivered in settings along the Texas/New Mexico border. The programs had proven effective in randomized trials, and the authors wished to determine if they would be as effective when administered by others to different populations. Participants showed improvements in health behaviors, health status, and self-efficacy at both four month and one year. Baseline self-efficacy and 4 month change in self-efficacy were significantly associated with improved one year outcomes. Lorig, K., Ritter, P. L., Laurent, D. D., & Fries, J. F. (2004). Long-term randomized controlled trials of tailored-print and small-group arthritis self-management interventions. Medical Care, 42(4), 346-346354. The objective of this study was to test the effectiveness of a mail-delivered, tailored selfmanagement interventions (SMART) and to compare it with the classic Arthritis Self-Management Program (ASMP). A mail-delivered arthritis self-management program SMART, was similarly effective to the classic ASMP, with slightly better results in the first year and a slightly more rapid attenuation over the next 2 years. Results suggest that both programs are effective, and that the addition of a mail-delivered program could improve accessibility to arthritis self-management treatment. Lorig, K., Ritter, P. L., & Plant, K. (2005). A disease-specific self-help program compared with a generalized chronic disease self-help program for arthritis patients. Arthritis Rheumatology, 53(6), 950-950-957. Objective: Both the Arthritis Self-Management Program (ASMP) and the generic Chronic Disease Self-Management Program (CDSMP) have been shown to be successful in improving conditions in patients with arthritis. This study compared the relative effectiveness of the 2 programs for individuals with arthritis. Results: Both programs showed positive results. The disease-specific ASMP appeared to have advantages over the more generic CDSMP for patients with arthritis at 4 months. These advantages had lessened slightly by 1 year. Conclusion: The disease-specific ASMP should be considered first where there are sufficient resources and participants. However, both programs had positive effects, and the CDSMP should be considered a viable alternative. Lorig, K., Ritter, P. L., Stewart, A. L., Sobel, D. S., Brown, B. W., Bandura, A., et al. (2001). Chronic disease self-management program: 2-year health status and health care utilization outcomes. Medical Care, 39(11), 1217-1217-1223. This study sought to assess the 1-and2-year health status, health care utilization and self-efficacy outcomes for the Chronic Disease Self-Management Program (CDSMP). The major hypothesis was that during the 2-year period CDSMP participants would experience improvements or less deterioration than expected in health status and reductions in health care utilization. It was found that a low-cost program for promoting health self-management can improve elements of health status while reducing health care costs in populations with diverse chronic diseases. Lumague, M., Morgan, A., Mak, D., Hanna, M., Kwong, J., Cameron, C., et al. (2006). Interprofessional education: The student perspective. Journal of Interprofessional Care, 20(3), 246-246-253. Nine students from seven different health care disciplines associated with the Toronto Rehabilitation Institute participated in an IPE clinical placement in the winter of 2005 on Toronto Rehabilitation's Stroke inpatient unit. These students participated in interprofessional group sessions led by different health care professionals. This paper discusses the students' perspectives on this IPE experience and the corresponding benefits and challenges. MacGregor, K., Handley, M., Wong, S., Sharifi, C., Gjeltema, K., Schillinger, D., et al. (2006). Behaviorchange action plans in primary care: A feasibility study of clinicians. Journal of the American Board of Family Medicine : JABFM, 19(3), 215-223. PURPOSE: Collaborative goal-setting--with clinician and patient together deciding on concrete Page40 Jefferson InterProfessional Education Center Bibliography – January 2009 behavior-change goals-may be more effective in encouraging healthy behaviors than traditional clinician-directed advice. This study explores whether it is feasible for clinicians to engage patients with coronary heart disease (CHD) risk factors in collaborative goal-setting and concrete action planning during the primary care visit. METHODS: Primary care clinicians were trained in goalsetting and action planning techniques and asked to conduct action plan discussions with study patients during medical visits. Clinicians' experiences were documented through post-visit surveys and with questionnaires and semistructured interviews at the end of the study. RESULTS: Fortythree clinicians and 274 patients with CHD risk factors participated in the study; 83% of the patient encounters resulted in a behavior-change action plan. Goal-setting discussions lasted an average of 6.9 minutes. Clinicians rated 75% of the discussions as equally or more satisfying than previous behavior-change discussions, and identified time constraints as the most important barrier to adopting the goal-setting process. CONCLUSIONS: Collaborative goal-setting between clinicians and patients for improved health behaviors is viewed favorably by clinicians in primary care. Time constraints could be addressed by delegating goal-setting to other caregivers. Mackay, S. (2004). The role perception questionnaire (RPQ): A tool for assessing undergraduate students' perceptions of the role of other professions. Journal of Interprofessional Care, 18(3), 289289-302. A systematic review of interprofessional education revealed that there were many weaknesses in the current body of knowledge of interprofessional education outcomes. This paper discusses the range of tools that were found in the literature and describes the production and validation of two questionnaires that can be used as part of an interprofessional evaluation strategy. Madden, T. E., Graham, A. V., Straussner, S. L., Saunders, L. A., Schoener, E., Henry, R., et al. (2006). Interdisciplinary benefits in project MAINSTREAM: A promising health professions educational model to address global substance abuse. Journal of Interprofessional Care, 20(6), 655-655-664. Our purpose was to evaluate the interdisciplinary aspects of Project MAINSTREAM, a faculty development program that trained 39 competitively selected health professional tutors in substance abuse education. Mid-career faculty fellows (tutors) from 14 different health professions across the US dedicated 20% of their academic time for two years to Project MAINSTREAM. Teams of three fellows carried out curricular enhancement and service-learning field project requirements in mentored Interdisciplinary Faculty Learning Groups (IFLGs). Formative and summative evaluations were conducted via written questionnaires and confidential telephone interviews. The importance of interdisciplinary education was rated positively (mean of 3.57 on 1 - 5 scale). Using 18 parameters, fellows preferred interdisciplinary over single disciplinary teaching (means ranged from 3.40 - 4.86), and reported high levels of benefit from their interdisciplinary collaborations (means ranged from 3.53 - 4.56). Fellows reported that interdisciplinary educational collaborations were feasible (3.31) at their home institutions. The majority (63%) said that their trainees, colleagues, supervisors and institutions valued interdisciplinary training either “highly” or “somewhat”, but 22% did not value it. The fellows identified scheduling conflicts (3.46), and lack of faculty rewards (3.46) such as pay or credit toward promotion, as two barriers that they encountered. Mangione, C. M., Gerzoff, R. B., Williamson, D. F., Steers, W. N., Kerr, E. A., Brown, A. F., et al. (2006). The association between quality of care and the intensity of diabetes disease management programs. Annals of Internal Medicine, 145(2), 107-107-116. Little is known about the effectiveness of disease management programs nationwide. This study was conducted to determine whether disease management by physician groups is associated with diabetes care processes, control of intermediate outcomes, of the amount of medication used when intermediate outcomes are above target levels. At the conclusion of the study, disease management strategies were associated with better processes of diabetes care but not with improved intermediate outcomes or level of medication management. Martinen, M., & Freundl, M. (2004). Managing congestive heart failure in long-term care: Development of an interdisciplinary protocol. Journal of Gerontological Nursing, 30(12), 5-12. Congestive heart failure is common among assisted living and nursing home residents. Nationally Page41 Jefferson InterProfessional Education Center Bibliography – January 2009 recognized guidelines for diagnosis and management have been promulgated but are poorly used in clinical practice. This article describes the efforts of one facility to implement an interdisciplinary protocol to improve heart failure care. The protocol addressed identification of residents with heart failure, appropriate use of ACE inhibitors, weight monitoring, resident and family education, and preventive immunization. Following implementation of the guideline, quality indicators were monitored and process improvements addressed. Diagnostic information, use of ACE inhibitors, nursing assessment, and symptom management improved. While episodes of clinical deterioration occurred, most cases were able to be managed in the long-term care setting. Martin-Rodriguez, L. S., Beaulieu, M. D., D'Amour, D., & Ferrada-Videla, M. (2005). The determinants of successful collaboration: A review of theoretical and empirical studies. Journal of Interprofessional Care, 19(Supplement 1), 132-132-147. Successful collaboration in health care teams can be attributed to several determinants, including interactional determinants, organizational determinants, and systemic determinants. This article presents a review of the literature that discusses each of these determinant types and highlights main characteristics of each of these. Then the article presents a "showcase" of Canadian policy initiatives (The Canadian Health Transition Fund) in order to illustrate how these determinants can be utilized in practice. Mason, D. J., & Lewis, L. (2005). The state of the science: Focus on chronic illness. American Journal of Nursing, 105(2), 27-27-28. This article reports on two papers presented at the National Congress on the State of the Science in Nursing Research. The first paper focuses on the adherence to treatment regimens for chronically ill patients and the nurses who treat them. The effect of co-morbidities on the treatment adherence was also examined. The second paper spoke about a team of advance practice nurses who coordinated patient care of chronically critically ill patients for two months after discharge to try to reduce the readmission rate. Mattick, K., & Bligh, J. (2005). An e-resource to coordinate research activity with the readiness for interprofessional learning scale (RIPLS). Journal of Interprofessional Care, 19(6), 604-604-613. This study aimed to create a virtual community of researchers with a shared interest in quantitative studies of interprofessional learning using the Readiness for Interprofessional Learning Scale. An eresource was created to provide access to relevant sources, coordinate research efforts, and promote communication. This paper discusses experiences and observations from the study. Mayor, S. (2005). Case management to be used for people with chronic conditions. British Medical Journal, 330(7483), 112-112. The UK government announced a new healthcare strategy using a community matron - a specially trained nurse - who will act as a case manager in providing care. The role of the community matron will involve designing a personalized care plan, regular monitoring of patients, and initiating care (including writing prescriptions). McCauley, K., & Irwin, R. S. (2006). Changing the work environment in ICUs to achieve patient-focused care: The time has come. (see comment). Chest, 130(5), 1571-1571-1578. Skilled communication and collaboration are essential to transforming work environments. This article discusses a project initiated by the American Association of Critical-Care Nurses (AACN), which seeks to implement patient-focused care. Communication, continuity, and concordance with patients' wishes are all essential to implementing patient-focused care. McCord, C. (2004). Asleep at the switch: Local public health and chronic disease. American Journal of Public Health, 94(12), 2059-2059-2061. This article discusses the need for increased public health activity in addressing chronic disease prevention and control. Page42 Jefferson InterProfessional Education Center Bibliography – January 2009 McEvilly, A., & Kirk, J. (2005). Twenty years of a multidisciplinary paediatric diabetes home care unit. Archives of Disease in Childhood, 90(4), 342-342-345. Twenty years ago a multidisciplinary diabetes home care service was established at Birmingham Children's Hospital to support children with diabetes mellitus within the home environment. Savings achieved by reductions in expensive hospital bed occupancy have more than offset the costs of maintaining the unit. McFadyen, A. K., Maclaren, W. M., & Webster, V. S. (2007). The interdisciplinary education perception scale (IEPS): An alternative remodelled sub-scale structure and its reliability. Journal of Interprofessional Care, 21(4), 433-443. doi:10.1080/13561820701352531 The original 4 sub-scale version of the Interdisciplinary Education Perception Scale (IEPS) was published by Luecht et al. (1990, Journal of Allied Health, 181 - 191). There appears however to be a lack of evidence of the stability of the original instrument and of the test-retest reliability of the items and sub-scales when used with undergraduates. Given that during its development only 143 subjects completed the questionnaire which contained 18 items the generalizability of the instrument should perhaps have been investigated further. The Interprofessional Learning Group (IPL) at Glasgow Caledonian University has been using both the IEPS and the Readiness for Interprofessional Learning Scale (RIPLS) (Parsell & Bligh, 1999, Medical Education, 33, 95 - 100) to monitor changes in attitudes and perceptions of undergraduate students from eight different health and social care programmes. This paper reports the development of an alternative sub-scale model for the IEPS based on a sample of 308 students. Various aspects of the reliability of this revised model based on a subsequent data set of 247 students are also reported. This revised model appears to be stable for use with undergraduate students yielding Cronbach Alpha values for two of the sub-scales greater than 0.80 and test-retest weighted kappa values for items being fair to moderate. McFayden, A., Webster, V., & Macleran, W. (2006). The test-retest reliability of a revised version of the readiness for interprofessional learning scale (RIPLS). Journal of Interprofessional Care, 20(6), 633633-639. The original version of the Readiness for Interprofessional Learning Scale (RIPLS) was published by Parsell and Bligh in 1999. The only aspect of reliability considered by the authors was the internal consistency. A revised version for use with undergraduate students was published in 2005 (McFadyen et al., 2005). This revised version of RIPLS would appear to have good reliability in three of its sub-scales but further research, with larger samples, is required before the fourth sub-scale can be reliably assessed. McNair, R., Stone, N., Sims, J., & Curtis, C. (2005). Australian evidence for interprofessional education contributing to effective teamwork preparation and interest in rural practice. Journal of Interprofessional Care, 19(6), 579-579-594. A pilot interprofessional education (IPE) placement for undergraduate health care professional students was implemented in Australia from 2001 to 2003. This article outlines the educational model used and focuses on the evaluation methods and results obtained from the student evaluations. The placement experience improved self-reported teamwork skills and knowledge, and supported participating students' belief in the value of interprofessional practice. McNair, R. P. (2005). The case for educating health care students in professionalism as the core content of interprofessional education. Medical Education, 39, 456-456-464. This article discusses the role of interprofessional education in preparing all health care professional students for the workforce. Interprofessional education provides appropriate methods for learning interprofessionalism, which will ultimately contribute to overcoming uni-professional exclusivity. Melin, A. L., Wieland, D., Harker, J. O., & Bygren, L. O. (1995). Health outcomes of post-hospital in-home team care: Secondary analysis of a swedish trial. Journal of the American Geriatrics Society, 43(3), 301-307. This study was conducted to determine patient and treatment-related factors predictive of health Page43 Jefferson InterProfessional Education Center Bibliography – January 2009 outcomes. Hospital inpatients stable for discharge from acute care, having at least one chronic condition, and dependent in 1 to 5 Katz activities of daily life (ADLs) were randomized to "team" (n = 150) or "usual care" (n = 99). Team patients were eligible for in-home primary care by an interdisciplinary team that included a physician, physical therapist, and 24-hour nursing services and geriatric consultation where necessary. "Usual-care" patients received standard district nurseadministered services at home upon hospital discharge. Mendes, D. L., & Carlos, F. (2007). Aging and the elapse of time: A comment on the analysis of change. Journals of Gerontology, 62(3), S198-S198-202. Meuser, J., Bean, T., Goldman, J., & Reeves, S. (2006). Family health teams: A new canadian interprofessional initiative. Journal of Interprofessional Care, 20(4), 436-436-438. This article describes an initiative to establish interdisciplinary healthcare teams (Family Health Teams) made up of family physicians, nurses, pharmacists, social workers and other healthcare professionals. Due to the diversity of populations across Ontario, each FHT would develop a team of professionals to address health needs of their particular locality. Goals of the FHT include the provision of patient-centred care, improved access to care from a variety of health care professionals, helping patients navigate their way through the health care system, and an increased emphasis on chronic disease management, health promotion, and disease prevention. Michaud, P. A., Suris, J. C., & Viner, R. (2004). The adolescent with a chronic condition. part II: Healthcare provision (review). Archives of Disease in Childhood, 89(10), 943-943-949. There are specific issues that arise when treating chronic conditions among adolescents. This paper discusses disclosure of the diagnosis, management of adherence to therapy, the need for an interdisciplinary network approach, lifestyles' anticipatory guidance and prevention, and the transition into an adult health care setting. Mikhail, N., & Cope, D. (2005). Primary care-based disease management for patients with diabetes (comment). American Journal of Medicine, 118(3), 1444-1444-1445. The authors provides comments on Rothman et al's "A randomized trial of a primary care-based disease management program to improve cardiovascular risk factors and glycated hemoglobin levels in patients with diabetes." Miller, A. R., Recsky, M. A., & Armstrong, R. W. (2004). Responding to the needs of children with chronic health conditions in an era of health services reform. (see comment). Canadian Medical Association Journal, 171(11), 1366-1366-1367. Though recommendations have been made supporting efforts to reduce the impact of chronic conditions on children's health and on their families, adoption by the Canadian health system has been minimal. The author discusses opportunities for the health system to take action to address the health needs of children with chronic conditions. Mitchell, P. H., Belsa, B., Schaad, D. C., Robbins, L. S., Gianola, F. J., Odegard, P. S., et al. (2006). Working across the boundaries of health professions disciplines in education, research, and service: The university of washington experience. Academic Medicine, 81(10), 891-891-896. The Institute of Medicine has a vision for health professions education to work collaboratively as a means to provide patient-centered care and as a means to improve the quality of care. The article addresses the questions: how can medical schools work with other health-sciences schools to promote their educational, research, and service missions? Strategies are also suggested for other institutions seeking to implement an interprofessional health sciences program. Mitchell, P. H., Robins, L. S., & Schaad, D. Creating a curriculum for training health profession faculty leaders. Advances in Patient Safety, 4, 299-299-312. An interprofessional, collaborative group of educators, patient safety officers, and federal program Page44 Jefferson InterProfessional Education Center Bibliography – January 2009 directors teamed together to create an integrated, patient safety-centered curriculum for the education of health professional faculty leaders. The team surveyed existing educational tools and materials and then synthesized materials about patient safety and interprofessional collaboration to provide faculty with tools for assessing and improving their current teaching practices that influence patient safety. Mitka, M. (2006). Less may be more when managing patients with severe chronic illness. JAMA : The Journal of the American Medical Association, 296(2), 159-160. doi:10.1001/jama.296.2.159 While conventional wisdom states that care for older patients with chronic diseases is best performed by specialty physicians in acute care settings such as academic medical centers, a new report suggests otherwise. Researchers with the Center for the Evaluative Clinical Sciences at Dartmouth Medical School in Hanover, NH, reported that medical costs varied across the nation but that quality of care is not necessarily linked to higher-cost care. For more than a decade, these researchers have been studying and issuing reports showing such variation, but this study shows for the first time differences among specific hospitals and their physician networks. These differences in cost, visits to specialists, days in the hospital, and use of intensive care beds exist after controlling for illness severity. Mole, L., Scarlett, V., Campbell, M., & Themessl-Huber, M. (2006). Using a simulated chaotic home environment for preparing nursing and social work students for interdisciplinary care delivery in a scottish context. Journal of Interprofessional Care, 20(5), 561-561-563. Based in the Clinical Skills Centre within the Faculty of Medicine, Dentistry and Nursing the three-hour workshop used a scenario for simulating a chaotic home environment of an older client with multiple health and social problems. A disorderly, dirty simulated home environment is created for students to collaboratively assess the elderly person’s health and social care needs...The hazards are placed as triggers to alert students to potential health and safety concerns when carrying out a client assessment. Morioka-Douglas, N. (2004). Medical education and chronic disease. (comment). Journal of the American Medical Association, 292(9), 1057-1057-1059. Dr. Morioka-Douglas comments that part of the lack of medical education in addressing chronic illness involves the lack of reimbursement for activities essential to management of chronic disease, such as telephone snd email consultation. Moskowitz, D., Glasco, J., Johnson, B., & Wang, G. (2006). Students in the community: An interprofessional student-run free clinic. Journal of Interprofessional Care, 20(3), 254-254-259. Students in the Community (SITC) is an interprofessional collaboration of health science students at the University of Washington. SITC runs a weekly free clinic at the Aloha Inn, a transitional housing facility for 70 homeless men and women in downtown Seattle. The focus of this clinic is on health education, chronic disease management, and re-integration of patients into the healthcare infrastructure. SITC serves as a valuable service learning opportunity for students. In addition to direct clinical services, students gain experience in planning health education strategies, community collaboration, and evaluating intervention outcomes. SITC also oversees a lecture and discussionbased elective course at the University of Washington focused on health issues of the homeless community and provides formal teaching which complements the service-learning component of the endeavor. Murray, S. (2006). Doubling the burden: Chronic disease. Canadian Medical Association Journal, 174(6), 771-771. This author discusses the implications of chronic disease, not just in wealthy countries, but in middle- and low-income countries as well. She discusses the shift in nutrition and lifestyle as contributing to rising rates of obesity and contributing to illness. Also, she discusses the government's and individual's roles in healthy lifestyle choices. Page45 Jefferson InterProfessional Education Center Bibliography – January 2009 Murray, S., Boyd, K., & Sheikh, A. (2005). Palliative care in chronic illness. (see comment). British Medical Journal, 330(7497), 963-963. These authors discuss the need for and importance of proactive approaches to palliative care in those with chronic illnesses. Naglie, G., Tansey, C., Kirkland, J. L., Ogilvie-Harris, D. J., Detsky, A. S., Etchells, E., et al. (2002). Interdisciplinary inpatient care for elderly people with hip fracture: A randomized controlled trial. CMAJ : Canadian Medical Association Journal = Journal De l'Association Medicale Canadienne, 167(1), 25-32. THis study was conducted to determine the efficacy of postoperative interdisciplinary care, compared to usual care, in elderly patients with hip fracture. The study found that interdisciplinary care did not result in better 3 or 6 month outcomes in patients with hip fracture. Nair, B. R., & Finucane, P. M. (2003). Reforming medical education to enhance the management of chronic disease. The Medical Journal of Australia, 179(5), 257-259. Medical education must adapt to change if it is to remain relevant to the needs of doctors, patients and society. Ideally, it should anticipate and lead change. Undergraduate education remains rooted in urban medical schools where the focus is on acute disease, while most graduates spend their working lives in the community, dealing mainly with chronic health problems. Medical graduates need to acquire specific knowledge, skills and attitudes if they are to effectively manage people with chronic disease. Strategies that create a better balance between education in acute and chronic disease are being developed. These include a transfer of clinical teaching to community and nursing home settings and the development of interdisciplinary teaching. National Association of Chronic Disease Directors. (2006). Educating professionals for public health impact: Competencies for chronic disease practice professionalsConcept Systems, Inc. Nazem, A. G. (2008). A piece of my mind. teach us how. JAMA : The Journal of the American Medical Association, 300(21), 2463-2464. doi:10.1001/jama.2008.767 Commentary by a third-year medical student on medical education and the US healthcare system. Nelson, J. E., Meier, D. E., Litke, A., Natale, D. A., Siegel, R. E., & Morrison, R. S. (2004). The symptom burden of chronic critical illness. (see comment). Critical Care Medicine, 32(7), 1527-1527-1534. The purpose of this study was to assess self-reported symptom burden of chronic critical illness among individuals on a respiratory care unit. Physical and psychological symptom distress is common and severe among patients receiving treatment for chronic critical illness. Due to the high mortality rate observed in the study, greater attention should be given to relief of pain and other distressing symptoms for the chronically critically ill. Nishtar, S. (2006). Lessons in tackling chronic disease. (see comment). British Medical Journal, 333(7573), 820-820. The author discusses the impact of chronic illness in Eastern Mediterranean Region. She suggests ways in which policymakers can promote lifestyle changes, such as amending essential drug lists to include those to treat chronic diesases, changing the nutrition education froma focus on undernutrition to focus on obesity, and government programs which have been successful throughout the region. Norman, J. (2005). Managing chronic diseases: Funding follow-up is key to long term specialist care. (comment). British Medical Journal, 330(7497), 964-964. This author comments that new NHS funding policies for follow-up care in primary and secondary care settings will be necessary for patients to recieve adequate chronic illness care. Norris, S. L., & Olson, D. E. (2004). Implementing evidence-based diabetes care in geriatric populations. the chronic care model. Geriatrics, 59(6), 35-35-39. Page46 Jefferson InterProfessional Education Center Bibliography – January 2009 This article discusses the chronic care model as a means to provide a framework for change in the practice and organization of care for chronic illnesses, specifically diabetes. Norris, T. E., House, P., Schaad, D., Mas, J., & Kelday, J. M. (2003). Student providers aspiring to rural and under served experiences at the university of washington: Promoting team practice among the health care professions. Journal of Medical Education, 78(12), 1211-1211-1216. The University of Washington's Area Health Education Center program and School of Medicine offer a voluntary extracurricular program for students. The Student Providers Aspiring to Rural and Underserved Experiences (SPARX) programs is an interprofessional, student-operated, center/schoolsupported program consisting of a wide range of activities. SPARX supports students interested in practicing among rural and urban medically under-served patients and in interacting with their peers in other health professions schools. Nusselder, W. J., Looman, C. W., Mackenbach, J. P., Huisman, M., Van Oyen, H., Deboosere, P., et al. (2005). The contribution of specific diseases to educational disparities in disability-free life expectancy. American Journal of Public Health, 95(11), 2035-2035-2041. This study sought to examine the contribution that specific diseases, as causes to both death and disability, make to educational disparities in disability-free life expectancy (DFLE). The study concluded that disabling diseases such as arthritis, back complaints, and asthma/COPD contribute substantially to differences in DFLE by education. Public health policy should focus on these nonfatal diseases in addition to fatal diseases. Oandasan, I., & Reeves, S. (2005). Key elements of interprofessional education. part 2: Factors, processes and outcomes. Journal of Interprofessional Care, 19(Supplement 1), 39-39-48. This paper is the second of two papers which discusses the key elements of Interprofessional Education (IPE). It is based on a literature review conducted for Health Canada relating to its "Interprofessional Education for Patient Centered Practice (IECPCP) initiative. This paper discusses micro level, meso level, and macro level factors that influence the success of an IPE initiative. The paper also discusses outcome measurements that can be used within the IPE framework. Ofman, J. J., Badamgarav, E., Henning, J. M., Knight, K., Gano, A. D., Levan, R. K., et al. (2004). Does disease management improve clinical and economic outcomes in patients with chronic diseases? A systematic review. (review). American Journal of Medicine, 117(3), 182-182-192. The purpose of this review was to assess the clinical and economic effects of disease management in patients with chronic diseases. Disease management programs were found to be associated with marked improvements in many different processes and outcomes of care. O'Neill, B. J., & Wyness, M. A. (2005). Student voices on an interprofessional course. Medical Teacher, 27(5), 433-433-438. This qualitative study examined students' insights regarding the interprofessional component of an elective course offered. Interviews explored perceptions regarding learning, including insights about the effectiveness of teaching-learning strategies, and improvements required. The course contributed to the students' development of their own professional voices and their understanding of those of other professions. Osborne, R. H., Hawkins, M., & Sprangers, M. A. (2006). Change of perspective: A measurable and desired outcome of chronic disease self-management intervention programs that violates the premise of preintervention/postintervention assessment. Arthritis & Rheumatism, 55(3), 458-458465. This study was conducted to determine if participants in chronic disease self-management courses have a change of perspective of their health status, and if this is measurable with a paper-based questionnaire. This study suggests that pre-intervention/post-intervention assessments of interventions such as self-management courses are confounded by a change in perspective of a large proportion of respondents. Page47 Jefferson InterProfessional Education Center Bibliography – January 2009 Packard, E. (2007). Team building: A better approach to elderly care. Monitor on Psychology, 38(9), 1-12. Retrieved from http://www.apa.org/monitor/oct07/teambuilding.html This brief paper explains key elements to improving health-care treatment for older adults. Key concepts include: being sensitive to ageism, knowing other team members' roles, knowing that conflict among team members is inevitable, preparing to work in virtual teams, being culturally aware, and assessing and re-assessing treatment progress and goals. Page, S., & Meerabeau, L. (2004). Hierarchies of evidence and hierarchies of education: Reflections on a multiprofessional education initiative. Learning in Health and Social Care, 3(3), 118-118-128. This article draws on the the experience of facilitating multi-professional groups undertaking a research appraisal skills program within the National Health Service based 'classroom' settings. The continuing existence of both medical dominance in the health care arena and a belief in a hierarchy of evidence was apparent from the courses. In addition, what might be called a hierarchy of educational backgrounds, presented some complex dynamics within the teaching situation and raised a number of hitherto seemingly un-addressed questions for the group of facilitators. Parker-Oliver, D., Bronstein, L. R., & Kurzejeski, L. (2005). Examining variables related to successful collaboration on the hospice team. Health & Social Work, 30(4), 279-286. Although social work participation on interdisciplinary teams is long-standing, little research has been done to examine its effectiveness. This study used the Index of Interdisciplinary Collaboration to explore relationships between selected variables and teamwork in the hospice setting.The findings indicate that hospice social workers report a high level of interdisciplinary collaboration with colleagues. Whereas education, hospice census, the presence of other social workers, and quality of care were found to be unrelated to overall levels of collaboration, individual items measuring collaboration proved to be linked with hospice census, the presence of other social workers on the team, and quality of care. Further research is required to investigate other possible related variables and their impact on successful interdisciplinary collaboration and service delivery. Patel, U. D., & Davis, M. M. (2006). Physicians' attitudes and practices regarding adherence to medical regimens by patients with chronic illness. Chronic Illness, 45(5), 439-439-445. This article discusses a study which sought to explore how physicians determine medical regimen adherence among patients with chronic illnesses. An internet-based survey was completed by twohundred seventeen physicians which sought to determine if prior physician training on the matter had an impact on patient adherence. Formal educational interventions may improve adherencerelated knowledge and skills. Pearson, D., & Pandya, H. (2006). Shared learning in primary care: Participants' views of the benefits of this approach. Journal of Interprofessional Care, 20(3), 290-290-301. This is a study exploring participants' views regarding a series of shared or interprofessional learning sessions carried out in a primary care setting in Bradford, UK. It was concluded that shared or interprofessional learning in the workplace is valued by clinicians, can help improve understanding of professional roles and also enhance clinical learning. Pearson, S., Inglis, S. C., McLennan, S. N., Brennan, L., Russell, M., Wilkinson, D., et al. (2006). Prolonged effects of a home-based intervention in patients with chronic illness. Archives of Internal Medicine, 166(6), 645-645-650. A long-term follow-up of a previously published randomized trial was conducted which compared allcause mortality and recurrent hospitalization during the median follow-up of 7.5 years in a heterogeneous cohort of patients with chronic illness initially exposed to a multidisciplinary, homebased intervention. This study suggests that a nonspecific home-based intervention provides longterm cost benefits in a range of chronic illnesses, except for chronic obstructive pulmonary disease. Pham, H. H., Simonson, L., Elnicki, D. M., Fried, L. P., Goroll, A. H., & Bass, E. B. (2004). Training U.S. medical students to care for the chronically ill. Academic Medicine, 79(1), 32-32-40. The prevalence of chronic illnesses is increasing and therefore it will be increasingly important for Page48 Jefferson InterProfessional Education Center Bibliography – January 2009 physicians and medical students to understand chronic illnesses and appropriate care during their training. A survey of medical school course directors revealed that overall the directors agreed on the need to address the improvement of training students in the care of the chronically ill, however, the directors reported a wide variety of methods for how they would like to address or are currently addressing this in their courses. Phelan, A., Barlow, C., & Oversem, S. (2006). Occasioning learning in the workplace: The case of interprofessional peer collaboration. Journal of Interprofessional Care, 20(4), 415-415-424. In this study, we explore the potential of peer collaboration as a means of promoting continuous learning at work. This study suggests that unstructured but focused conversations about daily practice, among close colleagues from other professions, can yield surprising possibilities for learning. Phelan, H. H., Simonson, L., Elnicki, M. D., Fried, L. P., Goroll, A. H., & Bass, E. B. (2004). Training U.S. medical students to care for the chronically ill. Journal of the Association of American Medical Colleges, 79(1), 32-32-41. The authors assessed the inclusion of competencies in the curriculum in relation to chronically ill patients. Directors of medical school courses were interviewed about the use of chronic care competencies and their opinion of importance of these competencies in their course. The course directors agreed about the important of chronic care competencies, but there was much variation found in the execution of these competencies in their courses. Phelan, E. A., Williams, B., LaCroix, A. Z., Grothaus, L., LoGerfo, J. P., & Wagner, E. H. (2004). Effects of provider practice on functional independence in older adults. Journal of the American Geriatrics Society, 52(8), 1233-1239. doi:10.1111/j.1532-5415.2004.52350.x This observational study was designed to examine provider determinants of new-onset disability in ADLs in community-dwelling elderly. A random sample of HMO enrollees age 65 and older participating in a longitudinal study of dementia and aging and their primary care providers formed the study population. New onset of ADL disability were examined in relation to provider characteristics and practice style. Results showed that neither provider experience in caring for elderly patients or having a certificate of qualifications in geriatrics was associated with patient disability at 2 or 4 years. A practice style embodying traditional geriatric principles of care was not associated with a reduced likelihood of ADL disability over 4 years of follow-up. The authors conclude that taking care of a large number of elderly patients, obtaining a certificate of added qualifications in geriatrics, and practicing with a traditional geriatric orientation do not appear to influence the development of ADL disability in elder, community dwelling HMO enrollees. Philippon, D. J., Pimlott, J. F. L., King, S., Day, R. E., & Cox, C. (2005). Preparing health science students to be effective health care team members: The interprofessional initiative at the university of alberta. Journal of Interprofessional Care, 19(3), 195-195-206. This paper describes the evolution of the University of Alberta's Interprofessional Initiative over the past decade and describes future directions. More specifically, attention is given to the administrative and academic structures and processes required to launch, develop, and sustain an initiative such as this. Phipps, L. L., & Cuthill, J. D. (2002). Breaking bad news: A clinician's view of the literature. Annals (Royal College of Physicians and Surgeons of Canada), 35(5), 287-293. In daily practice, a clinician may have to break bad news to patients and their families. How the patient responds depends largely on the manner in which the messenger conveys the news. The clinician may harbour fears of the patient's unpredictable emotional reactions, his or her own display of emotions, and a revival of bad news that he or she may have received. He or she may also feel ineffectual about an inability to deal with the patient's expectations for cure. He or she may use distancing tactics in discussing emotionally charged topics. The ensuing anxiety fosters an uneasy alliance in such situations. Moreover, the patient may question the information. This should be seen as a need for more information, and not as a challenge to the messenger's integrity or the validity of Page49 Jefferson InterProfessional Education Center Bibliography – January 2009 the news. Denial on the part of patients and families may indicate their inability to accept the news. The paucity of medical education in this area dictates more emphasis in teaching communication skills to medical students and postgraduate trainees. Receiving the news is the start of an adaptation process for a patient. He or she must know that there will be difficulties ahead. The patient and family will face them together with the clinician. The doctor will be available as necessary throughout the process to answer questions and provide support. This entails spending time to listen, hear, acknowledge the patient's emotions, and advocate on the patient's behalf. It is always possible to help the patient frame his or her fears. When the shadow of death approaches, life and time become more precious. Deeper meanings and clearer priorities often emerge for the dying person. He or she is forced to examine what makes a life meaningful. By sharing burdens, insight, and support, patients and professionals can pursue these discoveries together. Pierre, J. S. (2005). Delirium: A process improvement approach to changing prescribing practices in a community teaching hospital. Journal of Nursing Care Quality, 20(3), 244-50; quiz 251-2. An interdisciplinary continuous process improvement team developed an educational intervention for physicians, nurses, and other healthcare professionals that focused on the role of medications in the etiology of delirium among hospitalized patients aged 65 years and older. An analysis of prescribing practices after the educational intervention revealed a reduction in the use for 57% of the drugs targeted. Other outcomes from this process improvement methodology are also examined. Piette, J. D., Heisler, M., & Wagner, T. H. (2004). Cost-related medication underuse among chronically ill adults: The treatments people forgo, how often, and who is at risk. American Journal of Public Health, 94(10), 1782-1782-1787. This study sought to understand which medications are underused, by whom, and how often among chronically ill adults. These adults were asked to identify how often they underused prescriptions because of cost. Many chronically ill adults frequently cut back on medications as a result of cost. Placentra, M. Cost of chronic disease | philadelphia inquirer | 02/12/2008. Retrieved 10/30/2008, 2008, from http://www.philly.com/inquirer/gallery/15573857.html Platt, H. (2005). Managing chronic diseases: Condition based payment may improve care of chronic illness in canada. (comment). British Medical Journal, 330(7497), 964-964. This author comments on by DiPiero and Sanders', "Condition based payment: improving care of chronic illness." He describes the impact of chronic care practice enhancement payments instituted in British Columbia. Pollard, K., Miers, M., Gilchrist, M., & Sayers, A. (2006). A comparison of interprofessional perceptions and working relationships among health and social care students: The results of a 3-year intervention. Health & Social Care in the Community, 14(6), 541-541-552. Abstract: A longitudinal quantitative study in an English faculty of health and social care explored the effects of a pre-qualifying interprofessional curriculum for students from 10 professional programs. Students on the interprofessional curriculum completed questionnaires containing four attitude scales on entry to the faculty, during their second year and at the end of their final year. These data suggest that experiencing an interprofessional curriculum has an effect on students' attitudes at qualification, particularly with regard to their positive perception of their own professional relationships. Pollard, K., Miers, M. E., & Gilchrist, M. (2005). Second year skepticism: Pre-qualifying health and social care students' midpoint self-assessment, attitudes and perceptions concerning interprofessional learning and working. Journal of Interprofessional Care, 19(3), 251-251-268. A study in an English Faculty of Health and Social Care explores the effects of a pre-qualifying interprofessional curriculum incorporating interprofessional modules in each year of study. This paper represents results from 723 students at the second data collection point. The emergence of differences in responses based on a a professional program suggest that interprofessional education may not necessarily influence professional socialization. Page50 Jefferson InterProfessional Education Center Bibliography – January 2009 Priest, H., Sawyer, A., Roberts, P., & Rhodes, S. (2005). A survey of interprofessional education in communication skills in health care programmes in the UK. Journal of Interprofessional Care, 19(3), 236-236-250. Interprofessional education (IPE) is advocated as one way of improving health care communication for the development of interprofessional care. A multidisciplinary and cross university project was designed to identify opportunities for, and best practice in, IPE communication skills amongst undergraduate health care practitioners within one Workforce Development Directorate (WDD) in England. Based on the findings, recommendations are made for the planning, implementation, and evaluation of IPE in communication skills. Priest, M. L., & Ginwright, S. S. (2006). Bridge to health care: Alabama's health professionals partnership initiative. Academic Medicine, 81(6), 517-517-520. Further growth in minority graduates from UAB health professions schools is highly unlikely unless the resources of several organizations are brought to bear on the flow of students through earlier segments of the academic pipeline. It is equally important to chance the culture such that the faculty, students and administrators recognize that investing their time, effort, and funds in minority students is not only a humanitarian but also an educationally and economically sound investment. The principles and framework for interdisciplinary collaboration in primary health care.(2006). Enhancing Interdisciplinary Collaboration in Primary Health Care, , 1-1-7. This article discusses how Canada's Enhancing Interdisciplinary Collaboration in Primary Health Care (EICP) Initiative seeks to create conditions for health professionals to work together in the most effective and efficient way in order to produce the best health outcomes for individuals and their families. The article explores principles of interdisciplinary collaboration in primary health care, the EICP framework, health and human resources, funding, liability, regulation, information and communications technology, management and leadership, and planning and evaluation. Pruitt, S. D., & Epping-Jordan, J. E. (2005). Preparing 21st century global healthcare workforce. British Medical Journal, 330(7492), 637-637-639. To meet the growing global demands of caring for the increasing numbers of patients with chronic conditions, we need to develop a new approach to training. Traditional models of acute care are inadequate for training a workforce to manage today' most prevalent health problems: chronic conditions. Purden, M. (2005). Cultural considerations in interprofessional education and practice. Journal of Interprofessional Care, 19(Supplement 1), 224-224-234. Promoting cultural competency in health care was examined from the Canadian perspective, which explored practice environments and educational programs for future health professionals that foster cultural awareness and support culturally sensitive care. The main theme that was generated was the use of a participatory action approach to foster collaboration with patients, traditional healers, and the community. Interprofessional teams should not only comprise partners from all available health professions, but should also include aboriginal paraprofessionals. Quality of medical care gets better, not worse, when patients have more chronic illnesses. Retrieved 8/16/2007, 2007, from http://www.rand.org/congress/newsletters/health/2007/07/quality.html This website reviews a RAND corporation study which is the first large scale assessment of quality of care in patients with multiple chronic conditions. It reviews the article "Relationship between number of medical conditions and quality of care", by Takashiro et al (2007), which can be found in this database. Quam, L., Smith, R., & Yach, D. (2006). Rising to the global challenge of the chronic disease epidemic. Lancet, 368(9543), 1221-1221-1223. The authors comment on efforts to grasp opportunities to decrease deaths from chronic disease. The challenge, they say, is to get the international funders of action against infectious disease to fund action against chronic disease. Page51 Jefferson InterProfessional Education Center Bibliography – January 2009 Rabow, M. W., Dibble, S. L., Pantilat, S. Z., & McPhee, S. J. (2004). The comprehensive care team: A controlled trial of outpatient palliative medicine consultation. Archives of Internal Medicine, 164(1), 83-83-91. This study sought to determine whether palliative care is used by outpatients who continue to pursue treatment for their underlying disease or whether outpatient palliative medicine consultation teams improve clinical outcomes. This study was a year-long controlled trial involving 50 intervention patients and 40 control patients. The study concluded that consultation by a palliative medicine team led to improved patient outcomes in dyspnea, anxiety, and spiritual wellbeing, but failed to improve pain or depression. Ramirez-Cacho, W. A., Strickland, L., Beraun, C., Meng, C., & Rayburn, W. F. (2007). Medical students' attitudes toward pregnant women with substance use disorders. American Journal of Obstetrics and Gynecology, 196(1), 86.e1-86.e5. doi:10.1016/j.ajog.2006.06.092 OBJECTIVE: The objective of this study was to determine whether medical students' attendance at a clinic designed for pregnant substance users would yield changes in their attitudes toward the special needs of this population. STUDY DESIGN: This prospective study involved 104 consecutive third-year students rotating on our obstetrics-gynecology clerkship. Students were assigned to attend either a half day prenatal clinic designed specifically for women with substance use disorders during the first 4 weeks (study group) or during the second 4 weeks (control group). Each answered a confidential 24-question survey (using a 5-point scale from "strongly agree" to "strongly disagree"), dealing with comfort levels and attitudes, at the beginning and midway points of the 8-week clerkship. Student t tests were used for comparisons of averaged scores. RESULTS: At the beginning of the clerkship, no differences were found between the study (n = 52) and control groups (n = 52) in their responses to the survey. Regardless of gender, students who attended the clinic reported they became more comfortable in talking with patients about their substance use (P < .001) and more nonjudgmental in treating these patients (P < .02). Compared with before the clerkship, the control group became less comfortable in talking with these patients about their habits (P < .01), less aware about the prevalence of substance abuse during pregnancy (P < .02), and less aware about the efficacy of counselors (P < .05). CONCLUSION: Medical students became more comfortable and better informed about pregnant women with substance use disorders after attending a clinic dedicated toward this population's special needs. Rand Corporation. Quality of medical care gets better, not worse, when patients have more chronic illnesses. Retrieved August 16, 2007, from http://www.rand.org/congress/newsletters/health/2007/07/quality.html According to a study completed by the Rand Corporation, patients with multiple chronic illnesses do not receive worse quality of medical care than those without multiple chronic illnesses. Three groups of patients were examined to determine whether they received recommended medical care for a variety of common chronic illnesses. The study found that the likelihood that patients received recommended care increased by about two percent with each additional chronic illness. Reeves, S., Zwarenstein, M., Goldman, J., Barr, H., Freeth, D., Hammick, M., et al. (2008). Interprofessional education: Effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews (Online), (1)(1), CD002213. doi:10.1002/14651858.CD002213.pub2 Literature review to assess the effectiveness of IPE interventions and educational programs in which the same health and social care professioals learn separately; and to compare the effectiveness of IPE interventions compared to no educational intervention. Remington, T. L., Foulk, M. A., & Williams, B. C. (2006). Evaluation of evidence for interprofessional education. American Journal of Pharmaceutical Education, 70(3), 66-66. This article summarizes literature relevant to implementing interprofessional training programs in a way that will be most useful for clinician educators. Thirteen studies were identified. Interventions varied widely in intensity and design. Page52 Jefferson InterProfessional Education Center Bibliography – January 2009 Robins, L., Ambrozy, D., & Pinsky, L. E. (2006). Promoting academic excellence through leadership development at the university of washington: The teaching scholars program. Academic Medicine, 81(11), 979-979-983. The University of Washington Teaching Scholars Program (TSP) was established in 1995 to prepare faculty for local and national leadership and promote academic excellence by fostering a community of educational leaders. The curriculum is developed collaboratively and covers key topics such as the following: history of health professions education, learning theories, educational research methods, assessment, curriculum development, instructional methods, professionalism, and leadership. Rodehorst, T. K., Wilhelm, S. L., & Jensen, L. (2005). Use of interdisciplinary simulation to understand perceptions of team members' roles. Journal of Professional Nursing : Official Journal of the American Association of Colleges of Nursing, 21(3), 159-166. The aim of this study was to examine the effectiveness of an interdisciplinary approach to learning in helping care providers understand their overlapping roles in the clinical management of asthma. In addition, the perceived usefulness of an interdisciplinary approach for students in the health-care disciplines of nursing, medicine, pharmacy, and respiratory therapy to learn about the clinical management of asthma was explored. The diffusion of innovation framework was used to guide the process of development of CD-ROMs. An interpretative approach was selected for this research because of the emphasis on how a phenomenon is perceived and how meaning is constructed in situations. This approach assumes that multiple ways of interpreting experiences are available through interaction. A convenience sample of health-care practitioners from two rural campuses was selected to participate in this study. The cohort of participants represented students from the population of a large midwestern moderate-sized university that has four geographically distinct campuses. Preliminary results indicate that the use of interdisciplinary learning helps clarify the roles of each discipline and that learning from one another is enhanced. Rodin, M., Saliba, D., Brummel-Smith, K., American Geriatrics Society Clinical Practice Committee, & Department of Veterans Affairs/Department of Defense. (2006). Guidelines abstracted from the department of veterans Affairs/Department of defense clinical practice guideline for the management of stroke rehabilitation. Journal of the American Geriatrics Society, 54(1), 158-162. doi:10.1111/j.1532-5415.2005.00570.x OBJECTIVES: To assist facilities in identifying those evidence-based processes of poststroke care that enhance measurable patient outcomes. The guideline(s) should be used by facilities (hospitals, subacute-care units and providers of long-term care) to implement a structured approach to improve rehabilitative practices and by clinicians to determine best interventions to achieve improved patient outcomes. OPTIONS: The guideline considers five elements of poststroke rehabilitation care: interdisciplinary teams; use of standardized assessments; intensity, timing, and duration of therapy; involvement of patients' families and caregivers in decision-making; and educational interventions for patients, families, and caregivers. Evidence, benefits, harms, and recommendations for each of the five designated elements and specific annotated recommendations for poststroke managements are presented separately. OUTCOMES: The overall guideline considers improvement in functional status measures as the primary outcome. Achieving community-dwelling status and preventing complications, death, and rehospitalization are also important outcomes. Costs are not specifically addressed. PARTICIPANTS: The Department of Veterans Affairs/Department of Defense (VA/DoD) Stroke Rehabilitation Working Group consisted of 28, largely VA and military hospital, representatives of medical and allied professions concerned with stroke diagnosis, management, and rehabilitation. Nine additional members with similar credentials served as the editorial committee. Technical consultation was contracted from ACS Federal Health Care, Inc., and the Center for Evidence-Based Practice, State University of New York-Upstate Medical University, Department of Family Medicine conducted evidence appraisal. Consensus was achieved over several years of facilitated group discussion and iterative evaluation of draft documents and supporting evidence. SPONSOR: The guideline was prepared under the auspices of the VA/DoD. No other source of support was identified in the document, or supporting documents. Page53 Jefferson InterProfessional Education Center Bibliography – January 2009 Rodriguez, H. P., Rogers, W., Marshall, R., & Safran, D. G. (2007). Multidisciplinary primary care teams: Effects on the quality of clinician-patient interactions and organizational features of care. Medical Care, 45(1), 19-19-27. This study examined the influence of multi-disciplinary teams on patients' assessments of primary care, including access, integration, and clinician-patient interaction quality. The PCP visit discontinuities are associated with more negative care experiences, irrespective of whether discontinuities involve on-or off- team visits, highlights the challenges of incorporating teams into primary care relationships. Roland, M. (2005). Clinical practice guidelines for older patients with comorbid diseases (comment). Journal of the American Medical Association, 295(1), 716-716-724. In response to Boyd's "Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance," the author expresses concern over payfor-performance schemes and the effects that they may have on appropriate clinical practice. Rosenbaum, S. (2007). Improving the management of chronic disease (comment). New England Journal of Medicine, 356(9), 921-921-934. The author comments on Landon's "Improving the management of chronic disease at community health centers." The author points out that the study covered too short a period of time to capture health outcomes, and that they failed to provide for the policy implications of their work. Ross, F., & Harris, R. (2005). Can interprofessional education make a difference in the care of people with chronic disease? Chronic Illness, 1(1), 81-81-86. This article questions what is already known about interprofessional interventions and the care of people with long-term conditions. In addition, the article examines available evidence and the potential for interprofessional education in changing practices. Rothman, R. L., DeWalt, D. A., Malone, R., Bryant, B., Shintani, A., & Crigler, B. (2004). Influence of patient literacy on the effectiveness of a primary care-based diabetes disease management program. Journal of the American Medical Association, 292(14), 1711-1711-1716. The purpose of this study was to examine the role of literacy on the effectiveness of a comprehensive disease management program for patients with diabetes. The study concluded that literacy may be an important factor for predicting who will benefit from an intervention for diabetes management. Rowley, M. J., Hensley, M. J., Brinsmead, M. W., & Wlodarczyk, J. H. (1995). Continuity of care by a midwife team versus routine care during pregnancy and birth: A randomised trial. The Medical Journal of Australia, 163(6), 289-293. OBJECTIVE: To compare continuity of care from a midwife team with routine care from a variety of doctors and midwives. DESIGN: A stratified, randomised controlled trial. PARTICIPANTS AND SETTING: 814 women attending the antenatal clinic of a tertiary referral, university hospital. INTERVENTION: Women were randomly allocated to team care from a team of six midwives, or routine care from a variety of doctors and midwives. MAIN OUTCOME MEASURES: Antenatal, intrapartum and neonatal events; maternal satisfaction; and cost of treatment. RESULTS: 405 women were randomly allocated to team care and 409 to routine care; they delivered 385 and 386 babies, respectively. Team care women were more likely to attend antenatal classes (OR, 1.73; 95% CI, 1.23-2.42); less likely to use pethidine during labour (OR, 0.32; 95% CI, 0.22-0.46); and more likely to labour and deliver without intervention (OR, 1.73; 95% CI, 1.28-2.34). Babies of team care mothers received less neonatal resuscitation (OR, 0.59; 95% CI, 0.41-0.86), although there was no difference in Apgar scores at five minutes (OR, 0.86; 95% CI, 0.29-2.57). The stillbirth and neonatal death rate was the same for both groups of mothers with a singleton pregnancy (three deaths), but there were three deaths (birthweights of 600 g, 660 g, 1340 g) in twin pregnancies in the group receiving team care. Team care was rated better than routine care for all measures of maternal satisfaction. Team care meant a cost reduction of 4.5%. CONCLUSION: Continuity of care provided by a small team of midwives resulted in a more satisfying birth experience at less cost than routine Page54 Jefferson InterProfessional Education Center Bibliography – January 2009 care and fewer adverse maternal and neonatal outcomes. Although a much larger study would be required to provide adequate power to detect rare outcomes, our study found that continuity of care by a midwife team was as safe as routine care. Rudland, J. R., & Mires, G. J. (2005). Characteristics of doctors and nurses as perceived by students entering medical school: Implications for shared teaching. Medical Education, 39(5), 448-448-455. This study examines perceived professional characteristics of doctors and nurses by students entering medical school as a means to understand when interprofessional education should be introduced. Medical students appeared positive about shared teaching, however, these students also had an overall poor perception of the academic ability, status in society, and professional competence of nurses. Russell, L., Nyhof-Young, J., Abosh, B., & Robinson, S. (2006). An exploratory analysis of an interprofessional learning environment in two hospital clinical teaching units. Journal of Interprofessional Care, 20(1), 29-29-39. An analysis of a teaching environment with regard to interprofessional practice during practicums was done using both qualitative and quantitative methods. Results demonstrated that nurses and other health professionals had a more positive view of interprofessional collaboration than physicians. Students also had little understanding of the nature of collaborative behavior. These results have implications for the design of interprofessional curriculum in clinical practicums. Rust, G., & Cooper, L. A. (2007). How can practice-based research contribute to the elimination of health disparities? Journal of the American Board of Family Medicine : JABFM, 20(2), 105-114. doi:10.3122/jabfm.2007.02.060131 Racial, ethnic, and socioeconomic disparities in health care and health outcomes are well documented. Disparities research is evolving from documenting these disparities, to understanding their causes and mechanisms, and finally to conducting interventional research to reduce or eliminate disparities. Unfortunately, few studies to date have demonstrated substantial reductions in health outcomes disparities. Traditional experimental models of research that test a single intervention held constant throughout the study period may not have the power to impact complex clusters of comorbid health disparities in patients who receive care in underresourced primary care safety net practice settings. New models of research will be required to test dynamic, multidimensional interventions that triangulate on patients, providers, and communities and are continuously improved with every radar-sweep of feedback from rapid-cycle measurement of population health outcomes on a community-wide basis. In this article, we review 12 promising strategies that could substantially increase the impact of research on eliminating health disparities in America. Sadof, M. D. (2007). Improving the management of chronic disease (comment). New England Journal of Medicine, 356(9), 921-921-934. The author comment's on Landon's article "Improving the management of chronic disease at community health centers", in establishing appropriate outcomes for evaluating treatment. This includes allowing enough time before assessing an intervention and partnering with the right people/organizations to establish appropriate outcomes. Salzman, B. (2006). Myths and realities of aging. Care Management Journals : Journal of Case Management ; the Journal of Long Term Home Health Care, 7(3), 141-150. As the aging population expands, it will become increasingly important for health care providers to become aware of and sensitive to the needs and concerns of older adults. Ageism is a term that describes negative stereotyping of older adults and discrimination because of older age. Health concerns and symptoms in the elderly may be overlooked or dismissed as part of the normal aging process. Consequently, several conditions in olders adults are significantly underdiagnosed and undertreated Misconceptions about aging frequently encountered in medicine and in society at large include issues involving sexuality, sleep disturbance, depression, cognitive impairment, and substance abuse. We can learn to recognize ageist notions that influence medical practice. Perhaps Page55 Jefferson InterProfessional Education Center Bibliography – January 2009 by becoming more aware of myths and realities of aging, we can improve the health and quality of life of our elderly patients. Sarajuuri, J. M., Kaipio, M. L., Koskinen, S. K., Niemela, M. R., Servo, A. R., & Vilkki, J. S. (2005). Outcome of a comprehensive neurorehabilitation program for patients with traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 86(12), 2296-2302. doi:10.1016/j.apmr.2005.06.018 OBJECTIVE: To evaluate the outcome of a comprehensive neurorehabilitation program compared with that of conventional clinical care and rehabilitation for patients with traumatic brain injury (TBI). DESIGN: Nonrandomized, controlled trial with a 2-year follow-up. SETTING: Nationwide rehabilitation center and level I trauma center, both in Finland. PARTICIPANTS: We studied 19 consecutive adults with a significant TBI who underwent a comprehensive neurorehabilitation program and 20 control patients who received conventional rehabilitation referred by physicians in the general health care system. The outcome of the control patients was not known before the selection. The groups were similar in age, sex, education, injury severity (assessed on the Glasgow Coma Scale, radiologic and neuropsychologic findings, neurosurgical interventions), time from the injury, and preinjury employment status. INTERVENTIONS: A postacute, intensive, interdisciplinary, 6-week rehabilitation program for TBI patients who are considered to have adequate potential to achieve productivity by this means; focus on neuropsychologic rehabilitation and psychotherapy with vocational interventions and follow-up support. MAIN OUTCOME MEASURE: Status of productivity, judged as productive (defined as working, studying, or participating in volunteer activities) or nonproductive, evaluated on questionnaires filled in by patients and their significant others at the time of follow-up evaluation. RESULTS: At follow-up, 89% of the treated patients were productive compared with 55% of the controls. The rehabilitation program was significantly predictive of the productive status at follow-up (odds ratio=6.96; 95% confidence interval, 1.26-38.44; P=.017). Other factors did not explain the better productivity of the treatment group. Two neuropsychologistevaluators, who were blind to the rehabilitation history of patients and to each other's evaluations, were perfectly consistent in their classification of patients' productivity statuses. CONCLUSIONS: The findings support the proposition that comprehensive neuropsychologically oriented rehabilitation programs can improve psychosocial functioning in terms of productivity in postacute patients with moderate to severe TBI. Additional larger controlled studies are needed to establish the efficacy of TBI rehabilitation interventions. Sawyer, S. M., Drew, S., Yeo, M. S., & Britto, M. T. (2007). Lancet, 369(9571), 1481-1481-1489. This review focuses on the interaction between adolescents and chronic conditions and the health systems that support them. Evidence is showing that adolescents with chronic conditions are doubly disadvantaged due to engaging in riskier behavior to that of their peers and having greater potential for adverse health outcomes as a result of these behaviors. Schmalenberg, C., Kramer, M., King, C. R., Krugman, M., Lund, C., Poduska, D., et al. (2005). Excellence through evidence: Securing collegial/collaborative nurse-physician relationships, part 1. Journal of Nursing Administration, 35(10), 450-450-458. Collegial and collaborative nurse-physician relationships positively impact patient outcomes. This article discusses a multi-site evidence-based management practice initiative to identify structures that enable these relationships. Schnipper, J. L., Kirwin, J. L., Cotugno, M. C., Wahlstrom, S. A., Brown, B. A., Tarvin, E., et al. (2006). Role of pharmacist counseling in preventing adverse drug events after hospitalization. Archives of Internal Medicine, 166(5), 565-565-571. Frequently after hospitalization patients receive multiple changes in their medication regimens and inadequate education, which can lead to adverse drug events (ADEs). The purpose of this study was to identify drug-related problems during and after hospitalization and to determine the effect of patient counseling and follow-up by pharmacists on preventable ADEs. Page56 Jefferson InterProfessional Education Center Bibliography – January 2009 Sepulveda, M. J., Bodenheimer, T., & Grundy, P. (2008). Primary care: Can it solve employers' health care dilemma? Health Affairs (Project Hope), 27(1), 151-158. doi:10.1377/hlthaff.27.1.151 Employers are beginning to recognize that investing in the primary care foundation of the health care system may help address their problems of rising health care costs and uneven quality. Primary care faces a crisis as a growing number of U.S. medical graduates are avoiding primary care careers because of relatively low reimbursement and an unsatisfying work life. Yet a strong primary care sector has been associated with reduced health care costs and improved quality. Through the Patient-Centered Primary Care Collaborative and other efforts, some large employers are engaged in initiatives to strengthen primary care. Sequist, T. D., Adams, A., Zhang, F., Ross-Degnan, D., & Ayanian, J. Z. (2006). Effect of quality improvement on racial disparities in diabetes care. Archives of Internal Medicine, 166(6), 675-675681. It is well documented that racial disparities in health care are prevalent and solutions to this problem are not well documented. This study sought to determine whether generic quality improvement efforts were associated with changes in racial disparities in diabetes care. At the conclusion of the study, racial disparities were diminished in some aspects of diabetes care, however, reducing disparities may require a focus on minority health. Shaw, S. N. (2006). Interprofessional primary care: Patients' perspectives. Journal of Interprofessional Care, 20(2), 199-199-201. This study was designed to explore patient's experiences of interprofessional primary healthcare at Toronto Western's Family Health Center (part of University of Toronto), where care is provided by a variety of health professionals. Sheehan, D., & Jansen, D. (2006). The development of a national bicultural and interprofessional programme in clinical teaching and supervision in new zealand. Journal of Interprofessional Care, 20(6), 591-591-601. This project required close collaboration between two education providers, one a Maori private education provider and the other a traditional government-funded tertiary institution; and for both organizations to work cooperatively with Maori communities and Maori health providers. This paper describes how this course was designed, how it is delivered within a Maori paradigm, and how the outcomes are achieved. It also describes the cooperation between Maori and Pakeha (white New Zealanders) across health, community and educational organizations that was required to sustain this program over five years and identifies some themes that may be applied in a global context. Sheehan, D., Robertson, L., & Ormond, T. (2007). Comparison of language used and patterns of communication in interprofessional and multidisciplinary teams. Journal of Interprofessional Care, 21(1), 17-17-30. This article explores whether language used differentiates between a multidisciplinary team and an interprofessional team. Interview data was analyzed through a symbolic interactionist perspective. Differences were noted between the two types of teams. The implications of these communication differences were discussed. Sheps, S. (2006). Reflections on safety and interprofessional care: Some conceptual approaches. Journal of Interprofessional Care, 20(5), 545-545-548. Shield, F., Enderby, P., & Nancarrow, S. (2006). Stakeholder views of the training needs of an interprofessional practitioner who works with older people. Nurse Education Today, 26(5), 367-367376. This paper reports on research done in the United Kingdom to examine the education and training requirement of an interprofessional practitioner for the elderly. Views of clients, carers, and service providers were elicited using multiple methods. The majority of service providers identified the need Page57 Jefferson InterProfessional Education Center Bibliography – January 2009 for an interprofessional practitioner. It was felt that education for this need should be established at a national level. Shields, L., Pratt, J., Davis, L. M., & Hunter, J. (2007). Family-centred care for children in hospital. Cochrane Database of Systematic Reviews (Online), (1)(1), CD004811. doi:10.1002/14651858.CD004811.pub2 BACKGROUND: Family-centred care (FCC) is a widely used model in paediatrics, and is felt instinctively to be the best way to provide care to children in hospital. However, its effectiveness has not been measured. OBJECTIVES: The primary objective of this review was to assess the effects of family-centred models of care for hospitalised children when compared to standard or professionallycentred models of care, on child, family and health service outcomes. SEARCH STRATEGY: We searched: MEDLINE (1966 to February 2004); the Cochrane Central Register of Controlled Trials (CENTRAL), (The Cochrane Library, Issue 2, 2004); CINAHL (1982 to February 2004); PsycINFO (1972 to February 2004); ERIC (1982 to February 2004); Sociological Abstracts (1963 to February 2004); Social Work Abstracts (1977 to February 2004); and AMI (Australasian Medical Index) (1966 to February 2004). SELECTION CRITERIA: We searched for randomised controlled trials (RCTs) or quasi-randomised controlled trials including cluster randomised trials and controlled clinical trials (CCTs), and controlled before and after studies (CBAs), in which family-centred care models are compared with professionally-centred models of care for hospitalised children (aged up to 12 years). Studies also had to meet criteria for family-centredness and methodological quality. In order to assess studies for the degree of family-centredness, this review utilised a modified rating scale based on a validated instrument. DATA COLLECTION AND ANALYSIS: Two review authors undertook the searches, and three authors independently assessed trial quality and extracted data. We contacted study authors for additional information. MAIN RESULTS: No studies met inclusion criteria, and hence no analysis could be undertaken. Five studies came close to inclusion. Three of these studies were excluded primarily because of inadequate or unclear blinding of outcome assessment, while for one study the age group was outside the parameters of this review. One study met most criteria, but the children were aged up to 18 years. We contacted the study authors who kindly provided a subset analysis, but on further examination the study also proved to have inadequate blinding procedures and so was not included. It was not possible to undertake any subset analysis of populations. Of the other studies identified through the search, 13 met some of the inclusion criteria but were reports of qualitative research and are reviewed elsewhere. AUTHORS' CONCLUSIONS: This review has highlighted the dearth of high quality quantitative research about family-centred care. A much more stringent examination of the use of family-centred care as a model for care delivery to children and families in health services is needed. Shoultz, J., Oneha, M. F., Magnussen, L., Hla, M. M., Brees-Saunders, Z., Cruz, M. D., et al. (2006). Finding solutions to challenges faced in community-based participatory research between academic and community organizations. Journal of Interprofessional Care, 20(2), 133-133-144. The purpose of this paper is to discuss approaches and solutions used by this research team in response to the challenges they have faced in using CBPR. The team uses CBPR to understand and support the process of disclosure of intimate partner violence (IPV) within the context of the community health centers that provide services for multicultural and multi-lingual populations. While CBPR provides a route to develop trust and build on the strengths of partners from various settings, there are multiple challenges that arise when partnering organizations present with different infrastructures, missions, resources and populations served. Shrank, W. H., Hoang, T., Ettner, S. L., Glassman, P. A., Nair, K., DeLapp, D., et al. (2006). The implications of choice: Prescribing generic or preferred pharmaceuticals improves medication adherence for chronic conditions. Archives of Internal Medicine, 166(3), 332-332-337. This study explored whether patients enrolled in 3-tier pharmacy benefit plans who receive generic or preferred brand-name agents when initiating chronic therapy were more adherent to treatment than those who received non preferred brand-name medications. This study concluded that in a 3tier pharmacy benefit plan, prescribing generic or preferred medications within a therapeutic class is associated with improvements in adherence to therapy. Page58 Jefferson InterProfessional Education Center Bibliography – January 2009 Siegler, E. L., & Capello, C. F. (2005). Creating a teaching geriatric service: Ten important lessons. Journal of the American Geriatrics Society, 53(2), 327-330. doi:10.1111/j.1532-5415.2005.53122.x The restructuring of The Medical Service at the Weill/Cornell campus of the New York Presbyterian Hospital, coupled with funding from the Donald W. Reynolds Foundation to strengthen physicians' training in geriatrics, enabled the creation of a geriatrics inpatient team and a 17-bed Acute Care for Elders unit. It has also allowed a program to be designed that exposes residents to the fundamental principles of geriatric care, offers them opportunities to follow older patients in multiple venues, and provides a chance to enhance their skills and gain experience in interdisciplinary care. In creating the service, a number of mistakes were made, but a few lessons were also learned in the process. After a brief description of the program, 10 lessons that highlight the pitfalls and potential of an inpatient geriatrics teaching service are shared. Sitzia, J., Cotterell, P., & Richardson, A. (2006). Interprofessional collaboration with service users in the development of cancer services: The cancer partnership project. Journal of Interprofessional Care, 20(1), 60-60-74. Patient and Public Involvement (PPI) is a cornerstone of UK National Health Service (NHS) policy. The Cancer Partnership Project (CPP) is the leading national PPI initiative in cancer care. The CPP espouses a "partnership" model, with a "Partnership Group" - collaborative service improvement groups formed of NHS staff and service users - in each of 34 cancer networks in England. These groups aim to enable service users to influence local cancer service development and thereby improve the effectiveness of services. We interviewed 59 cancer service users and NHS staff in a reflective evaluation of CPP. Groups were active and visible in 30 networks, their main activities being: providing an accessible source of consumer opinion; prolific networking and representation; patient information and communication projects; and lobbying for service improvements. The groups exhibited some significant tensions. The motivations of professional staff varied markedly, and "obligatory" involvement as part of a person's job was counter-productive when not coupled with a "personal" belief in the value of PPI. Other controversial areas were the disclosure by patients' of personal health and treatment experiences, and emotional attachment to the group. It was concluded that partnership groups represent a useful PPI model, but more attention generally should be paid to the complexities of PPI and timescales required for meaningful cultural change. Smolkin, M. T. (2007). Improving the management of chronic disease. New England Journal of Medicine, 356(9), 921-921-934. This study was a controlled pre- and post-intervetion study of community health centers participating in the Health Disparities Collaboratives (sponsored by the Health Resources and Services Administration) of the care of patients with diabetes, asthma, or hypertenson. The results showed that the intervention centers had greater improvement in the measures of quality of care for patients with asthma and diabetes, but not hypertension. Solberg, L. I., Crain, A. L., Sperl-Hillen, J. M., Hroscikoski, M. C., Engebretson, K. I., & O'Connor, P. J. (2006). Care quality and implementation of the chronic care model: A quantitative study. Annals of Family Medicine, 4, 310-310-316. This article assessed whether changes in the Chronic Care Model (CCM) would correlate with changes in care quality. A survey was completed before and after implementation of CCM with respect to diabetes, coronary heart disease, or depression. There were few significant correlations between the changes, but improvements in quality measure did occur for the 3 chronic diseases. Spratt, J., Shucksmith, J., Philip, K., & Watson, C. (2006). Interprofessional support of mental well-being in schools: A bourdieuan perspective. Journal of Interprofessional Care, 20(4), 391-391-402. This paper draws on a Scottish study which looked at the responses of local authorities, schools and other local afencies to student's challenging behaviors which stem from poor mental health. Specifically, it explores how the presence of individuals from other agencies impacted the school's ability to respond to such behavioral issues. Page59 Jefferson InterProfessional Education Center Bibliography – January 2009 Starfield, B. (2007). Global health, equity, and primary care. Journal of the American Board of Family Medicine : JABFM, 20(6), 511-513. doi:10.3122/jabfm.2007.06.070176 Global health provides a special challenge for primary care and general practice, which will become increasingly important in the future as the prevalence of multimorbidity increases with increasing likelihood of survival from acute manifestations of illness, as populations age, and as costs of care increase with increasing availability of technologic interventions. World organizations of primary care physicians need to take up the challenge before it becomes a crisis. Steinert, Y. (2005). Learning together to teach together: Interprofessional education and faculty development. Journal of Interprofessional Care, (Supplement 1), 60-60-75. Interprofessional education for collaborative patient-centered practice has been identified as a key mechanism to address health care needs and priorities. Faculty development plays a significant role in the promotion of interprofessional education (IPE). This paper addresses barriers to teaching and learning, various approaches to facilitate IPE, and models to implement. Stevens, D. P., & Wagner, E. H. (2006). Transform residency training in chronic illness care -- now [commentary]. Journal of Medical Education, 81(8), 685-685-687. This article describes how the Chronic Care Model was implemented in 22 teaching hospitals. The results of their efforts were tracked by each of the team members, with respect to clinical and educational outcomes. The two most effective drivers of change were organization-wide leadership and the academic culture (competitiveness, the aspiration for excellence, focus on the research mission, comfort with data, and commitment to the education mission). Stew, G. (2005). Learning together in practice: A survey of interprofessional education in clinical settings in south-east england. Journal of Interprofessional Care, 19(3), 223-223-235. This article describes the outcomes of a two-year project, commissioned by the Department of Health, to investigate the development of pre-registration education for the allied health professions in Kent, Surrey, and Sussex, England. It was found that IPE is highly contextualized, and develops according to a variety of situational factors. Stone, N. (2006). Evaluating interprofessional education: The tautological need for interdisciplinary approaches. Journal of Interprofessional Care, 20(3), 260-260-275. This paper explored issues associated with evaluating interprofessional education (IPE) programs. Qualitative and quantitative approaches are suggested. An example of the Rural IPE (RIPE) project is provided which recommends an interdisciplinary approach to evaluating IPE programs. Stone, N. (2006). The rural interprofessional education project (RIPE). Journal of Interprofessional Care, 20(1), 79-79-81. This article reports on the evaluation of the Rural Interprofessional Education Project, an optional two week undergraduate rural placement program for health discipline students in Victoria, Australia. The study found that students had an increased understanding of their roles, and felt "'understood', 'condifent', 'effective', and 'respected'" while working with other health professionals and felt that IPE should be a part of every health professional student's training. Strong, K., Mathers, C., Leeder, S., & Beaglehole, R. (2005). Preventing chronic diseases: How many lives can we save? (see comment). (review). Lancet, 366(9496), 1578-1578-1582. This article discusses the impact chronic diseases have on the mortality of individuals in low-income and middle-income countries. The article proposes a new goal for reducing deaths from chronic disease. Sturkey, E. N., Linker, S., Keith, D. D., & Comeau, E. (2005). Improving wound care outcomes in the home setting. Journal of Nursing Care Quality, 20(4), 349-355. In 2001 through 2003, our agency received deficiencies in infection-control practices, specific to wound care, from JCAHO and Medicare surveyors. Efforts to correct this pattern were initially Page60 Jefferson InterProfessional Education Center Bibliography – January 2009 unsuccessful. As a result, in 2003, an interdisciplinary performance improvement team was formed to assess, plan, and implement a wound care program utilizing research-based best practice. The changes in process, practice, and education resulted in success, with improvement evidenced by 100% acceptable practice during our 2004 unannounced JCAHO/Medicare survey, a declined rate of wound infection per our Medicare OASIS Adverse Event Report, and a decrease in wound care patient visits. Suris, J. C., Michaud, P. A., & Viner, R. (2004). The adolescent with a chronic condition. part I: Developmental issues (review). Archives of Disease in Childhood, 89(10), 938-938-942. According to surveys, approximately 10% of adolescents suffer from a chronic illness. This paper seeks to analyze the reciprocal effects of chronic conditions and adolescent development by reviewing the effects of chronic disease on growth and puberty and on psychosocial development. Szabo, J. (2007). Disease management. medicaid programs look outside to manage the chronically ill. Hospitals and Health Networks, 81(4), 18-18. Taanila, A., Purola, H., & Larivaara, P. (2006). Nurses learning family-oriented interprofessional collaboration. International Journal of Circumpolar Health, 65(3), 206-206-218. This study was a qualitative two-year family-oriented interprofessional education program for professionals working in the field of primary services in Finland. The program aimed to provide participants with skills to work with families utilizing interprofessional collaboration. Content analysis was used. At the end of the study, the nurses showed changed working methods from expert- to client- and family-oriented. Taylor, S. J. C., Candy, B., Bryar, R. M., Ramsay, J., Vrijhoef, H. J. M., Esmond, G., et al. (2005). Effectiveness of innovations in nurse led chronic disease management for patients with chronic obstructive pulmonary disease: Systematic review of evidence. British Medical Journal, 331(7515), 485. This article describes a systematic review of the literature that searched for articles containing chronic disease management in inpatient, outpatient, and community-based interventions completed by nurses. The authors found little evidence supporting the use of nurse led medical management for patients with COPD. They concluded that while there is little data to support the role of the nurses, there is even less data stating any negative effect of the nurse in this medical management role. The Henry J. Kaiser Family Foundation. (2007). Key facts: Race, ethnicity & medical care Thistlethwaite, J., & Nisbet, G. (2007). Interprofessional education: What's the point and where we're at... The Clinical Teacher, (4), 67-67-72. This article creates a case for the importance of interprofessional education (IPE) and discusses the state of interprofessional education currently. In addition, the article provides models, learning outcomes, examples, evaluation, and barriers to IPE. Thomas, E. J., Sexton, J. B., & Helmreich, R. L. (2003). Discrepant attitudes about teamwork among critical care nurses and physicians. (see comment). Critical Care Medicine, 31(3), 956-956-959. The purpose of this study was to measure and compare critical care physicians' and nurses' attitudes about teamwork. The study concluded that critical care physicians and nurses have discrepant attitudes about the teamwork they experience with each other. This includes: suboptimal conflict resolution and interpersonal communication skills. Thompson, T. L., Emrich, K., & Moore, G. (2003). The effect of curriculum on the attitudes of nursing students toward disability. Rehabilitation Nursing : The Official Journal of the Association of Rehabilitation Nurses, 28(1), 27-30. Societal attitudes toward people with differing abilities are often based on a lack of understanding, Page61 Jefferson InterProfessional Education Center Bibliography – January 2009 fear of the unkNown, and stereotypes learned from others. Nursing students enter their educational programs with similar attitudes and experiences. Attitudes of nurses are key to how they respond toward individuals with disabilities and chronic illnesses. The nurses' attitudes affect the individual client's understanding of the disability and his or her self-concept as he or she adjusts to major life changes. The purpose of this descriptive study was to identify whether a change in curriculum and experience had an effect on nursing student attitudes. Using the Attitudes Toward Disabled Persons (ATDP) Scale, a pre-post study of 42 nursing students' attitudes toward individuals with disabilities was conducted. Tests were administered as the students entered their senior year and took the chronic illness course, and again at the completion of the senior year. The students' attitudes were significantly more positive at the completion of their senior year. The findings suggest that education about, and experience with, individuals with disabilities positively affect the attitudes of nursing students toward individuals with disabilities. Thrall, J. H. (2005). Prevalence and costs of chronic disease in a health care system structured for treatment of acute illness. Radiology, 235(1), 9-9-12. This article discusses the chronic disease, its prevalence, direct and indirect costs, and the importance of radiology in chronic disease. It also discusses the effects of the structure of the health care system on chronic disease. Tijhuis, G. J., Zwinderman, A. H., Hazes, J. M., Breedveld, F. C., & Vlieland, P. M. (2003). Two-year follow-up of a randomized controlled trial of a clinical nurse specialist intervention, inpatient, and day patient team care in rheumatoid arthritis. Journal of Advanced Nursing, 41(1), 34-43. AIM: To compare the long-term effectiveness of care delivered by a clinical nurse specialist (CNS) with inpatient team care and day patient team care in patients with rheumatoid arthritis and increasing functional limitations. Background. The role of CNSs in the management of patients with rheumatoid arthritis (RA) is evolving, and their effectiveness in comparison with care provided by a rheumatologist alone has been established. However, long-term controlled studies showing how the effectiveness of CNSs compares with that of other forms of co-ordinated care, such as multidisciplinary team care, are lacking. METHODS: Two hundred and ten patients rheumatoid arthritis patients were randomized to care delivered by a CNS in a rheumatology outpatient clinic (12 weeks), inpatient team care (2 weeks) and day patient team care (3 weeks). Clinical assessments recorded on study entry, weeks 12, 26, 52, 78 and 104 comprised the health assessment questionnaire (HAQ) and MacMaster Toronto Arthritis (MACTAR) patient preference interview as primary outcome measures. Grip strength, walk test, RAND-36, Rheumatoid Arthritis Quality of Life questionnaire and disease activity score (DAS) were applied as secondary outcome measures. RESULTS: No significant differences in medical treatment, use of services of other health professionals, introduction of adaptive equipment or number of hospitalizations were observed between the three treatment groups during 2 year follow-up, except that visits to nurse specialists were more frequent and home help was less frequent in the CNS group. A comparison of clinical outcomes among the three groups and a comparison between the nurse specialist and inpatient and day patient care groups together did not show any significant differences. Within all three groups functional status, quality of life and disease activity improved significantly (P < 0.05). In general, the results obtained after 12 weeks remained stable until 104 weeks after the start of the study. CONCLUSION: Care provided by a CNS in an outpatient rheumatology clinic has a similar long-term clinical outcome to inpatient and day patient team care in patients with rheumatoid arthritis. A CNS intervention appears to be an effective innovation in the care for patients with rheumatoid arthritis. Tijhuis, G. J., Zwinderman, A. H., Hazes, J. M., Van Den Hout, W. B., Breedveld, F. C., & Vliet Vlieland, T. P. (2002). A randomized comparison of care provided by a clinical nurse specialist, an inpatient team, and a day patient team in rheumatoid arthritis. Arthritis and Rheumatism, 47(5), 525-531. doi:10.1002/art.10665 OBJECTIVES: To compare in a randomized, controlled trial the clinical effectiveness of care delivered by a clinical nurse specialist, inpatient team care, and day patient team care in patients with rheumatoid arthritis (RA) who have increasing functional limitations. METHODS: Between December 1996 and January 1999, 210 patients with RA were recruited in the outpatient clinic of the Page62 Jefferson InterProfessional Education Center Bibliography – January 2009 rheumatology department of 6 academic and nonacademic hospitals. Clinical assessments recorded on study entry and weeks 6, 12, 26, and 52 included the Health Assessment Questionnaire (HAQ) and the McMaster Toronto Arthritis Patient Preference Disability Questionnaire as primary outcome measures, and the RAND-36 Item Health Survey, the Rheumatoid Arthritis Quality of Life questionnaire, the Health Utility Rating Scale, and the Disease Activity Score as secondary outcome measures. Patient satisfaction with care was measured on a visual analog scale in week 6 in all 3 groups and again in week 12 in the nurse specialist group. RESULTS: Within all 3 groups, functional status, quality of life, health utility, and disease activity improved significantly over time (P < 0.05). However, a comparison of clinical outcome among the 3 groups and a comparison between the nurse specialist group and the inpatient and day patient care groups together did not show any sustained significant differences. Subgroup analysis showed that age had a significant impact on differences between the 3 treatment groups with respect to functional outcome as measured with the HAQ (P < 0.001). With increasing age, the most favorable outcome shifted from care provided by a clinical nurse specialist and inpatient care to day patient care. Patients' satisfaction with care was significantly lower in the nurse specialist group than in the inpatient and day patient care groups (P < 0.001). CONCLUSION: Care provided by a clinical nurse specialist appears to have a similar clinical outcome in comparison with inpatient and day patient team care. Although all patients were highly satisfied with multidisciplinary care, patients who received care provided by a clinical nurse specialist were slightly less satisfied than those who received inpatient or day patient team care. Age appeared to be the only factor related to differences in functional outcome between the 3 treatment groups. The choice of management strategy may, apart from age, further be dependent on the availability of facilities, the preferences of patients and health care providers, and economic considerations. Tilling, K., & Wolfe, C. (2002). Re: Randomized controlled study of stroke unit versus stroke team care in different stroke subtypes. Stroke; a Journal of Cerebral Circulation, 33(7), 1741-2; author reply 17412. In response to the article "Randomized controlled study of stroke unit versus stroke team care in different stroke subtypes" by Evans et al, this letter by Tilling and Wolfe raises some important issues on the subgroup analysis and interpretation of data as well as on the delicate balance between presenting details of statistical analysis versus presenting a clear clinical message. Too much treatment? aggressive medical care can lead to more pain, with no gain.(2008, July 2008). Consumer Reports, , 40-41-44. Tu, H. T., & O'Malley, A. S. (2007). Exodus of male physicians from primary care drives shift to specialty practice (Tracking Report No. 17)Center for Studying Health Systems Change. An exodus of male physicians from primary care is diving a marked shift in the U.S. physician workforce toward medical-specialty practice, Two factors have helped mask the severity of the shift a growing proportion of female physicians, who disproportionately choose primary care, and continued reliance on international medical graduates, who now account for nearly a quarter of all U.S. primary care physicians. Primary care physicians' incomes have lost ground to both inflation and medical and surgical specialists' incomes. And women in primary care face a 22 percent income gap relative to men, even after accounting for differing characteristics. If real incomes for primary care physicians continue to decline, there is a risk that the migration of male physicians will intensify and that female physicians may begin avoiding primary care - trends that could aggravate a predicted shortage of primary care physicians. Turner, J., Pugh, J., & Budiani, D. (2005). "It's always continuing": First-year medical students' perspectives on chronic illness and the care of chronically ill patients. Academic Medicine : Journal of the Association of American Medical Colleges, 80(2), 183-188. PURPOSE: Caring for patients with chronic health conditions is an important component of health care in the 21st century. This study uses qualitative research methods to take an in-depth look at the attitudes of first-year medical students toward chronic illness and the care of chronically ill patients. METHOD: In Spring 2000, 26 first-year medical students at the College of Human Medicine, Page63 Jefferson InterProfessional Education Center Bibliography – January 2009 Michigan State University, were invited to participate in interviews focused on their attitudes toward caring for patients with chronic illness. Transcripts of the interviews were analyzed to identify iterative themes. Concurrently, all 105 first-year students were given a questionnaire that asked about their attitudes toward various aspects of patient care. RESULTS: Nineteen students participated in the interviews. Students viewed chronic illness as incurable, long running, life altering, and often terminal. Most students had firsthand experience with chronic illness in family members; many had premedical work experience with chronically ill patients. Most students described themselves as comfortable with a partnership relationship with patients. Students acknowledged responsibility for caring for those with chronic illness but anticipated sadness and frustration in this work. One hundred and four students completed the questionnaire. Respondents' attitudes were consistent with those expressed in the interviews, suggesting that the interview findings represent the class as a whole. CONCLUSION: Students enter medical school with complex attitudes toward chronic illness, many of which are more negative than previously reported. Qualitative instruments constitute important methods for studying the intricacies of students' attitudes and outlooks. Valderas, J. M., Starfield, B., & Roland, M. (2007). Multimorbidity's many challenges: A research priority in the UK (comment). British Medical Journal, 334(7602), 1016-1016-1017. The author's discuss the wide variation in the reported prevalence of chronic diseases in children as discussed in van der Lee et al's article "Definitions and measurement of chronic health conditions in childhood: a systematic review ." The problem that he addresses is the lack of consistent definition of "chronic disease" as a reason for this variation. Van Weel, C., & Schellevis, F. G. (2006). Comorbidity and guidelines: Conflicting interests. Lancet, 367(9510), 550-550-551. This article discusses the issues related to disease-specific guidelines in patients with co-morbid conditions. Varga-Atkins, T., & Cooper, H. (2005). Developing e-learning for interprofessional education. Journal of Telemedicine and Telecare, 11(Supplement 1), 102-102-104. An evidence-based, interprofessional educational course involving first-year undergraduate students at the University of Liverpool. Part of the course involved an online format. A focus group was conducted to understand the e-learning writing experience. Team working contributed to the success of the writing process, reflecting the theme of inter-professionally. Vaughan, D. (2008, May 19, 2008). Learning to work together. Nurse.Com Nursing Spectrum, , 18-19. Verma, S., Medves, J., Paterson, M., & Patteson, A. (2006). Demonstrating interprofessional education using a workshop model. Journal of Interprofessional Care, 20(6), 679-679-681. In response to the Inter-professional Education for Collaborative Patient-Centred Practice program initiative by Health Canada, the authors developed a programme of education and research called the Queen’s University Inter-professional Patient-Centred Education Direction (QUIPPED). The two-hour workshop described in this paper was an early outcome of the QUIPPED inter-professional education (IPE) approach to faculty development and was part of an international conference hosted by IECPCP in Canada, in May 2005. Verma, S., Paterson, M., & Medves, J. (2006). Core competencies for health care professionals: What medicine, nursing, occupational therapy, and physiotherapy share. Journal of Allied Health, 35, 109109-115. This paper describes the amalgamation of the core competencies identified for medicine , nursing, physical therapy, and occupational therapy and the harmonization of these competencies into a framework for interprofessional education. In addition, this paper highlights the relevance of crossdisciplinary competency teaching and 360-degree evaluation in teams. It also provides a launch pad for clarifying performance standards and expectations in interdisciplinary learning. Page64 Jefferson InterProfessional Education Center Bibliography – January 2009 Vincent, C. (2003). Understanding and responding to adverse events. The New England Journal of Medicine, 348(11), 1051-1056. doi:10.1056/NEJMhpr020760 An adverse outcome for a patient is difficult, sometimes traumatic, for all concerned. Such incidents pose considerable challenges to an organization, both in terms of the need to respond intelligently to their occurrence and in terms of the need to deal with their aftermath. The challenge is to find a way forward that provides the necessary support for the people involved while ensuring that the lessons of the incident are learned both by individual staff members and by the overall organization. In this article, I address two broad themes: first, how to investigate clinical incidents and learn useful lessons from them, and second, how to support the patients, families, and staff members who are involved. Vliet Vlieland, T. P., Breedveld, F. C., & Hazes, J. M. (1997). The two-year follow-up of a randomized comparison of in-patient multidisciplinary team care and routine out-patient care for active rheumatoid arthritis. British Journal of Rheumatology, 36(1), 82-85. The long-term effects of a period of 11 days of in-patient multidisciplinary team care were compared with routine out-patient care in 80 patients with active rheumatoid arthritis (RA). Endpoint measures included swollen and tender joint counts, the patient's assessment of pain, the patient's and the physician's assessments of disease activity, the ESR and the Health Assessment Questionnaire (HAQ). Two years after hospitalization, all 39 patients randomized to the in-patient group and 39 out of 41 patients randomized to the out-patient group were evaluable. At 2 yr, in the in-patient group the improvement according to mean changes from baseline was greater than that in the out-patient group for all endpoint measures except for the HAQ score, the differences not reaching statistical significance. Averaged over the time points 2, 52 and 104 weeks, the improvement was significantly greater in the in-patient group than in the out-patient group, except for the ESR and HAQ score. In conclusion, a short period of in-patient multidisciplinary team care has a beneficial effect on disease activity over a period of 2 yr and should be considered as a useful treatment modality in patients with active RA. Vliet Vlieland, T. P., & Hazes, J. M. (1997). Efficacy of multidisciplinary team care programs in rheumatoid arthritis. Seminars in Arthritis and Rheumatism, 27(2), 110-122. This study was designed to assess the efficacy of multidisciplinary team care in rheumatoid arthritis. Data were obtained through a Medline and manual literature search. The study concludes that shortterm inpatient team care, when compared to standard outpatient care, showed favorable outcomes. von Gunten, C. F. (2007). The hidden (real) curriculum. Journal of Palliative Medicine, 10(3), 632-633. doi:10.1089/jpm.2007.9963 The hidden agenda of medical education and training is for doctors to learn the rules of behavior and knowledge of procedures by observing the behavior of other doctors and health professionals in practicing medicine. Wagner, E. H. (2004). Chronic disease care. (comment). British Medical Journal, 328(7433), 177-177178. The author provides commentary on the Dixon et al article "Can the NHS learn from US managed care organisations?" Wagner, E. H. (1998). Chronic disease management: What will it take to improve care for chronic illness? Effective Clinical Practice : ECP, 1(1), 2-4. Wagner proposes comprehensive system change to improve chronic illness care. Walders, N., Kercsmar, C., Schluchter, M., Redline, S., Kirchner, H. L., & Drotar, D. (2006). An interdisciplinary intervention for undertreated pediatric asthma. Chest, 129(2), 292-299. doi:10.1378/chest.129.2.292 The objective of this study was to examine the effectiveness of an interdisciplinary intervention for pediatric asthma through an asthma management intervention. The primary outcome measure was change in asthma symptoms, and secondary outcomes included health-care utilization and asthma- Page65 Jefferson InterProfessional Education Center Bibliography – January 2009 related quality of life. Both groups demonstrated significant reductions in asthma symptoms and improvements in quality of life without any between-group differences identified over the course of follow-up. In contrast, the intervention group demonstrated less frequent health-care utilization over the 12-month follow-up period. While the intervention did not result in improvements in asthma symptoms, it accomplished modest reductions in the utilization of acute medical care. Warsi, A., Wang, P. S., LaValley, M. P., Avorn, J., & Solomon, D. H. (2004). Self-management education programs in chronic disease: A systematic review and methodological critique of the literature. Archives of Internal Medicine, 164(15), 1641-1641-1649. This article evaluated the efficacy of patient self-management educational programs for chronic diseases and critically reviewed their methodology. Self-management education programs resulted in small to moderate effects for selected chronic diseases. Weinstock, M. (2004). Chronic care: An acute problem. (see comment). Hospitals and Health Networks, 78(9), 44-44-48. Currently approximately 80% of all health care dollars are spent treating chronic conditions and more than 100 million Americans suffer from one or more chronic conditions. However, health care continues to be geared towards acute care. Wells, J. D., & Nicosia, S. (1993). The effects of multidisciplinary team care for acute spinal cord injury patients. The Journal of the American Paraplegia Society, 16(1), 23-29. The care of 169 survivors of spinal injury receiving acute treatment at the Hamilton General Hospital in Ontario, Canada, was studied. This paper compares treatment of groups of patients before and after formation of a multidisciplinary Acute Spinal Cord Injury Team. The establishment of multidisciplinary team care for acute spinal cord injury patients in our tertiary referral center correlates with clinically and statistically significant reductions in length of stay in the acute care hospital, alterations in the rate of surgical treatment for them, changes in the use of radiological resources, and reduction in the average number of days febrile. The team also brought stronger representation of allied health professionals to the hospital records of acute spinal cord injury patients. These important changes result from implementation of an effective multidisciplinary medical team without the addition of new funds, personnel, or hospital facilities and without alteration in referral patterns. Our team did not reduce mortality, duration of intensive care unit stay, or work for physicians. Westberg, S. M., Adams, J., Thiede, K., Stratton, T., & Bumgardner, M. A. (2006). Innovations in teaching: An interprofessional activity using standardized patients. American Journal of Pharmaceutical Education, 70(2), 1-1-5. Authors sought to describe the development and implementation of an interprofessional activity using standardized patients. It was found that an interprofessional activity involving multiple health professionals from multiple institutions can be successfully implemented. Pharmacy students indicated that this activity increased their awareness and ability to work as members of the health professional team. Whitcomb, M. E. (2007). Who will lead? [from the editor]. Journal of Medical Education, 82(2), 115-115116. New graduates will be required to provide high-quality patient care to patients with chronic diseases and will treat more racially and ethically diverse patients. The medical education programs need to address these challenges and prepare the future medical professionals. Whitcomb, M. E. (2007). Preparing the personal physician for practice (P(4)): Meeting the needs of patients: Redesign of residency training in family medicine. Journal of the American Board of Family Medicine : JABFM, 20(4), 356-64; discussion 329-31. doi:10.3122/jabfm.2007.04.070100 Family medicine stands at a critical point in its history. To achieve a place of enhanced prominence within American medicine, the discipline must acknowledge the fundamental changes that have occurred in the country's health care system in recent decades and discard its historical attachment Page66 Jefferson InterProfessional Education Center Bibliography – January 2009 to the fundamental beliefs that led to the establishment of the specialty almost 40 years ago. If the discipline is to serve the most critical needs of the American public, family medicine residency programs must be redesigned to train family physicians who will be experts in the ambulatory care of patients with chronic disease. To accomplish this, family medicine residency programs should provide residents in training with a more concentrated experience in the care of such patients. The enhanced focus of training on education for chronic illness care can be accomplished within a 2-year training period by eliminating training requirements that are no longer relevant to the practice of family medicine in most communities. White, P. (2005). Managing chronic diseases: End of life is more than death. (comment). British Medical Journal, 330(7497), 963-963. The author comments on Murray et al's "Palliative Care in Chronic Illness" Whitney, J., Vernon, S., Hughes, J., & Kinirons, M. (2006). Introducing exercise classes for older care home residents. Journal of Interprofessional Care, 20(3), 317-317-319. This report outlines the approach taken by the SLIPs physiotherapist to introduce an evidence based fall prevention exercise program with selected residential care homes. The article also presents some findings of qualitative evaluation of this work, focusing on implementation of the exercise program and participants' experiences. Willumsen, E. (2006). Leadership in interprofessional collaboration- the case of childcare in norway. Journal of Interprofessional Care, 20(4), 403-403-413. This study addresses leadership in interprofessional collaboration in childcare services (residential care). The aim was to explore the managers' experiences and present their views on how they exercised leadership in the residential institutions as well as how they organized and facilitated collaboration with relevant professionals and service users. The main findings were related to the managers' experiences of linked processes of leadership and collaboration, perceptions of the structures of communication, their responsibility as well as the interaction processes. Wilson, J., & Websdale, N. (2006). Domestic violence fatality review teams: An interprofessional model to reduce deaths. Journal of Interprofessional Care, 20(5), 535-535-544. In an effort to reduce injuries and prevent deaths from violence, interprofessional domestic violence fatality review teams (DVFRT) have developed across the United States and globally to study factors that contribute to intimate partner injury and deaths. Through interprofessional collective recommendations and cooperative actions, these teams are developing promising practices and systems' changes that offer better services, learning, and interventions to reduce injury and death from domestic violence. Wolff, J. L., & Boult, C. (2005). Moving beyond round pegs and square holes: Restructuring medicare to improve chronic care. (see comment). Annals of Internal Medicine, 143(6), 458-458-459. Medicare's benefit structure and reimbursement mechanisms are poorly aligned for high-quality chronic care in spite of chronic disease being highly prevalent. There is little evidence to suggest that successful quality improvement initiatives would reduce the costs of the Medicare program. This paper describes chronic care innovations to date and discusses ongoing and planned efforts by the Centers for Medicare and Medicaid Services to test related changes to Medicare's benefit structure and provider reimbursement. Woloschuk, W., Harasym, P. H., & Temple, W. (2004). Attitude change during medical school: A cohort study. Medical Education, 38(5), 522-534. doi:10.1046/j.1365-2929.2004.01820.x BACKGROUND: Attitudes influence behaviour. Developing and maintaining proper attitudes by medical students can impact on the quality of health care delivered to their patients as they assume the role of doctors. There is a paucity of longitudinal research reports on the extent to which students' attitude scores shift as they progress through medical school. OBJECTIVE: This study examined the change in attitude scores of a large student cohort as they progressed through medical school. Whether student gender is related to attitude change was also investigated. Page67 Jefferson InterProfessional Education Center Bibliography – January 2009 CONCLUSIONS: As students progress through medical school their attitude scores decline. The reasons for the shift in attitude scores are not clear but they may relate to a ceiling of high attitude scores at entry, loss of idealism and the impact of the unintended curriculum. Further study of the impact of medical education on student attitudes is warranted. Wood-Dauphinee, S., Shapiro, S., Bass, E., Fletcher, C., Georges, P., Hensby, V., et al. (1984). A randomized trial of team care following stroke. Stroke; a Journal of Cerebral Circulation, 15(5), 864872. A randomized controlled trial was conducted to examine the effects of interdisciplinary team care on acute hospitalized stroke patients. After obtaining baseline information on 42 stroke victims receiving conventional care in a general hospital, 130 stroke patients were stratified and randomly assigned either to Traditional or Team care. Assessments by independent evaluators permitted comparisons between Team and Traditional groups with reference to patient survival, motor performance and functional abilities. Data obtained prospectively from charts and treatment logs allowed the care process across groups to be compared. Results demonstrated that Team and Traditional patients fared similarly in survival. However there was an unexpected difference in survival depending upon sex. For motor performance, male survivors performed better with Team care and female survivors with the Traditional method. In terms of functional abilities, male patients receiving Team care again performed better than their Traditional counterparts, whereas in women there was no difference between the treatment groups. Woolf, S. H. (2004). Patient safety is not enough: Targeting quality improvements to optimize the health of the population. (see comment) (review). Annals of Internal Medicine, 140(1), 33-33-36. While patient safety is an important issue to address in health care, other issues such as chronic disease management and health promotion are also important, as lives are at stake when considering these topics as well. Policy makers need to consider the system as a whole and consider the potential effect on overall population health when prioritizing health care improvements. Woolf, S. H. (2008). The power of prevention and what it requires. JAMA : The Journal of the American Medical Association, 299(20), 2437-2439. doi:10.1001/jama.299.20.2437 This article focuses on prevention as an effective way of reducing healthcare costs and burden of illness in the population related to chronic disease. World Health Organization. (2008). World health report 2008: Primary health care now more than ever Yancik, R., Ershler, W., Satariano, W., Hazzard, W., Cohen, H. J., & Ferrucci, L. (2007). Report of the national institute on aging task force on comorbidity. Journals of Gerontology, 62(3), 275-275-280. Yeager, S. (2005). Interdisciplinary collaboration: The heart and soul of health care. Critical Care Nursing Clinics of North America, 17(2), 143-8, x. doi:10.1016/j.ccell.2005.01.003 In a health care system in which patient complexity, outcome indicators, and informed families are representative of current reality, an interdisciplinary approach to care is crucial to successful navigation of a patient's experience in the ICU. To guide practitioners toward favorable patient progression, a thorough understanding of interdisciplinary collaboration is necessary. This article focuses on definitions of, benefits of, and barriers to interdisciplinary collaboration and provides practical solutions for implementation. Young, L., Baker, P., Waller, S., Hodgson, L., & Moor, M. (2007). Knowing your allies: Medical education and interprofessional exposure. Journal of Interprofessional Care, 21(2), 155-155-163. This project aimed to develop interprofessional skills among 134 third year medical students that were of clinical educational value to the students, and through activities that directly benefited the rural health professionals in their daily work. The project proved successful in improving medical students' skills, knowledge, and perceptions concerning interprofessional practice. Page68 Jefferson InterProfessional Education Center Bibliography – January 2009 Zwarenstein, M., Bryant, W., & Reeves, S. (2003). In-service interprofessional education improves inpatient care and patient satisfaction. Journal of Interprofessional Care, 17(4), 401-401-402. The Level of Care Intervention Study (LOCIS) project is a 4-week reorganization and interprofessional training, developed in response to concerns that in-patients in medical wards at a South African teaching hospital were recieveing "routinized" care, rather than patient-specific care. LOCIS's goal was to improve teamwork, communication, and collaboration to provide better patient care. The impact of the program was measured against usual care in an adjacent ward. The evaluation contained 4 elements: team building, staff reorganization, a shift from task to team nursing, and patient planning. Zwarenstein, M., & Reeves, S. (2006). Knowledge translation and interprofessional collaboration: Where the rubber of evidence-based care hits the road of teamwork. Journal of Continuing Education in the Health Professions, 26(1), 46-46-54. A Health Canada-funded randomized trial is described in which quantitative and qualitative data will be gathered as a means to examine the impact of interprofessional education and collaboration interventions on interprofessional relationships, health care processes, and patient outcomes. Routes are suggested by which interprofessional education and collaboration interventions might affect knowledge translation and evidence-based practice. Zwarenstein, M., Reeves, S., Hammick , M., Koppel, I., & Atkins, J. (2007). Interprofessional education: Effects on professional practice and health care outcomes. The Cochrane Collaboration: Cochrane Reviews, (1) Interprofessional education (IPE) offers a way for professionals to work together. This study sought to assess the usefulness of IPE interventions compared to education in which the same professions were learning separately from one another. Zwarenstein, M., Reeves, S., & Perrier, L. (2005). Effectiveness of pre-licensure interprofessional education and post-licensure collaborative interventions. Journal of Interprofessional Care, 19(Supplement 1), 148-148-165. There is little empirical research evidence available regarding the effects of pre-licensure interprofessional education on patient/client care. There is an increasing body of evidence regarding the positive effects of post-licensure interprofessional education on patient/client care, however, the evidence is still weak. In order to guide practice in the future, it will be important to implement prelicensure and post-licensure interprofessional education with accompanying rigorous evaluation research. Page69