V02 [Please ensure this Protocol template
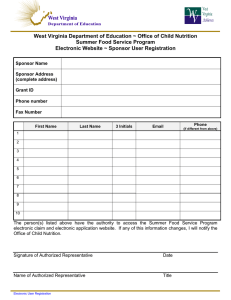
advertisement

D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Page 1 of 39 [Please ensure this Protocol template V02 is the most recent version: by logging on to http://www.ucl.ac.uk/jro/standingoperatingprocedures/document-library] Text in red is for instruction only and should be deleted. Text in blue should be included if appropriate for the trial. Full title of trial [Click here and type full descriptive trial title] Title to include phase, design (e.g. double-blind, randomised, placebo-controlled), single- site/multi-site, name of IMP, target disease, and subject population. Short title [Click here and type short title] The full and short title must be the same on all trial documents e.g. patient information sheet. Version and date of protocol [Type 'Draft' here if applicable] Version [Insert version number], [insert date] [The protocol you send to the MHRA and REC should be V1] Sponsor: University College London (UCL) Sponsor protocol number [Type sponsor protocol number] Funder (s) : [Names of ALL organisations providing funding for this trial] EudraCT no [Type EudraCT No] ACTIVE IMP(s): [Insert trial medication] PLACEBO IMP(s): [Insert trial medication] If Applicable Phase of trial Phase [Insert phase of trial] Sites(s) [Single site]/[Multi-site] Delete as appropriate UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 1 of 39 D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Chief investigator: Page 2 of 39 Sponsor Representative: [Insert name, title, address and contact details] Insert Name/ email address – JRO to Add Joint UCLH/UCL Biomedical Research Unit, 1st Floor Maple House, 149 Tottenham Court Road, London W1T 7NF. Postal address: Joint Research Office, UCL (1st Floor, Maple House), Ground Floor, Rosenheim Wing, 25 Grafton Way, London WC1E 6DB. UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 2 of 39 D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Page 3 of 39 Signatures The Chief Investigator and the JRO have discussed this protocol. The investigators agree to perform the investigations and to abide by this protocol The investigator agrees to conduct the trial in compliance with the approved protocol, EU GCP and UK Regulations for CTIMPs (SI 2004/1031; as amended), the UK Data Protection Act (1998), the Trust Information Governance Policy (or other local equivalent), the Research Governance Framework (2005’ 2nd Edition; as amended), the Sponsor’s SOPs, and other regulatory requirements as amended. Chief investigator [Insert name of CI] Signature Date Signature Date Sponsor Representative JRO to Add UCL This Protocol template is intended for use with UK sites only. UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 3 of 39 D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Page 4 of 39 Contents Signatures ............................................................................................................................. 3 Contents ................................................................................................................................ 4 List of abbreviations ............................................................................................................... 7 1 Trial personnel .............................................................................................................. 9 2 Summary..................................................................................................................... 10 3 Introduction ................................................................................................................. 11 3.1 Background .................................................................................................... 11 3.2 Preclinical data ............................................................................................... 11 3.3 Clinical data .................................................................................................... 11 3.4 Rationale and risks/benefits ........................................................................... 11 3.5 Assessment and management of risk............................................................ 12 4 Objectives ................................................................................................................... 12 5 Trial design ................................................................................................................. 12 Overall design ................................................................................................ 12 5.1 6 Selection of Subjects ................................................................................................... 13 6.1 Inclusion criteria ............................................................................................. 13 6.2 Exclusion criteria ............................................................................................ 13 7 Recruitment................................................................................................................. 14 8 Study procedures and schedule of assessments......................................................... 14 8.1 Informed consent procedure .......................................................................... 14 8.2 Randomisation procedures ............................................................................ 15 8.3 Unblinding....................................................................................................... 15 8.4 Screening Period ............................................................................................ 17 8.5 Baseline assessments ................................................................................... 18 8.6 Treatment procedures .................................................................................... 18 8.7 Subsequent assessments .............................................................................. 18 8.8 Flowchart of study assessments .................................................................... 19 8.9 Methods .......................................................................................................... 19 8.9.1 Laboratory procedures ............................................................................. 19 8.10 Definition of end of trial .................................................................................. 19 UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 4 of 39 Short title: Sponsor code: [Type sponsor protocol number] D:\612869192.doc 8.11 9 Page 5 of 39 Discontinuation/withdrawal of participants and ‘stopping rules’ .................... 19 Name and description of all drugs used in the trial ...................................................... 19 9.1 Treatment of subjects ..................................................................................... 20 9.2 Concomitant medication................................................................................. 20 10 Investigational Medicinal Product ................................................................................ 20 10.1 Name and description of investigational medicinal product(s)Error! Bookmark not defined. 10.2 Name and description of each NIMP ............. Error! Bookmark not defined. 10.3 Summary of findings from non-clinical studies .............................................. 22 10.4 Summary of findings from clinical studies ..................................................... 22 10.5 Summary of known and potential risks and benefits ..................................... 22 10.6 Description and justification of route of administration and dosage .............. 22 10.7 Dosages, dosage modifications and method of administration..................... 22 10.8 Preparation and labelling of Investigational Medicinal Product..................... 22 10.9 Drug accountability ......................................................................................... 22 10.10 Source of IMPs including placebo ....................................................................... 23 10.11 Dose modifications ......................................................................................... 23 10.12 Assessment of compliance ............................................................................ 23 10.13 Post-trial IMP arrangements .......................................................................... 24 11 Recording and reporting of adverse events and reactions ........................................... 24 11.1 Definitions ....................................................................................................... 24 11.2 Recording adverse events ............................................................................. 25 11.4 Procedures for recording and reporting Serious Adverse Events ................. 27 11.4.1 Notification of deaths ................................................................................... 29 11.4.2 Reporting SUSARs ...................................................................................... 29 11.4.3 Development Safety Update Reports ....................................................... 29 11.4.4 Annual progress reports........................................................................... 30 11.4.5 Pregnancy (If applicable) ......................................................................... 30 11.4.6 Overdose ................................................................................................. 30 11.4.7 Reporting Urgent Safety Measures .......................................................... 30 11.5 The type and duration of the follow-up of subjects after adverse events…… 31 11.5.1 Notification of Serious Breaches to GCP and/or the protocol (SPON/S15) .... 31 12 Data management and quality assurance ................................................................... 31 UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 5 of 39 D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Page 6 of 39 12.1 Confidentiality ................................................................................................. 31 12.2 Data collection tools and source document identification ............................. 32 12.3 Data handling and analysis ............................................................................ 32 13 Record keeping and archiving ..................................................................................... 33 14 Statistical Considerations ............................................................................................ 33 14.1 Outcomes ....................................................................................................... 34 14.1.1 Primary outcomes .................................................................................... 34 14.1.2 Secondary outcomes ............................................................................... 34 14.2 Sample size and recruitment ......................................................................... 34 14.2.1 Sample size calculation ........................................................................... 34 14.2.2 Planned recruitment rate.......................................................................... 35 14.3 Statistical analysis plan .................................................................................. 35 14.3.1 Summary of baseline data and flow of patients ........................................ 35 14.3.2 Primary outcome analysis ....................................................................... 35 14.3.3 Secondary outcome analysis ................................................................... 35 14.3.4 Sensitivity and other planned analyses .................................................... 36 14.4 Randomisation methods ................................................................................ 36 14.5 Interim analysis .............................................................................................. 36 14.6 Other statistical considerations ...................................................................... 37 15 Name of Committees involved in trial .......................................................................... 37 16 Direct Access to Source Data/Documents ................................................................... 37 17 Ethics and regulatory requirements ............................................................................. 37 18 Monitoring requirement for the trial .............................................................................. 38 19 Finance ....................................................................................................................... 38 20 Insurance .................................................................................................................... 38 21 Publication policy ........................................................................................................ 39 22 Statement of compliance ............................................................................................. 39 23 References.................................................................................................................. 39 UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 6 of 39 D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Page 7 of 39 List of abbreviations Commonly used abbreviations – add or delete as applicable: AE Adverse Event AR Adverse Reaction CA Competent Authority CI Chief Investigator CRF Case Report Form CRO Contract Research Organisation CTA Clinical Trial Authorisation CTIMP Clinical Trial of Investigational Medicinal Product DMC Data Monitoring Committee DSUR Development Safety Update Report EC European Commission EMEA European Medicines Agency EU European Union EUCTD European Clinical Trials Directive EudraCT European Clinical Trials Database EudraVIGILANCE European database for Pharmacovigilance GAfREC Governance Arrangements for NHS Research Ethics GCP Good Clinical Practice GMP Good Manufacturing Practice IB Investigator Brochure ICF Informed Consent Form IDMC Independent Data Monitoring Committee IMP Investigational Medicinal Product IMPD Investigational Medicinal Product Dossier ISF Investigator Site File ISRCTN International Standard Randomised MA Marketing Authorisation MHRA Medicines and Healthcare products Regulatory Agency UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 7 of 39 D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Page 8 of 39 MS Member State Main REC Main Research Ethics Committee NHS R&D National Health Development PI Principal Investigator PIS Participant Information Sheet QA Quality Assurance QC Quality Control QP Qualified Person for release of trial drug RCT Randomised Control Trial REC Research Ethics Committee SAR Serious Adverse Reaction SAE Serious Adverse Event SDV Source Document Verification SOP Standard Operating Procedure SmPC Summary of Product Characteristics SSA Site Specific Assessment SUSAR Suspected Reaction TMG Trial Management Group TSC Trial Steering Committee UCL Protocol template V2, 27/01/2012 Service Unexpected Research Serious Adverse Version [version no] [Insert date as DD/MMM/YYYY] Page 8 of 39 & D:\612869192.doc 1 Short title: Sponsor code: [Type sponsor protocol number] Page 9 of 39 Trial personnel Chief Investigator (CI) [insert name and address] e-mail: [add email address] tel: [tel no.] fax: [fax no.] Sponsor’s representative [insert name and address] e-mail: [add email address] tel: [tel no.] fax: [fax no.] Statistician [insert name and address] e-mail: [add email address] tel: [tel no.] fax: [fax no.] Central laboratories [insert name and address] e-mail: [add email address] tel: [tel no.] fax: [fax no.] Add appropriate name (eg Head of Department) and address of any central core services i.e laboratories, medical and/or technical departments (e.g. imaging, radiology), and any external Contract Research Organisation (CRO) or Clinical Trials Unit (CTU) involved in the trial. UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 9 of 39 Short title: Sponsor code: [Type sponsor protocol number] D:\612869192.doc 2 Page 10 of 39 Summary This summary should be 1–2 pages only. It should give the reader sufficient information to understand the rationale for the trial, its objectives and the methods that will be used to achieve these objectives. Title: Short title: Trial medication: List all IMPs to be used in the trial. (including Placebo is applicable) Phase of trial: Insert development phase (I, II, II or IV). Objectives: Summarise primary and secondary objectives. Type of trial: Example: Phase [N], open/single-blind/double-blind, randomised, crossover/partial crossover/parallel group, single/multi-site trial in [insert patient population]. Trial design and methods: Give brief summary of trial design, including dosing regime and the assessments that will be made to achieve the primary and secondary objectives. Trial duration per ie. from consent to last trial assessment. trial I.e. from when first patient enrolled to last patient follow-up. participant: Estimated total duration: Planned trial sites: Single-site or multi-site. If multi-site, include number of planned sites. Total number of Include planned number to be enrolled for the whole trial. participants planned: Main inclusion/exclusion Include the main disease/area to be investigated and the key criteria: inclusion/exclusion criteria. Statistical methodology Briefly describe the statistical methodology to be used in the and analysis: study. UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 10 of 39 D:\612869192.doc 3 Short title: Sponsor code: [Type sponsor protocol number] Page 11 of 39 Introduction 3.1 Background This section should describe: The disease to be studied in the trial, including its incidence. The trial population. 3.2 Preclinical data Add in any preclinical/non clinical studies and finding undertaken in summary form. Please cross refer to IMPD/IB/SPC. 3.3 Clinical data Previous clinical trials conducted/ or clinical use of the IMP (or where relevant inference to a similar class of medicine) in support for this clinical trial 3.4 Rationale and risks/benefits Include the rationale or “problem statement” i.e. the research question (the hypothesis to be tested). The current available treatment(s) and their limitations, and why you think the IMP(s) might be an improvement on those treatments. If the IMP(s) is to be used outside its licence, you should include a risk/benefit analysis. Justification should be provided to support that the IMP could achieve clinical improvement over current practice (and indicate its relevance to healthcare practice). This justification is particularly important if the trial proposes to use the IMP: in children or in adults unable to consent for themselves; in higher doses; for longer duration; in a subject population that might handle it differently (e.g. hepatic or renally impaired patients, children, elderly, immunocompromised); it is being used in combination with another medicinal product; or the indication/ medical condition compromises the subject’s tolerance. UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 11 of 39 D:\612869192.doc 3.5 Short title: Sponsor code: [Type sponsor protocol number] Page 12 of 39 Assessment and management of risk Include a section on risk management. What are the risks, how high is the risk compared to normal standard practice and how will risk be minimised? Consider the starting dose, dose increments, administration of doses, resources available particularly in terms of facilities and staff, procedures, type of patients, staff training required. Please refer to the following documentation is preparing this section: http://www.mhra.gov.uk/home/groups/l-ctu/documents/websiteresources/con111784.pdf This trial is categorised as: (delete as appropriate) • Type A = No higher than the risk of standard medical care • Type B = Somewhat higher than the risk of standard medical care • Type C = Markedly higher than the risk of standard medical care 4 Objectives Primary: Secondary: 5 Trial design 5.1 Overall design This section of the protocol should include the following information: Purpose of research (e.g. non commercial trial, licensing). Clear description and justification of the type of design (e.g. open label, blind, parallel group, crossover, placebo-controlled, sequential, cluster randomised and equivalence). If Applicable Include detail and justification for: o level of blinding to be used – double-blind or single-blind o how blinding of investigator team and participant will be implemented (e.g. through use of active and matching placebo treatment) UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 12 of 39 D:\612869192.doc 6 Short title: Sponsor code: [Type sponsor protocol number] Page 13 of 39 For a trial with a crossover design, information about possible carry over effects, detail of treatment ordering, washout (/in) periods. Schematic diagram(s) of overall trial design. Description and justification of the duration of treatment, subject participation and trial follow-up. Criteria for dose escalation if applicable. Selection of Subjects Please consider each criterion carefully as there must be NO deviations from it during the trial. You are defining these criteria and you are expected to comply with them. You need to know which document you will use to assess compliance with the criteria. These criteria need to be defined in such a way that a monitor/inspector can clearly identify from the CRF and medical notes that the CI is compliant with the eligibility criteria. Please add criteria as appropriate (for example, consider contra-indications to trial treatments, incompatible concurrent treatments, recent involvement in other research), and include points below if appropriate: 6.1 Inclusion criteria 1. Age 2. Gender 3. Clinical Parameters. Compliance with EACH parameter for each subject will need to be clearly documented. 6.2 Exclusion criteria 1. Females of childbearing potential and males must be willing to use an effective method of contraception (hormonal or barrier method of birth control; abstinence) from the time consent is signed until 6 weeks after treatment discontinuation. [If the SmPCs of the IMPs state that the IMPs are not teratogenic you might be able to state that this is NA for your trial]. Please note that the MHRA advise double contraception 2. Females of childbearing potential must have a negative pregnancy test within 7 days prior to being registered for trial treatment. [If the SmPCs of the IMPs state that the IMPs are not teratogenic you might be able to state that this is NA for your trial]. NOTE: Subjects are considered not of child bearing potential if they are surgically sterile (i.e. they have UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 13 of 39 Short title: Sponsor code: [Type sponsor protocol number] Page 14 of 39 undergone a hysterectomy, bilateral tubal oophorectomy) or they are postmenopausal. ligation, D:\612869192.doc or bilateral 3. Females must not be breastfeeding. Consider contraindications to trial treatment (e.g. as listed in SmPc), incompatible concurrent treatments, recent involvement in other research. 4. Allergies to excipients of IMP and placebo 7 Recruitment In this section you need to describe recruitment methods such as the use of adverts, websites, PICs (Patient Identification Centres) and the involvement of different centres. 8 Study procedures and schedule of assessments 8.1 Informed consent procedure Specify who will take informed consent, how and when it will be taken. Informed consent must be obtained before any trial-related procedures are completed. The person taking consent must be GCP trained, suitably qualified and experienced, and have been delegated this duty by the CI/PI on the delegation log. Please include if applicable: It is the responsibility of the Investigator, or a person delegated by the Investigator to obtain written informed consent from each subject prior to participation in the trial, following adequate explanation of the aims, methods, anticipated benefits and potential hazards of the study. “Adequate time” must be given for consideration by the patient before taking part. The PI must record when the patient information sheet (PIS) has been given to the patient. [If the amount of time between the PIS being given and the date of consent is less than 24 hours, the PI needs to explain the rationale for this]. The Investigator or designee will explain the patients are under no obligation to enter the trial and that they can withdraw at any time during the trial, without having to give a reason. No clinical trial procedures will be conducted prior to taking consent from the participant. Consent will not denote enrolment into trial. UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 14 of 39 D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Page 15 of 39 A copy of the signed Informed Consent form will be given to the participant. The original signed form will be retained at the study site and a copy placed in the medical notes. If new safety information results in significant changes in the risk/benefit assessment, the consent form will be reviewed and updated if necessary and subjects will be re-consented as appropriate If the trial is in children or adults unable to consent for themselves please include appropriate procedure. Refer to NRES website (http://www.nres.npsa.nhs.uk/applications/guidance/). 8.2 Randomisation procedures We strongly advise that for double blind trials, you enlist the service of a CTU or a specialist company (e.g. www.sealedenvelope.co.uk) to do randomisation, unblinding as they can offer 24/7 cover. You should cost for this in your grant application. Describe the type of randomisation to be used e.g. simple, block, stratified, minimisation. Refer to specific statistics section for more details if applicable. Include information regarding how randomisation will be implemented (include who will be doing it, where and how including the procedure to be used out of hours if applicable). Specify who will hold the randomisation list. Describe how subjects will be assigned to treatment groups e.g. through consecutive allocation of subject numbers, and the use of a Trial Subject Log. You should ensure to have a clear process on randomisation taking into consideration interaction between single centre and/or multicentre trials Describe the procedure for replacements. Describe the approach to be used to conceal allocation (e.g. sealed envelopes, telephone central allocation office). 8.3 Unblinding Specify the procedure(s) to be used for un-blinding for the following situations: Emergency Unblinding The study code should only be broken for valid medical or safety reasons e.g. in the case of a severe adverse event where it is necessary for the investigator or treating health care professional to know which treatment the patient is receiving before the participant can be treated. Subject always to clinical need, where possible, members of the research team should remain blinded. UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 15 of 39 D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Page 16 of 39 The code breaks for the trial are held [please add relevant department] and are the responsibility of [please add personnel]. In the event a code is required to be unblinded a formal request for unblinding will be made by the Investigator/treating health care professional. If the person requiring the unblinding is a member of the Investigating team then a request to the holder of the code break envelope/list, or their delegate will be made and the unblinded information obtained. If the person requiring the unblinding is not the CI/PI then that health care professional will notify the Investigating team that an unblinding is required for a trial subject and an assessment to unblind should be made in consultation with the clinical and research teams. On receipt of the treatment allocation details the CI/PI or treating health care professional will deal with the participant’s medical emergency as appropriate. The CI/PI documents the breaking of the code and the reasons for doing so on the CRF/data collection tool, in the site file and medical notes. It will also be documented at the end of the study in any final study report and/or statistical report. The CI/Investigating team will notify the JRO (acting on behalf of the Sponsor) in writing as soon as possible following the code break detailing the necessity of the code break. The CI/PI will also notify the relevant authorities. [Delete as appropriate] The written information will be disseminated to the Data Safety Monitoring Committee for review in accordance with the DSMC Charter. Unblinding for the submission of SUSAR reports: Amend as appropriate. The following procedure will be used to unblind for the submission of a SUSAR report to the regulatory agencies. A member of the JRO sponsor’s office will contact the pharmacy via telephone on ____________ in the first instance, requesting unblinding information from the randomisation list. The pharmacist will provide their email address and name for the request to be formalised in an email. The Sponsor will provide in the email the protocol number and trial name, name of the requester, reason for unblinding, patient name, subject name and timeline to receive the unblinded information. The Sponsor will provide the unblinded information on the e-SUSAR website form and CIOMS form if applicable. UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 16 of 39 D:\612869192.doc 8.4 Short title: Sponsor code: [Type sponsor protocol number] Page 17 of 39 This information will not be forwarded to the trial team and kept in the JRO site TMF. Screening Period Need to list all the planned screening assessments, including Physical Examination, Medical History and Concomitant Medication. Any assessments and or procedures performed as part of routine care which will be used to screen patients for eligibility will require defined timelines (e.g x-rays within the last 6 months). If applicable you may wish to define time period for overall screening i.e. screening has to be completed within 28 days. a. Baseline visit will occur 28 days of Screening visit b. During treatment phase, visits should occur +/- x days of the scheduled date. c. Follow up period should be 21 days after Visit 7 or Early Discontinuation visit. d. Randomisation is the last procedure to be completed at Baseline visit. e. Routine tests used to determine eligibility criteria as defined in Inclusion/Exclusion criteria Please note screening does not necessarily constitute enrolment. Screen failures i.e. patients who do not meet eligibility criteria at time of screening maybe eligible for rescreening subject to acceptable parameters. This will need to be discussed with the Sponsor. UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 17 of 39 D:\612869192.doc 8.5 Short title: Sponsor code: [Type sponsor protocol number] Page 18 of 39 Baseline assessments Need to list all the planned baseline assessments that will be performed once the patient has been entered into the trial and before their first dose of the IMP. Visit # Screening Baseline a 1 2 Day – X Day-1 Informed Consent X Medical History/Physical exam X X Vital Signs X X Eligibility determination Add ALL Protocol Assessments including bloods/urine etc as applicable both trial specific and routinee Treatment Phase b Follow Up c 3 4 5 6 7 8 Day 0 Week 4 Week 6 Week 8 Week 10 / Early Discontinuation visit F-UP X X X Randomisation d X IMP administration Adverse Events review Concomitant Medication review Physician’s Withdrawal Checklist X X X X X X X X X X X X X X 8.6 Treatment procedures Add IMP dosing details. 8.7 Subsequent assessments Describe all study procedures and assessments, including those that are part of routine care. Breakdown into visit numbers as appropriate. If home dosing, compliance should be checked at each visit. Diary cards should be checked at each visit. Include any follow-up assessments. UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 18 of 39 D:\612869192.doc 8.8 Short title: Sponsor code: [Type sponsor protocol number] Page 19 of 39 Flowchart of study assessments Add table of all procedures/tests/IMP administration to be completed at each visit. 8.9 8.9.1 Methods Laboratory procedures The following samples will be processed at Local Labs: The following samples will be processed at Central Labs: (delete as appropriate) Please obtain accreditation certificate and ref ranges. For any specialist sample handling, processing and or shipment please refer to lab manual. 8.10 Definition of end of trial Define the end of the trial. In most cases the end of the trial will be the date of the last visit/ telephone follow up/ home visit by the last participant. Any exceptions should be justified. 8.11 Discontinuation/withdrawal of participants and ‘stopping rules’ The protocol should: describe under what circumstances and how subjects will be withdrawn from the trial give details of documentation to be completed on subject withdrawal (including recording reasons for withdrawal and any follow-up information collected with timing) state whether withdrawn subjects would be replaced and how. state under what circumstances the trial might be prematurely stopped. Remember the safety profile of the IMP(s) and the objective(s) of the trial. It may be necessary to give the circumstances under which treatment may be resumed. 9 Name and description of all drugs used in the trial For this section of the protocol you might find the following document useful to read: “Guidance on Investigational Medicinal Products (IMPs) and other medicinal products used in Clinical Trials” UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 19 of 39 D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Page 20 of 39 This document can be downloaded at: http://ec.europa.eu/enterprise/pharmaceuticals/eudralex/vol-10/guidance-onimp_nimp_04-2007.pdf This section of the protocol should list all the drugs to be used in the trial. 9.1 Treatment of subjects Investigational product/treatment Please give a description of the intervention (medicinal product, medical device, food supplement, radiation, surgery, behavioural interventions, etc). Also use of comparator or placebo should be described If the trial uses a licensed drug, specify the generic name only, unless a specific brand must be used, for example as per an IMP supply agreement (e.g. if IMP is to be supplied free of charge by the manufacturer). Also, please add statement that any brand of the IMP can be used, if that is the case. 9.2 Concomitant medication Medication(s)/treatment(s) permitted and not permitted before and/or during the trial (specify time restrictions). Consider possible interactions or effects that could confound the results and conclusions. Please do not confuse this with NIMPs, refer to section 9.9 for further details 10 Investigational Medicinal Product According to the definition of the EU clinical trial directive 2001/20/EC, an investigational medicinal product is a pharmaceutical form of an active substance or placebo being tested or used as a reference in a clinical trial, including products already with a marketing authorisation, but used or assembled (formulated or packaged) in a way different from the authorised form, or when used for an unauthorised indication, or when used to gain further information about the authorised form. Thus in this section also information about the comparator product/placebo should be given. UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 20 of 39 D:\612869192.doc 10.1 Short title: Sponsor code: [Type sponsor protocol number] Page 21 of 39 Name and description of investigational medicinal product(s) Please refer to the following guidance for classification of IMPs: http://ec.europa.eu/health/files/pharmacos/docs/doc2006/07_2006/def_imp_ 2006_07_27_en.pdf The description of IMP should de proportional to the development status of the IMP (e.g. for marketed products reference to the authorized medicinal product with at least details of strength dosage form and PL holder should be given, for new or modified products a full although concise description should be given 10.2 Name and description of each NIMP Please refer to the following guidance for classification of NIMPs: http://ec.europa.eu/health/files/pharmacos/docs/doc2006/07_2006/def_imp_ 2006_07_27_en.pdf A similar system to that required for IMPs needs to be implemented if the NIMPS are unlicensed (i.e might come from another EU country or a country outside EEA) In all other cases • Host sites are responsible to maintain a system which allows adequate reconstruction of NIMP movements there should be a procedure that permit recording which patients received which NIMPs during the trial with an evaluation of the compliance. (Delete the previous sentence if the text in blue is applicable) Eg. Rescue medication (if applicable) Please describe type, dose per unit and maximum dose allowed 10.3 Summary of findings from non-clinical studies UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 21 of 39 D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Page 22 of 39 Please refer to the Investigator’s Brochure (IB), Investigational Medicinal Product Dossier (IMPD), Summary of Product Characteristics (SPC) or a similar document (if applicable), by mentioning the relevant pages in that document. Be sure that the information is up to date and references to peer reviewed papers in (biomedical/scientific) journals should be given where appropriate.> 10.4 Summary of findings from clinical studies See explanatory text of chapter 10.2 10.5 Summary of known and potential risks and benefits See explanatory text of chapter 10.2 10.6 Description and justification of route of administration and dosage Also should be included technical modalities if applicable (i.e if the product is to be given in a syringe and is a powder and needs to be reconstituted, this should be described here 10.7 Dosages, dosage modifications and method of administration This section should be precise and complete. Remember to include dosage for all subjects throughout the trial period, taking particular care to changes doses as infants and children grow. You should include the frequency and timing of dose in each part of the trial, methods for individualised doses, etc. 10.8 Preparation and labelling of Investigational Medicinal Product Preparation and labelling of the investigational medicinal products should be completed in accordance with the relevant GMP guidelines. Text for labels used for the Investigational Medicinal may be obtained by the IMP compliance Manager 10.9 Drug accountability Please describe the procedures for the shipment, receipt, distribution, return and destruction of the investigational medicinal products. 10.10 Source of IMPs including placebo If the IMPs to be used in the trial are being provided or manufactured by a company specifically for use in the trial please provide details of the UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 22 of 39 D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Page 23 of 39 arrangement. If the IMPs are being sourced from hospital stock please insert the following statement, and list the IMPs as applicable: ‘The following IMPs will be sourced from routine hospital stock and their handling and management will be subject to standard procedures of the pharmacy’. Sourcing of IMP is also discussed in the IMP management plan. 10.11 Dose modifications You should give details here on required dose modifications if applicable, for example in the case of certain adverse events (specify the exact dose modifications and events), and also the stopping rules (see also section 8.11). 10.12 Assessment of compliance Compliance includes both adherences to IMP and Protocol study procedures. Percentage of noncompliance acceptable for patient to continue on the trial is: e.g. <80% noncompliance equates to patient withdrawal (this includes compliance with IMP and study procedures i.e. visit window, refusal of study specific assessments) Percentage of IMP compliance acceptable for patient to continue on the trial is (insert percentage): Noncompliance to the Protocol study procedures will be documented by the investigator and reported to the Sponsor as agreed. Persistent noncompliance may lead the patient to be withdrawn from the study. Define procedures for: Monitoring (e.g. watching subject swallow pills and checking their mouth afterwards, getting patients to complete a diary card, package returns). Recording of subject compliance information (what will be recorded, when and where). Details of follow-up of non-compliant subjects. 10.13 Post-trial IMP arrangements Describe what arrangements are in place should the IMP be provided to trial subjects post trial participation. If there are not arrangements then you need to state that there will be no arrangements. UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 23 of 39 D:\612869192.doc 11 Short title: Sponsor code: [Type sponsor protocol number] Page 24 of 39 Recording and reporting of adverse events and reactions Under this section, the protocol needs to include the following definitions: 11.1 Definitions Term Definition Adverse Event (AE) Any untoward medical occurrence in a patient or clinical trial subject administered a medicinal product and which does not necessarily have a causal relationship with this treatment. Adverse (AR) Reaction Any untoward and unintended response in a subject to an investigational medicinal product which is related to any dose administered to that subject. This includes medication errors, uses outside of protocol (including misuse and abuse of product) Serious adverse event (SAE), serious adverse reaction (SAR) or unexpected serious adverse reaction Any adverse event, adverse reaction or unexpected adverse reaction, respectively, that: results in death, is life-threatening, requires hospitalisation or prolongation of existing hospitalisation, results in persistent or significant disability or incapacity, or consists of a congenital anomaly or birth defect Important Medical Event These events may jeopardise the subject or may require an intervention to prevent one of the above characteristics/consequences. Such events should also be considered ‘serious’. Unexpected adverse reaction An adverse reaction the nature and severity of which is not consistent with the information about the medicinal product in question set out: (a) in the case of a product with a marketing authorization, in the summary of product characteristics for that product, (b) in the case of any other investigational medicinal product, in the investigator's brochure relating to the trial in question. UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 24 of 39 D:\612869192.doc SUSAR Short title: Sponsor code: [Type sponsor protocol number] Page 25 of 39 Suspected Unexpected Serious Adverse Reaction 11.2 Recording adverse events All adverse events will be recorded in the medical records and CRF following consent. Those trials whereby nIMPs or trial specific procedures are administered prior to the IMP administration, adverse events will be required to be recorded. (Reporting of AEs normally occurs following IMP administration if AE data is collected before it should be recorded in the CRF, medical notes and AE log but not reported to the sponsor). (Please amend as appropriate). If you do not plan to record certain adverse events in the CRF (for example, if your trial is a phase IV trial of a licensed medication used within its license with a well-established safety profile) please state it here and provide justification. However, all SERIOUS adverse events must be recorded in the CRF and SAE log. If the investigator suspects that the subjects’ disease has progressed faster due to the administration of the IMP, then he will record and report this as an unexpected adverse event. Clinically significant abnormalities in the results of objective tests (e.g. laboratory variables, x-ray, ECG – make specific to trial) will also be recorded as adverse events. If the results are not expected as part of disease or IMP, these will also be recorded as unexpected. (Delete if inappropriate to trial) All adverse events will be recorded with clinical symptoms and accompanied with a simple, brief description of the event, including dates as appropriate. All adverse events will be recorded until (insert as appropriate) All adverse events will be reportable to the Sponsor up to 30 days post last IMP administration. (Amend as appropriate) UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 25 of 39 D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Page 26 of 39 11.3 Assessments of Adverse Events Each adverse event will be assessed for the following criteria: 11.3.1 Severity Category Definition Mild The adverse event does not interfere with the volunteer’s daily routine, and does not require intervention; it causes slight discomfort Moderate The adverse event interferes with some aspects of the volunteer’s routine, or requires intervention, but is not damaging to health; it causes moderate discomfort Severe The adverse event results in alteration, discomfort or disability which is clearly damaging to health 11.3.2 Causality The assessment of relationship of adverse events to the administration of IMP is a clinical decision based on all available information at the time of the completion of the case report form. The following categories will be used to define the causality of the adverse event: Category Definition Definitely: There is clear evidence to suggest a causal relationship, and other possible contributing factors can be ruled out. Probably: There is evidence to suggest a causal relationship, and the influence of other factors is unlikely Possibly There is some evidence to suggest a causal relationship (e.g. the event occurred within a reasonable time after administration of the trial medication). However, the influence of other factors may have contributed to the event (e.g. the patient’s clinical condition, other concomitant events). Unlikely There is little evidence to suggest there is a causal relationship (e.g. the event did not occur within a reasonable time after administration of the trial medication). There is another reasonable explanation for the event (e.g. the patient’s clinical condition, other concomitant treatments). UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 26 of 39 D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Page 27 of 39 Not related There is no evidence of any causal relationship. Not Assessable Unable to assess on information available. 11.3.3 Expectedness Category Definition Expected An adverse event that is classed in nature as serious and which is consistent with the information about the IMP listed in the Investigator Brochure (or SmPC if Licensed IMP) or clearly defined in this protocol. Unexpected An adverse event that is classed in nature as serious and which is not consistent with the information about the IMP listed in the Investigator Brochure (or SmPC if Licensed IMP) The reference document to be used to assess expectedness against the IMP is (add in either SPC/IB). The protocol will be used as the reference document to assess disease related and/or procedural expected events. 11.3.4 Seriousness Seriousness as defined for an SAE in section 11.1. Collection, recording and reporting of adverse events (including serious and non-serious events and reactions) to the sponsor will be completed according to the sponsor’s SOP(INV/S05). 11.4 Procedures for recording and reporting Serious Adverse Events All serious adverse events will be recorded in the hospital notes and the CRF, and the sponsor’s SAE log. The SAE log will be reported to the sponsor at least once or twice per year (amend as appropriate) All serious adverse events will need to be reported to the sponsor on a SAE form unless stated in the protocol that some expected SAEs will not be reported to the sponsor, with a justification as to why they will not be reported. For patients on the control arm of a trial, SAEs may not have to be reported to the sponsor but will be recorded in the CRF and medical records. UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 27 of 39 D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Page 28 of 39 The Chief or Principal Investigator will complete the sponsor’s serious adverse event form and the form will be faxed to the sponsor on 020 3108 2312, within one working day of his / her becoming aware of the event. The Chief or Principal Investigator will respond to any SAE queries raised by the sponsor as soon as possible. You may choose not to report EXPECTED SAEs to the sponsor for example if they are expected to occur on a regular basis and offer no further new information to your safety profile e.g. neutropenic sepsis. These events must continue to be recorded in the source data and CRF, however you may state that you will not complete an SAE form and forward it to the sponsor. Please provide the rationale for doing so. All SUSARs must be notified to the sponsor immediately (or at least within one working day) according to the sponsor’s written SOP. Example of exception: Example: As the IMPs used in this trial are licensed in the UK and used within their marketing authorization, EXPECTED SARs (as outlined in the SmPCs and listed below – please list) will be RECORDED in the subjects’ hospital notes and in the CRF. However, SAE forms will not be completed and sent to the sponsor. It is important to note that the SmPC will only refer to reactions that are expected to occur in the indication for which the drug has a marketing authorisation. Please document which version of the SmPC is being referenced but add that the most up-to-date version of the SmPc will be used during the trial. Managing serious adverse events in a multi-centre trial The protocol needs to have clear instructions for the reporting lines and timeframe for serious adverse events. These instructions will need to include where the investigator (PI) will send the reports to: e.g. if the PI sends the report directly to the sponsor, or whether the CI reviews the report first before it is notified to the sponsor and how safety information will be disseminated to all other PI sites. Reporting to the sponsor will be completed as per the sponsor’s SOP and using the UCL SAE form (INV/S05). 11.4.1 Notification of deaths The protocol needs to be explicit as to whether, how and when the chief investigator will notify deaths (expected or unexpected) to the sponsor. The following statements are examples of what needs to be stated in the protocol: UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 28 of 39 D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Page 29 of 39 “All deaths will be reported to the sponsor irrespective of whether the death is related to disease progression, the IMP, or an unrelated event”. This statement should be used for phase I/FTIM trials. “Only deaths that are assessed to be caused by the IMP will be reported to the sponsor. This report will be immediate”. “All deaths, including deaths deemed unrelated to the IMP, if they occur earlier than expected will be reported to the sponsor”. The protocol needs to specify the timelines of such reports. 11.4.2 Reporting SUSARs The sponsor will notify the main REC and MHRA of all SUSARs. SUSARs that are fatal or life-threatening must be notified to the MHRA and REC within 7 days after the sponsor has learned of them. Other SUSARs must be reported to the REC and MHRA within 15 days after the sponsor has learned of them. In a double-blind trial, the procedure for unblinding in the event of a SUSAR must be described (refer to sponsor’s SOP on randomisation, blinding and code-breaking for more information (INV/S06). 11.4.2.1 Reporting SUSARs in International Trials (include if applicable) The overall sponsor of the trial is responsible for reporting SUSARs which occur outside of the UK to the MHRA. UCL, as sponsor of the UK site only, will report SUSARs occurring in the UK to the MHRA. 11.4.3 Development Safety Update Reports The sponsor will provide the main REC and the MHRA with Development Safety Update Reports (DSUR) which will be written in conjunction with the trial team and the Sponsor’s office. The report will be submitted within 60 days of the Developmental International Birth Date (DIBD) of the trial each year until the trial is declared ended 11.4.4 Annual progress reports An annual progress report (APR) will be submitted to the REC within 30 days of the anniversary date on which the favourable opinion was given, and annually until the trial is declared ended. The chief investigator will prepare the APR. UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 29 of 39 D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Page 30 of 39 11.4.5 Pregnancy (If applicable) Describe the procedure in place to: record and notify pregnancies to the sponsor (use sponsor’s SOP), follow-up of pregnant subject: Describe in detail the process for monitoring and managing a pregnancy. follow-up of child born to a pregnant trial subject, including male trial subject who is the partner of the pregnant woman. (How long will followup be for). 11.4.6 Overdose Describe the procedure in place to: record and notify overdoses to the sponsor (this information should be placed on the deviation log) Where can overdoses be observed from (pill counts, diary cards, drug charts or patient comment) How will it affect you final analysis. Will patients be taken withdrawn from the trial? Consider what will constitute an overdose that warrants trial discontinuation If an SAE is associated with the overdose ensure the overdose if fully described in the SAE report form 11.4.7 Reporting Urgent Safety Measures If any urgent safety measures are taken the PI/Sponsor shall immediately and in any event no later than 3 days from the date the measures are taken, give written notice to the MHRA and the relevant REC of the measures taken and the circumstances giving rise to those measures. Please refer to the following website for details on clinical trials safety reporting: http://www.mhra.gov.uk/Howweregulate/Medicines/Licensingofmedicines/Clin icaltrials/Safetyreporting-SUSARSandASRs/index.htm 11.5 The type and duration of the follow-up of subjects after adverse events. This section needs to describe the type and duration of follow-up care for subjects following an adverse drug reaction. This section of the protocol also needs to specify how long after the last dose of IMP has been administered to the subjects will adverse events and reactions be recorded and reported. UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 30 of 39 D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Page 31 of 39 Please include ‘Any SUSAR related to the IMP will need to be reported to the Sponsor irrespective of how long after IMP administration the reaction has occurred.’ 11.5.1 Notification of Serious Breaches to GCP and/or the protocol (SPON/S15) A “serious breach” is a breach which is likely to effect to a significant degree – (a) the safety or physical or mental integrity of the subjects of the trial; or (b) the scientific value of the trial. The sponsor of a clinical trial shall notify the licensing authority in writing of any serious breach of – (a) the conditions and principles of GCP in connection with that trial; or (b) the protocol relating to that trial, as amended from time to time, within 7 days of becoming aware of that breach. The sponsor will be notified immediately of any case where the above definition applies during the trial conduct phase. The sponsor’s SOP on the ‘Notification of violations, urgent safety measures and serious breaches’ will be followed. 12 Data management and quality assurance 12.1 Confidentiality Include: All data will be handled in accordance with the UK Data Protection Act 1998. The Case Report Forms (CRFs) will not bear the subject’s name or other personal identifiable data. The subject’s initials, date of birth and trial identification number, will be used for identification.’ 12.2 Data collection tools and source document identification Describe procedures for data collection and recording. The protocol must specify which data is to be recorded directly onto the Case Report Form (CRF) and which data is recorded firstly into source documents, such as medical notes and patient questionnaires. If data is not to be recorded in the UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 31 of 39 D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Page 32 of 39 CRF but only recorded in source documents this must be clearly identified. Include a table or list identifying source documentation, and whether or not this is to be transcribed into the CRF. Describe whether the data are from a standardised tool (e.g. McGill pain score) or involves a procedure (in which case full details should be supplied). If a non standard tool is to be used, detail on reliability and validity should be given. The methods used to maximise completeness of data should be described (e.g. telephoning subjects who have not returned postal questionnaires) and data collection forms should be included as appendices. Include statement: ‘It will be the responsibility of the investigator to ensure the accuracy of all data entered in the CRFs. The delegation log will identify all those personnel with responsibilities for data collection and handling, including those who have access to the trial database.’ 12.3 13 Data handling and analysis Describe what software (e.g. Access, MACRO) is to be used for data entry (NB Excel is not a suitable system for data entry in a clinical trial). Provide detailed methods implemented to ensure validity and quality of data (e.g. double entry, cross validation etc) Describe how data will be stored and backed up, and how security will be ensured and whether data will be transferred. If data are to be transferred, describe the secure method of transfer. Document if there is a disaster recovery plan. Consider management of data across sites if multi-site trial. Where data are transferred electronically this must be in accordance with the UK Data Protection Act 1998 as well as UCL Information Security Policy and Trust Information Governance Policy. There should be a documented record of data transfer and measures in place for the recovery of original information after transfer. Statement of who is responsible for data entry and quality, and who is responsible for data analysis. Data analysis should be performed independently of data entry. Record keeping and archiving Archiving will be authorised by the Sponsor following submission of the end of study report. Specify location and duration of record retention for: UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 32 of 39 D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Essential documents the trial database Page 33 of 39 Please include the statement ‘Chief Investigators are responsible for the secure archiving of essential trial documents (for each site, if multi-site trial) and the trial database as per their trust policy. All essential documents will be archived for a minimum of 5 years after completion of trial. Destruction of essential documents will require authorisation from the Sponsor. 14 Statistical Considerations [Insert statistician’s name] is the trial statistician who will be responsible for all statistical aspects of the trial from design through to analysis and dissemination. Please note that the trial statistician should be appropriately qualified and experienced to undertake this work and be a fully engaged member of the research team. If the statistician is not employed by UCL, a contract will need to be put in place. For international trials whereby UCL are the named sponsor for UK sites only, you will need to be explicit within the section below in terms of what information relates to the trial as a whole such as sample size and what relates to the UK sites only (i.e. sample size for the UK sites), and whether the sample size calculation is based on UK sites only or on all sites in all countries involved. 14.1 Outcomes 14.1.1 Primary outcomes A full description of the primary outcome; its definition, when it is measured, any rules, references or programs for calculation of derived values and what form it will take for analysis (e.g. continuous, categorical, ordinal). 14.1.2 Secondary outcomes For each secondary outcome, detail as for primary outcome above. UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 33 of 39 D:\612869192.doc 14.2 Short title: Sponsor code: [Type sponsor protocol number] Page 34 of 39 Sample size and recruitment 14.2.1 Sample size calculation Details of the precision or power calculation used to estimate the required sample size (for analysis of the primary outcome), should contain all information required to reproduce the sample size calculation including: estimates used (e.g. Standard deviation, size of the clinically important effect to be detected, correlations, dropout and noncompliance rates) with relevant justifications in the form of appropriate references, pilot data or clinical arguments. assumptions made (e.g. assumptions of Normality, proportional hazards) allowance for planned subgroup and interim analysis and clustering effects chosen levels of significance and power methods / formula / software used with reference For international multi-centre trials only, if the power of the trial is based on the UK centres only, you must insert the following statement: ‘The power of the trial based on the UK centres alone is x%.’ If x<80%, the following statement should be added as well: ‘Therefore only descriptive analyses will be performed using the UK data. Tests of efficacy of the intervention will only be performed after combining the data with those from the other international centres.’ 14.2.2 Planned recruitment rate An estimate of the recruitment period for the trial (calculated based on the expected number of eligible and recruited participants available per month/year) with justification that the required sample size will be attainable in practice. 14.3 Statistical analysis plan 14.3.1 Summary of baseline data and flow of patients List variables to be used to assess baseline comparability of the randomised groups including for each factor: a definition, any rules, references or programs for calculation of derived values, what form it will take for analysis (e.g. continuous, categorical, ordinal) and how it will be reported (e.g. means, standard deviations, medians, proportions). UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 34 of 39 D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Plans to produce statement.org/), a consort flow Page 35 of 39 diagram (http://www.consort- 14.3.2 Primary outcome analysis Plans for statistical analyses of the primary outcome including: Summary measures to be reported Method of analysis (justified with consideration of form of the data , assumptions of the method and structure of the data (e.g. unpaired, paired, clustered) etc) Plans for handling multiple comparisons, missing data, non-compliers, spurious data and withdrawals in analysis Plans for predefined subgroup analyses Statement regarding use of intention to treat (ITT) analysis Description of any non-statistical methods that might be used (e.g. qualitative methods) 14.3.3 Secondary outcome analysis Plans for statistical analysis of each secondary outcome. Note that use of hypothesis tests may not be appropriate if the study has not been powered to address these and use of estimates with confidence intervals is preferred. Secondary analyses should be considered as hypothesis generating rather than providing firm conclusions. 14.3.4 Sensitivity and other planned analyses A decription of plans for sensitivity and other analyses. For example sensitivity to missing data or non-compliance. Please note that a more detailed statistical analysis plan should be produced as a separate document at some point prior to the final analysis (as recommended by the ICHE9 guidelines). In this document, a more technical and detailed elaboration of the principal features stated in the protocol should be included. The plan may include detailed procedures for executing the statistical analysis of the primary and secondary variables and other data. The plan should be reviewed and possibly updated as a result of the blind review of the data and should be finalised before breaking the blind. Formal records should be kept of when the statistical analysis plan was finalised as well as when the blind was subsequently broken. UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 35 of 39 D:\612869192.doc 14.4 Short title: Sponsor code: [Type sponsor protocol number] Page 36 of 39 Randomisation methods Include detail for each of the following: subject / cluster randomised design (randomising individuals or groups (eg general practices, wards) type of randomisation to be used - simple, block, stratified, minimisation (block size should not be stated in the protocol to maintain blinding) o if using stratified randomisation or minimisation, include definition of stratification/minimisation variables (should only consider variables that are likely to be strongly prognostic of the outcome) o if using blocked randomisation consider varying block sizes. 14.5 use of equal or unequal allocation between treatment arms Interim analysis Detail of approach for interim analyses (e.g. timing and statistical methods) and criteria for early termination of the trial Stopping / discontinuation rules and breaking of randomisation code: 14.6 define completion and premature discontinuation of the trial describe procedure regarding decisions on discontinuation of the trial (e.g. interim analyses, role of data monitoring committee) state documentation to be completed if discontinued describe circumstances under which the randomisation codes may need to be broken and the procedure for this. part / all of the trial is Other statistical considerations Procedures for reporting any deviation(s) from the original statistical plan (any deviation(s) from the original statistical plan should be described and justified in the protocol and/or in the final report, as appropriate). 15 Name of Committees involved in trial Please insert any applicable committees and their remits. Describe which of the three committees will be in place for the trial: Trial Management Group (TMG) (all trials should have a TMG), Independent Data Monitoring Committee (IDMC) and Trial Steering Group (TSC). The terms of UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 36 of 39 D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Page 37 of 39 reference for these committees will need to be provided in separate documents. Please note for ALL phase I trials, an IDMC must be in place prior to trial start up, and the sponsors IDMC charter must be completed and signed off by IDMC members. For Phase I/II trials the safety committee will be asked if an IDMC is required. Each member will need to sign the UCL IDMC charter prior to becoming a member. 16 Direct Access to Source Data/Documents Include the following statement: The investigator(s)/ institution(s) will permit trial-related monitoring, audits, REC review, and regulatory inspection(s), providing direct access to source data/documents. Trial participants are informed of this during the informed consent discussion. Participants will consent to provide access to their medical notes. 17 Ethics and regulatory requirements In this section you need to describe any ethical issues that need to be considered and how these will be addressed. The sponsor will ensure that the trial protocol, patient information sheet, consent form, GP letter and submitted supporting documents have been approved by the appropriate regulatory body (MHRA in UK) and a main research ethics committee, prior to any patient recruitment. The protocol and all agreed substantial protocol amendments, will be documented and submitted for ethical and regulatory approval prior to implementation. If the trial involves the use of radiation, document here if an Administration of Radioactive Substances Advisory Committee (ARSAC) licence is needed. Before the site can enrol patients into the trial, the Chief Investigator/Principal Investigator or designee must apply for NHS permission from their Trust Research & Development (R&D) and be granted written permission. It is the responsibility of the Chief Investigator/ Principal Investigator or designee at each site to ensure that all subsequent amendments gain the necessary approval. This does not affect the individual clinician’s responsibility to take immediate action if thought necessary to protect the health and interest of individual patients (see section 11.4.7 for reporting urgent safety measures). Within 90 days after the end of the trial, the CI/Sponsor will ensure that the main REC and the MHRA are notified that the trial has finished. If the trial is UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 37 of 39 D:\612869192.doc Short title: Sponsor code: [Type sponsor protocol number] Page 38 of 39 terminated prematurely, those reports will be made within 15 days after the end of the trial. The CI will supply the Sponsor with a summary report of the clinical trial, which will then be submitted to the MHRA and main REC within 1 year after the end of the trial. 18 Monitoring requirement for the trial Include the following statement: A Trial specific monitoring plan will be established for studies. The trial will be monitored with the agreed plan. 19 Finance A statement of the finance for the trial such as details of funding body. 20 Insurance Include the following: “University College London holds insurance against claims from participants for injury caused by their participation in the clinical trial. Participants may be able to claim compensation if they can prove that UCL has been negligent. However, as this clinical trial is being carried out in a hospital, the hospital continues to have a duty of care to the participant of the clinical trial. University College London does not accept liability for any breach in the hospital’s duty of care, or any negligence on the part of hospital employees. This applies whether the hospital is an NHS Trust or otherwise. Participants may also be able to claim compensation for injury caused by participation in this clinical trial without the need to prove negligence on the part of University College London or another party. Participants who sustain injury and wish to make a claim for compensation should do so in writing in the first instance to the Chief Investigator, who will pass the claim to the Sponsor’s Insurers, via the Sponsor’s office. Hospitals selected to participate in this clinical trial shall provide clinical negligence insurance cover for harm caused by their employees and a copy of the relevant insurance policy or summary shall be provided to University College London, upon request.” If a medical device is to be used in the trial, there must also be indemnity arrangements in place, with the manutacturer, to cover the malfunction and breakdown of the device. UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 38 of 39 D:\612869192.doc 21 Short title: Sponsor code: [Type sponsor protocol number] Page 39 of 39 Publication policy All proposed publications will be discussed with Sponsor prior to publishing other than those presented at scientific forums/meetings. Please refer to UCL publication policy. 22 Statement of compliance Include the following statement: The trial will be conducted in compliance with the approved protocol, the UK Regulations, EU GCP and the applicable regulatory requirement(s). 23 References List of the literature and data that are relevant to the trial, and that provide background for the trial. Please ensure the text contains appropriate cross references to this list UCL Protocol template V2, 27/01/2012 Version [version no] [Insert date as DD/MMM/YYYY] Page 39 of 39