Use of Diuretics in Elderly Patients with Congestive Heart Failure
advertisement

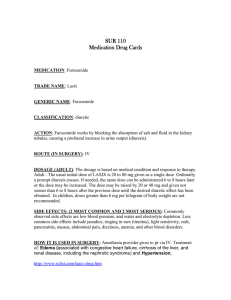
Use of Diuretics in Elderly Patients with Congestive Heart Failure Sean Ryan Atkins, Lilian M. Azzopardi, Anthony Serracino-Inglott Department of Pharmacy, Faculty of Medicine and Surgery, University of Malta, Msida, Malta satk0001@um.edu.mt Background University of Malta Objectives Diuretics are essential for symptomatic relief when fluid retention is present To classify and analyse loop diuretic dose management; in congestive heart failure (CHF). The dose of loop diuretics should be To evaluate pharmacist intervention in CHF by investigating diuretic decreased to the minimum required to maintain a fluid-free state after excess use in the clinical setting. fluid loss is achieved.1,2 Setting and Method 1. Ethics committee approval from St. Vincent de Paul Residence (SVPR), Rehabilitation Hospital Karin Grech Desirable scenarios (RHKG) and the University Research Ethics Committee was obtained prior to initiating the study. Dose decreased to lowest possible (i.e. 0.5 mg) Dose decreased to low dose (1 mg) 2. The medical records of patients over 65 years of age, who had suffered from past episodes of CHF over a Trial to decrease dose performed but had to increase again No dose change (low dose - 1 mg) period of eighteen months, were consulted. Dose was already at lowest possible (i.e. 0.5 mg) Diuretic removed 3. The relevant data was collected via a formulated patient profile. Undesirable scenarios 4. Patients were chosen by convenience sampling and were classified into two groups to evaluate pharmacist Dose decreased but remained high dose > 1 mg No dose change (high dose > 1 mg) intervention: Dose increased The control group (n1=54) from SVPR where there is no clinical pharmacy service; and Figure 1: Classification system The intervention group (n2=59) from RHKG where a clinical pharmacist actively participates together with the healthcare team. 5. The management of the loop diuretic dose for each patient was either classified as being desirable or undesirable according to the formulated classification system for the study (Figure 1). The classification system exhausts all possible scenarios with the: Undesirable consisting of those scenarios where patients have doses higher than 1 mg bumetanide (or its equivalent as furosemide); and Desirable consisting of those scenarios where patients have doses lower than 1 mg or where attempts were made to decrease the dose but had to increase again. 6. Data was analysed using IBM SPSS® Statistics version 19.0. Results A considerable number of the patients (n1=23; n2=28) lied within the The side effect of hyponatraemia tended to occur at doses higher than the undesirable category, with the control group proportion being 42.6% established 1 mg threshold used in the study. This association was more and that of the intervention group being 47.5% (Figure 2). There was apparent in patients at RHKG. The category which had the highest number no statistically significant difference in loop diuretic dose management of patients in both institutions was when the dose was between 1.5 and 4 mg between the institutions (p=0.604). daily bumetanide dose. The proportion of RHKG patients (60%) (n2=9) suffering from hyponatraemia at this dose range was greater than that of SVPR patients (50%) (n1=4). (Figure 3). Figure 2: Bar chart showing institution proportions of desirable and undesirable categories Figure 3: Bar chart showing incidence of hyponatraemia and daily bumetanide dose Conclusion This study highlights the need to emphasise clinical pharmacist intervention to follow appropriate loop diuretic dose management as most patients unnecessarily remained on a high dose. High diuretic doses were more likely to predispose patients to hyponatraemia. References 1. Dickstein K, Cohen-Solal A, Fillipatos G, McMurray JJV, Ponikowski P, Poole-Wilson PA et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008. Eur Heart J 2008; 29(19): 23882442. 2. McMurray JJV, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012. Eur Heart J 2012; 33(14): 1787-1847.