DEVELOPMENT OF A DYNAMIC TEST PHANTOM FOR OPTICAL TOPOGRAPHY
advertisement

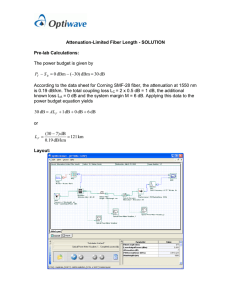
DEVELOPMENT OF A DYNAMIC TEST PHANTOM FOR OPTICAL TOPOGRAPHY Peck H. Koh, Clare E. Elwell, and David T. Delpy∗ Abstract: Optical topography (OT) is a near infrared spectroscopy (NIRS) technique that provides spatial maps of haemodynamic and oxygenation changes. When developing, testing and calibrating OT systems it is often necessary to use tissue simulating phantoms that are capable of providing realistic changes in attenuation properties. We present a novel dynamic tissue phantom that enables spatially and temporally varying tissue properties to be reproduced in a controlled manner. This new dynamic test phantom consists of a modified liquid crystal display (LCD) (enabling flexible and rapid changes in attenuation across different regions of the phantom) sandwiched between two layers of tissue simulating epoxy resin (providing static and homogeneous optical absorption and scattering). By activating different pixels in the liquid crystal display it is possible to produce highly localised and dynamic changes in attenuation which can be used to simulate the changes associated with the cerebral haemodynamic response to functional activation. The reproducibility of the dynamic phantom will be described with examples of its use with an OT system. 1. INTRODUCTION The development and testing of most imaging systems requires the use of tissue phantoms that are capable of providing realistic changes in attenuation properties. These phantoms can be used to test design prototypes and evaluate instrument performance. Many useful optical phantoms have been developed in recent years with a wide range of attenuation properties that are characteristic of biological tissues. Optical phantoms for NIRS studies were first developed for breast imaging studies1 and subsequent research into different types of optical imaging techniques has led to the generation of a variety of tissue phantoms. Many of these have focused on the design of regular-shaped objects with specific attenuation properties including the use of biological molecules such as ∗ Department of Medical Physics and Bioengineering, University College London, Gower Street, London WC1E 6BT, United Kingdom. pkoh@medphys.ucl.ac.uk 2 KOH ET AL haemoglobin and melanin as absorbing components2 and the generation of hybrid phantoms for multimodality imaging.3 Classical phantoms generally have static properties i.e. absorption (µa) and reduced scattering coefficients (µs’) matching those of the biological tissues4 that are not spatially variable. NIR topography systems are increasingly being used to monitor the haemodynamic response to functional activation via the resulting spatially and temporally varying changes in cortical attenuation. Simulation of this varying physiological signal cannot be carried out using the static phantom approach and there is a need for a dynamic phantom that can reproduce these optical changes spatially and temporally in a controlled manner. Design of a Dynamic Phantom using Liquid Crystal Display (LCD) One approach to producing a phantom which enables rapid and spatially varying changes in attenuation is to use the existing design of a multilayer resin phantom and to insert an additional layer of material within it, the optical properties of which can be altered easily. An LCD seems to fit the requirements for such an inserted layer since 1) it relies on external light to provide the image and does not emit light itself and 2) it has a layer of light-polarising liquid molecules whose orientation is electrically controlled which allows its attenuation properties to be changed rapidly and with high spatial specificity. This combination of static layers in which the optical properties are fixed (representing skin/skull and white matter) and a dynamic layer in which the attenuation properties can vary (representing cortical tissue) provides a reasonable simulation of the type of physiological signal changes that the OT systems are required to monitor. Figure 1a shows the configuration of the LCD dynamic phantom. The phantom incorporates a top layer of epoxy resin with a realistic thickness (to represent the attenuation due to extracerebral layers). The light then passes through the LCD display. In the current study the size of LCD unit used allowed six laser sources and three detectors to be configured to produce measurements over seven channels with a fixed optode spacing of 30 mm (Figure 1b). The lower block phantom material (representing the brain white matter) is large enough to ensure light is scattered back to the surface and light loss to the boundary is small. (a) (b) Figure 1. (a) Schematic of the dynamic phantom and (b) optode arrangement used in the current study. DEVELOPMENT OF DYNAMIC TEST PHANTOM FOR OPTICAL TOPOGRAPHY 2. 3 METHODS A QVGA (resolution: 320 x 240 pixels) transflective mode LCD (Nan Ya Plastics Corporation) was used. The 2.2 mm-thick passive display (active area: 76 x 57 mm) uses a Chip-on-Flex configuration. Each active pixel in the LCD has an area of 5.64 x 10-3 mm2. An external controller (CB-GT380, Amulet Technologies Limited) was selected to drive and control the display. A HTML script describing the sequence of the animation is programmed into the controller. All optical measurements were made using a ETG-100 OT system (Hitachi Medical Corporation, Japan).5 The results described are from the light intensity measurements of the 780 nm-wavelength, expressed in arbitrary units. The recipe used to construct the solid phantom has previously been published.4, 6 The matrix material was constructed using epoxy resin (MY 753 Aeropia Chemical Supplies). A concentrated dye solution (Pro Jet 900NP Zeneca Ltd.) as absorber and a Superwhite polyester pigment (Alec Tiranti Ltd.) as the scatterer were mixed with the solution. The resulting phantom has a µa of 0.01 mm-1 and µs’ of 1.0 mm-1 (at 800 nm) and the mean cosine of scatter is about 0.5.4 The area of the epoxy resin block was 110 x 90 mm2 with the base block having a thickness of 30 mm and the top block 5 mm. The absorption and scattering coefficients of the static phantom block were measured using a time-resolved optical system (MONSTIR).7 The test result showed that the variation between expected and measured coefficients was less than 5 %. 3. RESULTS In OT it is often assumed that the measured intensity correlates with the size of the activated attenuating region. However this will only operate over a limited range of sizes and shapes since in a scattering medium light can take various routes between the source and detector including paths which do not pass through the activated region. Initial studies were therefore conducted to investigate (i) the size of attenuating region that can be detected by OT, (ii) the effect of different region geometries and (iii) “crosstalk” between different optodes with spatially varying attenuation regions. Effect of Attenuation Region Size A circular attenuation region was programmed on the display area positioned centrally between source 1 and detector 3 (i.e. at the position of channel 4). The diameter of the region was varied between 1 and 27 mm. To determine the contrast (i.e. intensity difference between two different conditions) the detected intensities were normalised to an “all-dark display” baseline condition where all the pixels were activated. Figure 2 shows the normalised intensity as a function of region diameter. The results show a generally linear relationship between detected intensity and attenuator size down to a diameter of 5 mm. Below 5 mm, the contrast, which we have arbitrarily defined as a change of less than 1 %, approached the system noise level. 4 KOH ET AL Figure 2. Attenuation time course for varying attenuator sizes (indicated at top of figure). The alternate grey and white areas indicate the period for each size variation and the normalised intensity changes (indicated at bottom of figure) were calculated with reference to a baseline condition where the whole LCD was dark. Effect of Attenuation Region Shape Figure 3. Comparison of the effect of attenuation regions with different shapes. DEVELOPMENT OF DYNAMIC TEST PHANTOM FOR OPTICAL TOPOGRAPHY 5 The LCD was programmed to produce a range of attenuation regions with equal areas but different shapes, including squares, circles, rectangles with fixed width (vertical) and rectangles with fixed height (horizontal). The regions were centred on channel 4 and their areas were varied between 1 and 576 mm2. The intensity changes were subsequently normalised to the previously described baseline condition. Figure 3 shows a plot of the normalised intensity changes (expressed in percentage difference) for each of the attenuator shapes as a function of attenuator area. The result shows a generally linear trend between intensity and region sizes, but identifies a significant difference between the two rectangular shapes with same areas. The variation is due to the orientation of the optode pair relative to the region. The results suggest that along with size variation, differences in shape and orientation of the activated region can affect the OT signal. Effect of Attenuator Position on Crosstalk between Channels A circular attenuation region with a diameter of 27 mm was programmed on the LCD to move horizontally in sequence along the midline from channels 1-2, 3-5 and 6-7. The amount of “crosstalk” was defined as a residual change detected in the neighbouring channels. Figure 4 shows the intensity changes on all 7 channels as the 27 mm diameter attenuator was moved across the phantom. 10 episodes of crosstalk were identified (highlighted as circles) during this test. Subsequently, the attenuator region size was gradually reduced until the crosstalk effect was considered to be negligible (less than 1 % change in intensity). This occurred when the diameter of the attenuator region was less than 21.5 mm. Figure 4. Normalised intensity changes for all 7 channels with the 27 mm attenuator region. 10 “crosstalk” effects are circled. 6 4. KOH ET AL DISCUSSION A new dynamic phantom using a modified LCD has been developed as a tool for evaluating and optimising OT instruments. By placing the LCD between two blocks of static phantom materials which provide well-characterised optical properties, a more realistic simulation of the spatially and temporally varying attenuation changes seen during cortical functional activation can be achieved. The effects of attenuator size, shape and orientation on measured intensity have been described. In addition, evidence of “crosstalk” between different optode pairs has been identified. This initial assessment suggests that, for the phantom geometry described in this study, the OT system was able to provide reasonable spatial differentiation with various attenuator shapes and sizes. There are several issues which were not addressed in this study; the attenuation effects associated with the LCD particularly the loss of light due to the polarizers and effect of the clear glass on the LCD have not been quantified. While the contribution due to the difference in refractive indices between the epoxy resin (1.56 at 800 nm) and the LCD glass (~1.5) is considered to be negligible, coupling between the LCD and static phantom layer has not been investigated. The current setup can also only simulate attenuation changes in two dimensions, when in reality light attenuation due to physiological changes in tissue occurs in three dimensions. In most cases optical topography is used to measure the spatial changes in attenuation arising from changes in chromophore concentration and as such absolute quantification of the attenuation properties is not required. Since the dynamic phantom is also intended to be used as a calibration tool for system, the actual photon path (which in turn affects the sampling area) will not affect the measurement as long as the variation remain fairly consistent throughout the measurement volume. 5. ACKNOWLEDGEMENTS This work was funded with grants from EPSRC/MRC, (GR/N14248/01) and in collaboration with Hitachi Advanced Research Laboratory, Japan. 6. REFERENCES 1. 2. 3. 4. 5. 6. 7. J.Linford, S.Shalev, J.Bews, R.Brown, H.Schipper, Development of a tissue-equivalent phantom for diaphanography, Medical Physics, 13(6): 869-875 (1986). A.M.De Grand, S.J.Lomnes, D.S.Lee, M.Pietrzykowski, S.Ohnishi, T.G.Morgan, A.Gogbashian, R.G.Laurence, J.V.Frangioni, Tissue-like phantoms for near-infrared fluorescence imaging system assessment and the training of surgeons, Journal of Biomedical Optics, 11(1): 014007 (2006). W.D.D'Souza, E.L.Madsen, O.Unal, K.K.Vigen, G.R.Frank, B.R.Thomadsen, Tissue mimicking materials for a multi-imaging modality prostate phantom, Medical Physics, 28(4): 688-700 (2001). M.Firbank and D.T.Delpy, A design for a stable and reproducible phantom for use in near infra-red imaging and spectroscopy, Physics in Medicine and Biology, 38: 847-853 (1993). Y.Yamashita, A.Maki, H.Koizumi, Measurement system for noninvasive dynamic optical topography, Journal of Biomedical Optics, 4(4): 414-417 (1999). M.Firbank, M.Oda, D.T.Delpy, An improved design for a stable and reproducible phantom material for use in near-infrared spectroscopy and imaging, Physics in Medicine and Biology, 40: 955-961 (1995). F.E.W.Schmidt, M.E.Fry, E.Hillman, J.C.Hebden, D.T.Delpy, A 32-channel time-resolved instrument for medical optical tomography, Review of Scientific Instruments, 71(1): 256-265 (2000).