Benefits and Compensation Alert
April 2, 2010
Authors:
Mary Turk-Meena
mary.turk-meena@klgates.com
+1.704.331.7590
Lynne S. Wakefield
lynne.wakefield@klgates.com
+1.704.331.7578
Emily D. Zimmer
emily.zimmer@klgates.com
+1.704.331.7405
K&L Gates includes lawyers practicing out
of 36 offices located in North America,
Europe, Asia and the Middle East, and
represents numerous GLOBAL 500,
FORTUNE 100, and FTSE 100
corporations, in addition to growth and
middle market companies, entrepreneurs,
capital market participants and public
sector entities. For more information,
visit www.klgates.com.
Immediate Impact of Health Care Reform
Legislation on Employer-sponsored Group
Health Plans
On March 23, 2010, President Obama signed into law the Patient Protection and
Affordable Care Act, followed by the Health Care and Education Reconciliation Act
of 2010 on March 30, 2010 (collectively, the Acts). Together, these two Acts
constitute sweeping health care reform legislation with far reaching implications for
individuals, insurance companies, health care providers and employers. This Alert
focuses on those provisions of the Acts with the most immediate impact on
employer-sponsored group health plans. The attached charts summarize these key
provisions. Over the course of the next few weeks and months, we will be providing
a series of additional alerts outlining other key aspects of the Acts from an employer
perspective such as new reporting and disclosure requirements, the employer pay-orplay mandate, provisions of the Acts with effective dates later than 2011 and
important guidance issued by the various governmental agencies. In the meantime, if
you have any questions, please contact the individuals listed for this article, or the
K&L Gates lawyer with whom you work.
Benefits and Compensation Alert
Compensation and Benefits Alert: Immediate Impact of Health Care Reform Legislation on Employer-sponsored Group Health Plans
FINANCIAL CHANGES
Change
Loss of Deduction for
Medicare Part D
Subsidy
Creation of Retiree
Reinsurance Program
Description
Effective Date
Action Steps
Employers’ tax deductions will be reduced to the
extent the employer’s drug expenses are reimbursed
under the Medicare Part D retiree drug subsidy
program.
Deduction ends 1/1/2013
·
Full accounting impact of the
loss of this federal tax
deduction must be recognized
on current financial statements
·
This program provides for reimbursement by the
federal government of certain employer costs in
connection with employer-provided retiree health
coverage. To be eligible for the program, the
employer plan must:
· Include programs to generate cost savings for
participant with chronic and high cost conditions
· Provide documentation of the actual cost of
medical claims
· Submit an application for reimbursement to HHS
· Use recouped amounts to lower cost of plan (e.g.,
reduce premium costs, copayments, deductibles,
coinsurance or other out-of-pocket costs
Amounts recouped will be audited annually by HHS
Program begins within 90 days
of enactment and ends on the
earlier of exhaustion of $5
billion allocation or 12/31/2014
1
·
·
·
Coordinate with finance and
auditors to determine financial
impact
For public companies, consider
whether public announcement of
impact on financial statements is
necessary or appropriate
Once program is established,
determine whether information
needed for reimbursement
application is available
Determine whether retiree health
plan meets the criteria for
eligibility for reimbursement
Determine whether application
should be made for
reimbursement
Benefits and Compensation Alert
PLAN DESIGN CHANGES
Change
Coverage of Dependent
Children up to Age 26
Description
Effective Date
Coverage must be provided to dependent children of ·
covered employees until the dependent child reaches
age 26. The requirement applies regardless of the
·
dependent child’s marital or student status.
Coverage need not be provided to children of the
dependent child. Coverage is not taxable to
employee or dependent child.
·
·
Elimination of Lifetime
Limits
A plan may not impose a lifetime limit on the dollar
value of essential health benefits (as defined in the
Acts)
·
·
For plan years beginning on
or after 9/23/10
Before 1/1/14: applies to
grandfathered plans only
with respect to dependent
children not eligible for
coverage under another
employer’s health plan
On and after 1/1/14: applies
to all plans regardless of
dependent child’s eligibility
for coverage under anther
employer’s health plan
CBA effective date: Upon
termination of last
collective bargaining
agreement in effect on
3/23/10
For plan years beginning on
or after 9/23/10
CBA effective date: Upon
termination of last
collective bargaining
agreement in effect on
3/23/10
Actions Steps
·
·
·
·
·
·
·
·
·
2
Determine cost impact
Determine whether and how to
charge for coverage
Confirm coverage changes with
TPAs, insurers and stop-loss
providers
Revise plan documents,
enrollment materials, SPDs and
other employee communications
Identify each lifetime limit
currently imposed
Determine whether plan change is
required
Determine cost impact
Confirm coverage changes with
TPAs, insurers and stop-loss
providers
Revise plan documents,
enrollment materials, SPDs and
other employee communications
Benefits and Compensation Alert
PLAN DESIGN CHANGES
Change
Restriction/Elimination
of Annual Limits
Description
Effective Date
A plan may not impose unreasonable annual limits
on the dollar value of essential health benefits (as
determined by HHS)
·
·
Before 1/1/14: Restricted
annual limits permitted as
determined by HHS
On or after 1/1/14: No
dollar value limits
permitted
Actions Steps
·
·
·
·
·
Coverage of Preventive
Care
First-dollar coverage is required for certain
evidence-based preventive care, well child care and
immunizations (i.e., no deductible, copayment,
coinsurance or other cost sharing permitted)
·
·
Does not apply to grandfathered plans
For plan years beginning on
or after 9/23/10
CBA effective date: Upon
termination of last
collective bargaining
agreement in effect on
3/23/10
·
·
·
·
·
Prohibition on Preexisting Condition
Exclusions
A plan may not impose a pre-existing condition
exclusion on coverage for a child under age 19
·
·
3
For plan years beginning on
or after 9/23/10
CBA effective date: Upon
termination of last
collective bargaining
agreement in effect on
3/23/10
·
·
·
·
Identify each dollar limit
currently imposed
Determine whether plan change is
required
Determine cost impact
Confirm coverage changes with
TPAs, insurers and stop-loss
providers
Revise plan documents,
enrollment materials, SPDs and
other employee communications
Determine whether plan is
grandfathered and thus exempt
from this requirement
If plan is not grandfathered,
determine whether plan change is
required
Determine cost impact
Confirm coverage changes with
TPAs, insurers and stop-loss
providers
Revise plan documents,
enrollment materials, SPDs and
other employee communications
Determine whether plan change is
required
Determine impact on cost of plan
Confirm coverage changes with
TPAs, insurers and stop-loss
providers
Revise plan documents,
enrollment materials, SPDs and
other employee communications
Benefits and Compensation Alert
PLAN ADMINISTRATION CHANGES
Change
Change in
Reimbursement for
Certain Over-theCounter Items
Nondiscrimination
Rules for Insured Plans
Description
Effective Date
Over-the-counter items purchased without a Expenses incurred after 12/31/10
doctor’s prescription are not eligible for
reimbursement as a medical expense under
flexible spending accounts, health
reimbursement arrangements, health savings
accounts and Archer MSAs
Nondiscrimination requirements of Code
· For plan years beginning on or after
Section 105(h) previously applicable only to
9/23/10
self-insured plans are also applicable to
· CBA effective date: Upon
fully-insured plans; insured plans that do
termination of last collective
not meet Section 105(h) rules are prohibited
bargaining agreement in effect on
3/23/10
Does not apply to grandfathered plans
Action Steps
·
·
·
·
·
·
·
·
4
Revise plan documents,
enrollment materials, SPDs and
other employee communications
Coordinate change with medical
account plan vendors
Identify all insured arrangements
Determine whether plan is
grandfathered and thus exempt
from this requirement
If plan is not grandfathered,
determine if discrimination rules
can be met
If changes are necessary, evaluate
compliant alternatives, including
expanding coverage or
eliminating coverage
Coordinate any changes with
insurer
Confirm insurer will revise
affected policy and provide
updated enrollment materials,
SPDs and other employee
communications
Benefits and Compensation Alert
PLAN ADMINISTRATION CHANGES
Change
Revisions to Claim
Appeals Process
Employer May Not
Encourage
Disenrollment from
Employer-Based Plans
Description
Plan appeal procedure must:
· Provide notices in a culturally and
linguistically appropriate manner of
availability of process and any
applicable health insurance ombudsman
created by state to assist claimant with
appeal
· Allow claimants to review entire file
and provide testimony
· Allow claimants to continue coverage
during appeals process
· Establish external review process that
complies with Uniform External
Review Model Act (for self-insured
plans, HHS is to provide regulations
with similar protections)
Does not apply to grandfathered plans
Employers may not offer money or other
financial consideration to encourage
employees to disenroll from employerprovided coverage and enroll in state high
risk pool
Effective Date
·
·
For plan years beginning on or after
9/23/10
CBA effective date: Upon
termination of last collective
bargaining agreement in effect on
3/23/10
Action Steps
·
·
·
·
·
High risk pools are to be established by
6/23/10
·
·
5
Determine whether plan is
grandfathered and thus exempt
from this requirement
If plan is not grandfathered,
determine the extent to which
existing appeal process meets
new requirements
Determine how to meet coverage
continuation requirement
Revise plan documents,
enrollment materials, SPDs and
other employee communications
Coordinate change with claims
administrators
Review any cash or other
incentives currently provided; it is
unclear whether broad-based
incentives will continue to be
permitted if it results in
enrollment in state high risk pool
Consider alternatives to any cash
or other incentives currently
provided
Benefits and Compensation Alert
PLAN ADMINISTRATION CHANGES
Change
Prohibitions on
Rescinding Coverage
Increased Excise Tax
for Nonqualified
Distributions from
Health Savings
Accounts
Description
Employers may not rescind coverage except
in cases of fraud or intentional
misrepresentation, as prohibited by the
terms of the plan or coverage, and prior
notice to enrollee is required to terminate
coverage
Does not prohibit termination of plan as a
whole, but unclear whether prohibits
termination for nonpayment, such as by
employees on an unpaid leave of absence or
by retirees
The excise tax on use of HSA funds for
items other than qualified medical expenses
is increased from 10% to 20% (including
distributions for over-the-counter items not
purchased under a doctor’s prescription)
Effective Date
·
·
For plan years beginning on or after
9/23/10
CBA effective date: Upon
termination of last collective
bargaining agreement in effect on
3/23/10
HSA distributions after 12/31/10
6
Action Steps
·
Review grounds for terminating
an employee’s coverage and
ensure that they constitute fraud
or intentional misrepresentation
of a material fact
·
Revise any applicable enrollment
materials, SPDs and other
employee communications
Benefits and Compensation Alert
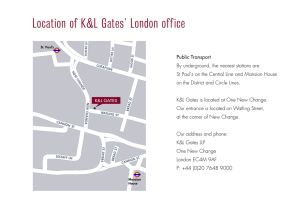
Anchorage Austin Beijing Berlin Boston Charlotte Chicago Dallas Dubai Fort Worth Frankfurt Harrisburg Hong Kong London
Los Angeles Miami Moscow Newark New York Orange County Palo Alto Paris Pittsburgh Portland Raleigh Research Triangle Park
San Diego San Francisco Seattle Shanghai Singapore Spokane/Coeur d’Alene Taipei Tokyo Warsaw
Washington, D.C.
K&L Gates includes lawyers practicing out of 36 offices located in North America, Europe, Asia and the Middle East, and represents numerous
GLOBAL 500, FORTUNE 100, and FTSE 100 corporations, in addition to growth and middle market companies, entrepreneurs, capital market
participants and public sector entities. For more information, visit www.klgates.com.
K&L Gates is comprised of multiple affiliated entities: a limited liability partnership with the full name K&L Gates LLP qualified in Delaware and
maintaining offices throughout the United States, in Berlin and Frankfurt, Germany, in Beijing (K&L Gates LLP Beijing Representative Office), in
Dubai, U.A.E., in Shanghai (K&L Gates LLP Shanghai Representative Office), in Tokyo, and in Singapore; a limited liability partnership (also named
K&L Gates LLP) incorporated in England and maintaining offices in London and Paris; a Taiwan general partnership (K&L Gates) maintaining an
office in Taipei; a Hong Kong general partnership (K&L Gates, Solicitors) maintaining an office in Hong Kong; a Polish limited partnership (K&L
Gates Jamka sp. k.) maintaining an office in Warsaw; and a Delaware limited liability company (K&L Gates Holdings, LLC) maintaining an office in
Moscow. K&L Gates maintains appropriate registrations in the jurisdictions in which its offices are located. A list of the partners or members in each
entity is available for inspection at any K&L Gates office.
This publication is for informational purposes and does not contain or convey legal advice. The information herein should not be used or relied upon
in regard to any particular facts or circumstances without first consulting a lawyer.
©2010 K&L Gates LLP. All Rights Reserved.
April 1, 2010
2