Document 13374182
advertisement
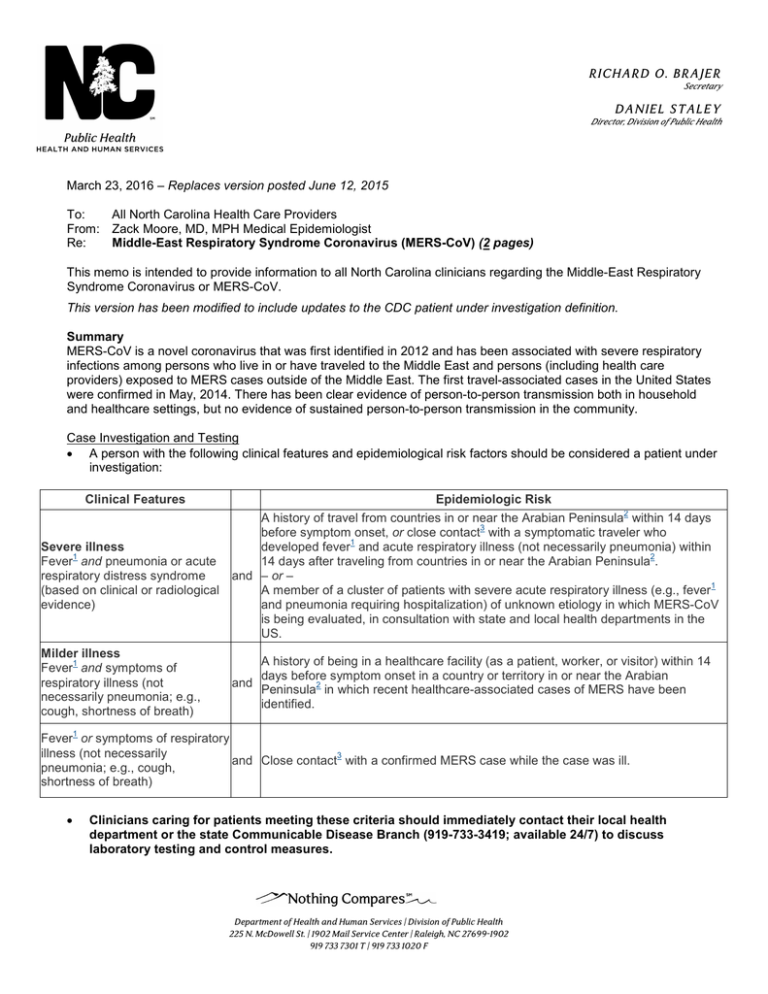
RI C HA R D O. B R A J E R Secretary DA NIE L S TA L E Y Director, Division of Public Health March 23, 2016 – Replaces version posted June 12, 2015 To: All North Carolina Health Care Providers From: Zack Moore, MD, MPH Medical Epidemiologist Re: Middle-East Respiratory Syndrome Coronavirus (MERS-CoV) (2 pages) This memo is intended to provide information to all North Carolina clinicians regarding the Middle-East Respiratory Syndrome Coronavirus or MERS-CoV. This version has been modified to include updates to the CDC patient under investigation definition. Summary MERS-CoV is a novel coronavirus that was first identified in 2012 and has been associated with severe respiratory infections among persons who live in or have traveled to the Middle East and persons (including health care providers) exposed to MERS cases outside of the Middle East. The first travel-associated cases in the United States were confirmed in May, 2014. There has been clear evidence of person-to-person transmission both in household and healthcare settings, but no evidence of sustained person-to-person transmission in the community. Case Investigation and Testing • A person with the following clinical features and epidemiological risk factors should be considered a patient under investigation: Clinical Features Epidemiologic Risk 2 A history of travel from countries in or near the Arabian Peninsula within 14 days 3 before symptom onset, or close contact with a symptomatic traveler who 1 Severe illness developed fever and acute respiratory illness (not necessarily pneumonia) within 1 2 Fever and pneumonia or acute 14 days after traveling from countries in or near the Arabian Peninsula . respiratory distress syndrome and – or – 1 (based on clinical or radiological A member of a cluster of patients with severe acute respiratory illness (e.g., fever evidence) and pneumonia requiring hospitalization) of unknown etiology in which MERS-CoV is being evaluated, in consultation with state and local health departments in the US. Milder illness 1 Fever and symptoms of respiratory illness (not necessarily pneumonia; e.g., cough, shortness of breath) A history of being in a healthcare facility (as a patient, worker, or visitor) within 14 days before symptom onset in a country or territory in or near the Arabian and 2 Peninsula in which recent healthcare-associated cases of MERS have been identified. 1 Fever or symptoms of respiratory illness (not necessarily 3 and Close contact with a confirmed MERS case while the case was ill. pneumonia; e.g., cough, shortness of breath) • Clinicians caring for patients meeting these criteria should immediately contact their local health department or the state Communicable Disease Branch (919-733-3419; available 24/7) to discuss laboratory testing and control measures. Department of Health and Human Services | Division of Public Health 225 N. McDowell St. | 1902 Mail Service Center | Raleigh, NC 27699-1902 919 733 7301 T | 919 733 1020 F RI C HA R D O. B R A J E R Secretary DA NIE L S TA L E Y Director, Division of Public Health • Persons who meet these criteria should also be evaluated for common causes of community-acquired pneumonia, if not been already done. Examples of respiratory pathogens causing community-acquired pneumonia include influenza A and B, respiratory syncytial virus, Streptococcus pneumoniae, and Legionella pneumophila. (Note: Viral culture should not be attempted in cases with a high index of suspicion.) MERS-CoV infection should still be considered even if another pathogen is identified, since co-infections have been reported. • Any clusters of severe acute respiratory illness in healthcare workers in the United States should be thoroughly investigated. Occurrence of a severe acute respiratory illness cluster of unknown etiology should prompt immediate notification of local public health for further investigation and testing. • Testing for MERS-CoV is available at the North Carolina State Laboratory of Public Health. Testing requires consultation and pre-approval from the state Communicable Disease Branch. Detailed information about specimen collection and transport is available at http://slph.ncpublichealth.com/topics.asp. Infection Control • Transmission of MERS-CoV has been documented in healthcare settings. • Standard, contact, and airborne precautions are recommended for management of patients in healthcare settings with known or suspected MERS-CoV infection. These include: o o o Use of fit-tested NIOSH-approved N95 or higher level respirators Use of gowns, gloves and eye protection Use of negative-pressure airborne infection isolation rooms if available • A facemask should be placed on the patient if an airborne infection isolation room is not available or if the patient must be moved from his/her room. • Additional guidance is available at http://www.cdc.gov/coronavirus/mers/infection-prevention-control.html. Treatment • No antivirals are currently available for treatment of MERS-CoV or other novel coronavirus infections. Reporting • MERS-CoV infections are reportable in North Carolina. Physicians are required to contact their local health department or the state Communicable Disease Branch (919-733-3419) as soon as MERS-CoV infection is reasonably suspected to exist. This is an evolving situation and recommendations are likely to change as new information becomes available. Updated information and guidance are available from the CDC at http://www.cdc.gov/coronavirus/mers/index.html. 1 Fever may not be present in some patients, such as those who are very young, elderly, immunosuppressed, or taking certain medications. Clinical judgement should be used to guide testing of patients in such situations. 2 Countries considered in the Arabian Peninsula and neighboring include: Bahrain; Iraq; Iran; Israel, the West Bank, and Gaza; Jordan; Kuwait; Lebanon; Oman; Qatar; Saudi Arabia; Syria; the United Arab Emirates (UAE); and Yemen (map on CDC site). 3 Close contact is defined as: a)being within approximately 6 feet (2 meters) or within the room or care area for a prolonged period of time (e.g., healthcare personnel, household members) while not wearing recommended personal protective equipment (i.e., gowns, gloves, respirator, eye protection); or b) having direct contact with infectious secretions (e.g., being coughed on) while not wearing recommended personal protective equipment. Data to inform the definition of close contact are limited. At this time, brief interactions, such as walking by a person, are considered low risk and do not constitute close contact. Department of Health and Human Services | Division of Public Health 225 N. McDowell St. | 1902 Mail Service Center | Raleigh, NC 27699-1902 919 733 7301 T | 919 733 1020 F Reporting Communicable Diseases – Mecklenburg County To request N.C. Communicable Disease Report Cards, telephone 704.336.2817 or 704.432.1742 Mark all correspondence “CONFIDENTIAL” Tuberculosis: TB Clinic Mecklenburg County Health Department 2845 Beatties Ford Road Charlotte, NC 28216 Sexually Transmitted Diseases, HIV, & AIDS: Syphilis and HIV/AIDS Reporting Other STD Reporting Mecklenburg County Health Department 700 N. Tryon Street, Suite 214 Charlotte, NC 28202 980-314-9470 FAX 704.432.2493 704-336-3349 or FAX 704-614-2993 704-432-1742 704.336.6200 All Other Reportable Communicable Diseases including Viral Hepatitis A, B & C: Report to any of the following nurses: Freda Grant, RN 704.336.6436 Brian Lackey, RN 704.336.5498 Elizabeth Quinn, RN 704.336.5398 Belinda Worsham, RN 704.336.5490 Vacant 704.353.1270 Shawn Wilson, RN (CD & child care) 704.432-1975 Vacant 704-432-4667 Julie Secrest, RN 704-432-0069 Communicable Disease Control FAX 704.353.1202 Mecklenburg County Health Department 700 N. Tryon Street, Suite 271 Charlotte, NC 28202 Public Health Emergency 24/7 704-432-0871 Animal Bite Consultation / Zoonoses / Rabies Prevention: Jose Pena Communicable Disease Control Mecklenburg County Health Department 700 N. Tryon Street, suite 214 Charlotte, NC 28202 State Veterinarian State after hours FAX 704.336.6440 704.353-1202 919.733-3410 919.733.3419 Suspected Food borne Outbreaks / Restaurant, Lodging, Pool and Institutional Sanitation: Food & Facilities Sanitation (Mon-Fri) 704.336.5100 Mecklenburg County Health Department (evenings; Sat/Sun) 704.432.1054 700 N. Tryon Street, Suite 208 (pager evenings; Sat/Sun) 704.580.0666 Charlotte, NC 28202 FAX 704.336.5306 Revised 1-28-16