MENTAL HEALTH IN PRIMARY CARE TUTORS’ GUIDE 2015-16 UCL Medical School
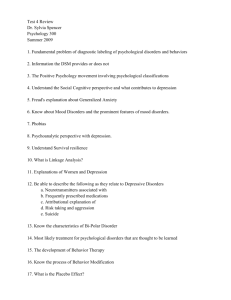
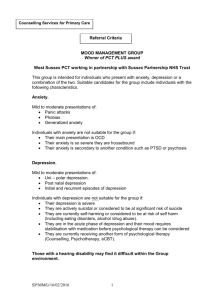
advertisement

UCL RESEARCH DEPARTMENT OF PRIMARY CARE AND POPULATION HEALTH MENTAL HEALTH IN PRIMARY CARE TUTORS’ GUIDE 2015-16 UCL Medical School Community Based Teaching Contents Contents 1 Contact details for the Department 2 1 1.1 1.2 1.3 1.4 1.5 Introduction 3 General aims and course history ................................................................................ 3 Structure..................................................................................................................... 3 Course content ........................................................................................................... 3 Overall structure ......................................................................................................... 4 Student outcomes ...................................................................................................... 4 2 Preparing for teaching 5 2.1 Getting Organised ...................................................................................................... 5 2.2 Planning and structuring a session ............................................................................. 5 2.3 Sample lesson plan & blank lesson plan..................................................................... 7 2.4 Recruiting patients ...................................................................................................... 9 2.5 Sample information sheet for patients ...................................................................... 11 2.6 The student - patient interview .................................................................................. 12 2.7 Advice for Students on Interviewing Patients with Mental Health Problems in Primary Care Settings ...................................................................................................................... 13 3 3.1 3.2 3.3 3.4 3.5 3.6 Details of sessions 14 Psychological morbidity in the community and somatic presentations ...................... 14 Depression and Anxiety............................................................................................ 23 Alcohol and Drug Abuse ........................................................................................... 31 Dementia in the older person.................................................................................... 44 Psychosis ................................................................................................................. 53 Eating Disorders ....................................................................................................... 62 4 4.1 4.2 4.3 4.4 Useful teaching skills 69 Questioning techniques ............................................................................................ 69 Getting and maintaining interest ............................................................................... 70 Facilitating feedback ................................................................................................. 71 Role Play .................................................................................................................. 71 5 5.1 5.2 5.3 5.4 5.5 Assessment, evaluation & support 72 Student examinations and final grades ..................................................................... 72 Feedback from students ........................................................................................... 73 Self and peer evaluation ........................................................................................... 73 Tutor support & professional development ............................................................... 75 Course evaluation and quality assurance ................................................................. 75 6 6.1 6.2 Further information 76 Reading & other resources list for tutors ................................................................... 76 The core curriculum for psychiatry ............................... Error! Bookmark not defined. Appendix 1 Error! Bookmark not defined. Appendix 2 77 Contact details for the Department Year 5 Course Lead: Dr Will Coppola w.coppola@ucl.ac.uk Course Administrator: Ms Carol Lynch carol.lynch@ucl.ac.uk 020 7794 0500 020 7472 6871 Department of Primary Care & Population Health UCL Medical School Royal Free Campus Rowland Hill Street London NW3 2PF Administrators for main hospital psychiatry attachment: Ms Deana D’Souza Undergraduate Administrator Department of Mental Health Sciences UCL Medical School Wolfson Building 48 Riding House Street London W1N 8AA Tel: 020 7679 9460 Fax: 020 7679 9426 Email: rejuuts@ucl.ac.uk Page 2 of 86 1 Introduction This module has been designed for medical students to gain experience of psychiatry from a general practice perspective. Our aim is that all students have the benefit of this attachment. 1.1 General aims The aims are that students should acquire knowledge and some experience of the common mental health disorders seen in General Practice, including their recognition, assessment, diagnosis and management; and students should develop their ability to take a holistic view of the patient, with an awareness of the broader physical, psychological and social issues. 1.2 Structure Hospital psychiatry teaching: All students have four weeks of psychiatry in their fifth year, half on a general adult psychiatry firm and the other half on a specialist firm (which can be anything from child & adolescent disorders through to old age psychiatry). These two blocks are incorporated into a thirteen week psychiatry, Care of the older person, ENT ophthalmology and palliative care teaching programme (HOPE) All students will have a week of introductory lectures at the beginning of the module. The students’ hospital experience in psychiatry and the type of patients they see can vary greatly, as there are a large number of different firms that they may be attached to. The amount of formal ‘clerking’ of patients and case presentation that they do during their hospital firms can be limited. Some have opportunities to do community outreach work with the consultant psychiatrist they are attached to, especially those attached to old age firms where home visits are more likely. In general though, students rarely meet patients with common mental disorders, unless these are very severe or are complicated by dual diagnosis. Core teaching programme: Students have core teaching all day every Monday and some Tuesdays. This is arranged as a series of ‘Problem Based Learning’ modules, which are based around problem scenarios such as ‘the sad patient’ or ‘the confused patient’. In the first week of their firm they are all taught psychiatric history taking and Mental State Examination, using videos. The modules are then arranged so that they get teaching on depression and schizophrenia early on in the programme. A copy of the core curriculum is given in Section Error! Reference source not found.. General Practice teaching structure: Students attend practices across North London in groups of 4 (occasionally in pairs) where they have 2 sessions of dedicated small group teaching with GP tutors. This is arranged as two half-day sessions or one full day and will be during the students’ 4 week psychiatry attachment. In addition, they receive a GP mental health seminar in week 3 of the placement. You will therefore find that students’ level of knowledge and experience of psychiatry may vary when they come to your practice. Attendance at their GP attachment is compulsory for all students. 1.3 Course content We have divided the content of the Psychiatry in General Practice course into 2 core sessions with topics which we would like all GP tutors to cover and then optional sessions from which two further sessions can be chosen at the tutor’s discretion. The topics can be covered in any order, apart from the session on psychological morbidity which is a logical first session. The topics are outlined below: Core Topics Page 3 of 86 Psychological morbidity in the community and somatic presentations Anxiety and depression Optional Topics Alcohol and drug abuse Dementia in the older person Eating disorders Psychosis in the community 1.4 Overall structure Our evaluations have shown that students like teachers to discuss the subject first, move on to seeing a patient and then have a final, more clinically orientated discussion. As noted earlier, they have relatively few opportunities to have structured feedback on either their history taking skills or case presentations and so they value this highly. The ‘patient contact’ has consistently been rated as the most positive aspect of their GP psychiatry attachments. Therefore as part of the teaching we expect all GP tutors to invite patients with common mental health problems to meet students. Students should be given opportunities to take full psychiatric histories from patients either singly or in pairs, to receive feedback on this individually and to discuss difficult management issues. We will discuss recommendations on managing the student-patient interview in Section 2. Details of each session are in Section 3. When it comes to deciding which of the optional sessions you wish to cover, if possible please discuss this with the students at the beginning of the attachment. Quite a few nowadays may be doing old age psychiatry as their general psychiatry placement and so may prefer other sessions. Those students not having an old age placement however may well be keen on the old age/dementia session. Obviously the key factor will be the patients you have available to help with teaching so it is fine not to offer the students the full range of optional sessions if you do not feel this is feasible in your practice. 1.5 Student outcomes By the end of the ‘Mental Health in the Community’ course we intend that the students should be able to: Identify common mental health problems in the community and describe factors that help and hinder the process of presentation and identification. Complete a full General Practice-orientated psychiatric assessment of a person with a common mental disorder, including a focused mental state examination. Apply management strategies in an integrated manner considering the person in their context rather than by their ‘diagnosis’ alone. Communicate effectively with adults with mental health problems. Show understanding of both patient and carer perspectives of living with a mental health problem. Page 4 of 86 2 Preparing for teaching The keys to effective teaching are organisation, planning and some basic teaching skills. In this section we will consider the organisation and planning involved in teaching psychiatry in General Practice for the first time. In Section 3.5 we will consider teaching skills helpful in small group teaching. 2.1 Getting Organised When am I teaching? This seems a very simple question, but make sure you are clear about the dates on which you will be required to teach as far in advance as possible. The course administrator should be able to give you dates for the blocks or firms of students that rotate throughout the academic year by August. Please inform them of any dates on which you know you will not be available e.g. holidays. Check that your practice knows when you are teaching, ensure that they understand that you need protected time, and advise your receptionist that the students will arrive at a certain time. It is also useful to write yourself a reminder in your diary two weeks before you are due to teach to allow yourself time to ask patients/ check that you have patients willing to participate. What am I teaching? The course curriculum for the ‘Mental Health in the Community’ module is detailed in Section 3. The emphasis of the GP part of the module is on helping students learn about the general practice perspective of mental health rather than teaching them ‘textbook’ psychiatry. We therefore do not expect them to learn exhaustive lists of diagnostic criteria for each topic, but rather consider the patient’s problems more holistically and help them understand some of the uncertainties. For each session there are some aims/objectives and a suggested basic structure and/or teaching methods. We do not mind which order you teach the sessions in this will usually depend most on availability of patients. The exact teaching methods are up to you, but we expect tutors to keep the overall aims of the module in mind and to try and achieve the suggested aims for each core session. 2.2 Planning and structuring a session Feedback from students over the years has given us a very clear idea of the structure that they find most helpful for learning. They like teachers to give sessions a clear beginning, middle and end (or introduction, body and closure). Introduction: Setting the right mood is very important. Students like to feel welcome in the practice, and as many of them will have had long journeys by public transport, refreshments on arrival are always popular. Check that there are no burning issues that they would like to discuss first. Give students a clear idea of what to expect by highlighting the aims/objectives (see below) and outlining a basic structure for the 4 sessions. Motivate the students to learn by explaining how relevant the skills learnt will be for them both as medical students and doctors, whatever their speciality. Remember that for students, assessment is a powerful driving force (see Section 5). Find out what students already know about the topic first. This helps to pitch the session at the right level and also aids learning. Long-term retention of knowledge is thought to develop by the formation of links between new knowledge and existing knowledge Page 5 of 86 networks in the brain. Activating this old knowledge in students’ minds at the start helps them to make these links. Aims & objectives: You are likely to hear the terms ‘aims and objectives’ frequently in your teaching role. In summary, an aim is the broad-brush intention of the teaching programme. An objective is a more detailed statement of exactly what you intend the student to know at the end of that period of time. This may seem a bit basic, but makes an important point. Students learn best if they know what they are setting out to do and how they are going to get there. We have given the aims and some suggested objectives for each topic. The students also receive these in their course book, but it helps to draw their attention to these (or your own adapted objectives) at the start of the session. Body or middle: We have outlined the overall structure of sessions in Section 1.4. Some useful tips to consider when planning the session: Less is more: most teachers have a tendency to try and cram in as much as they can in the session to ‘cover’ the topic. Students will actually learn more if you have less content, feel less rushed (and therefore more relaxed) and have opportunities to reflect and discuss key areas. Vary the stimulus: research has shown that human attention span is limited to around 15 minutes with no change in stimulus. It is therefore helpful when planning to break your session down into 15-minute chunks, and make sure you change the pace or teaching method for each ‘chunk’ or simply have a break. Go from the specific to the general: Students find it hard to learn general concepts without having examples in their mind of what you are talking about that they can relate this to. For example they may find it difficult talking about the concepts of overlap between physical, psychological and social aspects without first discussing this around a case example (either a real one they’ve seen or a hypothetical case). Closing a session A summary at the end would help students retain the most useful information. Their learning can also be helped by a sense of achievement; this can be done by assessing whether they’ve learnt anything by a short quiz or by returning to the objectives and asking them to recap the key points. You should check for their understanding and ask for their questions before closing the session, as otherwise you might get distracted on some small point rather than re-enforcing their learning of key points. The lesson plan A lesson plan is a simple method of planning what you will cover in advance. Using a lesson plan you will be able to see at a glance how much time you can allocate to each bit of a topic, what extra equipment you will need, and which areas you may like to read over beforehand. Within the session it is invaluable to help you tailor content to time, which is particularly useful if you find yourself getting side-tracked. You may find it useful to highlight in your lesson plan the core bits you don’t want to miss out, and identify areas or tasks you can omit if you are running out of time. A sample lesson plan and a blank lesson plan are included in Section 2.3 for you to photocopy and use if desired. Page 6 of 86 2.3 Sample lesson plan & blank lesson plan NB. This is only a sample given for one of the sessions – we suggest you use copies of the blank form to devise your own plans for other sessions. Content: Depression & anxiety Mood: introduce students, coffee, ask about experiences so far, informal chat, free to ask Q’s Motivate - why topic so important to know as Drs & for their exams Students learning needs on depression/ anxiety Introduction Outline your objectives; try to match these with their learning needs Outline structure of session, what going to do Prior knowledge; what do they already know about depression & anxiety? Small group discussion: students to define major & minor depression, anxiety. Discuss: When does normal distress, sadness or loneliness become depression or anxiety? What factors help & hinder diagnosis? Who is at risk? Recap - how common is depression & anxiety in primary care? Discuss background reading Summarise key learning points from discussion on flipchart Time Resources OHP (overhead projector)/ flipchart 5 min. tutors’ guide: aims & objectives 20 min. 5 OHP/flipchart Introduce patient interview: purpose of interview 5 (full history; also focus on patients experience of illness & treatments; at end formulate a focussed MSE - concentrate on affective components; prepare case presentation to me after) Body Recap on key parts in psychiatry history 10 examination for more junior students if necessary Ask students to prepare what will ask while brief patients re interview. 60 Student interview in surgery Closure Coffee for student Debriefing for patient 15 Student presentation cases Feedback on presentation skills & history/MSE Discussion of management issues. Use cases as examples & then generalise to general principles of management (directed by students) Any Q’s before close? Recap on key points from introduction & discussion -refer back to flipchart Get student to summarise key points in management (holistic not just drugs) Remind students about next session 10 5 Page 7 of 86 OHP/flipchart 20 OHP/flipchart 5 min. tutors’ guide: aims & objectives Title: Date: Content Introduction Body Closure Page 8 of 86 Time Resources 2.4 Recruiting patients It is worthwhile briefly considering what or who makes a good patient for teaching. A few attributes are clearly important. They should be approachable, available and willing to talk to the students at the appropriate time. Students should gain something from seeing them: they may, for example, have a good story to tell the students (this may be about their experiences of illness/health care and need not be limited to just an interesting medical history). There should be no significant communication barriers: for example, it may be necessary to arrange for interpreters to be present. A further factor worth considering is whether being involved in the teaching will be beneficial to the patient and/or to you: for example, if you feel that the patient would benefit from having longer than normal to talk about their illness, or if you expect that the students’ findings after their detailed interview will be informative to you. Research has shown that students gain more from teaching if they feel they have contributed to the patient’s care: it may be useful for the students (and for you) if you ask them to include a summary of their clerking in the patient’s notes. It is sensible to have a back-up plan as there will inevitably be times when the patient you’ve asked to come is not available. In this circumstance a stock of video clips (ideally locally made) or a pre-prepared written case vignette, each relevant to that session’s topic, would be useful. Case vignettes based on real patients, rather than ‘classical’ ones, tend to work best. Most tutors deliberately select a range of patients from different social backgrounds and different stages in their illness to meet the students. This seems to work very well and students respond positively to this. Students like, if possible, to see people who are at more acute stages of illness as well as those who are recovering/have recovered. We have found that patients who are still symptomatic when they see students respond well to the teaching, and many report a therapeutic benefit from spending time with students. Most patients value having the chance to talk about their problems at length to students, each of whom they generally view as an interested, sympathetic and non-judgemental third party. Being able to give something back and feel valued by their GP is also important and appears to raise patients’ self-esteem. A few patients find the students’ interview an emotional upheaval: this seems to be more likely in those who either have had or are currently having a severe or particularly traumatic episode; and possibly in those who lack insight into their problem. No patients or tutors have reported any long-term negative effects. Page 9 of 86 Briefing patients If you are involving patients in your teaching, it is important to get their informed consent for this. This will involve briefing the patients clearly regarding the interview. A further advantage of this briefing is that it may well alleviate the anxiety that some patients feel about meeting students for the first time. A checklist for what this briefing might include is given in the box below. It is good practice to provide written as well as oral information when asking for a patient’s consent. You could create a brief information sheet about the teaching to give to patients when you are recruiting them. We have included a sample information sheet, in Section 2.5, which you can adapt for your own practice. If you’d like patients to give some feedback about the interview, it’s also useful to give them some briefing about how to do this. Checklist for briefing patients about teaching Explain to patients: What the purpose of the student interview is: e.g. for students to learn about their particular condition; for students to practice talking to patients What the students will be doing/not doing: e.g. taking a history but not making physical examinations How long it is likely to take What level the students are at in terms of their experience What kinds of questions the students are likely to ask them What kind of information they should give students: e.g. give them their medical history; describe their experiences in hospital/General Practice; tell/not tell their diagnosis That medical students are bound by the same rules of confidentiality as doctors and will not disclose anything they have heard to anyone except the medical team involved in the patient’s care That, without affecting their medical care, they can refuse to take part, refuse to answer particular questions and change their mind about taking part at any time Who they should contact if they have any concerns about any issues raised by the contact with students, or if they want to give feedback to someone on how the student handled the interview. Page 10 of 86 2.5 Sample information sheet for patients Patient Information Sheet We would like to thank you for considering helping out with the training of student doctors from the UCL Medical School (University College London). Your GP practice is one of several across London that helps us to train student doctors. These students are on an attachment that is looking at mental health, emotional problems, stress, lifestyle (including alcohol and drugs) and physical problems related to stress. You have been asked to take part because your doctor (GP) thinks you may be able to help students to understand one or more of these problems better. These students are quite experienced and will be qualifying as doctors in a year or so. We feel it is quite important that they understand patients’ views of experiencing illness, and how to talk to patients about this. The students have been asked to talk to you about any health problems (physical, emotional or social) you have had and the effect these have had on your life. They will also be interested in any treatments you have had, and how helpful or unhelpful you have found these. They will not be performing any physical examination. The interview with the students usually lasts around an hour, and you are free to stop it at any time. You can also refuse to answer any particular questions if you want to - the students and your GP won’t mind. Your GP will probably see you very briefly afterwards to check how the interview has gone. If you have anything you would like to say about your time with the students, please feel free to tell your GP. Page 11 of 86 2.6 The student - patient interview This is the core part of the module and can be managed in a number of different ways. Some tutors like to sit in with students observing their interview; others leave them alone for an hour with a patient. Both ways generally work well, and it is rare for either the student or patient to become upset, although a few patients find it an emotional upheaval. From our evaluation the patients usually have no preference either way. Some students prefer to be left alone and others prefer to have the opportunity for their interviewing skills to be observed - it is probably helpful to offer the student a choice. We have done an extensive evaluation of student and patient attitudes towards the interviews and from this can make the following recommendations to tutors: Recommendations for tutors on the student-patient interview 1. It is important to provide briefing for both students and patient about what to expect from the interview. Patients like to know who they will be seeing and what questions they are likely to be asked. Students like to know the purpose of the interview and how it will differ from a standard psychiatric clerking. 2. Patients appreciate being reassured about the nature of the interview; that it is not a test and there are no right/wrong answers; and that they can stop the interview at any time if they wish. 3. Students often need help on how to start the interview. Both students and patients are often nervous at the start and it helps to give the students a structure they can use for breaking the ice. 4. Patients like to have feedback afterwards on things like whether they’ve been saying the right things and whether it has been useful to the students. Tutors should encourage students to do this at the end of their interview. 5. Some patients like the opportunity to be ‘de-briefed’ after the teaching. This is particularly the case when it is the first time they have been involved, but also when the interview has been emotionally distressing for them. Many tutors do this by seeing the patient very briefly immediately after the interview while sending the students off to have coffee and prepare their presentation. 6. Students may also benefit from ‘de-briefing’ about the process of interviewing patients before doing their ‘case presentation’. Page 12 of 86 2.7 Advice for Students on Interviewing Patients with Mental Health Problems in Primary Care Settings Interviewing patients with psychological morbidity in primary care History taking is paramount in interviewing patients with psychiatric or psychological problems, be it in primary or secondary care. You should already have had the chance to carry out full psychiatric clerking on several patients in the hospital part of your attachment. This is a crucial skill for you to acquire during your psychiatric attachment, but we would like to suggest that you alter the emphasis a little when interviewing some of the patients you will be meeting in a primary care setting and take the opportunity to gain some additional information which should help you to gain some understanding of mental illness from the patient’s perspective. Experience of the Illness: What has the illness meant to the patients, i.e. the experiences of having a mental health problem? How easy or difficult has it been to discuss it with professionals/family and friends? What impact has the illness had on work, personal or home life? What made them decide to consult a doctor about this problem and were the factors (e.g. fear of doctor’s response or sense of stigma about mental illness) that made this difficult? Experience of Treatment: What do they think about any treatment they have been given? If they have had drug treatment, do they, or did they, have any reservations about this (e.g. many patients think that anti-depressants are addictive)? Have they had any side effects? If they have had psychological therapies (counselling/contact with psychologist or psychotherapist), what was their experiences of and view about that? Have they had contact with any other health professionals or agencies, either health service or voluntary? What can they tell you about that experience? Information about their Problem: Do they know as much as they want to about their problem and the treatment they have had for it? Where have they got this information from? Are they satisfied with the care they have received? Is there anything they would like done differently? Mental State Examination: It is not usually feasible or practical to do a full mental state examination in primary care. However, it is important to keep in mind which areas you would like to cover. The majority of patients you will see in the GP surgery will have neurotic or affective disorders, so Appearance and Behaviour may be important, as well as Mood and sometimes Cognitive State. You may sometimes ant to screen for Psychotic Phenomena, such as abnormal beliefs or perceptions, as these may be hidden unless asked about it, but psychotic illness is much rarer in general practice that in hospital populations. When describing the mental state during this part of the attachment, just concentrate on the positive findings. Page 13 of 86 3 Details of sessions 3.1 Psychological morbidity in the community and somatic presentations Aims: For students to understand the differences in presentation of mental health problems in the community and primary care as contrasted with secondary care and factors influencing their detection. For students to gain experience in detecting somatic and other ‘inconspicuous’ presentations of psychological problems in primary care. Learning Objectives: By the end of this session students should be able to: Outline the distribution of psychological morbidity throughout the community and factors influencing patient presentation, recognition and diagnosis at different levels (Goldberg’s pyramid model of psychological morbidity). Discuss patient and doctor factors affecting diagnosis or not at a primary care level and the concept of conspicuous and inconspicuous psychological morbidity in primary care. Describe examples of patients presenting in primary care with somatic symptoms where there are significant underlying or accompanying psychological and / or social problems. Suggested learning methods: Introduction to the concepts and Goldberg’s pyramid model, asking students for their views (30-45 minutes) Students sit in individually on surgeries keeping the above concepts in mind whilst looking for conspicuous and possible inconspicuous psychological morbidity and / or somatic presentations amongst patients attending ordinary surgeries using log sheets provided. NB. These should be routine and not emergency surgeries to increase the likelihood of consultations with a psychological component. You may want to use previously videoed cases rather than acute surgeries and/or invite suitable patients to attend on the day. (1 –1/2 hours) Coffee break: (15 - 30minutes) Small group discussion of cases seen and how they may provide examples of the different levels of morbidity, conspicuous/inconspicuous morbidity and somatic presentations of psychological problems discussed. (45–60 minutes) Background reading: Hand-out: Psychological Morbidity in the Community Goldberg D & Huxley P. (1992). Common Mental Disorders: a bio-social model. London: Routledge. Page 14 of 86 Session 1 - Log of patients seen while sitting in with GP Presenting Complaint (include any psychological or Patient ID social factors the patient thinks may be important) GP Diagnosis (note any psychological or social factors that the GP thinks may be important) Page 15 of 86 Psychological morbidity Scale - 0 to 3 (3 = most severe) PSYCHOLOGICAL MORBIDITY IN THE COMMUNITY An estimated 15 - 30% of patients presenting to the GP have significant psychiatric or psychological problems1, which may either be the main reason that they are presenting or a significant associated reason. Because of a variety of possible factors, such as the perceived stigma of mental illness or a feeling that psychological symptoms are not appropriate to take to a ‘Medical consultation’ with a GP, not all patients will present with overt or ‘conspicuous’ psychological problems. As many as half of those seen who have significant psychological difficulties will present instead to their GP with physical or social problems – known as ‘inconspicuous’ psychological morbidity. Mental Illness in the Community - Model of Pathways to Psychiatric Care LEVEL 5: PSYCHIATRIC IN-PATIENTS 6/1,000 per year ........Filter 4.........Admission to Psychiatric Beds......... LEVEL 4: ALL PATIENTS of MENTAL ILLNESS SERVICES 24/1,000 per year .........Filter 3.........Decision to refer to Psychiatrist (5-10% of total detected)......... LEVEL 3: CONSPICUOUS primary care morbidity (GP identified) 102/1,000 per year .........Filter 2.........GP Ability to Detect Disorder…...... LEVEL 2: TOTAL psychiatric morbidity attending PRIMARY CARE 230/1,000 per year …......Filter 1.........Decision to consult / Illness Behaviour......... LEVEL 1: Psychiatric morbidity in the COMMUNITY 260-315/1,000 per year From Goldberg & Huxley’s Common Mental Disorders: a bio-social model (1992), this figure shows five levels and four filters, with estimates of the annual period prevalence rates at each level. Page 16 of 86 LEVEL 1 - Morbidity in the Community In a large national community based (door-step) survey involving interviews with 10,000 adults carried out in Great Britain2, the one week prevalence of any neurotic disorder was found to be 12.3% in males and 19.5% in females, so clearly these disorders are widespread in the community at any one time, as indicated previously in the work carried out by Goldberg et al. The breakdown into the various diagnostic categories is as below: Diagnosis Mixed Anxiety & Depression * General Anxiety Disorder * Depressive Disorder * All Phobias * Obsessive Compulsive Disorder* Panic Disorder * Any Neurotic Disorder (total) * Women per 1,000 99 34 25 14 15 9 195 Functional Psychosis # 4 Alcohol Dependence # 21 Drug Dependence # 15 * = one week prevalence Men per 1,000 54 28 17 7 9 8 123 4 75 29 # = one year prevalence All per 1,000 77 31 21 11 12 8 160 4 47 22 Certain socio-economic factors are linked with a higher prevalence of neurotic disorders: being female, of lower socio-economic class and/or with no formal educational qualifications, being unemployed, living in an urban area, being separated, divorced or widowed or also suffering from a physical complaint were all linked with a higher prevalence of common mental disorders. Certain ethnic groups also have a higher prevalence of some mental health problems, but this is a complex issue which varies across different ethnic groups and some of the differential can be explained by adjusting for the other socio-demographic variables listed above. There may be discrepancies in the use of diagnoses - especially anxiety/depression, so it may be more helpful to look at the symptoms of anxiety and depression as a continuum rather than categorical diagnoses. Current diagnostic labels do not predict outcome, but symptom severity does. As seen above in Goldberg’s pyramid, many but not all of those with a neurotic disorder will present to their GP. Filter 1 - Factors affecting patient’s decision to consult GPs The 'acceptability', or conversely the stigma of mental illness – this may affect men more than women Perceived attitude of GPs or other health-care professionals – i.e. facilitating attendance or not Attitude of the patient's family and social group – they may encourage or dissuade the patient from seeking help from particular agencies Severity of symptoms, their impact on function and their meaning to the person LEVEL 2 - Total Psychiatric Morbidity presenting to Primary Care The majority of patients with psychological symptoms of any severity do attend their GPs, although they may not attend with overt psychological symptoms. Concern that patients with significant morbidity may be being missed has led to a debate about the use of screening instruments in primary care. However, although there is some evidence that GPs may underdiagnose psychological morbidity in patients with whom they are not familiar, recent work has indicated that they are much less likely to miss significant psychological problems in Page 17 of 86 patients who they know well and with whom they have an on-going relationship3. The role of screening questionnaires should therefore be limited to ‘at risk’ groups – see also next session on Depression and Anxiety. Filter 2 - Factors affecting detection of psychological problems by GPs As stated above, probably only around 50% of patients present overtly with psychological problems. Whether or not an underlying psychological problem is detected can depend on both ‘doctor’ and ‘patient’ factors. GP factors associated with improved detection of psychological morbidity: Many of these are factors known as ‘good communication skills’, but there are also some which are specifically to do with the detection of psychological problems. Empathic manner - better eye contact, interrupts patient less, use of silences and sensitive to both verbal and non-verbal cues Clarification of presenting symptoms. Able to use directive questioning for physical symptoms, but also able to ask 'psychological' or open questions. Less giving of advice Avoids reading patient's notes during the interview and asks fewer questions about past history. Able to deal with over-talkativeness Flexibility and awareness that psychological problems can present via social problems or physical illness e.g. fatigue, palpitations, sleep disturbance, unexplained pains Previous training in psychiatry and acceptance cf. stigmatisation of mental illness (may also have a greater knowledge base in internal medicine generally) Use of video techniques in GP vocational training has been found to improve these skills. There are also certain groups of patients who are particularly at risk of having their psychological problems or difficulties missed by GPs, and probably other doctors also. Patient factors associated with reduced detection by GPs: Male Unmarried Children and young people: depression and suicide in young men is a particular current concern Elderly patients: anxiety or depression may be considered ‘inevitable’ and ‘part of life’ as people get older and have more losses Well-educated patients: (may seem counter-intuitive, but it may be an ‘identification with the patient’, with many doctors preferring not to think themselves at risk of psychological difficulties) Those who present with physical illness or physical symptoms (associated anxiety and depression is known to be under-diagnosed) Mothers with babies and / or young children Cases seen as ‘understandable' causes of depression e.g. bereavement, social difficulties Psychological morbidity in ethnic minorities: varies according to the disorder and the ethnic group LEVEL 3 - Conspicuous Psychiatric Morbidity in Primary Care Psychotic illnesses and people with personality problems are more likely to fall into the category of chronic disorders, with associated social disabilities in areas such as housing, employment and personal relationships. Although these patients form the minority of those on any GPs list with psychiatric problems, it is important that there is a system of regular review of their psychiatric, physical and social needs (this is likely to also involve the local Community Mental Health Team and possibly also Social Services). Page 18 of 86 As described above, however, most patients will present to their GP with ‘neurotic disorders’ and many of these will be self-limiting or short-lived and will not require active treatment. However, a significant minority of people will have symptoms severe enough to require either medication or psychological treatment or both, and some patients will go on to have chronic problems which may impact on the lives of both the patient and their family and friends, as well as being very expensive for the State in terms of both treatment (direct) costs and the costs of time off work and other social problems (indirect costs). If there is a delay in initiating effective treatment patients are at more risk of developing a chronic condition. Treatment strategies used to treat common mental disorders in primary care will be discussed further in later sessions. 90 – 95% of patients presenting to their GP will be treated by the GP alone, although they may also refer some patients to the practice counsellor or to a psychologist based either in the practice or in secondary care (local arrangements vary). Only a tiny minority will be referred to the secondary care psychiatrist, Crisis Team or Community Mental Health Team. Filter 3 - Decision to refer to the Psychiatric Services The 5 – 10% of patients most likely to be referred to psychiatric services by their GP are: Patients with psychotic symptoms Men - especially younger men Patients of higher socio-economic status Higher referral rates in urban areas Behavioural disturbance (violence, suicidal behaviour) Presence of co-morbidity (e.g. alcoholism and depression) Patients who have failed to respond to GP treatment Patients in social crises Request for referral from patient or family LEVEL 4 - patients seen by Psychiatric Services Filter 4 - Decision to Admit This is a controversial area at present. Factors influencing this include: Severity of the illness. Family and social factors. Other available support and local treatment resources. LEVEL 5 - Psychiatric In-patients 1 Goldberg D & Huxley P, (1992). Common Mental Disorders: a bio-social model. London: Routledge Jenkins R, Lewis G, Bebbington P, Brugha T, Farrell M, Gill B & Meltzer H. (1997). The national Psychiatric Morbidity Surveys of Great Britain – initial findings from the Household Survey. Psychological Medicine, 27, 775-789. 3 The MaGPIe Research Group (2005). The effectiveness of case-finding for mental health problems in primary care. British Journal of General Practice, 55, 665-669. 2 Page 19 of 86 MANAGEMENT OF ABNORMAL ILLNESS BEHAVIOUR & SOMATISATION NB. Use these notes in conjunction with the student hand-out which you will get at the ‘core teaching’ session on Somatisation in week 11 of the course. Adapted from Goldberg D, Benjamin S & Creed F. (1994) Abnormal Illness Behaviour in Psychiatry in Medical Practice (2nd ed. pp 243-6) London: Routledge. Management can be divided into: (i) prevention; (ii) general measures, which can be applied in any medical setting; (iii) specialised psychological approaches particularly for the more severe and persistent disorders. These will be considered briefly. The prevention of somatising disorders Doctors can unfortunately make a major contribution to the development and chronicity of abnormal illness behaviour and somatisation by responding to them inappropriately. It is important to avoid this by recognising these problems and learning more appropriate ways of responding. Suggestions include: Always provide clear information about negative clinical findings when you examine patients, and about negative investigations, otherwise they may assume the worst. Avoid giving patients speculative or spurious diagnoses. Medical records are full of these, and patients always remember these diagnoses rather than the subsequent retractions. Avoid treating disorders that the patient does not have - it is not unusual to find that patients who are told ‘There's nothing wrong with your heart' have been offered medication commonly used for heart disease, without adequate explanation. Obviously, the patient will believe they are seriously ill. Avoid carrying out and repeating investigations unless you think they are indicated, based on objective clinical findings. If you think they are indicated it is important to inform the patient of both the purpose and the result. Avoid arranging consultations and referrals unless you think they are indicated. Always explain why. Identify and acknowledge any psychological morbidity such as anxiety or depression and any psycho-social problems. The management of somatic presentations of mood disorders In cases where either no physical disease is demonstrable, or the physical disease which is present does not account for the patient's symptoms, it is essential to help the patient to see their symptoms in a different way. The worst thing you can do is to indicate by your words or actions that 'our investigations are normal, so there's nothing wrong with you’. The patient knows that isn't correct since the pain is real enough. The patient will often be complaining of numerous other psychological symptoms, but will not have connected them with the pain. You will have to help ‘make the link’. Let us suppose that a patient with severe epigastric pain has reported numerous symptoms of a depressive illness, and you have been asked to tell them that the results of all investigations, including a gastroscopy, are quite normal. You should now go through the following steps: Page 20 of 86 1. Provide clear information about negative physical findings while acknowledging the reality of the physical symptoms: “I'm glad to be able to tell you that you haven't got an ulcer or a tumour causing this pain, and all our investigations have been completely normal. Nevertheless, you have had a lot of pain, haven't you, and it has gone well beyond your usual indigestion pain?” (Having acknowledged the reality of the pain, pause for agreement.) 2. Specify the relevant mood state and associated symptoms and refer to the psychosocial factors that were previously noticed (this is called 'changing the agenda' - from the somatic complaints to the possible psychosocial causes): “When you came into hospital you told me how depressed you have been feeling since you didn't manage to get promoted at work. You mentioned that you have lost over a stone in weight and tended to wake early in the morning brooding about the things that you feel you've made a mess of in your life”. (Mention about three of the more striking symptoms, always including the mood disorder. Be prepared to remind your patient about the others if necessary.) 3. Explain about the relationship of mood and pain: “We think that you are probably depressed, and that your depression has made your pain very much worse than it would have been otherwise. It's one of the things that depression does, I'm afraid”. (Pause for patient's response; be prepared to repeat that you know that the pain is real, but depression can cause real pain.) 4. Emphasize the positive aspects of treatment and provide reassurance, based on a realistic idea of outcome: “We think that it is very important to give you some treatment for your depression. Most people get over this sort of illness completely but it is likely to take some time. I would now like to discuss some of the ways we might help you”. If you have got this far, you have done well. The patient's pain will act as a key symptom to indicate your success - or lack of it! - in dealing with the problem. The management of more persistent disorders All of the points covered in the preceding sections on treatment are relevant. If the problems continue, this is how to proceed: 1. Remember that anyone may have a physical disease, however obviously they show features of abnormal illness behaviour or an abnormal mental state. Frequently both physical and mental disorders occur in the same patient, so always look for evidence of both. All patients must be physically examined and investigated if they have a new episode of illness or new symptoms. 2. Few physical diagnoses are made as a result of further investigations more than six months after the initial presentation. Apart from the iatrogenic effects, repeated and inappropriate investigations also result in delay in initiating the appropriate psychological management. Page 21 of 86 3. At this stage it is essential to have a full psychological assessment, and the purpose should be explained to the patient and their cooperation sought. The first step is to look for evidence of affective disorder (described above) or other treatable mental disorders, and to treat them. 4. Review the past medical records, particularly if they are voluminous, because it may become evident that far from being a new disorder the present symptoms are part of a chronic or recurrent pattern of somatisation. 5. Arrange to see a key relative yourself in order to find out more about the psychological and social background of the disorder, to assess their knowledge and beliefs about the patient's symptoms (usually they have not been seen previously by a doctor and will probably share the patient's views that there is an undiagnosed physical illness), and to explain the nature of the disorder. 6. If appropriate ask a Social Worker to help by carrying out a home visit, by seeing other relatives on your behalf, or by providing some tangible social help for the family. 7. It is essential for all doctors involved to work closely together and to take a consistent approach towards psychological management. 8. The cause of these disorders is primarily psychological and therefore the management should be psychological. However, the specific causes of a patient's illness will rarely be evident from the initial history: the effect of somatisation and of secondary gain is that usually the patient is unaware of underlying problems and relates all the difficulties to physical disease. Other factors will usually only come to light after taking detailed histories from the patient and others. 9. Insight-orientated psychotherapy can help the patient to face underlying problems and find more constructive ways to adjust to them. Behavioural psychotherapy can help the patient to give up inappropriate disability, by using a structured rehabilitation programme and rewarding achievement. Cognitive therapy is used to reduce inappropriate focus on and beliefs about symptoms and to encourage positive attitudes and approaches to coping. 10. Often inappropriate attitudes and behaviours are reinforced by family members who are over-solicitous. They must therefore be included in the treatment plan to modify the effect they have on the patient. Sometimes they have a particular need to care for an invalid and are unable to tolerate the patient's recovery. They may then need help to find new ways of adjusting to their own problems. FURTHER READING Bass C & Benjamin S. (1993). The management of chronic somatization. British Journal of Psychiatry, 162: 472-80. Benjamin, S & Eminson DM. (1992). Abnormal illness behaviour: childhood experiences and long-term consequences. International Review of Psychiatry, 4: 55-70. Creed F & Guthrie E. (1993). Techniques for interviewing the somatizing patient. British Journal of Psychiatry, 162: 467-71. Ford CV. (1983). The Somatizing Disorders: Illness as a Way of Life. New York: Elsevier. Smith GR. (1991). Somatization Disorder in the Medical Setting. Washington, DC: American Psychiatric Press. Page 22 of 86 3.2 Depression and Anxiety Aims: To know about depression & anxiety in primary care: their prevalence, assessment and diagnostic issues, and the treatment options available. Learning Objectives: By the end of the session students should be able to: Discuss concepts of major and minor depression & anxiety disorders, their prevalence in primary care and factors affecting presentation and detection. (Some of this has already been covered in Section 3.1) Describe groups of patients at high risk of depression & anxiety, those who are at risk of being missed (e.g. post-natal mothers, the elderly etc.) and factors contributing to recurrent or chronic depression. Demonstrate the ability to undertake a psychiatric assessment of a patient with depression and/or anxiety in general practice. Describe the management of depression and anxiety in primary care, including a range of interventions and the potential role of other primary care team members. Suggested learning methods: Introduction to concepts & definitions, seeking students’ views. Students may have their own views on the concept of depression, its relationship to unhappiness, and its treatment. (30 - 45minutes) Students interview patients with depression and/or anxiety (this could include those who are fairly acutely/recently ill as well as more chronic examples). (1 - 1½ hours) Coffee break (15 - 30minutes) Small group discussion with case presentations by students, followed if time by thinking about different presentations of & treatments for anxiety & depression in primary care. (30 - 45minutes) Background reading: http://www.nice.org.uk/guidance/conditions-and-diseases/mental-health-and-behaviouralconditions/depression quick reference guide to NICE guidelines on depression Butler G & Hope T. (1995). Manage Your Mind. Oxford University Press. http://www.mind.org.uk/information-support/ for patient education https://moodgym.anu.edu.au/ for a CBT based programme of treatment Page 23 of 86 Prevalence Anxiety and depression are very common. They can occur independently or together. It is increasingly recognised that they most often occur together - at any one time about 8% of the UK population has “mixed anxiety and depression”, where each contributes to significant distress but neither is severe enough to be classified as a disorder in its own right. Some other common mental disorders are generalised anxiety disorder, depression categorised as “mild”, “moderate” or “severe” (see Box 1) and phobias. Both anxiety and depression are distressing and can be very debilitating. They can have a significant impact not only on the patient, but also on the patient’s family and friends, and are a major cause of absence from work. Depression and anxiety in primary care Most people feel down or anxious at times. Usually these feelings pass, but sometimes they linger and make it difficult for people to live their lives as normal. The degree to which people experience these symptoms and to which they interfere with their lives varies. In secondary care you may meet people whose depression is sufficiently severe to mean that they’ve been admitted to hospital. These patients will also be under the care of their GP once discharged. However, all GPs will also have many more patients who have problems with depression/anxiety of a severity that will probably never require admission. Some will benefit from an outpatient referral to secondary care (e.g. a psychiatrist if the depression is severe and not responding to treatment, or a psychologist for CBT if indicated) but many will have all their treatment entirely from the GP and possibly other members of the primary care team such as the practice counsellor. Identifying depression and anxiety in primary care We know that amongst people attending their GPs there are high rates of depression and anxiety. As discussed in the previous session on “psychological morbidity”, these symptoms may not be picked up on by the GP. Being alert to which groups are most at risk (e.g. mothers with young children, the elderly, people with chronic disease, people with a past history of depression or anxiety or other mental health problems) improves the chance of identifying the problem. Simply having a low threshold for asking about symptoms of depression and anxiety is worthwhile. Ask about symptoms when they’re suspected or when the patient is at particular risk. The following two screening questions can be useful when the GP (or other doctor such as in Casualty or Medical Out-Patients) is concerned about depression: During the past month have you often been bothered by feeling down, depressed, or hopeless? During the past month have you often been bothered by having little interest or pleasure in doing things you usually enjoy? An answer of “yes” to one of these should prompt the GP (or other doctor) to ask further questions. An answer of “no” suggests that depression is unlikely1. Given the high rates of depression amongst GP attendees, the routine screening of all patients for depression has been suggested. However a systematic review of studies using standardised questionnaires for this in primary care concluded that using them routinely was not worthwhile2. Using standardised questionnaires for focussed screening, though, may be useful; the Edinburgh Post-Natal Depression questionnaire, which health visitors routinely use in many areas of the UK, improves detection of post-natal depression in this high-risk group. Page 24 of 86 Psychiatric assessment Once a patient has mentioned symptoms of depression or anxiety they should be allowed to complete a description of their symptoms and the impact on their life. The GP, with limited time for individual appointments, will not usually carry out a full psychiatric assessment at this point, but will consider what more they need to know to inform management. They may well know the patient and already have details of their past medical and psychiatric history, and also their family and social history. They will however need to use prompts to encourage the patient to elaborate in areas where they do not have sufficient information to assess the severity of the current problems, and to get an idea of what treatment options may be appropriate and acceptable to the patient. There is still considerable stigma around both the identification of depression and its treatment. It is very important to establish the patient’s views, preconceptions and wishes about possible treatments, as the patient will need to understand the rationale for any treatment offered and agree to this if they are to be actively involved in the therapy, be it pharmacological or psychological. (There is considerable evidence that, although patients are prescribed large amounts of anti-depressants in the UK, many do not take the medication prescribed – often because their concerns have not been fully and clearly discussed with them). As a student, meeting the patient for the first time, a more complete assessment is likely to be appropriate. Remember to include: The symptoms – both biological and psychological NB. If the patient appears depressed, ask about suicide risk The impact of the problem on the patient, their family, friends, home and work Underlying circumstances which may be precipitants or perpetuating factors e.g. social or occupational factors, adverse life-events Remember to consider a physical cause e.g. hypothyroidism, drugs Past psychiatric and, given enough time, medical history Drug history (including recreational drugs, alcohol, + caffeine if anxiety) What the patient has tried for the symptoms and any problems e.g. side effects What are their thoughts and beliefs are about other possible treatments? Mental state examination, noting features of appearance, behaviour, rapport, speech, mood, thoughts, perception and cognition consistent with a possible mental health disorder. You are unlikely to need to ask about psychotic symptoms in this population. Page 25 of 86 Suicide risk Whenever a patient admits to symptoms of depression, suicide risk should be assessed. There is no evidence that this makes a patient more likely to attempt suicide; in fact being able to discuss these thoughts is a relief to many patients. Once the patient has let you know they have symptoms of depression and once you feel you have established some rapport (or as much as you can in that consultation), ask whether the patient has ever felt that life isn’t worth living, whilst explaining that this is both an extremely common thought and sometimes a difficult area for people to discuss. If they answer positively you should go on to ask whether they’ve ever thought of killing themselves. If so, then it is important to obtain more details as only with this information can you make a proper assessment of someone’s likely suicide risk. You need to know: Have they made any concrete plans? If so what, when and where? Are the means to carry this out available to them? Have they ever tried to harm themselves before? What did they do and what was the outcome? Did they tell anyone else? Have they made any concrete preparations (e.g. making a will, written a suicide note)? Do they think that any factors would stop them harming themselves e.g. consideration of the impact of the act on their close relatives or friends? Assess the risk of suicide and act appropriately. If an urgent, acute risk, refer to be seen that day by the Crisis Team. For less acute cases, but where there is still concern it may be appropriate to, start therapy and arrange more frequent GP follow-up. An urgent, but not same day, referral to secondary care may also be considered. Asking about suicide risk should be considered at every consultation re ongoing depression, including at follow-up. It may become irritating for the patient to have this specifically addressed at each visit if they are being followed up long-term. The GP or other doctor needs to use their knowledge of the patient to decide how and when to approach this subject. In addition, the GP should emphasise to the patient to come to the surgery sooner than otherwise planned if they have more negativity, hopelessness, a decline in mood or suicidal ideas (or more marked suicidal ideas if these have already been discussed). The GP should also ensure that the patient knows how to seek help urgently should they seriously consider suicide. Management of Depression and Anxiety The main medical treatments available are pharmacological and psychological, and the level of intervention offered should be appropriate to the severity of the problem. Patients should be encouraged to be actively involved in the choice of treatment. It is also crucial to consider the psycho-social aspects, which may be contributing to or even in some cases directly causing the problem. It is important to address these where possible in the patient’s management e.g. if financial debts are the main cause of someone’s anxiety or depression, part of the management should include helping them to find appropriate advice to deal with this, such as by contacting the Citizen’s Advice Bureau. However the psycho-social difficulties causing the problem may not always be resolvable e.g. someone may be the victim of severe torture or abuse in the past and may only be able to come to terms with this to a limited extent despite appropriate psychological therapy and they may then choose to take anti-depressants to help control their depression. When considering what options to offer someone seeing their GP for depression or anxiety a ‘stepped care’ approach may be useful, with more intensive ‘medical’ interventions being added in for more severe problems. Page 26 of 86 DEPRESSION ‘Mild’ or probably ‘self-limiting’ episodes ‘Watchful waiting’ – with a review within 2 weeks – may be appropriate. Information regarding the disorder and giving details of possible treatments (it is generally a good idea, to give patients something written to read later if appropriate to their condition). Guided self-help programme: advice on reading matter and/or useful websites/software. See recommended reading for suggestions. Exercise – the patient can be referred for help with this in some areas. Advice on anxiety management if appropriate, as anxiety and depression are often found together. Advice on sleep hygiene if insomnia e.g. keep bedroom quiet and dark, avoid stimulants in evening; go to bed at the same time every night; avoid catnaps. Referral for benefits or housing advice if appropriate. Pharmacological therapy is usually not indicated in mild depression. Exceptions include: where the patient has persistent troublesome symptoms (e.g. a condition of chronic low mood lasting at least two years and termed ‘chronic dysthymia’); and where the current mild depression is considered likely to progress to moderate or severe depression given that this has happened before in the same patient. ‘Moderately’ severe depression All the above may apply, apart from watchful waiting’ if the patient has significant, troubling and persistent symptoms when first seen. Antidepressant therapy should be considered in this group and discussed with the patient. Psychological therapies are more likely to be considered in this group (See box 2 re “talking therapies”). This is particularly important for a recurrent problem. Advice to the patient and possibly family and carers about self-help groups and support groups e.g. Alcoholics Anonymous, Depression Alliance, CRUSE (for bereavement), Medical Foundation for the Victims of Torture. See http://www.nimh.nih.gov for many more. ‘Severe’ Depressive Episode As above: in the moderately severe group, with secondary care referral if appropriate. Secondary care referral may be to a psychiatrist for particularly severe symptoms, further assessment of suicide risk, or if someone has failed to respond to GP care despite trying more than one group of anti-depressant drugs. It may also mean secondary care referral to a psychologist or psychotherapist if, as is often the case, these resources are not available within the practice. There is some evidence that pharmacotherapy and psychological therapy work better in combination rather than alone, particularly in the severely affected group. The National Institute for Clinical Excellence (NICE) recommends that patients in the severe group are offered both pharmacotherapy and cognitive behavioural therapy. Looking to the future Having had one episode of depression increases your chances of having another. For many, depression is a relapsing, remitting disease. When a patient is recovering from a bout of depression, it’s worth discussing what they might be able to do to avoid a recurrence of their symptoms, and what to do should their symptoms recur. It is important to advise the patient to seek help early in any future bout of depression, as there is evidence that early treatment reduces the severity of an episode. It is also worth warning people that any recurrence of their depressive symptoms once they are feeling better can feel particularly catastrophic and Page 27 of 86 unpleasant to them, but that they will get better again, just as they have done before, and that recognising and dealing with symptoms early can often reduce their severity and duration. People who have had severe depression often say after the event how important it was to them that other people such as health professionals continued to tell them that they would get better and held out hope at a time when they were feeling completely hopeless. ANXIETY The treatment of anxiety has much in common with the treatment of depression. Psychological therapy, guided self-help programmes and advice on self-help and support groups may all be used. The patient may be encouraged to address the problem underlying the anxiety. Information about the disease is particularly useful: a patient with panic attacks may be relieved that their symptoms don’t mean they’re going to die (although they may take some convincing of this!). Psychological approaches, particularly cognitive behavioural therapy, are indicated for patients who have not improved with relatively simple management strategies. There are no specific anxiolytic medications indicated, as drugs in the Benzodiazepine group may relieve symptoms of anxiety but cause major problems with addiction. However some people find benefit from the prn use of beta–blockers such as Propranolol to help with the physical symptoms of anxiety, and some anti-depressants may be indicated in more refractory cases, both for their anxiolytic effect and to treat any secondary depression. There is at least one SSRI licensed for each of PTSD, panic attacks, obsessive-compulsive disorder, agoraphobia and social phobia; and Venlafaxine is licensed for general anxiety disorder. Patients should be advised of potential side effects and withdrawal effects, and about the planned duration of treatment. As with depression, consideration of a possible medical cause is important e.g.: thyrotoxicosis. Avoidance of substances that can perpetuate symptoms is advisable: consumption of drinks containing caffeine/xanthine such as coffee, tea and Coca-Cola is often overlooked. 1 Arroll B, Khin N & Kerse N. (2003). Screening for depression in primary care with two verbally asked questions: cross sectional study. British Medical Journal, 327:1144-6. 2 Gilbody S, House A & Sheldon T. (2001). Routinely administered questionnaires for depression and anxiety: systematic review. British Medical Journal, 322:406-9. Page 28 of 86 Box 1: ICD-10 classification of depression (World Health Organisation) A symptoms: Depressed mood Loss of interest and enjoyment Reduced energy with increased fatigability B symptoms: Reduced concentration and attention Reduced self-esteem and self-confidence Ideas of guilt and unworthiness Bleak and pessimistic views of the future Ideas or acts of self-harm or suicide Disturbed sleep Diminished appetite Mild depression: at least 2 of A and 2 of B for at least 2 weeks Moderate depression: at least 2 of A and 3 of B for at least 2 weeks Severe depression: at least 3 of A and 4 of B for at least 2 weeks People with mild depression have some difficulty and people with moderate depression have considerable difficulty in continuing with social, work and domestic activities. People with severe depression are unlikely to be able to continue with these activities except to a very limited extent. Page 29 of 86 Box 2: Psychological or ‘Talking therapies’ Counselling Treatment focused on helping people cope with crises, understand feelings, identify issues, explore / make choices and ease distress. Usually short-term (maximum of 6 -12 sessions), are carried out by general practice counsellors and some voluntary organisations. Counsellors have varying degrees of training and are generally not psychologists. The GP may suggest the patient goes for counselling directed at a specific problem, e.g. through CRUSE (for bereavement) or through RELATE (for relationship guidance). Severity of problems Patient factors low to moderate preference for brief treatment Cognitive Behavioural Therapy Useful for marked symptomatic anxiety, depression – especially with negative thinking, behaviour problems A structured treatment focused on symptom change or other concrete / practical objectives agreed with patients, carried out by psychologists. The patient is expected to practice (“homework”) between sessions. A CBT session usually lasts an hour and a course of treatment is usually between 6 and 12 sessions - treatment for longer may sometimes be appropriate, particularly for people with chronic depression. Severity of problems Patient preference moderate to severe symptom change rather than self-exploration Psychodynamic Psychotherapy Useful for personality problems and severe interpersonal difficulties, particularly if the problem can be understood in terms of the patient’s life circumstances or way of viewing the world The treatment is focused on increasing the patient’s understanding of themselves, their problems and relationships and fostering internal change, usually longer term (more than 6 months). The therapist listens to the patient’s experiences exploring connections between present feelings and actions and past events. Can be individual or in a group. Private, NHS and some voluntary organisations Severity of problems Patient preference moderate to severe interest in self exploration Page 30 of 86 3.3 Alcohol and Drug Abuse Aims: To learn about the prevalence of drug and alcohol problems in primary care, their detection and appropriate management. Learning Objectives: By the end of the session students should be able to: Describe methods used in the recognition and management of alcohol and drug abuse by the primary care team. Demonstrate the ability to take an appropriate alcohol and/or illicit drugs history. Discuss the impact of alcohol and drug abuse on the mental and physical health and social functioning of the client group. Outline the resources available to manage alcohol and drug abuse in the community, and their appropriate uses. Suggested learning methods: Overview of the recognition of alcohol and drug abuse by the primary care team and ways in which patients may present in primary care. May include discussion of students’ own ‘alcohol diary’ for previous week and/or role-play (see Section 4.4 of tutor’s guide). (30 - 45 minutes) Students to interview patients who have been asked to come up to the surgery or at a community alcohol/drug centre. (1 - 1½ hours) Coffee break (15 - 30minutes) Small group discussion of cases seen, the associated morbidity of alcohol and drug abuse and their management in the community. (30 - 45minutes) Background reading: Alcohol History hand-out Five shot, AUDIT-C questionnaires ‘Facts about drugs’ hand-out Page 31 of 86 ALCOHOL MISUSE: the size of the problem Responsible for 30% of hospital admissions1 Involved in 80% of suicides Responsible for 25,000-200,000 deaths in England and Wales from 1997-20022,3,4 (i.e. 5,000 – 40,000 deaths per annum) Costs of medical and social services for heavy drinkers >£2,000m per year About 1.2 million incidents of alcohol-related violence in England & Wales in 19995. Current limits of “safe drinking” Royal College of Physicians: men 21 units/week; women <14 units / week Department of Health: men 3-4 units/day, women 2-3 units /day 1 unit ~ 10 ml of ethanol = half pint of beer, or = a small glass of wine, or = a single shot of spirits Drinking excessively Alcohol abuse is a common problem. It may be a cause, contributing factor or consequence of mental illness. There are three levels of pathology shown below. The progression between them is not clear-cut. Excessive Drinking Problem Drinking Alcohol Dependency Drinking alcohol is in excess Excessive drinking with Excessive drinking with of safe limits adverse consequences physical and psychological dependency (see criteria below) Alcohol dependence syndrome This is a cluster of behavioural, cognitive and physiological phenomena that develops after repeated alcohol use and typically includes: A strong desire to drink alcohol Difficulty in controlling its use Persisting in drinking alcohol despite harmful consequences A higher priority given to alcohol than to other activities/obligations e.g. family, work Increased tolerance to the effects of alcohol Sometimes withdrawal symptoms Alcohol withdrawal symptoms occur when the blood alcohol level is low, most commonly in the mornings. They include sweats, tremors, anxiety, sometimes hallucinations and even seizures. Alcohol brings relief to these symptoms; that’s why some people feel the need for a drink first thing in the morning. Page 32 of 86 ALCOHOL IN THE UK 7% of men (1.6 million) and 14% of women (3.3 million) aged 18 and over drink more than 21 and 14 units a week 6% of men (1.3 million) and 2% of women (0.5 million) drink over 50 and 35 units a week, the levels regarded as harmful About 47 in 1000 adults, more than 1 in 25, are dependent on alcohol Effects of excessive drinking Physical GI: e.g. dyspepsia, cirrhosis, varices, esophagitis, carcinoma oesophagus CVS: e.g. ischaemic heart disease, CVA and cardiomyopathy CNS: e.g. peripheral neuropathy, cerebellar degeneration, myopathy, Wernicke’s encephalopathy Psychological Depression and anxiety Alcoholic hallucinosis (“DTs”=delirium tremens) Memory impairment, including alcoholic amnesia and Korsakov’s syndrome Social Marital and family problems Work problems Debt Crime and vagrancy Detection of alcohol problems Early detection is valuable as brief intervention by the GP is more likely to be effective at an earlier than at a later stage. When problem drinking is long established, especially when the patient is alcohol dependent, it is much more difficult to treat the patient. The diagnosis is largely made on history. Examination and investigative findings (e.g. evidence of liver disease, macrocytosis) may raise the GP’s suspicions that excessive alcohol intake is a problem. Some GPs and Practice Nurses will use a questionnaire to screen for excessive alcohol intake during lifestyle reviews or if they suspect that alcohol use may be problematic (see examples after this hand-out). Some prefer simply to ask about alcohol and ask relevant questions until they are satisfied that they know whether alcohol is likely to be a problem for the patient, and if so to what degree. Imagine what it might feel like being asked about your alcohol intake. It is very important that health care professionals maintain a non-judgemental approach when asking about alcohol. This way the patient is less likely to underestimate their consumption in an attempt to avoid scorn, and more likely to be receptive to ideas about hazards related to their drinking. Page 33 of 86 GPs & Practice Nurses are likely to ask about alcohol: As part of a general lifestyle review (including smoking, exercise, diet etc.) When the patient has scored beyond the threshold for likely alcohol problems on a screening questionnaire (see examples after this hand-out) When the patient presents with problems that may be related to alcohol, e.g. depression; indigestion; hypertension; seizures; frequent accidents; financial, marital or legal problems When examination/investigative findings suggest possible adverse effects of alcohol When alcohol consumption is excessive a full alcohol history should be sought, taking care not to offend the patient. The history should include: What is drunk: (beer, spirits, cider etc.) How much is drunk How often (usual consumption a week is a useful measure) Where (in the pub, at home, at work etc.) When drinking starts during the day – may be worth specifically asking about ‘eyeopeners’ Triggers - availability of alcohol, current stresses How long ago they started drinking excessively and why? Any withdrawal symptoms – may be worth specifically mentioning DTs, black-outs, fits What patient did & how long they succeeded in any previous attempts to cut down Predisposing factors: family history of alcoholism, depression Complications – psychological, physical, social, economic The patient’s view on their own drinking – are they interested in cutting down? Note that factors underlying the alcohol problem, for example depression, debt and relationship problems, may be exacerbated by the alcohol problem. Management When considering what one might do for any patient with addiction, whether to alcohol, drugs or tobacco, it is worth considering the cycle of change. Pre-contemplation Relapse Change persistence Contemplation Change instigation From Prochaska & Di Clemente, 19866 Page 34 of 86 When change would improve the patient’s health, the GP and Practice Nurse will aim to encourage the patient from pre-contemplation (when the patient has no interest in changing) towards change instigation and persistence. The actual change may be a reduction in use; change to safer use (e.g. from injecting heroin of uncertain strength to taking oral methadone of reliable strength); or abstinence. Relapse occurs often and health care professionals may share the patient’s disappointment at this, but should try not to share the patient’s despondency: it frequently takes more than one attempt before the patient manages to stay in “persistence”. Management of alcohol problems As stated previously, detecting an alcohol problem early on makes it easier to deal with. There is evidence that a 5 - 10 minute intervention in general practice with follow-up can lead to around 25 - 35% reduction in alcohol consumption; and to the return of 20 - 30% of excessive drinkers to sensible levels of drinking7. It is therefore definitely worth doing, although it can be difficult to predict who the responders will be. Such a brief intervention might use the FRAMES model (adapted from Miller and Sanchez, 19948): F feedback - assessment and evaluation of problem, follow-up R responsibility - emphasising drinking by choice A advice - explicit advice on changing drinking behaviour, offer written information M menu - offering alternative goals and strategies e.g. drinking record sheet E empathy - role of counsellor important, ensure patient feels you’re on their side S self-efficacy - instilling optimism that goals achievable The more significant the patient’s alcohol-related problems, especially when the patient is alcohol dependent, the more difficult treatment is. During assessment the patient may recognise their problem more clearly. If the patient is interested in change, the health care professional should help them to identify goals. These goals should include dealing not just with alcohol consumption but also with accompanying problems such as financial, occupational and marital issues. When a patient has significant alcohol problems, the goal regarding alcohol is often abstinence, as controlled drinking is very difficult to achieve for many such people. The patient may negotiate goals with the GP; alternatively the GP may refer the patient on to an alcohol support service (which usually offers support for people on illegal drugs too). Supportive therapy such as cognitive behavioural therapy (e.g. re how to deal with social situations without drinking alcohol) and drug therapy (e.g. short term benzodiazpines to reduce withdrawal symptoms on stopping alcohol) may be offered. In addition the patient may choose to join a voluntary group for people with alcohol problems such as Alcoholics Anonymous or AlAnon. Some heavy drinkers may choose to live for a while (often 3 months) in a supervised community of people coming off alcohol. There is often a rule of abstinence from alcohol during the stay. Staff offer support and treatment to the residents. For some heavy drinkers withdrawal may put them so at risk of severe symptoms (e.g. seizures), that the withdrawal necessitates intense medical supervision and so hospital admission. Some patients may prefer this method of withdrawal, finding the supervised environment supportive to their abstinence. Relapse prevention Someone who has been a heavy drinker is always at risk of returning to their old drinking habits. Persistence in better habits is difficult: continuing support from the GP, NHS support services and from voluntary organisations is valuable. The patient should have a plan as to what to do if they feel very tempted to revert to old habits or if they relapse. Sometimes role- Page 35 of 86 play is useful: the patient can practice what they’ll do when they’re exposed to a strong trigger to drink. SUBSTANCE MISUSE See ‘facts about drugs’ hand-out for a list of illegal drugs, why they are taken, what their effects on health are and what they are commonly known as by users. These drugs are classified according to law: Class A drugs are amphetamines when they’ve been prepared for injection, cocaine, crack, ecstasy, heroin, methadone, LSD and magic mushrooms. As with alcohol, many people manage to use recreational drugs without major problems. However, the use of recreational drugs (“substances”) can become out of control for some people, and is then no longer just for recreational purposes; substances have become a more essential element of these peoples’ lives. Users of opiates are particularly at risk of becoming such “problem drug users”, as opiates are physically addictive. This addiction, together with the risk of withdrawal symptoms, means that use of opiates is more likely to become out of control than use of, say, ecstasy or cocaine. Problem drug users can have major health and social problems, with huge costs to themselves and to the public. 3-6% (1.5-3 million) of people in England & Wales use Class A drugs regularly without major problems. About a third of these are under 259. A further 0.5-1.0% (280,000 – 500,000) of people in England & Wales are problem Class A drug users9. There were about 7000 deaths related to poisoning with Class A drugs in England and Wales from 1997-2002. The vast majority of these were related to opiates2,3,4. NHS costs of problem Class A drug use are estimated at £288-514 million. Total costs of health and social consequences of problem Class A drug use are estimated at £13 – 22 billion per year, crime making up a large part of this. Just as with alcohol, problematic use of recreational drugs can be classified. The definition of “substance dependence” has just the same features as alcohol dependence, except that the word “alcohol” is exchanged throughout for “substance”. Detection of problems with substance misuse As with alcohol, the GP or Practice Nurse may ask about recreational drugs during lifestyle review, and when suspicions are raised on clinical grounds (e.g. clouded consciousness; depression; over- stimulation; odd behaviour; weight loss; needle tracks and thrombosis of veins; issues related to injecting such as infected injection sites, hepatitis, HIV; social/occupational problems; frequent accidents/arguments). In the case of benzodiazepine addiction, the GP may well be aware of the problem as the GP may be prescribing it: this addiction is usually iatrogenic, with the patient having started the drug at a doctor’s advice and then not found out they are able to stop it themselves. The history of recreational drug use has much in common with the history regarding alcohol consumption. The patient may, however, be taking a range of drugs and it is important to find out details regarding all of these (Withdrawal symptoms vary with different drugs; see details in ‘facts about drugs’ hand-out). In addition, the patient should be asked about risky behaviour such as injecting, especially injecting into the groin or neck (risk of arterial embolus) or into an infected site, and if injecting at all, whether they know how to prevent transmission of blood-borne viruses. Page 36 of 86 Urine testing can be helpful: approximate detectable duration of drugs in urine is shown below: Drug/Metabolite Duration of detectability Amphetamines 2 days Benzos Short acting e.g. triazolam Intermediate e.g. temazepam Long acting e.g. diazepam 24 hours 2-5 days >=7 days Buprenorphine 8 days Cocaine 2-3 days Methadone 7-9 days Codeine,dihydrocodeine, morphine, heroin etc 48 hours Cannabis Single use Chronic heavy use 3-4 days Up to 45 days Management The management of the problematic use of recreational drugs has much in common with the management of problematic alcohol use. The health care professional needs to take a complete history and to negotiate goals with the patient. In addition, though, the patient needs support and advice about how to minimise the risks posed by injecting if this is relevant. Patients on opiates usually benefit from transferring from the injection of heroin to the oral intake of methadone. There are some particular hazards in making this transfer – patients may overestimate their heroin consumption (which may be difficult to estimate anyway as when bought illegally it is often bulked up with other powder) with the goal of receiving a pleasurably high dose of methadone, paying little attention to the risk of overdose and death. To minimise the risks of initiating methadone, a doctor will act cautiously. Before prescribing methadone, they will perform a urine toxins test to check that the patient is actually taking opiates. They will start the patient on a small dose, titrating up to an effective beneficial dose. They will initially only prescribe methadone for supervised consumption, usually monitored by the pharmacist. Early prescriptions may be for just a day or two at a time and subsequent prescriptions will be of one to two weeks duration at most. Methadone is not without its own problems – many people say that withdrawal symptoms from methadone are problematic and there is also a risk of overdose, with the possibility of respiratory depression, coma and death. Some centres are now starting people addicted to heroin on a withdrawal regime using buprenorphine. This has been around for many years in the form Temgesic, and is used as an analgesic. It is, however, also now licensed for the treatment of opiate addiction. It has been used extensively in France and other European countries and is beginning to take off in the UK. It is especially being used in outpatient detoxification programmes and has also been suggested as an alternative to methadone in pregnant drug users. Page 37 of 86 Buprenorphine acts as a partial opiate agonist, which means that the net effect it has is dependent on what state the patient’s receptors are in. If there is a lot of heroin or methadone around then it displaces them but has less agonist activity itself and often puts the patient into opiate withdrawal. If they are already in early withdrawal then the net effect is of an agonist and it relieves the withdrawal. It is therefore important that the first dose is taken under supervision, with the patient having been clean of opiates for at least 24 hours, and that their clinical state is then monitored for a few hours. Patients who prefer buprenorphine to methadone say that it is less sedative, reduces the effect of any "on- top" heroin use and is less nausea-inducing than methadone. Buprenorphine has what is known as a therapeutic ceiling, which means that if you continue to increase the dose the effect that the drug has starts to level off. When deaths have occurred with buprenorphine they have usually been attributed to mixing the drug with alcohol and benzodiazepines. It is long acting and only needs to be taken once a day. Withdrawal symptoms are less severe than with methadone. It is taken sublingually as a tablet and needs to be left under the tongue until it has fully dissolved. If it is swallowed it is virtually ineffective. Buprenorphine is probably more suitable for people who are able to be more regular and organised in taking their medication. It can also be used to wean patients off methadone in a two-stage process to come off opiates. Drug support centres are generally a good source of advice for doctors regarding how best to help their patients. Many GPs make use of these for the initiation of methadone or buprenorphine regimes, and for the additional social and psychological support they can offer. Some GPs will then prescribe the methadone or buprenorphine themselves, under the condition that the patient stays in contact with both the GP and the drug support centre. Other GPs will ask the drug support centre to arrange the continuing prescription of these drugs. Some patients on methadone or buprenorphine may choose to reduce the dose gradually so that they come off altogether; others may choose to continue on a stable “maintenance” dose, with no aim of coming off it. This is probably more likely with methadone, which many patients say is very difficult to withdraw from because of the withdrawal effects. Whilst on methadone or buprenorphine the patient has less inclination to obtain drugs on the street and so is less likely to turn to stealing to fund this. They are also less likely to inject, thus avoiding the associated risks, and have more chance of addressing social and psychological issues. Both drugs are less sedating than heroin. Maintenance, then, is an improvement on taking heroin and should be regarded as a success in terms of the cycle of change. Relapse prevention Whatever improvement the patient makes in terms of their drug use, their persistence in this change can be assisted by additional support. As with treatment for alcohol problems, a range of psychological treatments are available: counselling, cognitive behavioural therapy, group therapy. The patient may identify strong triggers for substance use and practice what they will do when exposed again to such triggers. Becoming part of normal society may be difficult for some people who have had problems with drugs. In particular their social circle may revolve around drug use and it can be hard for them to make new friendships. Such difficulties may push them back towards problem drug use. Rehabilitation aims to help people back into normal society: work and social activities are offered initially in sheltered surroundings, often with supervised accommodation. The aim is for patients to gradually take more responsibility for their lives, although support should still be available when the transition to normal work and accommodation has been made. Page 38 of 86 FIVE SHOT QUESTIONNAIRE (At cut-off = 2.5, sensitivity = 74.2%, specificity = 80.9% for alcohol abuse/dependence) 1. (0.0) (0.5) (1.0) (1.5) (2.0) How often do you have a drink containing alcohol? Never Monthly or less Two to four times a month Two to three times a week Four or more times a week 2. (0.0) (0.5) (1.0) (1.5) (2.0) How many drinks containing alcohol do you have on a typical day when you are drinking? 1 or 2 3 or 4 5 or 6 7 to 9 10 or more 3. (0.0) (1.0) Have people annoyed you by criticising your drinking? No Yes 4. (0.0) (1.0) Have you ever felt bad or guilty about your drinking? No Yes 5. Have you ever had a drink first thing in the morning to steady your nerves or get rid of a hangover? No Yes (0.0) (1.0) Page 39 of 86 AUDIT – C (At cut-off = 5, sensitivity = 78%, specificity = 74.9% for alcohol abuse/dependence) AUDIT – C is derived from the lengthier AUDIT questionnaire 1. (0) (1) (2) (3) (4) How often do you have a drink containing alcohol? Never Monthly or less Two to four times a month Two to three times a week Four or more times a week 2. (0) (1) (2) (3) (4) How many drinks containing alcohol do you have on a typical day when you are drinking? 1 or 2 3 or 4 5 or 6 7 to 9 10 or more 3. (0) (1) (2) (3) (4) How often do you have six or more drinks on one occasion? Never Less than monthly Monthly Weekly Daily or almost daily 1 Chick J. (1994). Alcohol problems in the general hospital. British Medical Bulletin, 50:200-10. Office for National Statistics. (2002). Deaths related to drug poisoning: results for England and Wales, 1993-2000. Health Statistics Quarterly, 13: 76 - 82. 3 Office for National Statistics. (2003). Deaths related to drug poisoning: results for England and Wales, 1997-2001. Health Statistics Quarterly, 17: 65 - 71. 4 Office for National Statistics. (2004). Deaths related to drug poisoning: England and Wales, 19982002. Health Statistics Quarterly, 21: 59 - 66. 5 Kershaw C, Budd T, Kinshott G, Mattinson J, Mayhew P & Myhill A. (2000). The 2000 British Crime Survey. Home Office Statistical Bulletin, 18/00. London: Home Office. 6 Prochaska, J & DiClemente, C. (1986). Toward a comprehensive model of change. In WR Miller & N Heather (Eds): Treating addictive behaviours: processes of change, pp 3-27. New York: Plenum. 7 Freemantle N, Gill P, Godfrey C, Long A, Richards C, Sheldon TA, Song F & Webb J. (1993). Brief interventions and alcohol use. Quality in Health Care, 2(4): 267-73. 8 Miller W & Sanchez M. (1994). Motivating young adults for treatment and lifestyle change. In G Howard (Ed): Issues in alcohol use and misuse by young adults, pp 55-82. Notre Dame: University of Notre Dame Press. 9 Godfrey C, Eaton G, McDougall C & Culyer A. (2002). The economic and social costs of Class A drug use in England & Wales, 2000. Home Office Research Study 249. London: Home Office. 2 Page 40 of 86 Page 41 of 86 Page 42 of 86 Page 43 of 86 3.4 Dementia in the older person Aims: To introduce students to the care of elderly people with dementia in the community, and to the resources available to provide and support this. [If you have difficulty finding people with dementia for the students to see, you might wish to use this session to teach about depression in the elderly.] Learning Outcomes: By the end of this session students should be able to: Describe the prevalence, common presentations and approaches to management of dementia in the community. Complete an assessment of an older person with cognitive impairment. Complete an assessment of the needs of the older person’s main carer(s), with regard to their role as carer. Discuss the range of resources available in the community to support older people with dementia and their carers. Suggested learning methods: Introduction to the common presentations of dementia and its management in the community. Discussion regarding the clinical skills required to identify dementia and the resources available to support the management of dementia in the community. (30-45 minutes) Interview a patient with dementia and their main carer at home, and practice cognitive assessment. (1 - 1½ hours) Coffee break (15 - 30 minutes) Presentation of case history with feedback and discussion of management issues (30- 45 minutes) Background reading: “About dementia” on Alzheimer’s Society website www.alzheimers.org.uk. Deals with all dementias, not just Alzheimer’s. Useful website for all involved. Mini Mental State Examination Page 44 of 86 Definition Dementia is a progressive loss of a variety of mental functions which usually, but not always, occurs in old age. Common symptoms include forgetfulness, spatial disorientation, apraxia and difficulty in naming people and things. These may be accompanied by a decline in emotional control, social behaviour and motivation, along with personality change. The scale of the problem There are an estimated 700,000 people with Alzheimer's disease and the other dementias in the UK. This has risen by about 100,000 over the past 10 years and, given the aging population, is expected to rise further1. The majority of people with dementia live at home1. About a third of people with dementia live alone1. The average full time GP can expect to be responsible for about 20 people with dementia, depending on the age profile of the population they serve. Presentation Dementia is not only a psychiatric illness, but has widespread physical and social manifestations. There is commonly some delay in the presentation of dementia. It may become apparent to the GP because: The person with dementia complains of memory loss. More commonly, someone close to the person with dementia complains of their decline in memory and/or personality and behavioural changes. Dementia may be suspected when the person receives medical care for another illness. The most notable feature of early dementia is usually short term memory loss. Family or friends may notice the memory loss, and may also comment to the GP on: A decline in standards of self-care and presentation (e.g. not washing as often, wearing dirty clothes, leaving hair uncombed). Difficulty in performing simple tasks (e.g. bringing a chair from another room, making a pot of tea). Loss of interest in activities in which the person previously participated frequently (e.g. housework, attending religious services, visiting friends). Personality change with disinhibition, lack of emotions, irritability or low mood. Disorientation in both time and place, with the person forgetting routes close to home and getting muddled about times of day. Differential diagnosis It is important that reversible diseases that mimic dementia are excluded. The most important of these are depression and delirium. Delirium is usually of recent onset and is associated with impairment of consciousness. Depression may be difficult to exclude. Asking the patient and their social contacts regarding mood is essential. Note that both delirium and depression can co-exist with dementia and are more common in people with dementia. Rarer causes of dementia, such as hypothyroidism, syphilis, low vitamin B12 and low folate, should be excluded. The combination of incontinence, a wide-based gait and dementia should alert the doctor to the possibility of normal pressure hydrocephalus, which can be corrected surgically. An alcohol history should be taken to assess whether the dementia might be related to alcohol consumption and/or thiamine deficiency, in which case abstinence from alcohol and thiamine supplements could halt decline. Page 45 of 86 Common types of dementia Alzheimer's disease is the most common form of dementia. Although there is some disagreement over the precise numbers, the proportions of those with different forms of dementia can be broken down as follows1: Alzheimer's disease Vascular dementia Dementia with Lewy bodies Other dementias 55% 20% 15% 10% Each type of dementia involves a progressive decline in a variety of cognitive functions, affecting memory, personality and behaviour. Alzheimer’s is differentiated from other dementias largely on the basis of the additional features of the other dementias. Differentiating which sort of dementia the patient has is useful for management, including advising carers of what is to come. However, post mortems have shown that we often differentiate wrongly. Remember that a patient may have more than one form of dementia. The title “Vascular dementia” incorporates multi-infarct dementia, sub-cortical vascular dementia and perhaps incorrectly the cognitive decline that may ensue following a single stroke. Multi-infarct dementia is associated with a more stepwise decline in cognitive function than the gradual decline in Alzheimer’s, whilst sub-cortical vascular dementia has a less clearly stepwise decline and may be difficult to differentiate from Alzheimer’s. However, vascular dementia is generally more likely than Alzheimer’s to be associated with focal motor signs; these features reflect its pathology. Visual hallucinations are more common and more florid in Lewy body dementia than in vascular dementia or Alzheimer’s. People with Lewy body dementia tend to have more marked fluctuations in cognitive impairment and are more prone to extrapyramidal disorder (like Parkinson’s disease). These Parkinsonian features may first become apparent when the patient takes neuroleptics; care should be taken to avoid these in Lewy body dementia. Assessment of the person with impaired cognitive function The GP will be assessing a number of features simultaneously. It is very important to identify delirium, as failure to act on this can be disastrous. Depression will also be at the forefront of the GP’s mind. Remember that the GP will need the help of the patient’s close contacts for a reliable history. The assessment is lengthy and the GP will probably complete this over more than one consultation. History Find out what has been going on: Has the patient been forgetful? If so, how has this been evident? Has the patient changed in other ways? Any change in behaviour/personality? How long have these changes been going on? Have these been gradual or is there a more stepwise deterioration? If the history is of a recent abrupt decline in cognitive function, and there is impairment of consciousness, then assume this is delirium - look for the physical cause and consider admission to hospital. Mental / physical assessment The main aim here is to pick up reversible disease. You may also identify symptoms and signs that will help to categorise the dementia. Ask about physical symptoms – a review of systems may be appropriate. Ask about symptoms of depression. Find out about the patient’s social circumstances. Page 46 of 86 Review the patient’s medication. All sorts of medicines can cause a decline in cognitive functioning as a side effect, and the elderly are particularly susceptible to the side effects of drugs. Remember to ask about alcohol and smoking. A detailed physical (including neurological) examination should follow. The investigations chosen will depend on your assessment. But for elderly patients with impaired cognitive function, basic tests will generally include: FBC & ESR Serum B12 & red cell folate Thyroid function tests Urea and electrolytes Liver function tests Serum calcium Random/fasting blood glucose Syphilis serology Testing urine for infection and for proteinuria/haematuria If vascular dementia is a possibility, it may be worth checking lipids Given the possibility of a brain tumour mimicking dementia and of normal pressure hydrocephalus, and given that imaging may aid differentiation and so management, there is a strong argument for brain imaging in many patients with dementia. When the diagnosis is clear or when the patient is too frail for intervention, though, brain imaging is not necessary or appropriate. Currently GPs don’t have direct access to CT scanning, so referral to a specialist with an interest in dementia is necessary to get one. Assessing cognitive function If cognitive function seems impaired, and this doesn’t seem to be due to delirium, then a formal test of cognitive function may be used to supplement your assessment. The Mini Mental State Examination (see at end of this section) assesses a range of cognitive functions (but not frontal functions). Remember to make sure the patient can see and hear adequately to do these tests and that poor command of English isn’t going to impair their performance. Management Once the diagnosis of dementia is made, try to categorise the dementia and then adjust management appropriately. For example, if the patient has vascular dementia, consider addressing risk factors for vascular disease and starting a platelet inhibitor such as aspirin/clopidogrel. If the patient has Alzheimer’s disease, anticholinesterase inhibitors may be appropriate to slow disease progression. When a patient has dementia, their health - both mental and physical - deteriorates. Regular assessments, say about every six months, are useful. Wherever possible, a carer(s) should be involved in each assessment. The GP may consider the following issues at assessment. The patient’s choices: Although patients will become increasingly dependent, ideally they will take as much responsibility for themselves as possible for as long as possible - encourage carers to let them do as much for themselves as they can. Most patients have insight into their decline early in the disease. They may wish to make plans for their future at that time. The Mental Capacity Act (2005) allows the patient to nominate people to have a “lasting power of attorney”. There are two types of LPA: A property and affairs LPA gives the attorney(s) the power to make decisions about financial and property matters, such as selling a house or managing a bank account. Page 47 of 86 A personal welfare LPA gives the attorney(s) the power to make decisions about health and personal welfare, such as day-to-day care, medical treatment, or where the person should live. Patients may also wish to make an “Advance Directive” stating e.g. to what degree they want medical intervention should they become physically unwell later in the disease. “Medical” issues: Depression is common in people with dementia, affecting over half of people with vascular dementia, but symptoms may be difficult to differentiate from the dementia itself e.g. poor concentration, apathy. The GP should have a low threshold for diagnosing and treating depression. Movement difficulties can be associated with dementia, especially with Lewy body and with vascular dementia. Walking aids and adjustments in the home may help. When dementia is present, it is usually a feature of old age (although not a usual feature of old age!). With old age, physical health declines. The GP will be looking out for new diagnoses and ensuring that other physical diseases are appropriately managed. Dosette boxes can be used to help ensure drugs are taken properly; a carer may need to oversee this. Activities of daily living: Consider what assistance the patient needs. The GP might ask an occupational therapist to help with this. It may be that a carer, often a family member, will offer all the help necessary - providing meals and help with dressing and washing. Often Social Services will need to provide help at home, e.g. home help (for housework, preparing meals), home care (helping with self-care) and meals on wheels. Patients are frequently resistant to this to start with, but good home carers/helpers can form a valued relationship with the patient. Risks to the patient and others: Consider how the patient’s dementia may prove hazardous. For example, the patient may forget to light gas appliances when turned on - these could be exchanged for electric appliances. The patient may need to be advised not to drive. Falls are more common in people with dementia. Adjusting furniture and removing mats to minimise risk of falls is advisable. Carers are important!: Family and friends who look after people with dementia are a valuable resource. Without them many fewer people with dementia would be able to stay in their own homes. The burden of caring for an increasingly dependent adult is immense. This, coupled with the particular distress associated with witnessing a loved one’s decline through dementia, can be a huge drain on a carer’s resources of emotion, time and finance. It is of advantage to the person with dementia, the NHS and Social Services, and to carers themselves, that carers’ needs are considered and addressed. Carers need to look after themselves if they are to continue looking after the patient. They often need encouragement to do this. The more help there is, the longer carers are likely to be able to cope long-term. Where one of a number of potential carers seems to be doing most of the work, it is worth encouraging and helping that carer to get the others involved. Where possible, the burden on carers can be reduced by e.g. use of home care/help and by arranging that the patient goes to a day centre for the elderly. Respite care – the patient temporarily going into a “home” - may allow a valued break. Check that carers have a GP of their own and know where they can turn to for help (e.g. Age Concern, Alzheimer’s Society, Social Services and their GP). Page 48 of 86 Benefits: Ensure the patient and their carer(s) receive all the benefits they are entitled to, e.g. Attendance Allowance, Carer’s Allowance. Moving on: Many patients with dementia die in their own or their family’s home. For others there comes a time when living at home is no longer possible. This may be because they reach a degree of need that the carer(s) cannot meet, or because the carer(s) themselves may find they can no longer cope. Depending on the patient’s level of dependence and their wishes, this may necessitate a move to sheltered accommodation, to an elderly people’s home, a nursing home or to a home for the elderly mentally infirm. The patient will still have a GP who should continue to care for their physical and mental health. The needs of their carers will also still need to be considered. 1 Alzheimer’s society information, largely available at http://www.nia.nih.gov/alzheimers Page 49 of 86 Clinical features of dementia An individual's pathway through dementia is unique and influenced by their previous life experience. Some of these changes may not appear in the order listed. Some may not appear at all. EARLY STAGES Emotional changes Cognitive Changes Shallowness of mood Lack of emotional responsiveness and consideration for others Depression and/or anxiety Short-term memory deficit with particular difficulty in registration and recall of new information Thinking becomes concrete with a reduced range of concerns Perseveration of thoughts and action, accompanied by repetitive speech Behavioural Social withdrawal changes Emotional and physical disinhibition Difficulty in carrying out purposeful tasks: domestic tasks, dressing etc. Socially inappropriate behaviour, selfneglect Disorientation progressively for time, place and eventually for person Physical Usually in later stages changes Page 50 of 86 LATER STAGES Irritability and hostility Aggression Language disorder. Both receptive and expressive dysphasia can occur Thought process becomes fragmented, so that speech becomes disordered and fragmented Psychotic features occur in 30-40% Persecutory ideas and delusions Auditory and visual hallucination – not mood congruent Wandering and restlessness Evening and nocturnal restlessness prominent Turning night into day Aggression and violence Weight loss Self-neglect Malnutrition Incontinence Receptive and expressive dysphasia Bradykinesia Tremor Epileptiform seizures (usually late) Emergence of primitive reflexes Rigidity (usually late) Instability Visuospatial problems – less able to compensate for physical disabilities Immobility (‘off the legs’) chair Mini Mental State Examination pen (Adapted from Folstein MF, Folstein S, McHugh PR. (1975). Mini Mental State: a practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12(3): 189-98) Patient: Attention and concentration (max 5 points) For the next test I would like to ask you if you prefer to do subtraction or spelling. Date: If prefers subtraction (or expresses no preference): I would like you to take 7 away from a 100. Take 7 away from the number you get and keep subtracting 7 until I tell you to stop. (Record the numbers below and tick 1 point each time the difference is 7 even if a previous answer was wrong.) Answer each question as shown below and give each correct answer one point and add the results. Orientation to time (max 5 points) 93 What day of the week is it? 86 What is the date today? 79 Day 72 Month 65 Year If prefers spelling: Do you know how to spell the word WORLD? If says yes ask him to spell it. If it is correct ask: Can you now spell it backwards? (Record the reverse spelling below and tick 1 point for each correct answer and record number of points in the box.) What is the season? (Allow flexibility when the season changes e.g. when in May the correct answer can be spring or summer.) Orientation to Place (max 5 points) D-L-R-O-W Can you tell me where are we now? For example: what country are we in ? Memory (recall) (max 3 points) Can you remember the three objects 1 asked you to repeat a few minutes ago? Give 1 point for each item correctly remembered without prompting. what is the name of this town (or city) ? what are the two main streets nearby (or near your home)? what floor of the building are we on? Expressive Language (naming) (max 2 points) what is the name (or address) of this place? Memory (registration) (max 3 points) I am going to name three objects. After I have finished saying their names I want you to repeat them after me. I want you to remember them because I want you to name these objects in a few minutes. (Name the following objects, taking at least one second to say each clearly. Tick which items the patient correctly repeats on the first attempt.) Show pen or pencil What is this called? Show wristwatch What is this called? Expressive Language (repetition) (max 1 point) Listen carefully as I am about to say something which I would like you to repeat after me: No ifs, ands, or buts. (Say it clearly and slowly - only one attempt is allowed. Score 1 point if correct.) apple Page 51 of 86 Language (reading and comprehension) (max 1 point) Praxis (spontaneous writing) (max 1 point) Write a complete sentence on anything you want on this sheet. CLOSE YOUR EYES Can you read what this says? Can you do what it says? Praxis (ideational) (max 3 points) (Read the following statement and hand a piece of paper to the patient. Make sure the paper is handed to the patient's middle. Do not repeat the instructions or show how it should be done. Score 1 point for each correct move only if it is in the right sequence.) I am going to give you a piece of paper. When I give it to you, take the paper in your right hand. Fold the paper in half with both hands and put the paper down on your lap (or table). (Ask the patient what he has written. The sentence should have a verb and a subject. Phrases like 'Go away!' are not allowed.) takes paper with right hand folds it with both hands puts it on lap (or table) TOTAL (maximum score 30) Praxis (copying and drawing) (max 1 point) I want you to copy this design as best as you can. (Each pentagon should have 5 sides and 5 clear corners and the overlap should form a diamond.) Page 52 of 86 3.5 Psychosis Aims: To understand the principles of mental health teamwork and the integration of primary care and community mental health teams, using management of psychosis as an illustrative example. Learning Objectives: By the end of the sessions students should be able to: Outline the roles of different members of the primary care and community mental health teams and the interaction between them. Describe the workings of the CPA. Discuss the management of chronic psychotic illness in a primary care setting. Suggested Learning Methods: Introduction to the roles of the primary care and community mental health teams and pathways to care. (45 minutes) Interview with a patient with chronic psychosis in the community. (1 hour) Coffee Break (15-30 minutes) Presentation of case history with feedback and discussion of management issues. (45 minutes) Background Reading: Osborn DPJ, King MB, Nazareth I. (2003). Participation in screening for cardiovascular risk by people with schizophrenia or similar mental illnesses: cross sectional study in general practice. British Medical Journal, 326:1122-3. http://www.rcpsych.ac.uk/about/campaigns/changingmindscampaign1997-.aspx http://www.nice.org.uk/guidance/CG82 up to date NICE guidance Page 53 of 86 THE ROLE OF PRIMARY CARE IN THE MANAGEMENT OF PEOPLE WITH SEVERE MENTAL ILLNESS Psychosis affects 3% of the UK population including schizophrenia, bipolar disorder and chronic psychosis, a similar number to those with insulin dependent diabetes1. 30% of people with schizophrenia are only seen in Primary Care for reasons including patient choice and symptom resolution2. Patients with severe mental illness have been found to consult more often than the general population3. Conversely, many people with schizophrenia are unfortunately not registered with a GP making monitoring of their physical and mental health more difficult. Primary Care practitioners are uniquely placed throughout the lifetime of a patient with severe mental illness. They may be involved at diagnosis; they are particularly likely to pick up early signs of psychosis as they know the patient and concerned family members may present to them initially. The GP also has an ongoing role in providing mental and physical health care for the patient and if appropriate, their family. They should be the cornerstone of care but is this, the case in reality? The new NICE guidelines emphasize the key role of primary care, particularly in the monitoring of patient’s physical health. A yearly mental health review for those with severe mental illness is part of QOF (quality outcomes framework) and as part of this there is emphasis on cardiovascular disease risk assessment bearing in mind that that people with schizophrenia are at higher risk of cardiovascular disease than the general population. Sharing of this information with secondary care is encouraged. Continuity of care is an important part of the primary care role, but this can be a challenge when people move about in inner cities because they need to change their GP. Epidemiology of psychosis Kraepelin described “dementia precox” literally “dementia of the young mind” in 1896. Bleuler (1977) observed some recovery in such patients with schizophrenia and further studies have shown around half have a favourable outcome4,5. Schizophrenia is more common in men, and increased in black and minority ethnic groups. Studies have shown a link to socioeconomic deprivation and also cannabis use6,7. It mostly presents before the age of 35 and as described, environmental and genetic factors play a role in its development. Early Intervention GPs will see an average of 1-2 people with a new diagnosis of psychosis a year. There is evidence that if there is active primary care involvement with the patient, the need for use of the MHA is reduced8. The critical period is that prior to diagnosis. On average it takes 1-2 years for a diagnosis of schizophrenia to be made and there are better outcomes if the diagnosis is made early9. The GP is well placed to pick up early signs and family concern. What are the symptoms and signs of schizophrenia? There are many, including: mood change, poor sleep, anxiety, poor hygiene, social withdrawal, outbursts, bewilderment…. Active watching of a person in whom concerns have been raised is crucial. Hallucinations and delusions may need to be actively sought by asking questions such as: Page 54 of 86 Have you ever felt that something odd might be going on that you cannot explain? Have you been feeling that people are talking to you, watching you or giving you a hard time for no reason? Have you been feeling, seeing or hearing things that others cannot? Have you felt especially important in some way, or that you have powers that let you do things that others cannot? Asking about problems with social functioning, cognition and mood is also important as well as asking about drug use. Where there are acute symptoms of schizophrenia, urgent referral to psychiatric services in key and this is emphasized in the new NICE guidelines. If it is necessary for the GP to start antipsychotics they should have experience in treating and managing schizophrenia; no particular antipsychotic is recommended but choice should be tailored to the patient. Early Intervention Services have been set up country-wide and are endorsed by the WHO; evidence shows these lead to improved clinical outcome10 and relapsed rates11. However in the UK such services are only available to around one third of the population. The new NICE guidelines also recommend referral to patients for CBT and family intervention for their close relatives. Monitoring of Mental Health As mentioned previously, many patients with chronic stable schizophrenia will not be under secondary care. They are managed in primary care and will be on regular antipsychotics; if this is via depot it may be given by the practice nurses or GPs. The GP is well placed to monitor the health of the patient, drug concordance and side effects. They are likely to also know the family well and so be able to communicate with them if appropriate. There is evidence patients with psychosis appreciate continuity of care and want someone to listen to them12. A GP who knows the patient, listens, approaches patients with therapeutic optimism and seeks advice from secondary care as needed would be seen by the majority of patients as providing “good enough” care. A recent study by Osborn et al (2008) showed that people with severe mental illness contact their GP more than those without and this contact may increase in the week before suicide13. If there is deterioration in the mental health of the patient and they are refusing to go to hospital the GP may be involved in putting them on a Section 3. (Question: who else would be needed to do this?) However, if signs of a relapse are picked up early this may not be needed. Page 55 of 86 Monitoring of Physical health in the Community Patients with severe mental illness live 10 years less than those without, often due to physical health problems14. Worryingly this health gap has worsened over last few decades15. People with severe mental illness are particularly at risk of cardiovascular disease. This is for three main reasons: 1. Antipsychotic side effects. The second-generation antipsychotics cause weight gain, glucose dysregulation and maybe dyslipidaemia. 2. Patients are prone to unhealthy lifestyle e.g. smoking, little exercise, poor diet. 3. There is evidence that irrespective of the above, people with severe mental illness have a genetic tendency to having higher cardiovascular risk. A recent systematic review by Osborn et al (2008) showed an almost two fold increase in diabetes in patients with schizophrenia16. Patients on the severe mental illness register should have yearly checks (part of QOF) involving checking BP, weight, smoking status, glucose and cholesterol levels, lithium levels if the patient is on lithium, and appropriate intervention e.g. starting statins taken. Unfortunately UK studies show patients with schizophrenia are more likely to encounter reluctance from GPs to participate in their physical health care than those without mental illness but hopefully with increased awareness this can be altered in the future17. There is good evidence that people with severe mental illness are interested in their physical health care so it important to capitalize on this18. Page 56 of 86 THE HISTORY OF COMMUNITY CARE The Asylums Many Psychiatric Hospitals (also known as mental health asylums) were set up in the 19th century. As the number of people living in cities increased, there became an increasingly large population of mentally ill people. In rural areas the mentally ill had been able to rely on local support or managed to simply go unnoticed amongst the rest of the population. However, in larger cities they faced a higher degree of difficulty and had a much greater chance of causing disruption or simply being a nuisance. This led to the building of the early asylums. Initially these early asylums were essentially prisons for the mentally ill, keeping them away from mainstream society. Conditions were often extremely poor and serious treatment was not yet an option. These Victorian asylums were often used inappropriately, for example to house single mothers, and once in them patients often remained there for their whole lives. Scene of Bethlem Hospital from the final plate of William Hogarth's A Rake's Progress (http://en.wikipedia.org/wiki/Image:The_Rake%27s_Progress_8.jpg) Bethlem Royal Hospital (Bedlam) which was the first recorded Psychiatric Hospital in Europe, admitting some mentally ill patients from 1357, became infamous for its treatment. In the 18th century outsiders would pay a penny to come and watch their patients as a form of entertainment. The view of the time was that madness was a result of moral weakness, leading to "moral insanity" being used as a common diagnosis. Inmates were referred to as “unfortunates”. Conditions in asylums slowly improved thanks to pioneers such as William Ellis, a Methodist, who along with his wife introduced humane treatment and “moral therapy” combined with “therapeutic employment”. His methods were taken up in other asylums and in recognition of all this work he received a knighthood. Attitudes towards the treatment of the mentally ill began to drastically improve during the mid-19th century. Page 57 of 86 The Introduction of Community Care The shift towards Community Care began in the 1950s in the post-war setting: the welfare state and NHS were set up and phenothiazine drugs were also introduced around this time. Psychiatrists were keen to improve the quality of life of their hospital patients and enable those capable to do so to live independently. It was suggested that new drugs would mean patients did not need to be long-term inpatients and it was postulated that the negative symptoms seen in Schizophrenia were due to the asylum setting. Politically there was also drive for change as asylums were expensive to run. Although obviously an improvement from old style mental asylums, public concern about lack of care for patients in the community surfaced in the 1980s. Their concern was that mentally ill patients were ending up on the streets, in prisons and with unsupported relatives and there were frequent readmissions. In 1989 there was a white paper, “Caring for People: Community Care in the next decade and beyond”, and legislation in the “NHS and Community Care Act” 1990. These gave responsibility for the social care of people with mental health problems to local authorities, encouraged to purchase services from voluntary and private providers. There remains a problem with funding however, with many mental health patients still waiting in hospital for suitable accommodation to be found. Another problem is that the medical and social needs of patients are met by two different agencies (NHS and Department of Social Security). Point for discussion: What is community care? Is it a useful term? (It appears to suggest a clear distinction between the hospital and community care which is perhaps not the case. Also, it suggests there is no sense of community in a Psychiatric hospital; also not always true. The House of Commons Social Services Committee report on community care (1985) noted, “The phrase ‘community care’ means little in itself. It has in fact come to have such general reference as to be virtually meaningless”. Do you agree?) The Care Programme Approach (CPA) The Care Programme Approach was introduced in England in 1991, reflecting the fact that case management is the main model of community care provided. It requires Health Authorities, in collaboration with Social Services Departments, to put in place specified arrangements for the care and treatment of mentally ill people in the community. The majority of these people suffer from schizophrenia. The Care Programme Approach has four main elements as defined in “Building Bridges: A guide to arrangements for inter–agency working for the care and protection of severely mentally ill people” (DoH, 1995). The aim is to provide support for patients and minimize the risk of relapse. 1. Assessment Systematic arrangements for assessing the health and social needs of people accepted by the specialist mental health services. 2. A Care Plan The formation of a care plan which addresses the identified health and social care needs. 3. A Key Worker The appointment of a Key Worker (now Care Coordinator) to keep in close touch with the patient and monitor care. Page 58 of 86 4. Regular Review Regular review, and if need be, agreed changes to the care plan. Patients are required to have a crisis plan and contingency plan. Recent Changes There have been very recent changes with the introduction of the Mental Health Act 2007, amending the Mental Health Act 1983. Perhaps the most important of the changes is the introduction of Supervised Community Treatment through the making of a Community Treatment Order. This aims to reduce a patient’s stay in hospital whilst ensuring that their treatment is continued in the community. For more information about this please see http://www.nhs.uk/nhsengland/aboutnhsservices/mental-health-servicesexplained/pages/thementalhealthact.aspx Also key is the fact that the emphasis is on recovery, social inclusion, work and education, in contrast to previously when people have been “written off” as being mentally ill and unable to work. An example of this is the government’s “Pathways to work” scheme for people receiving incapacity benefits. The Community Mental Health Team This is the team responsible for the Psychiatric care of a certain population. It can include: Team Manager Psychiatrist Community Psychiatric Nurses Psychologist Social Workers Occupational Therapists Housing Workers They usually meet weekly to discuss referrals. If a referral is accepted, the patient will be assessed, usually by two members of the team, and a plan of care agreed at subsequent meetings. In some areas a START team is responsible for initial assessment and management of referrals. Which CMHT a person is allocated to is decided by GP and postcode (if a person is homeless it is decided on the basis of surname). Duty Team This is a team which can be contacted during normal working hours if there is concern about a patient. It is mostly used if there is a concern about a patient already known to the CMHT and then an appropriate assessment of the patient can be made if needed. The Crisis Team This is a team set up to try to reduce hospital admissions. Crisis teams are across the country now and gate-keep all admissions as well as providing early discharge. This is for cost reasons as well as because people don't like inpatient care. Page 59 of 86 If a GP for example sees a patient they think may need admission, they typically refer to the crisis team. Two members of the team then assess the patient (24 hours a day in some areas). They may feel they can work with the patient at home e.g. by providing close monitoring and supervising medication. However, if they feel they cannot work with the patient, they may need to be admitted to hospital. Other teams In some areas there are other specialist teams and these are becoming increasingly widespread. For example an early intervention team which deals with young people newly diagnosed with a psychotic illness. They will work closely with the person and this often avoids the need for hospital admission. There are also assertive outreach teams for those who are severely ill or have frequent admissions. Provision of Appropriate Housing Some patients live with their families (who may also need support) and some live independently in rented accommodation. However, other need more help. This can be provided in group homes where four or five patients live together in a house which is often owned by voluntary organization charities. They receive support and supervision, usually from a community nurse. Group homes are sadly disappearing or tending to move people out after a couple of years with a drive towards more independent living. Staffed hostels describe hostels where members of staff are present throughout the day and usually at night. Sheltered housing is a form of accommodation where individuals can live in independent units while enjoying the benefits of communal facilities and the services of a scheme manager or resident warden. Some schemes are operated by a local authority or housing association for rental to suitable tenants; others are created for private owner-occupiers or are a mix of both types of resident. These schemes are increasingly important for people with learning disabilities or mental health problems. Rehabilitation Patients being discharged from a Psychiatric Ward often need rehabilitation rather than simply rehousing. Rehabilitation is the process by which mental health impairment is minimized, so the person is able to successfully reintegrate into the relevant community, gaining confidence through success in social roles. Principles include tailoring the program to the individual, thorough initial assessment including self-care, social relationships, work and leisure, medication and individual goals. A MDT approach is crucial. Rehabilitation can be provided in a variety of settings: Day hospitals (run by the NHS) and day centres (typically voluntary), social clubs, supported accommodation. SUMMARY The GP is ideally placed to pick up on early signs of mental illness and to continue care by picking up signs of relapse, checking on medication concordance and side effects, supporting the patient and their family and monitoring physical health. It is obviously important for the patient with chronic psychotic illness that there is good communication and shared care between primary and secondary care services. Page 60 of 86 1 Bird L. (1999). The fundamental facts about mental illness. London: Mental Health Foundation. Kendrick T, Burns T, Freeling P et al. (1994). Provision of long term care to general practice patients with disabling long-term mental illness: a survey in 16 practices. British Journal of General Practice, 44:301-5. 3 Nazareth I, King M & Haimes, A. (1993). Care of schizophrenia in general practice. British Medical Journal, 307:910. 4 Bleuler, M. (1977). The Schizophrenic Disorders. Translated by Siegfried M. Clemens. New Haven and London: Yale University Press. 5 Harrison G, Hopper K, Craig T et al. (2001). Recovery from psychotic illness: a 15 and 25 year international follow-up study. British Journal of Psychiatry, 178:506-17. 6 Kirkbride JB, Fearon P, Morgan C et al. (2006). Heterogeneity in incidence rates of schizophrenia and other psychotic symptoms: findings from the 3-center AeSOP study. Archives of General Psychiatry, 63:250-8. 7 Moore T, Zammit S, Lingford-Hughes A et al. (2007). Cannabis use and risk of psychosis or affective mental health outcomes: a systematic review. The Lancet, 370: 319-28. 8 Burnett R, Mallett R Bhugra G et al. (1999). The first contact of patients with schizophrenia with psychiatric services: social factors and pathways to care in multi-ethnic populations. Psychological Medicine, 29:475-83. 9 Birchwood M, Todd P, Jackson C. (1998). Early Intervention in psychosis, the critical period hypothesis. British Journal of Psychiatry, 172:Suppl.33, 53-9. 10 Peterson L, Jeppeson P, Thorup A et al. (2005). A randomised multi-centre trial of integrated versus standard treatment for patients with a first episode of psychotic illness. British Medical Journal, 331:602-6. 11 Craig T, Garety P, Power P et al. (2004). The Lambeth Early Onset Team; randomized controlled trial of the effectiveness of specialized care for early psychosis. British Medical Journal, 329:1067-71. 12 Osborn DPJ, King MB, Nazareth I. (2003). Participation in cardiovascular risk screening by people with schizophrenia or similar mental illnesses: A cross sectional study in general practice. British Medical Journal, 326:1122-3. 13 Lawrie SM, Martin K, McNeill G et al. (1998). General Practitioner’s attitudes to psychiatric and medical illness. Psychological Medicine, 28:1463-7. 14Osborn DP, Wright CA, Levy G, King MB, Deo R & Nazareth I. (2008). Relative risk of diabetes, dyslipidaemia, hypertension and the metabolic syndrome in people with severe mental illnesses: systematic review and metaanalysis. BMC Psychiatry, 8:84. 15 Saha S, Chant D & McGrath J. (2007). A systematic review of mortality in schizophrenia. Archives of General Psychiatry, 64:1123-31. 16 Alleback P. (1989). Schizophrenia: a life-shortening disease. Psychiatry Bulletin, 15(1):81-9. 17 Lester HE, Tritter JQ & Sorohan H. (2005). Providing primary care for people with serious mental illness: a focus study group. British Medical Journal, 330:1122-8. 18 Osborn DPJ, Levy G, Nazareth I & King M. (2008). Suicide and severe mental illnesses: cohort study within the UK general practice research database. Schizophrenia Research, 99(1-3):134-8. 2 Page 61 of 86 3.6 Eating Disorders Aims: To introduce the students to eating disorders in the community; their prevalence, ways in which they may present and potential difficulties in detection. To consider the treatment options and the potential impact on the family. Learning objectives: By the end of the session the student should be able to: Outline the epidemiology and aetiology of eating disorders in the community, their definitions and ways in which they may present including their non-psychiatric presentations. Describe the role of the primary care team in the detection and management of patients with these conditions, and understand the indications for referral for specialist care. Discuss the difficulties in detection and the reasons for this, particularly associated stigma and secretiveness. Describe some of the potential physical complications and the range of treatment options in primary and secondary care. Discuss the potential impact of the condition on the individual and their family. Suggested Learning Methods: Small group seminar – discussion of background reading including prevalence in primary care, presentations and difficulties in detection/stigma. (45 minutes) Interview with a patient who has an eating disorder (or use of video training materials). This can be broadly interpreted as any problem associated with eating habits and body self-image, including over-eating and associated obesity, binge-eating and restricted food intake even if the criteria for a diagnosis of anorexia or bulimia nervosa are not met If suitable patients not available, consider using a training video (see teaching resources) or role playing scenarios (consider using http://www.trickcyclists.co.uk/ website as resource) (1 hour) Coffee Break (15-30 minutes) Small group – presentation of cases, discussion of management, impact on the family and any other issues raised. (1 hour) Background Reading: Wilhelm KA & Clarke SD. (1998). Eating disorders from a Primary Care Perspective. MJA Practice Essentials, 168: 458-63. The Royal College of Psychiatrists’ leaflet on eating disorders, available at: http://www.rcpsych.ac.uk/healthadvice/problemsdisorders/eatingdisorderskeyfacts.aspx Page 62 of 86 The size of the problem Eating disorders are a big problem. In adolescent girls, eating disorders are the third most common disorder after obesity and asthma. In Western cultures 0.5% of young women have a history of anorexia nervosa and 2% have a history of bulimia nervosa. Although more common in females, there is an increasing prevalence in men, which often goes undetected1. An eating disorder is a distress call. It can be a reflection of personal dissatisfaction and interpersonal difficulties; a way of exerting control in people who have little control in other areas of their life, or a way of trying to “disappear”. Undoubtedly the emphasis on promoting slimness as beautiful and the unrealistic media portrayal of thin models is also fuelling illness. 90% of patients with an eating disorder present to their GP with complaints secondary to their eating disorder (e.g. sensitivity to cold, low mood), but the eating disorder itself may not be diagnosed2. Only 40% of cases of AN, and 10% of BN are detected in primary care. What is an eating Disorder? There are several different eating disorders and their classification is described below. Essentially they are a disturbance of eating habits or weight control behaviour resulting in significant impairment of physical health or psychosocial functioning. This should not be secondary to a medical condition or other psychiatric disorder. Anorexia Nervosa (AN) Weight loss (or failure to gain weight whilst growing) leading to body weight <85% expected (WHO ICD-10 definition BMI 17.5 or less). Body image disturbance (fear of becoming fat, denial of seriousness of low body weight, viewing self as overweight despite low objective measures). Amenorrhoea in postmenarchal females (absence of three consecutive cycles). Bulimia Nervosa (BN) Recurrent episodes of binge eating (lack of control over eating, eating more food than most people would eat over a set period of time and under similar circumstances) at least twice a week for three months. Inappropriate compensatory mechanisms (e.g. self-induced vomiting, misuse of laxatives, diuretics, excessive exercise). Body image disturbance (e.g. self-evaluation unduly influenced by body shape and weight). Most eating disorders do not satisfy the criteria for these two syndromes and other disorders are recognized: Binge Eating Disorder Overeating episodes No or minimal compensation mechanisms Often overweight “Purging Disorder” Purging behaviours, no overeating Atypical AN or BN (“Eating Disorder-NOS/EDNOS”) Fails to meet one of the criteria for AN or BN Page 63 of 86 Aetiology Many potential aetiological factors in the development of eating disorders have been described: Genetics – twin studies have shown a likely genetic predisposition to developing an eating disorder. Early experiences including peer relationships and life events. Occupational – certain occupations have an increased risk of developing an eating disorder e.g. ballet dancers. Media pressure has been implicated (Three years after the introduction of TV to Fiji rates of vomiting to control weight went from 0 to11% in young women3). (Optional activity perhaps for seminar at end of session – get students to spend some time looking at how body image is presented in magazines – discuss whether they consider media image is an aetiological factor in EDs.) Discussion point Are eating disorders illnesses of developed countries? Food is available and marketed as a source of fun and comfort, lifestyles are increasingly sedentary, dieting is heavily promoted… Risk Factors for developing an eating disorder Certain features may make someone more likely to develop problems with eating, and screening of high risk groups could be considered: Females are more likely to develop problems than males, particularly in adolescence People with a family history of psychiatric disorder, especially eating or affective disorders Premorbid obesity Perfectionist and obsessional personality Dysfunctional family and social systems Upper social class bias in anorexia nervosa Precipitating factors Various events may precipitate the development of an eating disorder, for example: comments about body shape, fall in self esteem, leaving home, onset of puberty, the start of a relationship, loss. Prevalence of eating disorders1 All eating disorders (including EDNOS): 5% (Up to 5% of females, 0.5% of males) Anorexia Nervosa: Females 0.3-0.7%, Males 0.1% Over 20 years 50% make a good recovery, 30% have a fair outcome, 20% a poor outcome Mortality is up to 20% (causes including suicide, cardiac arrhythmias, infection). Suicide rates are 60 times that of the general population (higher than for any other Psychiatric disorder)4. Bulimia Nervosa: Females 0.5-1%, Males 0.1% Binge Eating: Normal weight 1-3%, Obese 8.5% This means that a GP with 2000 patients will on average be looking after 3 patients with AN, 11 with BN and 15 with EDNOS1. Diagnosis A. History People often present inconspicuously – they may present to their GP with weight loss, amenorrhoea, delayed puberty, irritability, depression, subfertility, food allergy/IBS Page 64 of 86 symptoms among others. It may be parent/relative/friend/teacher who seeks advice (what are the ways of managing this?). NICE recommends screening in high risk groups by using two screening questions (Do you think you have an eating disorder? Do you worry excessively about your weight?) or the SCOFF questionnaire5. The ESP questionnaire can also be useful for screening6. SCOFF questionnaire Do you make yourself Sick because you feel uncomfortably full? Do you worry you have lost Control over how much you eat? Have you recently lost more than One stone in a 3 month period? Do you believe yourself to be Fat when others say you are too thin? Would you say that Food dominates your life? One point for every yes, >or equal to 2 = likely AN or BN Eating Disorder Screen for Primary Care (ESP) Are you satisfied with your eating patterns? (A “no” to this question was classified as an abnormal response). Do you ever eat in secret? (A “yes” to this and all other questions was classified as an abnormal response). Does your weight affect the way you feel about yourself? Have any members of your family suffered with an eating disorder? Do you currently suffer with or have you ever suffered in the past with an eating disorder? One point for every yes, >or equal to 2 = likely AN or BN It is important to get an idea of eating patterns and weight control strategies, to elicit psychological pathology (e.g. triggers, low mood) and physical symptoms. Useful questions to ask a person who you think has an eating disorder: Eating behaviour What do you eat on a typical day/last 24 hours? Do you avoid eating with others? Do you avoid certain foods? Do you try to suppress your appetite? Do you vomit after eating? Do you use laxatives? What exercise do you do? Do you binge eat? How often? Psychopathology What do you think of your weight? What weight would you like to be? How much of the day do you spend thinking about food and your weight? What and when was your heaviest weight? Page 65 of 86 Why is it important to you to lose weight? How is your mood? Do you ever feel suicidal? Drug use/alcohol? Physical When was your last period? Have you noticed any muscle weakness? Are you sensitive to the cold? Have you fainted or had dizzy episodes? B. Examination There may be no signs that a person has an eating disorder. Signs may be present however. The most important sign in anorexia is a low BMI. Lanugo hair may also be seen, hypotension, bradycardia, poor peripheral circulation and loss of body fat. One good test to carry out identifies low muscle power: the SUSS test. This involves asking the patient to rise from squatting and sit up from lying flat, scoring 0 if the person is unable to, 1 if they can using their hands, 2 if it is with difficulty and 3 if they are able to do so without difficulty. Signs of repeated vomiting may include dental erosion, parotid enlargement and Russell’s Sign (calluses over MCP joints of dominant hand) C. Investigations No investigations may be indicated. However, if a diagnosis of anorexia nervosa is made then blood tests should be undertaken including: FBC, U and E (hypokalaemia a complication), calcium, magnesium and phosphate, LFTs, glucose, CK. An ECG is likely to be useful, particularly if there is low potassium. A bone density scan is indicated if the patient has been amenorrheic for more than 6 months, and a pelvic US and day 21 progesterone to detect ovulation may also be useful. A urinary drug screen for laxative abuse may sometimes be helpful. Management of eating disorders in Primary Care Various management strategies can be employed in Primary Care encompassing physical, psychological and social problems and assessing risk. Obviously forming a good therapeutic alliance with the patient and their family is very important as well as monitoring risk and aiming for nutritional health. Brief interventions such as a discussion of the concepts of normal regular eating and diet/exercise advice may be helpful. Some people find keeping a food diary beneficial. In patients who have low BMIs a usual goal is to achieve a weight gain of around 0.5kg a week, requiring on average an intake of 2500kcal a day. It also may be useful to reflect on food related communication, for example exploring the idea that it may be safer to make negative comments about one’s body than express difficult emotions or real feelings. Practice nurses, counsellors and dieticians may also help provide support. The use of guided self-help is recommended by NICE (www.nice.org.uk) as first line treatment in bulimia nervosa. This involves the patient using self-help resources with regular review either by the GP, practice nurse or counsellor. Resources include: Schmidt U & Treasure J. (1993). Getting better bit(e) by bit(e). Psychology Press. Fairburn CG. (1995). Overcoming Binge Eating. New York: Guilford Press. Palmer R.L. (1989). Anorexia Nervosa: A guide for sufferers and their families. Penguin Books. B-EAT Eating Disorders Association www.b-eat.co.uk Overeaters Anonymous Page 66 of 86 Guidance may be given by helping the patient set realistic goals and plan for relapses, as well as providing general support and a point of contact. When to refer? When to refer to secondary care services is obviously a clinical judgement in each case though there should be a lower threshold for intervention in adolescents than adults7. If someone has a diagnosis of anorexia nervosa they are likely to need referral. Other reasons for referral may include: if the clinical picture is uncertain or abnormal eating behaviours are entrenched or out of control. Also if guided self-help is failing, there is concurrent psychiatric disturbance or severe family dysfunction. Studies show 80% of people with AN and 60% with BN are referred. Primary Care Guidelines for AN Mild AN (BMI >17, no comorbidity) – support, information, monitoring (?weekly), consider food plan, dietician, therapist Monitor for 8 weeks – refer if no response Moderate AN (15-17 BMI, no evidence system failure) – routine referral to eating disorder unit Severe AN (BMI < 15, rapid weight loss, system failure) – urgent referral, consider medical unit if life threatening Primary Care Guidelines for BN Mild – moderate BN (less than daily purging, no co-morbidity) – support and monitoring, information, explore problem. Monitor for 8 weeks, consider referral if no response Severe (daily purging with electrolyte imbalance, co-morbidity) – Urgent referral to ED specialist Even if a patient is referred to secondary care, it is likely they and their families will continue to need support in primary care. NICE priorities (NICE, 2004) The NICE guidelines emphasize the importance of communication and involving family members if consent is given. They note that for AN most treatment is as an outpatient with physical risk management and psychotherapy. Family therapy is particularly prioritized especially for younger patients, though there is some evidence for supportive individual therapy and a trial is currently looking at evidence for CBT. Day hospitals may sometimes be beneficial providing increased psychosocial support and monitoring, and can provide other therapies such as art therapy. Sometimes hospital admission is needed, usually if there is a rapid reduction in BMI, decompensation (e.g. organ failure, raised CK), severe hypokalaemia, lack of response to treatment or suicidality. Treatment can include refeeding, physical monitoring and psychosocial interventions. Where is this care best provided? Obviously it partly depends on the presentation of the patient, but often the patient is either admitted to an acute medical Page 67 of 86 ward (if medical problems e.g. hypokalaemia are the main concern) or a psychiatric ward (if psychiatric problems e.g. suicide risk are the main concern). As long as the patient’s physical condition is not too compromised, an inpatient specialist eating disorders service may be the most effective option. Sometimes a patient will need to be admitted under Section, typically section 3 for treatment. NICE reiterates that evidence based self-help is first line treatment in BN (including email/computer guided self-help if available), or alternatively a trial of an antidepressant (e.g. fluoxetine), although the long term outcome with antidepressants has not been established. There is good evidence for CBT (how would you describe what this involves to a patient?), with 16-20 sessions over 4-5 months, and Interpersonal Therapy (ITP). The latter concentrates on the patient’s relationships with other people, helping to rebuild supportive relationships. CBT is also recommended for binge eating disorder. For other eating disorders (EDNOS) it is recommended that the guidance for the eating disorder most resembling the patient’s symptoms is followed. Conclusion Primary Care plays a very important role in the diagnosis and management of people with eating disorders. Screening of high risk groups is advised, and it is important to try and diagnose patients presenting inconspicuously with related physical complaints. A therapeutic relationship with the patient and their family is then vital in establishing healthy eating patterns, while also addressing underlying psychological issues. Guidelines can be used to aid referral when needed, although the GP is likely to continue to be involved in patient care even if the patient is referred. 1 Golden NH et al. (2003). Eating disorders in adolescents position paper of the society of adolescent Medicine. Journal of Adolescent Health, 33:496-503. 2 Cotton MA, Ball C & Robinson P. (2003). Four simple questions can help screen for eating disorders. Journal of General Internal Medicine, 18(1):53-6. 3 Morgan JF. (1999). The SCOFF questionnaire: assessment of a new screening tool for eating disorders. British Medical Journal, 319:1467-8 4 Herzog W et al. (2000). Mortality in Eating Disorders: a descriptive study. International Journal of Eating Disorders, 28:20-6. 5 Becker AE, Burwell RA, Gilman SE, Herzog DB & Hamburg P. (2002). Eating behaviours and attitudes following prolonged television exposure among ethnic Fijian adolescent girls. The British Journal of Psychiatry, 180:509-14. 6 Noordenbos G. (1998). Eating disorders in Primary Care: early identification and intervention by general practitioners. In W Vandereycken & G Noordenboos (Eds): The prevention of eating disorders, pp 214-29. London: Athlone Press. 7 Hoek HW. (1993). Review of the epidemiological studies of eating disorders. International Review of Psychiatry, 5(1):61-74. Page 68 of 86 4 Useful teaching skills The aim of this section is to describe some basic teaching techniques that will be useful for all teaching situations. Many of you will already be teaching using the skills described in this section without necessarily being conscious of doing so. This section should help clarify these basic teaching skills and, by making you aware of your current practice, increase your effectiveness as a teacher. 4.1 Questioning techniques Teachers Questions A teacher’s questioning can be used to reveal factual knowledge, to encourage a student to display understanding or to stimulate a student to formulate her/his own theories about a particular topic. Questions can be helpful in monitoring how your session is proceeding and in checking that you have achieved your lesson objectives. They can be used in assessing students and in evaluating your teaching. The way you ask questions contributes to your teaching style and the educational climate you engender. Bloom was an educationalist who formulated a hierarchy of questions in 1956. His approach to questions is still useful and valid for today’s teachers. We have simplified his original 6 stage model into 3 levels: In reality 80-90% of teachers’ questions require factual answers, thus testing recall but not necessarily understanding of the topic. Questions that require students to apply their knowledge regarding an individual patient or to solve a clinical problem will promote this deeper understanding. Another common mistake is that teachers do not allow enough time for students to consider an answer: in general you should allow at least 3 seconds for them to answer – the more complex or deep a question, the longer a student needs to construct an answer. Teachers frequently answer their own questions or leave questions unanswered. Repeating an unanswered question will not produce an answer if the students do not understand the question. You can try rephrasing the question or replacing it with a simpler question on the same topic. Also, beware of posing questions with more than one part. Students’ Questions The ratio of teachers’ questions to students’ questions is said to be 100:1. If you wish to encourage students to be relaxed enough to ask you questions, you should attend to the whole atmosphere of the lesson and offer them explicit encouragement. You must also allow enough time for questions and answers. Students can get very adept at distracting teachers from the main topic of a lesson, leading their teachers down interesting but not necessarily relevant pathways. Your lesson plan should be useful in these circumstances by focusing on the main objectives for the lesson and in reminding you of time constraints. Page 69 of 86 4.2 Getting and maintaining interest Getting Interest When planning your lesson you should consider how to get your students’ interest and attention by motivating them i.e. giving them good reasons why they should pay attention. It is a sad but true fact that the most effective motivating force for students is the assessment for each course or year. We have detailed the assessment methods we use for psychiatry in Section 5. Don’t forget that students will also encounter psychiatric problems in their finals exams, both in the current long/short case clinicals and in the OSCE exam. If you discuss your aims and objectives with the students at the start of a learning session and are prepared to negotiate changes to suit the students, then they will feel more involved with the lesson and more interested. Of course you will need to set the limit to changes that are appropriate to the course or session. Moving from the specific to the general may catch students’ interest: consider relating a personal experience with patients, then using the incident to broaden out into the underlying general principles. Maintaining interest Some teachers have no trouble in keeping students’ attention but most will need to use a few tips from the following list. Active learning Involve the students in the sessions by making them think about the subject. Vary the teaching method at least every 15 minutes - this may simply mean stopping a prepared talk and asking for questions. Use quizzes, or discussion between students in pairs. Ask students to summarise, construct theories and present results of their discussions. Use questioning skills to probe knowledge and get students to think actively. Presentation Skills Try to vary the pitch and pace of your speech and the projection of your voice. Students respond positively to enthusiasm in a teacher so, if you are enthusiastic about your subject, share your feeling with your students. Distributing questions evenly between students will keep them alert in case they are asked to contribute. Don’t engage in prolonged exclusive discussion with one member of the audience as others will feel excluded. Use eye contact to involve all students. Look around the group as you talk remembering that if you are sitting in a circle the students closest to you on either side are the easiest to ignore. Use “signposting” to signal that you are about to start a new section of the session. This will enable students to be mentally prepared for the next topic. Monitor student responses Be aware of students’ interest by noting their body language and move to the next part of the lesson plan if they are bored. Page 70 of 86 4.3 Facilitating feedback The aim of feedback is to improve a students’ performance. If a student is upset by the manner in which feedback is offered then s/he will not be in a psychological state to benefit from it. There are some general principles for giving feedback which have been listed in the box below. General principles for facilitating feedback Address the behaviour and not the person: there is no point criticising things that cannot be changed. Constructive rather than destructive: criticisms should be constructive and phrased as areas for improvement or targets they can work on for next time Consider the positive before the negative: it has been shown that feedback is more effective if the student leaves feeling generally good but with some specific ideas for improvement. Therefore it is important to focus on positives as well as negatives. One approach is the ‘criticism sandwich’ where you start with comments on what went well, followed by some areas for improvement and end with some overall positive comments. Specific rather than general: it is especially valuable to give students specific examples of where they did particularly well or could improve, rather than general comments. Allow the student to start first: most of the time students will know where they went wrong but will struggle to find parts where they did well. It makes your job a lot easier, and more comfortable for the students, if you allow them to give their own feedback on their performance first. Consider the timing: generally the sooner the feedback is given the better. 4.4 Role Play You might choose to use role play in one of the sessions. This is useful when preparing students for communication that can be difficult, for example when asking about problems with alcohol or substance use. It has an advantage in quiet groups of students in that it tends to bring the students out of themselves. To make role play work well, it’s helpful to remember a few tips: 1. The students should feel safe – it may be necessary to set ground rules about how they treat each other and about confidentiality. 2. Set the scene: discuss the nature of the session and the learning objectives. 3. Have a scenario prepared and make sure the students know what their roles are. The observers should know what they’re looking out for e.g. things that worked well, verbal/non-verbal communication. 4. Debriefing: Ensure the students have stepped out of role, especially if the role play was emotionally charged. Allow enough time for reflection and feedback on what each of the students has experienced. Page 71 of 86 5 Assessment, evaluation & support 5.1 Student examinations and final grades Assessment in Year 5 comprises in-course assessments in the form of portfolio requirements, module assessments, and a summative examination at the end of the year. For 2015-16 this will cover the following subject headings: Child and Family Health with Dermatology, Psychiatry, Care of the Elderly, Cancer and Palliative Care, ENT, Ophthalmology, Women’s Health, Men’s Health and Breast and Urology. Questions appear in approximate proportion to the curriculum time dedicated to each subject. For the academic year 2015-16 the exam timetable is as follows: Taught revision: Monday 4 July - Friday 8 July 2016 Personal revision: Monday 18 July - Friday 22 July 2016 Clinical Assessments: Wednesday 13th and Friday 14th July 2016 Written Assessments: Tuesday 26 July 2016 Exam Board: Tuesday 2nd August 2016 There are 2 written papers, each lasting 3 hours and consisting of 150 Single best answer questions, each with 5 items. Written questions are all standard set by a panel of examiners, and overseen by external examiners from each module, to obtain an overall pass mark. The Medical School cannot release real questions from our exam bank, but sample questions are available on the school website, and books of questions are available commercially. End of module assessment, signoff for GP placements and Supervised Learning Events - ePortfolio An end of module assessment is completed for each student at the end of the block by one of the module leads. These are completed using the student ePortfolio and will include a grade of the student’s performance and take account of any comments on their procedures card, together with the SLEs and MSFs that have been recorded, so your feedback does contribute to the students’ final module assessment Placements in CoreGP, Dermatology, Women’s health, Child health, and Mental health in GP are not graded, but require tutors to sign the student off as having satisfactorily completed the placement on their student procedures card, which they will present to the tutor. Tutors may also be asked to complete Supervised Learning Events (SLEs) – formerly called Workplace-based assessments. The individual events are the same as last year except they now have text feedback only. Their generic name has changed however in line with the Foundation portfolio, on which the Undergraduate ePortolio is based. We would be very grateful if tutors could complete a few SLEs for their students while in practice – they really value the opportunity to get quality feedback from tutors, in a Primary Care environment. GP tutors and OSCE examinations We very much encourage GP tutors to take part as OSCE examiners. This helps you to see how the examination works and demonstrates to students that GP teachers are an integral part of the medical school. The OSCE exams for 2014-15 will be on Thursday 23rd and Friday 24th July 2015 and will take place at all 3 campuses from 9am to 5pm, and there is a substantial requirement for examiners on these 2 days. Please do try and keep one of these days free to examine. You Page 72 of 86 will be invited to offer your availability to examine in the second half of the academic year. You will also be asked to indicate which subject you would like to examine in, but we hope that as GPs you will feel able to examine across a range of subjects. Payment for GP Tutors examining in the OSCE is £320 (i.e. 2 sessions) for the day. If you have any specific questions regarding the Year 5 assessment or the ePortfolio please contact Dr Will Coppola on w.coppola@ucl.ac.uk. Other relevant assessments General practice: In Year 5 General Practice attachment students complete an end of firm assessment. In this exam students are highly likely to be assessed on their understanding of psycho-social dimensions of illness, and what they learn in this, the Mental Health in Primary Care attachment, will be very relevant and useful for this. Final MBBS: Although the exam at the end of the Year 5 is part of finals, the final MBBS exam at the end of year 6 also includes an OSCE exam in which there may well be a number of stations where knowledge of psychological or psychiatric problems is needed. In addition there are a number of primary care-orientated SBA questions written by members of the department of primary care in the written final exams. These may include the psychosocial dimensions of illness or be on common mental disorders. 5.2 Feedback from students Students are asked to complete an evaluation form online at the end of their attachment. We subsequently send a letter regarding their students’ feedback to each of the GP tutors. If you would like to discuss your students’ feedback with one of us, then we would be happy to oblige, please contact Dr Will Coppola on w.coppola@ucl.ac.uk. 5.3 Self and peer evaluation Self-evaluation Part of developing and growing as a teacher involves continually reflecting on your teaching. We would encourage you to do this regularly, and ideally at the end of each teaching session, taking a few moments to consider what went well and what you would like to change for the next time. Many teachers find it helpful to write this down, either on your lesson plan or on a structured form. This can then be referred to when you next teach that topic. We have created a sample structured form that you could use for this (see following sheet). Peer evaluation We currently do not have any formal method of having your teaching observed by your peers. This may be introduced in the future, and at present we are happy to facilitate informal arrangements for this. If you are interested then please contact the course coordinator who can give you guidance on the best ways of doing this. Page 73 of 86 ASSESSING YOUR OWN TEACHING Reflecting on your teaching and students’ learning is key in developing your skills as a teacher. Spend a few moments completing this form as soon as possible after your teaching experience. This can be included in your ‘Teaching Portfolio’. Please rate the following: Overall: poor 1 2 3 excellent 4 5 Set: Motivated students Assessed learner needs/knowledge: Aims & objectives 1 1 1 2 2 2 3 3 3 4 4 4 5 5 5 Body: Pace: Student interaction: Use of questions: Assessed student learning: 1 1 1 1 2 2 2 2 3 3 3 3 4 4 4 4 5 5 5 5 1 2 3 4 5 Closure: Summarise/relate to objectives: What happened in the session? Concentrate on what actually took place. What did I do which should help the students learn? (both before and during the session) What do I need to concentrate on improving next time I teach? Page 74 of 86 5.4 Tutor support & professional development We have a system of support and professional development for tutors in this module. We invite all tutors (both GPs and community psychiatry tutors) to review meetings once every 6 months or so. These are usually from 1pm to 3pm/3:30pm with lunch provided. This includes 1 hour for meeting your fellow tutors and discussing course development and problems. The remaining hour is usually aimed at professional development in mental health. For this we usually invite an external expert to attend and discuss how to address teaching about a particular mental health problem in a primary care or community setting. This also usually includes a discussion of current practice in diagnosis and management for that problem. If you have any concerns about the teaching, or about dealing with a particular student then we would strongly encourage you to contact Dr Will Coppola. If you have an administrative query about the placements then please contact Carol Lynch. 5.5 Course evaluation and quality assurance Course evaluation We have completed an extensive evaluation of the course, the findings of which have been published in the BMJ1. This involved a questionnaire survey of all the patients who had taken part in this course over one year – 95 of the 115 asked completed the questionnaire; and indepth interviews of 20 patients, 12 GP tutors, and 14 students. The questionnaire showed high levels of satisfaction with teaching encounters for participating patients, which were corroborated in the interviews. Many patients and general practitioners reported specific therapeutic benefits for patients from contact with students, including raised self-esteem and empowerment; the development of a coherent "illness narrative"; new insights into their problems; and a deeper, more balanced, and understanding doctor-patient relationship. For a few patients the teaching caused some distress, which may relate to a lack of insight into their condition or deficits in students' interviewing skills. Teaching Quality Assurance All medical schools now have to participate in an external review of their teaching quality. This is termed the Teaching Quality Assurance exercise (TQA), will occur every 5 years, is similar to OFSTED inspections for schools and is led by an independent panel of experts from the Quality Assurance Agency (QAA). Each medical school is assessed and graded on its teaching and support of learning in 6 areas, and given an overall score out of 24. UCL had its first TQA exercise in 1999 and scored 21/24. This information is freely available on their website, if you are interested in reading the full report http://www.qaa.ac.uk/reviews-and-reports/provider?UKPRN=10007784#. As part of our internal quality assurance we ensure tutors receive student feedback and offer opportunities for professional development and support. We will also from time to time talk to tutors individually about their teaching and to review opportunities for their development as teachers. 1 Walters K, Buszewicz M, Russell J & Humphrey C. (2003). Teaching as therapy: cross sectional and qualitative evaluation of patients' experiences of undergraduate psychiatry teaching in the community. British Medical Journal, 326:740-5 Page 75 of 86 6 Further information In the following pages we have included additional resources, which may be useful to you. We are also keen for tutors to share resources so if you have any lesson plans, websites or nuggets of information you wish to share, please email Dr Will Coppola or Dr Mel Gardner. 6.1 Reading & other resources list for tutors This is a list of recommended reading for students and some more postgraduate textbooks, which you may find useful for reference. The videos we have included as you may find these useful as a back-up plan for when patients are not able to attend at short notice. Basic textbooks: Katona C & Robertson M. (2000). Psychiatry at a Glance. Oxford: Blackwell Science. £13.95 Gelder M, Mayou R & Geddes J. (2005). Psychiatry (3rd ed.). Oxford: Oxford University Press. £19.95 paperback version Puri, BK. (2008). Pocket Essentials of Psychiatry (3rd ed.). Saunders. £15.95 Rees L, Lipsedge M & Ball C. (1997). Textbook of Psychiatry. London: Arnold. £17.99 Goldberg D, Benjamin S, Creed F. (1994). Psychiatry in Medical Practice (2nd ed.). London: Routledge. £18.99 More detailed or specialised texts: Gelder M, Gath D, Mayou R. (2009). New Oxford Textbook of Psychiatry (2nd ed.). Oxford: Oxford University Press. (Expensive but detailed & probably still the widest used postgraduate textbook in psychiatry.) Sims A. (1995). Symptoms in the mind (2nd ed.). Saunders. Sadock & Sadock. (2007). Kaplan and Sadock’s Synopsis of Psychiatry (10th ed.). Lippincott Williams and Wilkins. Fish F. (1978). Fish’s Outline of Psychiatry (3rd ed.). Bristol: Wright. Taylor D, McConnell H, McConnell D & Kerwin R. (2001). The Maudsley 2001 Prescribing Guidelines (6th ed.). London: Martin Dunitz. WHO. (1993). The ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic Criteria for Research. Geneva: Author. Videos: A series of videos are available for purchase through the University of Manchester (see their online catalogue at http://www.medicine.manchester.ac.uk/psychiatrytrainingvideos/catalogue) Page 76 of 86 Appendix 1 Objective Structured Clinical Assessments (OSCEs) GP Tutor notes The student exam at the end of the year takes the form of an OSCE (Objective Structured Clinical Assessment). We find that as students come towards the end of the year they increasingly request, and value, practice for this exam. Some tutors do incorporate this into their teaching and find it a useful tool for motivating and assessing the students. What follows is an outline of the OSCE exam and some suggestions about how to give your students practice for this if you wish to. There are many reasons to assess students’ knowledge and skills; for example to judge competence, to pick up problems, to motivate, to evaluate the effectiveness of the teaching, to monitor improvement over time and to rank students. Ideally an assessment should be valid (measure what is intended to be measured) and reliable (give consistent results), A well-designed OSCE should achieve both these criteria and so OSCEs are used increasingly in student exams. An OSCE takes the form of a series of stations at each of which the student is asked to complete a specific task. The nature of the task varies from station to station, for example; history taking, patient education, interpersonal skills (e.g. giving news to a relative), interpreting results, physical examination and practical procedures. In the neuropsychiatry block OSCE there are 20 stations, each lasting 5 minutes, with additional time allowed during which the student transfers to the next station and the examiner records the marks. In order to plan a whole OSCE, the examiners create a blueprint. As you can see from the blueprint for the neuropsychiatry block OSCE (page 79), the blueprint is a matrix with subject areas to be included down one side (in this case mostly clinical areas within neurology, ophthalmology and psychiatry), and competencies (in this case regarding aspects, including ethics and law, of the subjects areas, and regarding communication and examination skills) down the other. The examiners aim to test a wide variety of these competencies with regard to as many of the subject areas as possible. Of course, no one station can test all these: the blueprint is used to help the examiners contemplate which competencies are best tested in which subject areas, and as a guide to how good a spread of testing of both subject areas and competencies is achieved. At each station in the neuropsychiatry block OSCE, only one subject area is usually tested per station, although this is not always the case. On the other hand, more than one competency is usually tested at each station, with communication skills being tested at most interactive (as opposed to written) stations and, as in the example given here (page 80), typically making up 25% of the marks for such a station. If you decide to create your own OSCE stations for your students, you won’t need to achieve the same spread of testing that the examiners aim for in the neuropsychiatry block final exam. However, you’ll probably find it useful to look at the blueprint to help you consider which competencies and subject areas you want to test in each station. Once you’ve decided this, you will need to work out an appropriate task and then how the student’s performance will be marked. Considering one of the neuropsychiatry block OSCE stations may help you do this. See the details of the OSCE station on page 80 regarding assessing a patient after an overdose. Like many of the OSCE stations in the neuropsychiatry exam, this station uses an actor or simulated patient. The actor is given clear instructions on the role that they’re playing, and the student is given a brief history regarding the “patient” and asked to assess the patient appropriately. In order to assess each student reliably, the competencies to be tested have been broken down into a list of criteria, each with allocated marks. For each Page 77 of 86 criterion the student achieves he/she is awarded the set mark. Although there is some room for the marker’s judgement, the marking schedule is quite prescriptive. This makes marking less daunting than it might be. If you would like experience being involved in the neuropsychiatry block OSCE, please let Carol Lynch know (carol.lynch@ucl.ac.uk). When you’re making up a task to test the subject area(s) and competencies you’ve chosen, that task needn’t be very complicated. For example, you might ask the student to answer someone’s questions regarding their elderly mother who has just been diagnosed with Alzheimer’s disease; or you might wish to ask the student to explain treatment options to a patient with moderately severe depression, ensuring that the “patient” asks for details of drug therapy and the different types of talking therapy. It’s probably a good idea to use topics that you have taught on in the GP mental health module. Decide whether you want a student to help in the OSCE by playing a role. This can be fun and may be educational in itself, in that it helps that student to consider how it feels to be in the position of the person they’re playing; on the other hand it won’t work well if the student doesn’t engage well, and may occasionally be distressing for the student – careful use of the guidance regarding role play (page 71 in the tutors’ guide) should guard against this. If you don’t want a student to act out a part, you’ll need to work out how else you’ll arrange the station and may choose to act out a role yourself. Whatever you decide, it’s useful, by the time you practice using the OSCE station, to have clear instructions for the “student actor” or yourself, and a clear task defined for the student who is going to be asking the questions as in the OSCE exam. The other two students can be asked to devise a marking sheet, compare this with whatever you’ve decided the marking structure should be, and then use the final product to “assess” the student practising the OSCE station. Although you may not be interested in giving the student an exact mark for their performance, it is useful to consider a break down of the competencies you’re testing, just as in the example station below regarding assessing suicide risk (page 80), and to decide which criteria an ideal student should achieve. This will help you give specific feedback to the student on what they have done well and what they can improve on. You may wish to try some stations out on a colleague before using them with the students. You may also find that once you’ve tried out some stations with the students, you’ll want to make some adjustments to them. Unlike in the neuropsychiatry block OSCE, when you give the students OSCE practice they will be examined one at a time. Meanwhile the other students will observe. In order to reduce the stress level of the examined student, and to emphasise the educational over the assessment component, some tutors tell the students who have volunteered to ‘be examined’ that they can choose “time out” during their OSCE station. This gives them time under less pressure during which to reflect on the task and even to ask the other students for advice; and is particularly useful when a student “freezes” on assessment. Planning OSCE stations well is challenging but should be rewarding. Students are motivated by them and are pleased at the opportunity both to demonstrate their learning and to practice for their forthcoming exam. In addition, tutors may find them a useful guide to the success of their teaching. Page 78 of 86 Neuropsychiatry block OSCE blueprint diagnosis Aetiol./ clinic. Path. Ix epidem feats. Mx Psychosis Dementia P Depression Elation Delirium P Self-harm Anxiety Subst abuse Eating dis Learn dis Psychol Rx Somatisation Forensic etc Person. dis Comm care C&A Dementia N Delirium N MS Stroke Headache Epilepsy Parkinson’s CNS infect Pub Health Page 79 of 86 use of ethics/ comm. clinical MSE meds. law skills exam EXAMPLE: OSCE station regarding assessment after an episode of self-harm (this can be used with your students – it is not an actual exam question) NB: http://www.trickcyclists.co.uk/ is a useful website for inspiration when planning OSCE questions Student’s instructions You are a GP. You have been called out to see a patient by her parents who are extremely concerned about her. She called them over having cut her wrists. Her wounds are superficial and do not need further treatment. Assess her / him appropriately regarding their mental state and suicide risk. Simulated Patent / Actor’s role You are a 23 year old musician. You are depressed and have just cut your wrists. These are cuts which bled initially, but have now stopped bleeding and been bandaged. Actor to volunteer this information to the student: You cut your wrists but then became very scared and phoned your parents. They came round and brought you straight to the GP surgery as they are so concerned about you. + Actor to only give this further information if directly asked/encouraged by the student: You had drunk a bottle of wine before cutting your wrists. You were on your own but got frightened after doing so, and called your parents. You hadn’t planned it or left a note. You feel there’s nothing to live for and that you make everyone’s life more complicated. You’ve been depressed for at least 2 months but haven’t sought any medical help/advice. You feel isolated and hopeless. You feel you are a failure and that you’re not as good a musician as other people. You do have good friends but have no partner, and live alone. You can’t sleep, have little appetite and have lost some weight. Now, you still feel down and can’t smile. You speak quietly in short sentences. You do regret what you did and feel embarrassed about it. You didn’t really want to die, but you feel things can’t go on like this. You want some help. You feel worthless and guilty for the distress you’ve caused. You are otherwise fit, have never seen a psychiatrist before and only drink socially. Marking criteria: (Neuropsychiatry OSCEs are traditionally marked out of 20) 1. Communication skills Polite introduction and puts patient at ease 1 Balance of open and closed questions 1 Facilitates responses (e.g. non-verbal communication, silences) 1 Responds to cues 1 Overall mark for empathy 1 2. Event details What done? 1 Degree of planning? 1 Preparation to die / suicide note? 1 Timed self-harm to prevent discovery? 1 Events after self-harm 1 Page 80 of 86 3. Background Biological features of depression 1 Psychological features of depression 1 Previous attempts/ past psychiatric history 1 Social risk factors 1 Brief alcohol history 1 4. Current suicide risk Views on self-harm / regret 1 Current suicidal thoughts 1 Current suicidal concrete plans 1 View of future 1 5. Examiner to ask student re current suicide risk (low to moderate) 1 Page 81 of 86