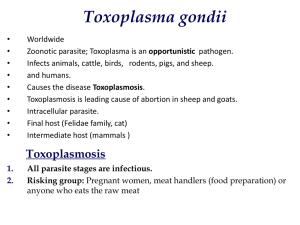
The incidence of toxoplasmosis in a mentally retarded population
advertisement

The incidence of toxoplasmosis in a mentally retarded population by Marlene Joyce Mackie A thesis submitted to the Graduate Faculty in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE in Microbiology Montana State University © Copyright by Marlene Joyce Mackie (1970) Abstract: Serums from 478 mental defectives from the Boulder River School and Hospital in Boulder, Montana were tested for antibodies for Toxoplasma gondii using the Indirect Fluorescent Antibody Test (IFAT) and the Indirect Hemagglutination Test (IHA). Serums for a control population consisting of specimens for Billings and Helena, Montana were tested concurrently. All populations were separated according to age and sex. In the control populations, the IFAT showed an increase in the percent of serums positive from ages 20-40 years. The age groups from 30-50 years showed a high percent positive in the IHA test. The Boulder group showed no rise in incidence until age 50 years in the IFAT while the IHA test showed a more even distribution in all age groups. In all three groups, the percent of serums positive for each sex was essentially no different. Agreement between the IFAT and the IHA1test was 38 percent in Helena, 43 percent in Billings, and 36 percent in Boulder. In the mentally defective group, the patients positive by the IFAT or IHA test were separated according to time in residence at the institution and type of mental retardation. The results showed little variation of the percent of positive serums in the length of time in residence or in the type mental retardation. Elevation and yearly rainfall statistics for Boulder, Helena and Billings, Montana were compared with the percent positive serums in these areas. The results showed essentially no difference. Statement of Permission to Copy In presenting this thesis in partial fulfillment of the require­ ments for an advanced degree at Montana State University, I agree that the Library shall make it freely available for inspection. I further agree that permission for extensive copying of this thesis for scholarly purposes-may be granted by my major professor, or, in his absence, by the Director of Libraries. It is understood that any copying or publication of this thesis for financial gain shall not be allowed without my written permission. THE INCIDENCE OF TOXOPLASMOSIS IN A MENTALLY RETARDED POPULATION by MARLENE JOYCE MACKIE A thesis submitted to the Graduate Faculty in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE in Microbiology Approved: Chairman, Examining(Committee Grad­ uate Dean MONTANA STATE UNIVERSITY Bozeman, Montana August, 1970 iii ACKNOWLEDGEMENT The author wishes to express her gratitude and appreciation to Dr. Alvin G. Fiscus for his time and guidance while working on this project. She would like to thank Dr. J. Allen Miller and the labor­ atory staff of St. Peter's Hospital and Montana Crippled Children's Hospital in Helena, Montana and Bynum Jacksop and his staff at St. Vincent's Hospital in Billings, Montana for their assistance in collecting of the serums,comprising the control populations. Also, this project could not have been completed without the cooperation and advice given by Dr. Phillip Pallister and the assistance of his staff at the Boulder River School and Hospital, Boulder, Montana. She would also like to thank Dr. Alvin G. Fiscus, Dr. D. G. Stuart, Dr. W. D. Hill and Dr. S . Rogers for their advice in prepar­ ing this manuscript. This research was supported by Public Health Service Grant, AHT-68-034 and Grant 379, Department of Botany and Microbiology, Montana State University, Bozeman, Montana. iv TABLE' OF CONTENTS Page VITA ........................................................... ii ACKNOWLEDGEMENT . . . . . . . . . . . . . . . . . . . . . . . . . iii TABLE OF CONTENTS ............................................... iv LIST OF TABLES ................. vi LIST OF F I G U R E S .................. ABSTRACT vii ..................................................... viii I N T R O D U C T I O N .............. MATERIALS I AND M E T H O D S ..................... Study groups Group I . ...................... 15 ...................... ; ................. 15 Group 2 Group 3 ............... 15 ...................... .. . .................. . . ; ................ . Maintenance of the organism . . . . . Indirect Fluorescent Antibody Test Antigen preparation ........ .................. .............. Preparation of the anti-human Antigen preparation 16 16 . . . . . . . . . conjugate. . . . . . Indirect Fluorescent AntibodyTest procedure Indirect Hemagglutination Test . . . . . 16 .... 17 17 18 21 ......................... 23 .............................. 23 Tanning of the sheep red blood c e l l s .......... 24 v 'Page RESULTS Sensitization of the tanned sheep red blood cells ...................................... 24 Technique of the microtitration test . . . . . . . . 25 ............................................ .. 26 The incidence of toxoplasmosis correlated to age and sex ..................................... 26 Correlation between length of time institution­ alized and incidence of toxoplasmosis ............ 31 Incidence of toxoplasmosis correlated to the typq of mental retardation ......................... 31 Correlation of toxoplasmosis with elevation and rainfall ....................................... 34 DISCUSSION 36 SUMMARY , BIBLIOGRAPHY 43 vi LIST OF TABLES Page Table Table Table Table Table Table Table I II III IV V VI VII Incidence of Toxoplasma antibodies in various geographical locations .......... ... 12 The total number of serums tested in the 3 test groups , . ........................ 27 The total number of serums tested in each group ................. . . . . . . . . . . 28 Percent agreement between the Indirect Hemagglutination Test and the Indirect Fluorescent Antibody T e s t .............. .. 29 Correlation between incidence of positive serums and the years in residence at. Boulder River Training School and Hospital . . . 32 Indirect Fluorescent Antibody Test and Indirect Hemagglutination Test positive patients separated according to diagnosis of type of mental r e t a r d a t i o n .......... .. 33 Correlation of incidence of toxoplasmosis with elevation and rainfall in the three geographical locations .................. 35 ... vii LIST OF FIGURES , Page Figure I Pattern of congenital toxoplasmosis. , ........ 6 Figure 2 Toxoplasma gondii as it appears in the Indirect Fluorescent Antibody Test . , ........ 22 Figure 3 The Indirect Hemagglutination Test for toxoplasmosis............ . . r ........ 22 Figure 4 Distribution of patients testing positive according to the Indirect Fluorescent Anti­ body Test (IFAT) and the Indirect Hemagglutination T e s t .......... .. ........... 30 viii ABSTRACT Serums from 478 mental defectives from the Boulder River School and Hospital in Boulder, Montana were tested for antibodies for ' Toxoplasma gondii using the Indirect Fluorescent Antibody Test (IFAT) and the Indirect Hemagglutination Test (IHA). Serums for a control population consisting of specimens for Billings and Helena, Montana were tested concurrently. All populations were separated according to age and sex. In the control populations, the IFAT showed an in­ crease in the percent of serums positive from ages 20-40 years. The age groups from 30-50 years showed a high percent positive in the IHA test. The Boulder group showed no rise in incidence until age 50 years in the IFAT while the IHA test showed a more even distribution in all age groups. In all three groups, the percent of serums positive for each sex was essentially no different. Agreement between the IFAT and the IHAltest was 38 percent in Helena, 43 percent in Billings, and 36 percent in Bowlder. In the mentally defective group, the patients positive by the IFAT or IHA test were separated according to time in residence at the institution and type of mental retard­ ation. The results showed little variation of the percent of positive serums ip the length of time in residence or in the type mental re­ tardation. • Elevation and yearly rainfall statistics for Boulder, Helena and Billings, Montana were compared with the percent positive serums in these areas. The results showed essentially no difference. INTRODUCTION In 1908, Toxoplasma gondii was isolated by two different groups working independently. Nicolle and Manceaux (1908) isolated the organism from Ctenodactylus gondii, a rodent in Africa and Splendore (1908) isolated it from rabbits in Brazil. In 1908, Darling isolated cyst forms from the arm muscle of a Barbadian negro. From 1908 to 1939, data were published which dealt primarily with morphological descriptions and the occasional occurrences in various animals and man,(Feldman, 1968a). Wolf et al. (1939) demonstrated that the organism invaded the fetus in utero resulting in a stillborn or diseased infant. Two years later, acquired toxoplasmosis was describ­ ed in children as an encephalitis by Sabin and in adults as a spotted fever syndrome by Pinkerton and Henderson (1941). Since that time, numerous reports citing toxoplasmosis as a multisystem disease (Altman, 1968) have emanated from North and South America;; ,Europe, Africa, Asia, and Oceania (Wright, 1957). Toxoplasma is an obligate, intracellular, parasite (Sabin and Olitsky, 1937) able to ipfect a wide range of animal hosts including marsupials, moles, rodents, carnivores (Moller, 1952), swine (Farrell et al., 1952), sheep, cattle (Jacobs, 1960b), various simians (Sabin and Ruchman, 1942; Cowen and Wolf, 1945), birds (Jacobs and Jones, 1950; Jacobs et al., 1952) and some reptiles (Frenkel, 1953; Jacobs, 1956). 2 It proliferates in all cells in the vertebrate host with the exception of the non-nucleated red blood cells (Feldman, 1968)-. Entry into the cell is facilitated by the use of lysozome-like structures and hyaluronidase (Norby et al., 1968; Lycke et al., 1965). Once inside the host cell, Toxoplasma is capable of competing with thq host cell for nutrients and metabolites (Jacobs, 196,3). Eventu­ ally, this process results in host cell rupture with the resultant spread of virulent organisms to other cells (Jacobs, 1963). A variation of the virulent life cycle often occurs when cysts develop in a vacuole of the host cell (Jacobs, 1967). As this occurs, the proliferation of the organism subsides, the symptoms of the disease disappear, leaving the host with chronic toxoplasmosis for life. The condition does not incapacitate the host but symptoms may recur when a cyst ruptures releasing viable organisms which are able to reinfect susceptible cells (Jacobs, 1963). More recent evidence indicates that the chronic state may not be induced by cyst rupture only, but by the persistence of residual trophozofte.gr-. in trace! Iular Iy without host cell rupture (Jacobs, 1967). In summary, the characteristics of Toxoplasma which are crucial in its' pathogenicity are: (l) its' ability to grow in many types of cells; (2) its' ability to form a cyst; and (3) its' obligate, intra­ cellular development (Altman, 1968). 3 Early studies on transmission of Toxoplasma gondii centered about the trophozoite;- The organism was found to be fragile, not resistant fo osmotic pressure changes, and incapable of surviving for long periods extracellularIy (Jacobs, 1968). Since the acute i disease is characterized by a parasitemia, investigations were directed toward blood sucking arthropods as reservoirs of the disease. Mosquitoes, fleas, triatomid bugs, bedbugs, lice, mites, and ticks were tested with no success (Jacobs, 1968). Large numbers of trophozoites introduced directly into the stomach of the recipient host failed to produce the disease while the feeding of tissue from chronically infected animals did (Jacobs, 1968). This initiated studies which isolated the qyst from animal tissue, showed its * incidence and characterized its* resistant qualities (Jacobs et al., 1960a; Work, 1968). Data published by Jacobs et al. (1960a) and Work (1968) showed that the cyst is resist­ ant to gastric juices for 2-3 hours, resistant to freezing, but susceptible to heat. They also showed that the viable trophozoites released from a cyst are capable of surviving in an environment simulating the small iptestine, firmly establishing the feasibility of.the opal route of transmission through undercooked meat (Kean et al, , 1969). Although this offered a partial explanation, addition­ al information was needed since many animals and human populations 4 which are strict herbivores (Jacobs et al., 1954b; Jacobs et al., 1960b) have a high incidence of toxoplasmosis. Research initiated in 1968 by Hutchinson et al. linked transmission of the organism with the egg of the nematode, Toxocara cati, in the feces of an infected cat. However, further studies showed that it is possible to transmit Toxoplasma in the absence of a nematode infection (Frenkel et al., 1969; Sheffield and Melton, 1969). Work and Hutchinson (1969) have since isolated what appears to be a new cyst form, from fecal floats of infected cats, which is able to produce the disease whep inoculated into laboratory mice intraperitoneally. The oral route of trans.-..' mission could explain the widespread incidence in populations with poor sanitation standards (Remington, 1970). In addition to the modes of transmission discussed above, congenital transmission via the placenta has long been established in humans and animals (Wolf et al., 1939; Remington et al., 1961; Jacobs, 1968). The syndromes caused by Toxoplasma gondii are extremely varied but can be placed into two major groups, congenital and acquired. Congenital toxoplasmosis occurs as an accidental complication of an inappafent primary infection of a pregnant human (Feldman and Miller, 1956b). The manifestations in the infant depend on the virulence of the org-anism, the resistance of the mother, and the 5 stage of pregnancy (Feldman and Miller, 1956b). If the infection occurs in the first trimester of pregnancy, fetal death is most common; if it occurs during the second trimester, the result is widespread disease causing infant death or such severe conditions as hydrocephalus, microcephalia, psychomotor retardation, cerebral calcifications, chorioretintis or microphtalmus. Infections occur­ ring during the last trimester produce acute symptoms of encephalitis with fever, generalized convulsions, and various paralyses and viceral involvement ill the form of jaundice, anemia, purpura, petichiae, % lymphadenopathy, hepatosplenomegaly, and chorioretinitis (Altman, 1968). The pattern of congenital toxoplasmosis is outlined in Figure I (Macer, 1963). Of the infants infected congenitally, one-fourth are premature with a mortality rate of 27 percent. Of those babies carried to term, 12 percent die and of those that survive, 80 percent are defective (Altman, 1968). Feldman (1953) found psychomotor retard­ ation in 56 percent, hydrocephalus or microcephalia is 33 percent -r each, convulsive disorders in the first three years in 50 percent, chorioretinitis in 80-90 percent with bilateral involvement in 85 percent, and cerebral calcifications in 63 percent of youngsters who tested Methylene Blue Dye test positive (Altman, 1968; Sabin and Feldman, 1948). It is important to note that often the only evidence 6 I I Mother (may be asymptomatic) Parasitemia. Spontaneous abortion MongoIismj Same infants appear normal at birth I -i Gradual increase in head size Tetrad of Congenital Toxoplasmosis Figure I. hydrocephaly convulsions chorioretinitis cerebral calcifications Microcephaly Hydrocephaly Icterus Rash Hepatosplenomegaly Splenomegaly Lymphadenitis Convulsions Chorioretinitis Pattern of congenital toxoplasmosis. 7 of congenital toxoplasmosis is the ocular involvement and that the acute, fulminating disease producing the classic tetrad of symptoms including chorioretinitis, hydrocephaly or microcephalia, psycho­ motor retardation and cerebral calcifications is much less common than the subacute.-asymptomatic form (Fair, 1959; Franke, 1960). Feldman and Miller (1956) generalized the following about con­ genital toxoplasmosis: (l) transmission can take place in any season (2) a recent infection is usually observed in the mother but rarely in the father; (3) sex of the fetus was not a factor; (4) twins are usually both infected, but not to the same extent; (5) mothers who have antibodies before conception do -not produce congenitally in­ fected children; (7) not all intrapregnancy infections lead to fetal disease and some fetuses escape infection altogether; and (8) subse­ quent children are not congenitally infected. The last generaliz­ ation has been disputed by researchers who feel that his may not always be the case. They stress that chronic toxoplasmosis is an important cause of repeated spontaneous abortions, stillbirths, and premature deliveries (Feldman, 1968b). Acquired toxoplasmosis presents an even more diverse symptomologic picture. The four manifestations of the disease are: (l) , lymphodonosa , (2) exanthematica, (3) cerebrospinalis, and (4) Opthalmica (Siim, 1956). The most common is the lymphatic fonp. The 8 onset may be acute or subacute and the course may be febrile, afebrile, or subclinical (Feldman, 1968b). Non-specific symptoms such as headaches, nausea, abdominal pain, arthralgias and myalgias may be present during the course of the disease (Feldman, 1968b),. All nodes, including hilar, mesenteric, and retroperitoneal may be involved. Biopsy of the node reveals typical forms of Toxoplasma which when inoculated into laboratory animals will produce the <_ disease (Siim, 1956; Feldman, 1968b). This form of the disease may mimic many other diseases such as infectious mononucleosis (Remington et al. , 1962), glandular fever (Siim, 1956), Hodgkin’s disease (Jacobs, 1967) and lymphadenopathy of unknown origin (Siim, 1956) and for this reason is often misdiagnosed. Immunity against the organism consists of macroglobulin (19S) which occurs in both the acute congenital or acquired syndromes. 7S antibodies are demonstrated only in infants born to chronically infected mothers (Remington et al., 1966). IBe macroglobulins pro­ vide the basis for many of the serologic tests presently used in diagnosis of the disease. The Methylene Blue Dye test developed by Sabin and Feldman in 1948 was the first serologic tool for the diagnosis of toxoplasmosis. However, the inconvenience of dealing with live parasites and the difficulty in obtaining large amounts of the "accessory" factor, 9 found only in fresh human serum, initiated a search for new methods of testing. A complement fixation procedure was developed in 1954 by Awad (Eichenwald, 1956). The test was not a useful diagnostic tool be­ cause antibody titers did not rise until late in the course of the disease and receded after a short time, making it difficult to obtain an early diagnosis. \ A hemagglutination test was developed in 1957a by Jacobs and Lunde. The procedure showed promise'-because of the stability of the antigen and the rapid reading of the test results (Jacobs and Lunde, 1957a). Additional adaptation to microtechniques has further simplified it by increasing the rapidity of performance and decreas­ ing the reagent demand (Lewis and Kessel, 1961). Other tests have been described including a direct agglutination test (Fulton and Turk, 1959) and a flocculation test using acrylic particles (Siim and Lind, I960), however, these have not been used frequently. In 1959, Carver and Goldman reported a method of staining Toxoplasma gondii present in tissue sections with fluorescein labeled antibody. This work led directly to the development of the Indirect Fluorescent Antibody test (Kelen et al., 1962). The procedure was further developed and the specificity validated by Fletcher in 1965, 10 Sulzer and Hall in 1967, and Chessum in 1970. They found that the test was as sensitive as the Methylene Blue Dye test but more desirable because it had a sharpened point, stable reagents which were easily prepared and standardized,, and there was no need.for live parasites or the "accessory",factor. A skin test using a water-lysed suspension of organisms relies on the production of a delayed type of hypersensitivity.(Jacobs, 1963). It is used primarily in epidemiological studies where large , numbers of people are tested. Finally,, toxoplasmosis can be diagnosed through isolation of the organisms from the tissues (Walls et al., 1963) and inoculation into laboratory animals with the resultapt production of the disease (Eichenwald, 1956). Although there is a generalized parasitemia present during the acute disease, isolation procedures frequently fail (Remington et al., 1962). The methods discussed are used in the diagnosis of acquired toxoplasmosis. They may be used in the congenital form but more often conclusive diagnosis is made by the demonstration of the para­ site in Wright stained smears of the newborn’s spinal or ventricular fluid. Serological studies at the time of birth and 3 months later should be performed to confirm the diagnosis (Feldman, 1968b). 11 Newer methods in serological diagnosis and the development of the i'ntradermal skin test have facilitated studies on the incidence of Toxoplasma in all parts of the world. Table I lists some of these studies. Further research has been done in an attempt to correlate the incidence of Toxoplasma antibodies with geographical location (Walls and Kagan, 1967b; Walls et al., 1967a; Paul et al., 1964), occupation­ al associations (McCulloch et al., 1963; Walls and Kagan, 1967b; Kabayashi, 1963; Murakami, 1964), urban versus rural residence (French et al., 1970; Gibson, 1956; Schnurrenberger et al., 1964), animal contact (Schnurrenberger et al., 1964; Kijriball et al., 1960), and climatological variations such as altitude and rainfall (Walton et al. , 1966b). Generalizations drawn from these studies are; (I) the incidence of antibodies tends to increase with age; (2) a higher incidence occurs in geographical locations with a lower elevation and a greater rainfall; (3) a higher incidence occurs in rural populations; (4) persons in contact with animals or animal products have antibodies more frequently than those who are not; (5) con­ sumption of raw beef or eggs increases the incidence of antibodies; (6) the incidence was not influenced by sex. Several groups (Burkinshaw et al., 1953; Cook and Derrick, 1961; Fair, 1959; Kongo et al.., 1964) have published data on the occurrence Table" I. Author Feldman and Miller M !I Il I! M Il Il Il II Incidence of Toxoplasma antibodies in various geographical locations. Date Country Locality 1956 1956 1956 USA USA Iceland Alaska Southwest USA USA USA USA Haiti ■ Honduras Tahiti USA USA Costa Rica USA USA Guatemala Mexico USA USA Portland, Ore St Louis, Mo New Orleans Pittsburgh 1956 1956 1956 1956 1956 1956 1956 Gibson et al„ 1956 Jacobs et al = 1954 1958 Gibson Gibson 1956 Gibson 1956 Gibson 1958 Unpub Biagi* Jacobs et aI* Unpub 1965 Feldman Tennessee ■ New York City Turrialba Memphis, Tenn Memphis, Tenn Esciunta Tampico Washington,DC Northeast North MidAtlantic South Atlantic East North Central East South Central Type of group Eskimo Navdjo Normal pop. Il ft Il Il Il It Il Test used No. tested No. + %.+ Dye test Dye test Dye test 21 236 108 0 10 12 0 4 11 Dye test Dye test Dye test Dye test Dye test Dye test Dye test Dye test Dye test Dye test Dye test Dye test Dye test Intradermal Dye test 293 184 270 144 104 266 121 987 62 156 317 700 100 231 124 51 47 84 51 37 170 82 215 9 138 75 42 94 HO 33 17 26 31 35 36 64 24 6 94 48 27 109 22 20 193 469 30 18 16 18 549 97 18 256 49 19 Negro Jewish Adults Adults Children > 16 All ages Negro Military recruits Dye test 68 22 15 89 Table I' (Continued)* Author Date Country Locality West North Central West South Central ■Mountain Pacific Lamb and Feldman 1968 Brazil Midtvedt Ludlam Wallace 1965 1965 1969 Norway Africa Pacific Atolls Kobayashi et al„ Murakama * Wright3 1957 1963 Japan 164 ■ Japan All -parts Niger Delt Eauripik Waluae Ifalik Tokyo Entire country Type of group Test used ' .-- Military recruits Dye test Children Dye test All ages Dye test All ages Dye test All ages Dye test All ages Dye test Abattoir workers Intradermal Pluck handlers Intradermal Ham making workers Intradermal Normal res. " 20=24 yrs. Dye test No, tested No. + %'.+ 315 37 12 201 182 406 27 6 32 13 3 8 1455 320 64 751 36 40 52 11 65 134 99 105 9 43 59 7 43 56 90 61 68 137 46 34 -84 1-81 25 54 35 30 30 7 483 14 of Toxoplasma antibodies in the residents of schools for the mentally retarded. Generally they found that Toxoplasma as a cause of mental deficiency ' was rare. All studies, except one in Georgia, had been done outside of the United States. Due to the fact that only one epidemiological study in a school for the mentally retarded had been done in the United States, it was advisable to undertake this type of study in Montana. Antibody titers as determined by the Indirect Fluorescent Anti­ body Test and the Indirect Hemagglutination Test were correlated to the type of mental retardation, age, sex, and length of time insti­ tutionalized. Control populations were tested concurrently to deter­ mine incidence in a normal population. MATERIALS AND METHODS STUDY GROUPS Group I. .478 serums were drawn from residents selected from groups classified according to diagnosis at the Boulder River School and Hospital located at Boulder, Montana. The groups included: (1) Chromosomal defects (XXYjXX/XO,XXY / t) and mongolism (2) deformity syndromes, unclassified (three minor defects or more) and classified (3) genetic, including PKU, homocysteinuria , deafness, pseudo­ hypothyroidism, Mast syndrome (4) prematurity pf unknown cause and caused by attempted abortion or placenta praevia (5) post infection, in utero, unknown, Rubella, Coxsackie B , poliomyelitis, mumps encephalitis, Western Equine encephal­ itis, measles encephalitis, and tubercular meningitis (6) genetic and environmental Including jaundice, kernicterus, toxemia of pregnancy and unclassified j (7) familial (no deformities) caused by consanguinity, socio­ cultural deprivation, mental retardation with mental ill­ ness and aphasia (8) trauma caused by a fall, an accident or during birth (9) unclassified group associated with microcephaly, spasticity, epilepsy, and hydrocephalus and another group with mental retardation with no apparent cause. Residents were selected without regard to age or sex. specimens were talcep. and the serums were frozen. Blood 16 Group 2, One portion of the control population consisted of 285 serums drawn from patients admitted' to St. Peter’s Hospital and Montana Crippled Children's Hospital in Helena, Montana from September 1969 through November 1969. The patients were selected randomly without consideration for sex and age, except in the children's hospital where all were under 10 years of age. Group 3. Another portion of the control population, consisting of 197 serums was drawn from patients admitted to St. V incentbs.-'Ho.ap.i.f41 in Billings, Montana from March 1970 through May 1970. Again, the patients were delected without regard to sex or age. In selecting the control group from two different cities in Montana, an attempt was made to demonstrate the effect of climatol­ ogical variations such as elevation and rainfall on the incidence of the disease. MAINTENANCE OF THE ORGANISM : .^Toxoplasma gondii suspended in sheep red blood cells was received from the National Communicable Disease Center, Atlanta, Georgia, courtesy of Dr. Kenneth Walls. This suspension was propagated by inoculating 0.5 ml intraperitoneally (IP) into Swiss Manor mice (Walls, 1969). Thereafter, it was maintained by inoculating 0.1 ml 17 IP of peritoneal fluid diluted 1:100 in sterile saline into 6-8 week old animals (Eyles and Coleman, 19563),. The organism was passaged every 4 to 6 days (Fletcher, 1965), and was preserved by freezing according to the procedure of Eyles et al. (1956b)\ This was accomplished by collecting the peritoneal fluid from infected mice and diluting it 1:5 with a solution of 20 percent serum in physiolo­ gical saline. ampoules. One ml samples were placed into sterile 2 ml glass To each ampoule, I ml of a 10 per cent glycerol solution was added, the contents mixed with a syringe, and the necks sealed with heat. The ampoules were frozen by placing them in a basket which had been lined with a layer of absorbent cotton approximately I inch in thickness. -70°C. The baskets were placed in a REVCO freezer at The suspensions were warmed in a 37°C water bath for 5 minutes and 0.5 - 1.0 ml was injected into Swiss Manor mice (Eyles et al., 1956b). INDIRECT FLUORESCENT ANTIBODY TEST Antigen preparation. Peritoneal fluid was collected from mice that had been inoculated 4-5 days earlier. The exudate was centrifuged at 200 rpm for 10 minutes to sediment the leucocytes. The supernatant was removed, phosphate buffered saline (PBS) pH 7.2 added, and recentrifuged at 2000 rpm for 15 minutes to sediment the organisms. 18 The supernatant was discarded and the organisms were resuspended in PBS pH 7.2. The wash procedure was repeated 3 times after which the organisms were suspended in a sufficient volume of PBS pH 7.2 to obtain a concentration of 25-30 organisms per high, dry, field. A small drop of the suspension was placed in each of four 1.5 cm circles inscribed on microscope slides with a waterproof, felt-tip pen. The slides were allowed to dry af room temperature and stored at -70°C (Fletcher, 1965; Sulzer and Hall, 1966). Preparation of the anti-human, conjugate. Fourteen human serums were drawn from patients randomly selected at St. Peter's Hospital in Helena, Montana. The serums were pooled prior to their inoculation into 3 randomly bred rabbits. Three ml of serum was injected intramuscularly into each rabbit. Three similar injections followed at 10 day intervals, at the end of which the rabbits were bled from the marginal ear vein. The precipi­ tin titers as determined by the tube test were number I, I:10^280; number 2, 1:5280; and number 3, 1:5280. Each rabbit was given an additional injection of I ml of human serum intravenously in order to elevate the titer, after which they were: number I, 1:20,560; number 2, 1:20,560; and number 3, 1:10^280 (Campbell et al., 1964). serums stored at -15°C. The rabbits were exsanguinated and .the 19 An aliquot of rabbit anti-human serum was diluted with 10 volumes of distilled water to which an equal volume of saturated ammonium sulfate (Mallinkrodt) was added. The mixture was placed at 4°C overnight after which the ammonium sulfate was removed by aspiration, leaving the globulins suspended in a small volume of 50 percent saturated ammonium sulfate. A second precipitation was done by dissolving the globulins in a volume of distilled water equal to the volume of the precipitated globulins. Again, an equal volume of saturated ammonium sulfate was added to the solution. The pre­ cipitated globulins were collected by centrifugation. For dialysis, the globulins were dissolved in a volume of water equal to the original volume of the whole serum. They were refrig­ erated at 4°C for 10 minutes to dissolve all the globulins. The solution was placed into dialysis, tubing and dialized against 0.85 percent sodium chloride at 4°C. Two dialyses, of 12 liters each were performed, one from 1:00 p.m. to 5:00 p.m. in the afternoon and the other from 6:00 p.m. to 7:00 a.m. the next morning. At the end of the second dialysis, the 0.857. NaCl used for dialysis was checked with a I percent solution of barium chloride. The absence of turbidity indicated the elimination of the sulfate ion (Goldwasser . and Shepherd, 1958). The globulin solution was pipetted from the tubing and the volume measured. 20 Carbonate-bicarbonate buffer (0.5 M pH 9.0) was added to the globulin solution in an amount equal to 10 percent by volume. The fluoroisothiocyanate (FITC) added to the globulin mixture at this point was calculated using the globulinrvolume after dialysis, the amount of globulin present in the dialized solution as calculated by the Biuret procedure (Bauer et al., 1968), and 20 milligrams of FITC needed per gram of protein (Fletcher, 1965; Walls, 1969). Conjugation was performed at room temperature for 2 hours by shaking the dye-globulin mixture gently on a mechanical rotator. Unconjugated FlTC was removed by filtering the conjugate through a G-50, fine, globular Sephadex column which had been calibrated with 0.02 M PBS pH 7.2. The conjugated serum was stored into I ml aliquots at -15°C (Fletcher, 1965). The optimum dilution of the conjugate was determined by making dilutions of 1:20, 1:40, 1:80, and 1:100 in PBS pH 7.2. The dilutions were used in the performance of the Indirect Fluorescent Antibody Test on known positive and negative serums. The optimum dilution of conjugate was that dilution which gave maximum fluorescence at the known titer of the positive serum and negative fluorescence with the negative serum. 21 Indirect Fluorescent Antibody Test procedure. were diluted 1:16 and 1:64. Initially, serums Antigen slides were washed in a light stream of distilled water, blotted with laboratory tissue, and placed on wet filter paper in 15 cm petri plates. Each smear was covered with a different serum dilution, the pan was covered and placed in a' 37°C incubator for 30 minutes, after which the serums were rinsed with a light stream of distilled water. The slides were immersed in a staining dish containing PBS pH 7.2 and rotated at 15 rpm for 15 minutes. plates. The slides were blotted dry, and ,replaced in the petri At this time, the smears were covered with the optimum dilution of anti-human conjugate which had been diluted in PBS pH 7.2. The slides were handled as above. After rotation, the slides were removed, washed with distilled water, blotted dry; and coverslipped with buffered glycerol pH 8.0 (Fletcher, 1965). The slides were examined on a fluorescent microscope (Leitz) using a BG-12 exciter and an GG-I barrier filter (Helen et al., 1962). With every test the following controls were used: saline, a negative serum, and a positive serum of known titer. The positive serum was tested at four dilutions, one below, one at, and two above the known titer. was tested at l:64only. The negative serum A reaction was considered positive when , yellow green fluorescence was observed to extend around the entire porifery of the organism (Sulzer and Hall, 1966), as shown in Figure 2. 22 Figure 2 Toxoplasma gondii as it appears in the Indirect Fluorescent Antibody Test. Figure 3 The Indirect Hemagglutination Test for toxoplasmosis. Column A represents the positive control, column H the negative control and columns B through G are negative serums. 23 The titer was the highest dilution at which more than half of the organisms exhibited this degree of fluorescence. Interpretation of the results was as follows: 1:16* to 1:64 indicated past exposure or early stages of the disease followed by rising titers; 1:256, recent exposure or a present infection; 1:1024, acute toxoplasmosis.- If a test serum had a titer of 1:64 during initial testing, the serum was diluted 1:16, 1:64, 1:256, and 1:1024 and repeated (Walls, 1969). INDIRECT HEMAGGLUTINATION TEST Antigen preparation. The peritoneal exudate from an infected mouse was centrifuged in tared centrifuge.tubes for 10 minutes at 1300 rpm. The supernatant was discarded and the sediment containing Toxoplasma gondii was washed twice in 10 ml of cold saline. ( The Toxoplasma suspension was centrifuged after the last saline wash and the super­ natant discarded. The organisms were resuspended in 10 volumes (W/V) of cold distilled water and kept at 4°C overnight. The solution was frozen and thawed for 5 to 10 cycles (-70°C to 37°C). An equal volume -of double strength saline (1.7%) was added to restore isotonicity. The solution was spun for one hour at 30,000 x G in an. angle head centrifuge (Beckman Model L) to remove cellular debris. The super­ natant comprised the antigen, the dilution of which was 1:20. The antigen was stored at -20°C (Lunde and Jacobs, 1959; Chordi et al., 24 1960), Tanning of the sheep red blood cells. Sheep red blood cells were obtained under aseptic conditions in Alseverfs solution. They were washed 5 times with PBS pH 7.2, and adjusted to a I percent suspension by adding PBS pH 7.2 to the packed cells. An equal volume of I:100,000 dilution of tannic acid (Mallinkrodt) was added. The solution was mixed thoroughly and placed in an ice water bath for 15 minutes. The tannic acid treated cells were removed from the ice water bath, centrifuged for 5 minutes at 1500 rpm. The supernatant was discarded and the cells were washed once with PBS pH 7.2 (Chordi et al., 1964). The cells were resuspended in 4 I percent suspension in 0.6 percent normal rabbit serum in PBS pH 7.2 (Lewis and Kessel, 1961). Sensitization of the tanned sheep red blood cells. The optimum dilution of the antigen was determined by preparing four dilutions of the antigen in PBS pH 6.4. They were! I;50, 1:100, 1:200, and 1:400, The cells wete sensitized with these dilutions as described below. A tannit? acid cell control was prepared by sensitizing tanned cells with PBS pH 6.4 only. The optimum dilution was that dilution of the antigen which gave the correct titer of, the known positive serum and a negative reaction with a known negative serum (Walls, 1969). 25 Sensitization was accomplished by mixing equal volumes of tanned cells and the optimum antigen concentration- This mixture was allowed to incubate for 15 minutes in a 37°C water bath. After this period, the cells wefe centrifuged, washed twice with 0.6 percent normal rabbit serum (NRS) in PBS pH 7.2 and adjusted to a I percent suspen­ sion with 0.6 percent NRS (Chordi et al., 1964). Technique of the microtitration test. Using microtitration equip­ ment, serum dilutions of 0.05 ml in 0.6 percent NRS were made. two-fold series of dilutions beginning at 1:2 was used. A The first four dilutions were disregarded, the 1:32 dilution was used as a tanned cell control, and the 1:64 dilution was used as the initial test dilution. were added. To each serum dilution, 0.025 ml of sensitized cells The plates were shaken immediately after this addition and were left at; toom temperature for 2 hours. The tests were read as follows: a discrete button indicated a negative test and a disper­ sion pf the cells with no pattern indicated a positive test (Fulton and Turk, 1959). was as follows: This is shown in Figure 3. Interpretation of data a titer of 1:64 to 1:128 indicated a past exposure or early infection; 1:256 to 1:512, a recent infection; and 1:1024, acute toxoplasmosis (Lewis and Kessel, 1961). RESULTS The incidence of toxoplasmosis correlated to age and sex. Previous studies have indicated a trend toward increasing incidence of toxoplasmosis with increasing age and that sex had no correlation. Therefore, the age and sex of the patients in the present study which were positive when tested by the Indirect Fluorescent Antibody Test (IFAT) were compared with the total number tested in each of the age groups as related to sex. The results are presented in Table I. In the general population, there was an increase from ages 20 to 40 years while institutionalized patients showed no consistent rise until after age 50. The same pattern was also shown by using the Indirect Hemagglutination Test (IHA) (Table III) but was not as clear-cut. The results displayed graphically in Figure 4 are similar to data published by Cook and Derrick, 1961 and Fair in 1959. Using both tests, no significant differences were shown in the presence of anti­ bodies when patients were separated according to sex, nor did there appear to be any significant differences between a normal population and an institutionalized, mentally retarded one. Correlation of test results showing those serums positive in both tests, those positive in the IFAT only and those positive in the IHA test only are included in Table IV. Agreement between the two ranged between 36 and 43 percent for the three geographical locations 27 Table II. Age gtoup in' years The total number of serums tested in the 3 test groups. Patients have been separated by sex and age. The number positive and percent positive as tested by the Indirect Fluorescent Antibody test has been included. number tested number positive males females males females 0 - 9 10 - 19 20 - 29 30 * 39 40 - 49 50 - 59 60 - 69 70 - 79 80 - 89 TOTAL 18 7 7 12 13 19 23 15 16 130 16 12 22 15 18 20 18 15 19 155 0 - 9 10 - 19 20-29 30 - 39 40 - 49 50 - 59 60 - 69 70 - 79 80 - 89 TOTAL 0 14 12 6 14 15 7 8 2 78 I 15. 25 21 20 20 10 4 3 119 0 - 9 10 - 19 20 - 29 30 - 39 40 - 49 50 - 59 TOTAL 17 85 85 36 32 9 267 11 75 78 30 12 4 211 HELENA 2 0 2 I 0 I I I I 9 percent positive males females percent total 0 0 2 I 0 2 I 2 2 10 11.0 00 27.5 8.3 0 5.3 4.4 6.7 6.3 6.8 0 0 9.1 6.7 0 10.0 5.5 13.2 10.6 6.5 5.9 0 13.8 7.4 0 5.1 4.9 10.0 8.5 6.3 BILLINGS 0 0 2 I 0 4 I 3 0 4 I 0 I I I 0 0 0 10 8 0 7.2 0 16.6 28.5 0 14.2 12.4 0 10.2 0 13.4 16.0 14.3 0 5.0 10.0 0 0 8.5 0 10.3 10.8 14.8 11.8 2.9 11.8 8.4 0 9.2 5.8 5.9 9.5 2.7 6.2 22.0 7.5 9.1 . 13.3 2.6 10.0 0 25.0 8.2 7.0 9.4 6.2 6.2 4.6 32.0 7.8 BOULDER I I 10 5 2 8 I 3 2 0 2 I, 20 17 28 Table III. Age group in years The total number of serums tested in each group. The patidnts have been separated on the basis of sex and age. Positive results as determined by the Indirect Hemagglut­ ination Test have been included. number tested number positive males females males females percent positive males females percent total 18 7 7 12 .13 19 23 15 16 130 16 12 22 15 18 20 18 15 19 155 HELENA I 0 0 I 0 I 2 I I 7 0 0 0 I I 0 I 0 0 3 5.6 0 0 8.3 0 5.3 8.7 6.7 6.3 5.4 0 0 0 6.8 5.6 0 5.6 0 0 2.0 2,8 0 0 7.4 3.2 2.6 7.6 3.4 2.9 3,5 9 19 29 39 49 59 69 79 89 0 14 12 6 14 15 7 8 2 78 I 15 25 21 20 20 10 4 3 119 BILLINGS 0 0 0 0 3 0 0 I 0 4 0 I 2 2 0 I 0 0 0 6 0 0 0 0 21.5 0 0 12.5 0 5.1 0 6.8 8.0 8.5 0 5.0 0 0 0 5.1 0 3.5 5.4 7.5 8.8 2.9 0 8.3 0 5.6 0 - 9 10 - 19 20 r- 29 30 - 39 40 - 49 50 - 59 60-69 TOTAL . 17 85 85 36 .32 9 3 267 11 75 78 30 12 4 I 211 BOULDER 0 I 3 5 I 2 I I 2 0 0 I 0 0 10 7 0 3.5 1.9 2.8 6.7 0 0 2.6 9.1 6.7 2.6 3.3 0 25.0 0 4.6 • 3.6 5.0 1.8 3.1 4.6 7.7 0 3.5 0 - 9 10 - 19 20 - 29 30 - 39 40 - 49 50 - 59 60 - 69 70 - 79 80 - 89 TOTAL 0 10 20 30 40 50 '60 70 80 - Table IV. Location Percent agreement between the Indirect Hemagglutination Test and the Indirect Fluorescent Antibody Test. Total positive No., of serums positive in both tests No. of serums positive in IFAT only No. of serums positive in IHA only No. No. No. Percent Percent ' Percent' Helena 21 8 38.0 11 52.0 2 10.0 Billings 21 9 43.0 10 48.0 2 9.0 Boulder 39 ,- .14 36.0 23 56.0 2 O OO % Posi 30 Boulder Helena Billings 20 30 40 50 60 70 80 90 Age in years Figure 4 Distribution of patients testing positive according to the Indirect Fluorescent Antibody Test (IFAT) and the Indirect Hemagglutination Test (IHA). 31 tested. Forty-eight to 56 percent of the tests were positive in the IFAT only. Of these, all but two were positive in the first dilution (1:16) with the two exceptions positive at 1:64. Eight to 10 percent of the tests were positive in the IHA test only. The titers of these ranged from 1:64 to 1:256 with most occurring in the lower dilution. Correlation between length of time institutionalized and incidence of toxoplasmosis. Table V shows the number of patients tested and the incidence of Toxoplasma antibodies correlated with the number of years institutionalized. The incidence of positive serums was evenly distributed throughout all periods of residence. A longer time of residence did not appear to increase the number-; of patients with Toxoplasma antibodies. Incidence of toxoplasmosis correlated to the type of mental retardation. The Boulder residents tested, were divided into groups according to diagnosis as discussed on page 15. Table VI includes the number tested in each group, the number positive, and the percent positive. No group showed a predominant incidence over any other group except gen­ etic and environment. This may be attributed to the small number of serums tested in this category and therefore appears statistically insignificant. Of the 478 serums tested in the mentally retarded population, 5 were considered as possible cases of congenital Table V. Correlation between incidence of positive serums and the years in residence at Boulder River Training School and Hospital. Years in residence Number tested Number positive Percent positive (3-5 59 6 10.2 6-10 160 16 10.0 11 - 19 160 10 6.3 20 - 29 65 3 4.7 30 - 39 25 2 8.0 40 - 49 9 I 11.2 478 38 7.9 TOTAL Table VI, Indirect Fluorescent Antibody Test and Indirect Hemagglutination Test positive patients separated according to diagnosis of type of mental retardation. Group* Description H o . tested Group I Chromosomal 81 5 Group 2 Deformity syndrome 50 6 12.0 Group 3 Genetic 40 I 2,5 Group 4 Prematurity 10 0 0 Group 5 Post-infection 54 3 5.6 Group ~b -Genetic.and environment 3 I 33.0 Group 7 Familial 79 5 6.3 Group 8 Trauma 30 2 6.7 Group 9 Unknown 130 15 Microcephalus 23 3 13.6 HydrocephaIus 8 3 37.5 18 2 11.2 478 38 7.9 Epilepsy TOTAL * Groups, discussed in detail on page 15. No, positive . Percent positive 6.2 . . 11.6 - 34 toxoplasmosis. A brief history for each of these follows: (1) Ten year old girl, mental and physical invalid with micro­ cephaly, multiple congenital defects, bilateral exophtalmus. Mother ill during 1st trimester of pregnancy'. IFAT positive at 1:64; IHA positive at 1:128. (2) Thirteen year old boy, partial invalid with hydrocephalus. Mother ill during pregnancy. Infection at 7 months of age accompanied by severe penicillin reaction. IFAT negative; IHA positive at 1:64. (3) Twelve year old boy, history suggests kernicterus but jaundice not noted, blind at birth. Mother had I premature birth and several miscarriages before patient's birth. IFAT positive at 1:64; IHA negative. (4) Twenty-seven year old man, microcephalic with congenital cataracts. IFAT positive at 1:16; IHA negative. (5) Six year old boy, complete invalid, institutionalized since six months of age, hydrocephalic. Mother ill during pregnancy. The nature of the illness was unknown. IFAT positive at 1:16; IHA, negative. These cases are listed as possible since a diagnosis was not established at birth and it is conceivable that infections were acquired in later years. Correlation of toxoplasmosis with elevation and rainfall. An attempt was made to correlate the incidence of Toxoplasma antibodies with climatological conditions. The variation of incidence relative to altitude and rainfall did not appear significantly different for the three geographical locations tested. Table VII. Comparative data is included in Table VII. Location Correlation of incidence of toxoplasmosis with elevation and rainfall in the three geographical locations tested. Elevation* Annual Rainfall* "No, tested 28-5" 19 10 6.3 3.5 10 9.2 . 5.6 ' 17 7.8 3.5 "No. positive IFAT IHA Helena 3893 9.79 in. Billings 3139 13.10 in. 197 18 Boulder 5165 11.90 in. 478 37 , 'Eercent positive IFAT IHA Co Cn * Elevation and rainfall statistics (Dightman, 1960). DISCUSSION This study concurs with previously published data (Burkinshaw et al., 1953; Cook and Derrick, 1961; Kongo et al., 1964) which showed that the incidence of toxoplasmosis was no more frequent in a mentally retarded than in a normal population. Establishing a firm causal relationship for congenital toxo­ plasmosis in any particular patient was not possible with information and procedures available to this study. All residents, except hospit­ alized patients, are primarily restricted to the school grounds but on occasion are allowed to go to the neighboring town, thus coming into contact with dogs and cats. Several of the residents (ages 10-30 years) have jobs in the school farm or dairy which brings them into contact with cattle and chickens. Also, most residents-. Vi'sit'their homes and some are placed into homes to work, again providing an opportunity to come into contact with farm or domestic animals which have been proven to be carriers of the disease (Jacobs, 1957b; Siim, 1963; Jacobs, 1968). One might expect isolation from contact with Toxoplasma in those patients which had been institutionalized for long periods of time. Except in strictly hospitalized patients, this did not appear to be the case, since non-hospItalized patients were not in residence all year and, as mentioned above, home visits, placement procedures, and farm and domestic animals on the grounds provide the opportunity for ) 37 contact with the organism. This information might explain why little correlation between time in residence and antibody titers can be established. That the incidence was not higher than the normal population in all groups, suggests that one method of transmission is not direct contact as opportunities for case to case spread both by the respiratory and alimentary routes are frequent in this type of institution. Similar studies published by Cook and Derrick (1961) presented results very similar to the present study. In all cases tested, the mental deficiency was produced by factors operating before, at, or shortly following birth (see Table VI, page 33). However, since the data presented in Tables II and III suggest that the incidence of antibodies does not increase until much later in life, congenital toxoplasmosis is unlikely to be a frequent cause of mental deficiency. This conclusion is supported by earlier studies done by Burkinshaw et al., (1953), Fair (1959), Cook and Derrick (1961), and Labzoffsky et al. (1965). Little correlation could be found between the type ofi-imental retardation and the incidence of antibodies for Toxoplasma (Table VI, page 33)• Previous reports published by Burkinshaw et al.,(1953) and Cook and Derrick (1961) support this conclusion. According to the information, the groups affected by genetic and environmental causes and hydrocephalus appeared to have a much higher incidence of 38 antibodies than did any other group. However, because of the small number of serums tested in these groups, the figures do not appear to be statistically significant. A previous study published by Walton et al. (1966b) related increased incidence of toxoplasmosis to a higher rainfall and lower elevation. The Variations in rainfall, elevation, and apt!body occurrence were so slight ip the three geographical areas tested that one can conclude that pp differences existed. Complicating the analysis, was the fact that the residepts in the Boulder Rfver School and Hospital'had resided ip all parts of Moptana and two had come from outside of the state. Also, since background information was not available concerning the patients drawn for the control populations, it cannot be assumed that they had lived all of their lives ip either Helena or Billings, Montana. Agreement between the Indirect Fluorescent Antibody Test (IFAT) and the Indirect Hemagglutination Test (IHA) was surprisingly low. This may be attrfbptable to the fact that responses to two different antigens yrere measured (Kefen et al., 1962)« Due to the nature of the test, the surface antigens of Toxoplasma were tested ip the fFAT while intracellular antigens were measured in the IHA (Siim, 1968). Studfes have been made comparing the Methylene Blue Dye test (MBD) results with IFAT results. Correlation between the two ranged 39 from poor (Lalpzoffsky et al., 1965) to excellent (Goldman et al., 1962-j Walton et al.^ 1966a). lifo data have been published comparing IHA titers and IFAT titers, however, several studies have been published comparing IfIA titers and MBD timers. Since the MBD test and the IFAT have been found to agree; well, an attempt has been made to use these studies to compare the IFAT titers and the IHA titers obtained in the present study. Kagen et al. (1967) reported that less than 4 percent of the serums which tested IHA negative were positive by the MBD test and that those were oply at low levels of activity. Ip the present study all except 2 serums which were positive in the IFAT and negative in the IHA were positive only in the first dilution. The 2 exceptions were positive in the second dilution. Walton et al. (1966a) showed 96 percent agreement between the IHA and MBD tests while Walls et al. (1967b) showed 83 percent correlation. A study done by Labzoffsky et al. (1965) reported only 26 percent agreement between the two tests. Application of this information to the present study which showed 36 to 43 percent correl­ ation between the IFAT and IHA test, reveals comparable data. Frevibus studies have also shown MBD test positive serums which are negative by IHA procedures, and others in which the reverse is true (Feldman, f.968a). Similar data in the present study showing positive IHA titers accompanied by negative IFAT titers were found 40 but in all cases but one the titers were low. the titer measured at 1:256. In this exception, This phenomenon may be explained by the fact that the antibodies appear at different times during the infec­ tion. It has been noted that MBD antibodies can be detected sooner than IHA test antibodies, apd while both antibodies can be detected for many years the IHA remains longer^(Jacobs, 1963;;Kagen et al., 1967; Feldman, 1968a). Again, assuming that the IFAT and MBD tests measure similar antigaps, we may say that the IFAT antibody appears sooner than the IHA antibody and the IHA antibody remains detectable lpnger. These findings may explain the differences, however, no evidence to indicate that this is the case has been offered. SUMMARY Serums were drawn from 478 mental defectives residing in the Boulder River School and Hospital in Boulder, Montana. Control pop­ ulations consisting of 197 sefums from Billings, Montana and 285 serums from Helena, Montana were drawn. The incidence of antibodies for Toxoplasma gondii was measured in all serums by the Indirect Fluorescent Antibody Test and the Indirect Hemagglutination Test. Antibody incidence in the mentally defective group was correl­ ated to age, sex, years in residence at the institution and type of mental retardation. There was an increase in the number of patients with Toxoplasma antibodies after age - 50"< years but no consistant pattern preceeding that age. Sex, the type of mental retardation and the time in residence at the institution had no apparent effect on the number of patients with Toxoplasma antibodies. Since no cases of congenital toxoplasmosis couli be validated in 478 serums,, it was concluded that the disease is rarely a cause of mental deficiency. The Indirect Fluorescent Antibody Test and Indirect Hemmaglut!nation Test were found to agree in 36 to 43 percent of the serums which tested positive. The serums drawn from Billings, Helena, and Boulder were compar­ ed in relation to elevation, rainfall and percent incidence of Toxoplasma antibodies. The variations in the three criteria between the three geographical locatiops mere so slight that no differences appeared to be present. BIBLIOGRAPHY Altman, Kenneth A. 1968. Toxoplasmosis„ Medicine 68; 2151-2156. New York State Journal of Bauer, J.D., Philip Ackermann,. and Gelson Toro. 1968. Bray1s Clinical Laboratory Methods, pp. 321. C.V. Mosby Co., St. Louis. Burkinshaw, John, Brian Kirman9 and Arnold Sorsby. 1953, Toxoplas­ mosis in relation to mental deficiency. British Medical Journal I; 702-704. Campbell, Dan H., J.S; Garvey, N.E. Cremer, and D.H. Sussdorf. 1964. Methods in Immunology. W.A. Benjamin Co., New York. p. 137. Carver, R.K., Morris Goldman, 1959. Staining Toxoplasma gondii with fluorescein-labeled antibody. III. The reaction in frozen and paraffin sections. Am, J. Clin. Path. _32; 159-164. Chessum, B.S. 1970. Examination of sera for toxoplasmosis antibody using immunofluorescence. J. Med. Lab. Technol. 27^: 49-54. Chord!, Andres, Kenneth Walls, and Irving Kagan. 1964. Studies on the specificity of the Indirect Hemmagglutination Test for toxoplasmosis. J. Immun. j}3: 1024-1033. Cook, Ian, E.H. Derrick. 1961. The incidence of Toxoplasma antibodies in mental hospital patients. Abst. Ann. Med. _10; 137-141. Coweh, D., A. Wolf. 1945. Toxoplasmosis in the monkey. An acute fatal infection experimentally produced in a young Macaca mulatta. J. Inf. Dis, 77; 144-157. Darling, S.T. 1968. Sarcospoidiosis; With a report of a case in man. Proc.. Canal Zone Med. Assn. I.; 141-152. Dightman, R.A. 1960. Climates of the States, Montana. of Commerce Weather Bureau. No. 60-24. U.S. Dept, Eichenwald, Heinz F. 1956. The laboratory diagnosis of toxoplasmo­ sis. Ann. N.Y. Acad. Sci. 64; 207-214. Eyrleg^', Don E 9, Nell Coleman. 1956a. Relationship of size of inocul­ um to time of in mice infected with Toxoplasma gondii. J. Parasit. 42; 272-276. 44 Eyles, Don E., Nell Coleman, and D .J„ Cavanaugh. 1956a. Preservation of Toxoplasma gondii by freezing. J. Parasit. 42: 408-413. Fair, John R. 1959. Congenital toxoplasmosis. IV. Case finding using the skin test and opthaImoscope in state schools for mentally retarded children. Am. J. of Opthamology 48: 813-819. Farrell, B.L., F.L. Docton, D.M. Chamberlain, and C.R. Cole. 1952. Toxoplasmins. I. Toxoplasma isolated from swine. Am. J. Vet. Res. 13: 181-185. Feldman, Harry £., Louise T. Miller. . 1956a. Serological study of toxoplasmosis prevalence. Am. J. Hyg. 64: 320-335. Feldman, Harry A., Louise T. Miller. 1956b> Congenital human toxoplasmosis. Ann. N.Y. Acadei Sci. 64: 180-185. Feldman, Harry. A. 1965. A nationwide serum survey of United States military recruits, 1962. VI, Toxoplasma antibodies. Am.. J. Epidem. 81: 385-391. Feldman, Harry A, 1968a. Toxoplasmosis. New England J. Med. 279: 1370f1375. Feldman,. Harry A. 1968b. 279: 1431-1437. Toxoplasmosis cont. New England J. Med. Fletcher, S . 1965, Indirect fluorescent antibody technique in the serology of Toxoplasma gondii. J. Clin. Path. I1S : 193-199. Franke, H, 1960. On the diagnosis and clinical aspects of acquired toxoplasmosis, p. 103. In Slim J,C . ed. Human Toxoplasmosis: Proceedings of the 8th International Convention on Pediatrics. Copenhagen, Munksgaard. French, Jean G., Harley B. Messinger, and Jesie MacCarthy. 197.0. A study of Toxoplasma gondii infection in farm and non-farm groups in the same geographical location. Am. J. Epidem. 91: 185-191. Frenkel, J.K. 1953. Host, strain and treatment variation as factors in the pathogenesis of toxoplasmosis. Am. J. Trop. Med. Hyg. 2: 390-411. 45 Frenkel, J.K., J.P. Dubey, N.L. Miller. 1969. Toxoplasma gondii: fecal forms separated from eggs of the nematode Toxocara cati. Science 164: 132-133. Fulton, J.D., J lL. Turk. 1959. Toxoplasma gondii. Lancet Direct agglutination test for 2: 1068-1069. Gibson, Colvin L., Don E. Eyles, Nell Coleman, and Clinton S . Smith. 1956a. Serological response of a rural negro population to the Sabin-Feldman cytoplasm-modifying test for toxoplasmosis. Am. J. Trop. Med. Hyg. 5: 772-783. Gibson, Colvin L. 1956b. Distribution of Toxoplasma antibodies in comparable urban and rural groups. Public Health Reports 71: 1119-1123. Gibson, Colvin L., Nell Coleman. 1958. The prevalence of Toxoplasma antibodies in Guatemala and Costa Rica. Am. J. Trop. Med. Hyg. . I; 334-338. Goldman, Morris, M.A. Gordon, and R.fc. Carver. 1962. Comparison of ' titers of dye and fluorescence-inhibition tests in the serologic diagnosis of toxoplasmosis. Tech. Bui. of the Reg. of Med.-Tech. 32: 57-66. Goldwasser, R.A., C.C. Shepard. 1958. Staining of complement and modifications of fluorescent antibody procedures. J. Immunl. 80: 122-131. Kongo, Setuya, Shozo Torii, and Shizuko Takeuchi. 1964. Seroepidemiological studies on the role of Toxoplasma infection as an import ant cause of mental deficiency. Jap. J. Parasit. h3: 34-42. Hutchinson, W.M.,. J.F, Dunachie, and K„ Work. 1968. The faecal trahs mission of Toxoplasma gondii. Acta Path. Microbiol. Scandinav. 74: 462-464. Jacobs, Leon, Frances E . Jones. 1950. The parasitemia in experiment­ al toxoplasmosis. J. Inf. Dis. 6%: 78-89. Jacobs, L., M.L. Melton and M.K. Cook. 1952. The prevalence of toxoplasmosis in wild pigeons. J. Parasit. ^8:. 457-461. 46 Jacobs, Leon, Katherine Cook and Edith Neumann. 1954b. Serologic survey data on the prevalence of toxoplasmosis in the Jewish population of New York. J. Parasit. 40: 701-702. Jacobs, Leon. 1956. Propagation, morphology, and biology of Toxoplasma. Ann. N.Y. Acad. Sci. 64: 154-179. Jacobs, Leon, Milford N. Lunde. 1957a. A hemagglutination test for toxoplasmosis. J. Parasit, 4J: 308-314. Jacobs, Leon, 1957b. The interrelation of toxoplasmosis in swine, cattle, dogs, and man. Public Health Reports _72; 872-882. Jacobs, Leon, Jack S . Remington, and Marjorie Melton. I96Oa. The resistance of the encysted form of Toxoplasma gondii. J. Parasit. 46: 11-21. Jacobs, Leon, Jack S. Remington, and Marjorie Melton. 1960b. A survey of meat samples from swine, cattle, and sheep for the presence of encysted Toxoplasma. J. Parasit. 46: 23-38. Jacobs, Leon. 1963. Toxoplasma and toxoplasmosis. Microbiol. 17: 429-450. Ann. Rev. Jacobs, Leon. 1967, Toxoplasma and toxoplasmosis. Parasitology. j>: 1-45. Advances in Jacobs, Leon. 1968. The transmission of toxoplasmosis. . Israel J. Med. Science 4: 1074-1085. Kagan, Irving G., Howard A, Fox, Kenneth W. Walls, and George R. Healy. 1967. The parasitic diseases of childhood with emphasis on the newer diagnostic methods. Clinical Pediatrics 6_: 641-654. Kean, B.H., Ann C. Kimball, and William Rf. Christenson. 1969. An epidemic of acute toxoplasmosis. J.A.M.A. 208: 1002-1004. Kelen, A.E., L. AyIlon-Leindi, and N.A. Labzoffsky. 1962. Indirect fluorescent antibody method in serodiagnosis of toxoplasmosis. Canadian J. Microbiol, j8: 545-554. Kimball,. Ann C., Henry Bauer, Charles G. Sheppard, Joe R. Held, and Leonard Schuman. 1960. Studies on toxoplasmosis. III. Toxoplasma antibodies in obstetrical patients correlated with residence, 47 animal contact, and consumption of selected foods. Tl; 93-119. Am. J. Hyg. Kobayashi, Akio, Toshio Ishii, Tsutomu Koyama, Matsuyoshi Kumada, and Yoshitaka Komiya. 1963. Studies on Toxoplasma. V. Incidence of Toxoplasma antibodies in ,abattoir workers, pluck handlers, ham-making workers, and normal residents. Jap. J. Parasit. 12: 28-36. , Labzoffsky, M.A., N.A. Fish, E. Gyulai and F. Roughley. 1965. surxzeyyof toxoplasmosis among mentally retarded children. Med. Ass. J. 92: 1026-1028. A Canad. Lamb, George, Harry Feldman. 1968.. A nationwide serum survey, of Brazilian military recruits, 1964. Am. J. of Epidem. 8_7: 323-328. Lewis, W.P., J. Kessel. 1961. Hemagglutination in the diagnosis of toxoplasmosis and amebiasis. Arch. Opthal, 66/. 471-476. LudIam, G.B. 1965. Toxoplasma antibodies in inhabitants of the Niger Delta. Trans. Royal Soc. Trop. Med. Hyg. 59/ 83-86. Lunde, Milford, Leon Jacobs. 1959. hemagglutination test antigen. Characteristics of the Toxoplasma J. Immunol. 82t 146-150. Lycke, E. Ebba Lund, and 0. Strannegard. 1965. Enhancement by Iyso'Zpme and hyaluronidass of the penetration by Toxoplasma gondii into cultured host cells. Brit. J. Exp. Path. 46/ 189-199. Maser, George„ 1963, Toxoplasmosis in obstetrics, its possible rel­ ation to mongolism. Am. J. Ob. Syn0 8%: 66-70. Murakami, Fumiya. 1964, Epidemiological studies on toxoplasmosis. I. Prevalence of Toxoplasma antibodies in residents in Nagasaki prefecture, including pregnant women, slaughter house workers, butchers, veterinarians and dog-catchers. End. Dis. Bui. of Nagasaki U. _6: 1-12. McCulloch, William F., John L. Braun, Darrol W. Hoggen, and Franklin H. Top. 1963. Studies of Medical and veterinary students skin tested for toxoplasmosis. Pub. Health Rep. _78: 689-697, Moller, T. 1952. Toxoplasmosis in Vulpis vulpis. Acta. Path. Microbiol. Scand. SuppI, J93: 308-320. 48 Midtvedt5 Tore. 1965. The frequency of positive dye test in children from different parts of Norway. Acta Paediatrica Scandinavica 54: 81-85. Nicolle5 D.5, L.'Manceaux. 1908. Sur Une Infection a Corps de Leishman (ou organismes voisins) due gondi. Compt. rend. Acad, d. Sc. 147-? 763-766. Norby5 Ragner5 Leif Lindhelm5 and Erik Lycke. 1968. Lysosomes of Toxoplasma gondii and their possible relation to the host-cell penetration of Toxoplasma parasites. J. Bact. _96: 916-919. Paul5 J.R., J.C. Neidermann5 R.J.C. Peason5 and C. Vu Ve Florey. 1964. A nationwide serum survey of United States military recruits, 1962. I. General considerations. Am. J. Hyg. 80; 286-292. Pinkerton5 H. 5 R.G. Henderson. 1941. Adult toxoplasmosis, previously unrecognized disease entities simulating typhus spotted-fever group. J.A.M.A. 116: 807-814. Remington5 Jack S., Leon Jacobs, and Marjorie Melton. 1961. Congen­ ital transmission of toxoplasmosis from mother animals with acute and chronic infections. J. Inf. Dis. 108: 163-173. Remington5 Jack, Charles,Barnett5 -Maureen Meikel5 and Milford Lunde0 1962. Toxoplasmosis and,infectious mononucleosis. Archives of Int. Med. 110: 744-753. Remington5 Jack, Michael Miller. 1966. 198 and 78 anti-toxoplasma antibodies in diagnosis of acute congenital and acquired toxo­ plasmosis. Proc. Soc. Exp. Biol. Med. 121: 357-363. Remington5 Jack 8. 1970. Toxoplasmosis: recent developments. Rev. Med. 21i 201-218. Ann. Sabin5 Albert, Peter K. Olitsky« 1937. Toxoplasma and obligate intracellular parasitism. Science. 8J5: 336-338. Sabin5 A.B., 1941. 116: 801-807. Toxoplasmic encephalitis in children. J.A.M.A. Sabin5 Albert, Isaac Ruchman. 1942. Characteristics of the Toxoplasma neutralizing antibody. Proc. Soc. Exp. Biol. Med. 49 51: 1-6. Sabin, Albert, Harry Feldman. 1948. Dyes as microchemical indicators of a new immunity phenomenon affecting a protozoan parasite (Toxoplasma). Science 108: 660-663. Schnurrenberger, P.R., R.A. Tjalma, F.H. Wentworth, and B.B. Wentworth. 1964. An association of human reaction to intradermal toxoplasmin with degree of animal contact and rural residence. Am. J. Trop. Med. Hyg. 13: 281-286. Sheffield, Harley and Marjorie Melton. 1969. .Toxoplasma gondii, transmission through feces in abscehce of Toxocara cati eggs. Science 164: 431-432. Siim, J. Chr. 1966. Toxoplasmosis acnuisita lymphodonosa: Clinical and pathological aspects. Ann. N.Y. Acad. Sci. 64: 185-206. Siim, J.C., K. Lind, 1960. Path. Microbiol. Scan. Siim, J.C, 1963. A Toxoplasma jH): 445-446. flocculation test. Toxoplasmosis in domestic animals. Acta. Adv. Vet. Scii-. 8 : 335-429. Siim, J.C.(Chairman.) 1968. Meeting of the Investigators on Toxoplas­ mosis, p . 19. Geneva, Switzerland, Splendore, A. 1908„ Uno Nuovo Protozoa Parassita dei Conigli: Incontrato Nelle Lesioni Anatomiche d'una Malattia che Recorda in Molti Punti il Kala Asar dell 1uomo„ Rev. Soc. Sci. Sao Paulo 3: 109-112, Sulzer, Alexander and Elmer Hall. 1967. Indirect fluorescent anti­ body tests for parasitic diseases. IV. Statistical study of variation in the indirect fluorescent antibody test for toxoplas­ mosis. Am. J. Epidem. 816: 401-407. Wallace, George. 1969. Serologic and epidemiologic observations ontoxoplasmosis on three Pacific Alotts. Am. J. Epidem, 90_i 103- 111. Walls, Kenneth, rW, Taraska, J. Joan, Morris Godman. 1963. Isolation - of Toxoplasma gondii from cysts in human brain. J, Parasit. 49: 930-931. 50 Walls, Kenneth, Trying Kagan and Albert Turner. 1967a. the prevalence of antibodies to Toxoplasma gondii, military recruits. Am. J. Epidem. 85: 87-92. Walls, Kenneth, Irving Kagan. 1967b, antibodies to Toxoplasma gondii. 86: 305-313. Walls, Kenneth. 1969. Studies on I, U.S. Studies on the prevalence of II. Brazil. Am. J. Epidem. Personal communication. Walton, B.C., B.M. Benchoff, and W.H. Brooks. 1966. Comparison of the indirect fluorescent antibody test and methylene blue dye test for detection of antibodies to Toxoplasma gondii. Am. J. Trop. Med. Hyg. 15: 149-152. Walton, B.C., I, DeArjonn, and B.M. Benchoff. 1966b. Relationship of Toxoplasma antibodies to altitude. Am. J. Trop. Med. Hyg. JL5: 492-495. Wolf, A., D . Cowen, and B. Paige, 1939, Human Toxoplasmosis: Occurrence in infants encephalomyelitis. Verification by transmission to animals. Science 8jh 226. Work, Kresten. 1968. Resistance of Toxoplasma gondii encysted in pork. Acta. Path. Microbiol. Scand. 13% 85-92. Work, K., W.M. Hutchinson. 1969. A new cystic form of Toxoplasma gondii. Acta. Path. Microbiol. Scand, TJL: 191-192. Wright, Willard, 1957. A summary of the newer knowledge of toxoplas­ mosis. Am. J, Clin. Path. J28: 1-17. t M211 cop. 2 I - Mackie, Marlene J The incidence of toxoplasmosis in a gent ally retarded population. I INXMk A N D A D O * e » S /1 /37 ? M 2.// top. 5 /