VOL. 26, NO. 3
AUTUMN 2013
BENEFITS LAW
JOURNAL
From the Editor
Equitably Unfair: Supreme Court
Says Health Plan Document
Trumps Participant’s Request
to Split Legal Fees
I
t took the US Supreme Court three cases and more than a decade
to lay down the ERISA law on subrogation: It’s whatever the health
plan document says. Thus, the unanimous Supreme Court decision in
US Airways, Inc. v. McCutchen, 133 S.Ct. 1537, 2013, allows employers
to draft their health plans to provide that the plan gets first dibs on
any third-party recovery by a participant injured in an accident, even
before deducting the participant’s legal fees. Of course, employers
do not have to (and should not) impose this rule on their employees
injured in an accident when it would be harsh or foolish, but instead
should use McCutchen to reasonably and fairly draft and administer
subrogation clauses. And, beyond the health plan arena, McCutchen
strengthens the principle that in any dispute the plan document is king.
The facts of McCutchen show how the strict application of a right
of subrogation can be unfair. James McCutchen was in an awful
multivehicle auto accident. He incurred $66,866 in medical expenses, which were covered by his employer-sponsored health plan.
Although James estimated his total injury was north of $1 million, he
was only able to recover $10,000 from the driver who caused the accident (she was underinsured, and there was a fatality plus a number of
other serious injuries) plus an additional $100,000 from his own auto
insurer. After his lawyer’s 40 percent contingency fee, James was left
with $66,000. And the health plan wanted it all—plus an additional
$866 out of James’ own pocket. As Justice Kagan acknowledged,
From the Editor
James “would pay for the privilege of serving as [the plan’s] collection agent.” Adding insult to injury, it did not matter that the bulk of
James’s recovery came from the proceeds of an insurance policy paid
with his own money.
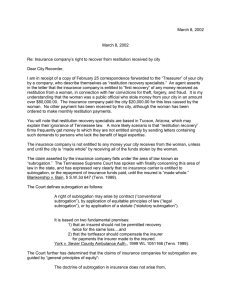
The health plan’s claim was based on two prior Supreme Court
cases, Great West Life & Annuity Ins. Co. v. Knudson (534 U.S. 204,
2002) and Sereboff v. Mid Atlantic Medical Services (547 U.S. 356,
2006), holding that a plan’s claim for subrogation was “appropriate equitable relief” authorized by ERISA Section 502(a)(3). (Think
back to law school or perhaps when you were cramming for the
bar exam: Until the beginning of the last century, courts were
separated into law and equity, and subrogation was considered an
equitable remedy.) “Fine” said James, but if you can assert a Section
502(a)(3) equitable claim against me, I can counter with equitable
defenses. Specifically, James argued that the plan should not be
able to recover anything until he is “made whole” from all his losses
or, barring that, the plan should at least have to pay its share of
the legal costs in obtaining the recovery under the “common-fund”
doctrine. (Again, back to law school: Under the common-fund
doctrine, if two or more parties share a common asset—e.g., an insurance recovery—they must split the costs of obtaining that asset.)
The Court agreed that James ordinarily could use equitable defenses unless the plan document said he could not. The plan was viewed
as a contract between the participant and the plan fiduciaries, and
the parties could contractually “agree” that equitable defenses would
not apply. In an excellent turn of phrase destined to be repeatedly
quoted for decades, “[b]ut if the agreement governs, the agreement
governs.”
In this case, the plan stated that James was “required to reimburse
the plan for amounts paid for claims out of any monies recovered.”
Thus, the plan document trumped James’s right to assert any other
equitable defenses to the plan’s right of recovery. This should have
been the end of James’s day in court. However, five of the justices
found that the plan was vague because it was silent on the application
of attorney fees. Under the contract-is-the-contract approach, a vague
or incomplete subrogation provision may be reinterpreted by a court
to discern the parties’ intent. The case was sent back to the district
court to determine how to allocate legal fees.
This punt (cop-out?) back to the district court is particularly interesting because the lower court had already found the plan document
to be clear, ruling that James must pay. Perhaps the majority felt that
poor James was getting screwed by its opinion and, even though it
was fashioning a rule that could potentially short change many others,
wanted to give James a bone for his efforts.
BENEFITS LAW JOURNAL
2
VOL. 26, NO. 3, AUTUMN 2013
From the Editor
Where does this leave us, and what should employers and plaintiff lawyers do? If nothing else, the Court has left us a very clear
and simple rule: Employers are free to determine the scope of their
desired subrogation policy and set it out in the plan document. To
avoid instances of a sympathetic judge finding what’s clear to be
unclear, the plan language should be very specific. But just because
an employer can get first dibs on any recovery, that does not mean
that this is necessarily the best policy. In my practice I’ve found that
while every plan has a subrogation clause, employers are reasonable in applying this language. I’ve never seen a McCutchen-type
situation where the employer expected the employee to lose money
from its over aggressive subrogation claim. Indeed, I have a sneaky
feeling that even James and his employer would have worked
something out but for the fun their lawyers had arguing before the
Supreme Court.
With a subrogation provision, employers always benefit when their
employees recover after an accident. It is in the employer’s interest to
encourage, or at least not actively discourage, a participant victimized
in an accident from retaining counsel and suing. Also, a “plan-first”
subrogation clause pushes the participant-plaintiff to demand an
over-large recovery and not to settle for less, knowing that a more
modest recovery might put nothing in their pocket or, even worse,
cost them money. Thus, it behooves employers, the participantplaintiff, and his or her counsel to reach an accommodation with the
plan before bringing a suit as to how any monies recovered will be
divided. The lawyer should get his or her contingency fee. But, if the
recovery is large enough (compared to the medical costs and injury
suffered by the participant), the plan should be repaid in full, sans
legal fees.
More important than the simple and clear rule on subrogation is the
unanimous Court reemphasizing that, absent a contrary ERISA provision, employers are absolutely free to set the terms of their plans. In
other words, as long as it is legal, the plan document rules. Employers
should consider whether they wish to draft documents to foreclose
other forms of participant claims that go beyond what’s mandated by
ERISA. While this may seem cruel, in reality the freedom to set terms
encourages employers to provide benefits to employees and their
families.
David E. Morse
Editor-in-Chief
K & L Gates LLP
New York, NY
BENEFITS LAW JOURNAL
3
VOL. 26, NO. 3, AUTUMN 2013
Copyright © 2013 CCH Incorporated. All Rights Reserved.
Reprinted from Benefits Law Journal Autumn 2013, Volume 26,
Number 3, pages 1–3, with permission from Aspen Publishers,
Wolters Kluwer Law & Business, New York, NY, 1-800-638-8437,
www.aspenpublishers.com