Ultrasound Guided Procedures: Disclosures Tips and Techniques for both Common and Uncommon
advertisement

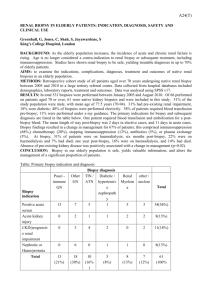
Ultrasound Guided Procedures: Tips and Techniques for both Common and Uncommon Indications Disclosures ! None Geoffrey Wile, MD (VUMC) Acknowledgements Learning Objectives ! Dr. Hisham Tchelepi ! Patient selection and preparation ! Dr. Melanie Caserta ! Image optimization ! Standard techniques in difficult biopsies ! Advanced techniques US vs. CT ! Advantages of US guided biopsy ! No ionizing radiation ! Faster and less expensive ! Portable ! May enhance safety ! When to do CT Patient Preparation Planning is Essential to Success and may be risk stratified* ! Lab work* ! INR < 1.5 ! Platelets > 50,000/mL ! May need to use FFP or platelet transfusion in selected cases ! Stop Anticoagulation* ! ASA – 325mg 5-7 days off ! In most cases, biopsy can be performed safely on aspirin** ! Adrenal and retroperitoneal masses ! Plavix – 5-7 days ! Coumadin – 5-7 days, may need to bridge with heparin ! Calcified masses ! Heparin – 4-6 hours; Lovenox 12-24 hours ! Improved visualization of structures difficult to see with US* ! Gas filled collections ! Lung lesions not abutting the pleura ! Certain pelvic masses or collections ! Newer agents and special concerns ! NPO 6 hours prior to procedure if using sedation * Patel IJ, Davidson JC, Nikolic B, et al. Consensus Guidelines for Periprocedural Management of Coagulation Status and Hemostasis Risk in Percutaneous Image-guided Interventions. JVIR. 2012;23(6):727–736. **Atwell TD, Smith RL, Hesley GK, et al. Incidence of Bleeding After 15,181 Percutaneous Biopsies and the Role of Aspirin. AJR 2010; 194:784-789 1 Procedure ! Pain Control/Sedation ! Liberal local anesthesia with lidocaine – 10-20 mL ! Moderate Sedation ! Versed and Fentanyl ! Needle safety is critical ! Needle guide is helpful but not always necessary (superficial biopsies) ! Image optimization ! Key feature of biopsy – should do this prior to becoming sterile ! Use highest possible frequency probe Optimizing Technique ! Keys to success ! Seeing the needle ! ! ! ! ! ! Sound beam should be perpendicular to needle Can try to move inner stylet without moving outer needle Rotate the needle Echogenic needle coatings may be helpful Doppler artifact Add compounding ! Seeing the lesion ! Harmonics should be standard ! Can play with dynamic range to broaden the spectrum of frequency ! Can use various colors (B color mode) to improve conspicuity ! Assistant can change the parameters on the machine Procedure: Multiple Passes vs Coaxial Technique Post procedure ! Multiple Passes ! May have higher success rate because can biopsy different areas of lesion* ! Performed during suspended respiration in liver to minimize “tearing” of capsule, may be difficult in sedated patients ! Focal discrete punctures may bleed less ! Disadvantages*: ! ! May have to puncture many times in a difficult case If lesion access is difficult the coaxial technique decreases complexity once needle is in position ! Coaxial Technique* ! Can be helpful in challenging cases to place an introducer and then obtain multiple samples through a “single hole” ! Less trauma to adjacent tissue ! Theoretically less risk of tumor seeding ! Disadvantages ! ! ! Potential shearing of capsule Larger puncture hole Repetitive sampling of same area * Winter TC, Lee FT, Hinshaw JL. Ultrasound Guided Biopsies in the Abdomen and Pelvis. Ultrasound Quarterly 2008; 24: 45-68. ! Imaging ! Personal preference to image post biopsy ! Most bleeds are small and asymptomatic ! Atwell et al. found that overall risks of major bleeding and death due to percutaneous biopsy are low (0.5% and 0.02% respectively) ! Monitoring ! Observe for 3-4 hours in holding area after intra-abdominal biopsy ! Transplant biopsies are observed by transplant surgery team following biopsy. ! Superficial lymph node biopsies and thyroid biopsies do not require observation Atwell TD, Smith RL, Hesley GK et al. Incidence of Bleeding After 15,181 Percutaneous Biopsies and the Role of Aspirin. AJR 2010; 194: 784-789 Complications ! Serious complications are infrequent ! Intra-abdominal bleeding is the most serious complication ! Rarely requires intervention beyond monitoring and supportive care ! Bleed rate <5% for 18g and smaller needles* ! Pneumothorax ! Damage to bowel or adjacent vessels infrequent ! Infection (<1%) Neck ! Thyroid Biopsy ! Generally performed with FNA ! Performed with on site cytology ! Lymph Node Biopsy ! May be FNA or core ! Hard to access nodes in superior mediastinum may also be sampled from neck/supraclavicular region ! Mass/Other ! Superficial or deep neck masses * Winter TC, Lee FT, Hinshaw JL. Ultrasound Guided Biopsies in the Abdomen and Pelvis. Ultrasound Quarterly 2008; 24: 45-68. 2 Chest Liver ! Random Liver ! Preferred site is left liver, epigastric area ! Biopsy in the chest with US is an accepted technique for lesions involving the chest wall, abutting or involving the pleura. ! Pleural ! *Appelbaum et al. found that 3 passes (18g core) would be diagnostic in almost 90% of cases if no cytology service was available ! Lung Parenchyma ! Post-Biopsy complications i.e. pneumothorax may also be recognized/excluded quickly with US. Yang, P. C. (2000). Ultrasound-guided transthoracic biopsy of the chest. Radiologic Clinics of NA, 38(2), 323–343. Kidney ! Abscess drain/aspiration ! Always put on color to avoid vasculature ! HV and PV can be safely traversed if needed** ! Avoid hepatic artery *Appelbaum L, Kane RA, Kruskal JB et al. Focal Hepatic Lesions: US Guided Biopsy- Lessons from Review of Cytologic and Pathologic Examination Results. Radiology 2009; 250 (2): 453-458. ** Winter TC, Lee FT, Hinshaw JL. Ultrasound Guided Biopsies in the Abdomen and Pelvis. Ultrasound Quarterly 2008; 24: 45-68. Transplant Kidney ! To assess for rejection ! Tissue sampling is becoming more acceptable ! According to AASLD practice guidelines no need to biopsy liver nodule >1cm with diagnostic features for HCC by imaging ! Exceptions may be made if imaging features are atypical or tissue is needed for systemic therapy or study requirements. ! Chest Wall ! ! ! ! ! Targeted biopsy Extremely low risk of tumor seeding* Useful in suspected lymphoma Useful in suspected metastasis vs RCC Performed prior to RFA** ! Nonfocal biopsy ! Biopsy may be performed at one month post-transplant to assess for early rejection ! Other biopsies are done as clinically indicated ! Three approaches ! Cortical tangential* ! Transverse lower pole ! Lateral parasagittal ! Evaluate for nephropathy *Uppot RN, Harisinghani MG, Gervais DA. Imaging-Guided Percutaneous Renal Biopsy: Rationale and Approach. AJR 2010; 194: 1443-1449 **Uppot, R. N., Silverman, S. G., Zagoria, R. J., Tuncali, K., Childs, D. D., & Gervais, D. A. (2009). Imaging-Guided Percutaneous Ablation of Renal Cell Carcinoma: A Primer of How We Do It. AJR. American Journal of Roentgenology, 192(6), 1558–1570. doi:10.2214/AJR.09.2582 Complications of Renal Tx Bx * Patel MD, , Phillips CJ, Young SW, et al. US Guided Renal Transplant Biopsy: Efficacy of a Cortical Tangential Approach. Radiology. 2010; 256: 290-296. Complications of Renal Tx Bx ! Arteriovenous Fistula ! Elevated velocity in feeding artery ! Turbulent flow ! Color aliasing ! Reverberation artifact ! Pseudoaneurysm ! To and Fro motion on spectral doppler ! Yin Yang appearance Case Courtesy of Hisham Tchelepi, MD 3 Pancreas Transplant Complications of Renal Tx Bx ! Relatively safe biopsy ! Watch out for bowel ! Color Doppler is important ! Technique ! Two 18 g passes Turbulent swirling flow = yin yang Pancreas Transplant ! Choice of needles ! Bard Monopty Device ! Fixed 2.2 cm throw ! Angiotech Biopince Device ! Adjustable throw: 1.3, 2.3, and 3.3 cm ! Angiotech Super Core ! Adjustable throw: 1.2 and 2.2cm ! Can advance needle under real time US before you cut The choice of which biopsy device to use is based on the requirements for the procedure. There is no financial incentive in choosing a specific device. Spleen* ! Not widely performed because of perceived risk of increased complications ! US provides real time guidance and shorter procedure time * Singh JK, Shankar S, Gervais DA et al. Image Guided Percutaneous Splenic Interventions. RadioGraphics 2012; 32: 523-534 Peritoneum Peritoneum ! Challenges ! Advantages ! Ability to compress the tissues ! Mesentery and omentum are mobile and soft structures ! Bowel and major vessels are close ! Possibility of displacing bowel out of the way ! Real time needle visualization provides a major advantage over CT Lee JK, Baek SY, Lim SM, Lee KH. Reticular Infiltrations Alone without Mass in the Mesentery and Omentum Identified at Contrast Enhanced CT: Efficacy of US Guided Percutaneous Core Biopsy. Radiology. 2011 261; 1: 311-317. Ovarian Serous Adenocarcinoma 4 Pelvis ! Inguinal Masses or Lymph Nodes can typically be accessed by ultrasound New Techniques: Fusion Imaging ! Useful in interventional procedures ! Hard to see ! Adnexal Masses ! Hard to get to ! Typically avoid this ! Theoretical concern for risk of seeding ! Diagnostic accuracy of ovarian cyst aspiration is controversial ! In special circumstances and when requested by Gyn Onc – we may aspirate or biopsy adnexal mass for diagnosis. ! Helps to make biopsy safer and easier on difficult cases ! Abscess What is Fusion Imaging? Fusion Imaging Technique ! Import the image data set into the US machine prior to the case ! Complete DICOM data set can be uploaded via PACS or directly via CD ! Fusion imaging combines volumetric anatomic data from CT, MRI or PET with the real time multiplanar capability of US ! To register the US image with the 3D MR or CT data set, a series of common anatomic points or planes are manually identified on both the US image and CT data set ! Left portal vein is a reliable landmark ! Can also use umbilicus Fusion Imaging Display § Target Point (T) can be assigned § First assigned on the CT or MR image then automatically generated on US ! US displayed on left, Multiplanar Reformat (MPR) from 3D data set on right Key Points ! Patient selection and pre-procedure planning increases the probability of success even in difficult cases ! Basic knowledge of ultrasound image optimization is critical ! In most cases careful application of basic tools allows for uncomplicated access/tissue acquisition ! Advanced techniques may be helpful in very challenging cases ! As US probe is moved, the MPR image tracks in real time ! MPR image can also be overlapped on the US image Case Courtesy of Hisham Tchelepi, MD 5 References 1. Winter TC, Lee FT, Hinshaw JL. Ultrasound-guided biopsies in the abdomen and pelvis. Ultrasound Q. 2008;24(1):45–68. 2. Kliewer MA, Sheafor DH, Paulson EK, Helsper RS, Hertzberg BS, Nelson RC. Percutaneous liver biopsy: a cost-benefit analysis comparing sonographic and CT guidance. American Journal of Roentgenology. 1999;173(5):1199–1202. 3. Atwell TD, Smith RL, Hesley GK, et al. Incidence of Bleeding After 15,181 Percutaneous Biopsies and the Role of Aspirin. AJR Am J Roentgenol. 2010;194(3):784–789. 4. Malloy PC, Grassi CJ, Kundu S, Gervais DA. Consensus guidelines for periprocedural management of coagulation status and hemostasis risk in percutaneous imageguided interventions. Journal of Vascular and …. 2009. 5. Yang PC. Ultrasound-guided transthoracic biopsy of the chest. Radiologic Clinics of NA. 2000;38(2):323–343. 6. Appelbaum MD L, Kane MD RA, Kruskal MD PhD JB, Romero MD J, Sosna MD J. Focal Hepatic Lesions: US-guided Biopsy--Lessons from Review of Cytologic and Pathologic Examination Results. Radiology. 2009;250(2):453–458. 7. Singh AK, Shankar S, Gervais DA, Hahn PF, Mueller PR. Image-guided Percutaneous Splenic Interventions. Radiographics. 2012;32(2):523–534. 8. Uppot RN, Harisinghani MG, Gervais DA. Imaging-Guided Percutaneous Renal Biopsy: Rationale and Approach. AJR Am J Roentgenol. 2010;194(6):1443–1449. 9. Uppot RN, Silverman SG, Zagoria RJ, Tuncali K, Childs DD, Gervais DA. Imaging-Guided Percutaneous Ablation of Renal Cell Carcinoma: A Primer of How We Do It. AJR Am J Roentgenol. 2009;192(6):1558–1570. 10. Patel MD, Phillips CJ, Young SW, et al. US-guided Renal Transplant Biopsy: Efficacy of a Cortical Tangential Approach. Radiology. 2010;256(1):290–296. 11. Lee JK, Baek SY, Lim SM, Lee KH. Reticular Infiltrations Alone without Mass in the Mesentery and Omentum Identified at Contrast-enhanced CT: Efficacy of USguided Percutaneous Core Biopsy. Radiology. 2011;261(1):311–317. 12. O’Neill MJ, Rafferty EA, Lee SI, et al. Transvaginal Interventional Procedures: Aspiration, Biopsy, and Catheter Drainage1. Radiographics. 2001;21(3):657–672. 13. MD DDC, MD HT. Ultrasound and Abdominal Intervention: New Luster on an Old Gem. Ultrasound Clinics. 2009;4(1):25–43. 6