Rates of Problematic Substance Use and Other Excessive
advertisement
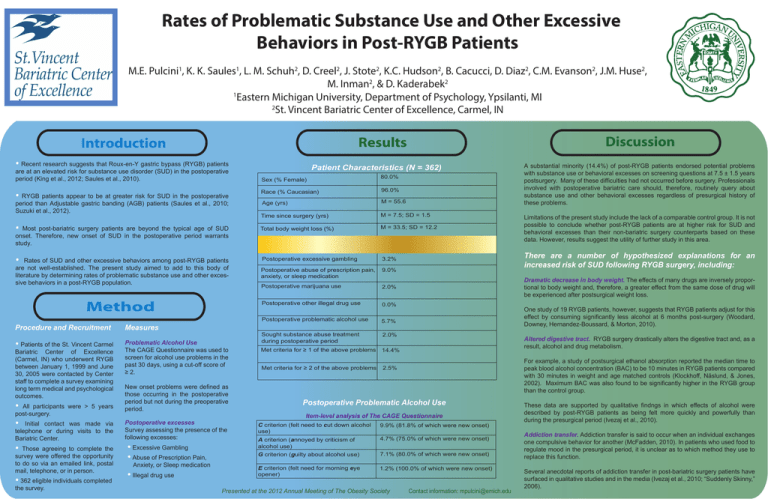
Rates of Problematic Substance Use and Other Excessive Behaviors in Post-RYGB Patients M.E. Pulcini1, K. K. Saules1, L. M. Schuh2, D. Creel2, J. Stote2, K.C. Hudson2, B. Cacucci, D. Diaz2, C.M. Evanson2, J.M. Huse2, M. Inman2, & D. Kaderabek2 1 Eastern Michigan University, Department of Psychology, Ypsilanti, MI 2 St. Vincent Bariatric Center of Excellence, Carmel, IN Discussion Results Introduction • Recent research suggests that Roux-en-Y gastric bypass (RYGB) patients are at an elevated risk for substance use disorder (SUD) in the postoperative period (King et al., 2012; Saules et al., 2010). A substantial minority (14.4%) of post-RYGB patients endorsed potential problems with substance use or behavioral excesses on screening questions at 7.5 ± 1.5 years postsurgery. Many of these difficulties had not occurred before surgery. Professionals involved with postoperative bariatric care should, therefore, routinely query about substance use and other behavioral excesses regardless of presurgical history of these problems. Patient Characteristics (N = 362) Sex (% Female) 80.0% Race (% Caucasian) 96.0% Age (yrs) M = 55.6 Time since surgery (yrs) M = 7.5; SD = 1.5 • Most post-bariatric surgery patients are beyond the typical age of SUD onset. Therefore, new onset of SUD in the postoperative period warrants study. Total body weight loss (%) M = 33.5; SD = 12.2 Limitations of the present study include the lack of a comparable control group. It is not possible to conclude whether post-RYGB patients are at higher risk for SUD and behavioral excesses than their non-bariatric surgery counterparts based on these data. However, results suggest the utility of further study in this area. • Postoperative excessive gambling 3.2% Postoperative abuse of prescription pain, anxiety, or sleep medication 9.0% There are a number of hypothesized explanations for an increased risk of SUD following RYGB surgery, including: Postoperative marijuana use 2.0% Postoperative other illegal drug use 0.0% Postoperative problematic alcohol use 5.7% Sought substance abuse treatment during postoperative period 2.0% Met criteria for ≥ 1 of the above problems 14.4% Met criteria for ≥ 2 of the above problems 2.5% • RYGB patients appear to be at greater risk for SUD in the postoperative period than Adjustable gastric banding (AGB) patients (Saules et al., 2010; Suzuki et al., 2012). Rates of SUD and other excessive behaviors among post-RYGB patients are not well-established. The present study aimed to add to this body of literature by determining rates of problematic substance use and other excessive behaviors in a post-RYGB population. Method Procedure and Recruitment Measures • Problematic Alcohol Use The CAGE Questionnaire was used to screen for alcohol use problems in the past 30 days, using a cut-off score of ≥ 2. Patients of the St. Vincent Carmel Bariatric Center of Excellence (Carmel, IN) who underwent RYGB between January 1, 1999 and June 30, 2005 were contacted by Center staff to complete a survey examining long term medical and psychological outcomes. • All participants were > 5 years post-surgery. • Initial contact was made via telephone or during visits to the Bariatric Center. • Those agreeing to complete the survey were offered the opportunity to do so via an emailed link, postal mail, telephone, or in person. • 362 eligible individuals completed the survey. New onset problems were defined as those occurring in the postoperative period but not during the preoperative period. Postoperative excesses Survey assessing the presence of the following excesses: • Excessive Gambling • Abuse of Prescription Pain, Anxiety, or Sleep medication • Illegal drug use Dramatic decrease in body weight. The effects of many drugs are inversely proportional to body weight and, therefore, a greater effect from the same dose of drug will be experienced after postsurgical weight loss. Following bariatric surgery, patients find themselves abruptly confronted with an inability to eat, but perhaps limited resources for managing food urges through other means, which can create conditions that foster drug and/or alcohol dependence. One study of 19 RYGB patients, however, suggests that RYGB patients adjust for this effect by consuming significantly less alcohol at 6 months post-surgery (Woodard, Downey, Hernandez-Boussard, & Morton, 2010). Altered digestive tract. RYGB surgery drastically alters the digestive tract and, as a result, alcohol and drug metabolism. Following bariatric surgery, patients find themselves abruptly confronted with an inability to eat, but perhaps limited resources for managing food urges through other means, which can create conditions that foster drug and/or alcohol dependence. 9.9% (81.8% of which were new onset) Postoperative Problematic Alcohol Use Item-level analysis of The CAGE Questionnaire C criterion (felt need to cut down alcohol use) 9.9% (81.8% of which were new onset) A criterion (annoyed by criticism of alcohol use) 4.7% (75.0% of which were new onset) G criterion (guilty about alcohol use) 7.1% (80.0% of which were new onset) E criterion (felt need for morning eye opener) 1.2% (100.0% of which were new onset) Presented at the 2012 Annual Meeting of The Obesity Society Contact information: mpulcini@emich.edu For example, a study of postsurgical ethanol absorption reported the median time to peak blood alcohol concentration (BAC) to be 10 minutes in RYGB patients compared with 30 minutes in weight and age matched controls (Klockhoff, Näslund, & Jones, 2002). Maximum BAC was also found to be significantly higher in the RYGB group than the control group. These data are supported by qualitative findngs in which effects of alcohol were described by post-RYGB patients as being felt more quickly and powerfully than during the presurgical period (Ivezaj et al., 2010). Addiction transfer. Addiction transfer is said to occur when an individual exchanges one compulsive behavior for another (McFadden, 2010). In patients who used food to regulate mood in the presurgical period, it is unclear as to which method they use to replace this function. Several anecdotal reports of addiction transfer in post-bariatric surgery patients have surfaced in qualitative studies and in the media (Ivezaj et al., 2010; “Suddenly Skinny,” 2006).