Deep Brain Stimulation: Surgical Process Kia Shahlaie, MD, PhD
advertisement

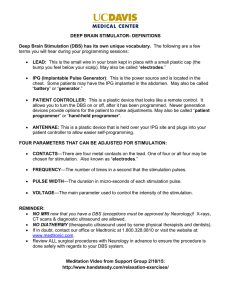
Deep Brain Stimulation: Surgical Process Kia Shahlaie, MD, PhD Assistant Professor Bronte Endowed Chair in Epilepsy Research Director of Functional Neurosurgery Minimally Invasive Neurosurgery Department of Neurological Surgery University of California, Davis UC Davis Deep Brain Stimulation Program Outline • Brief history • Basal ganglia review – Physiology (rate model) – Parkinson’s disease • DBS Procedure – Step 1: direct, indirect, physiological targeting – Step 2: pulse generator implantation • Postop care and outcomes – Programming – Risks and benefits of DBS UC Davis Deep Brain Stimulation Program Irving Cooper (1922‐1985) • Born in Atlantic City, NJ – Son of a salesman – Worked his way through school • BA, MD, MS, PhD, NSG residency – Faculty at NYU, then NYMC • Pioneer in functional neurosurgery – Anterior choroidal artery ligation… Cooper IS: Parkinsonism: Its Medical and Surgical Therapy. Springfield, Ill: Charles C Thomas, 1961 UC Davis Deep Brain Stimulation Program What do the basal ganglia do? • Scale Movement – amplitude and velocity • Focus Movement – select specific muscles – suppress antagonist muscles H Y P E R D I R E C T I N D I R E C T D I R E C T • Rate Model: Direct: Facilitate “wanted” movements Indirect: Inhibit “unwanted” movements UC Davis Deep Brain Stimulation Program Rate Model THALAMOCORTEX STRIATUM BASAL GANGLIA GPi UC Davis Deep Brain Stimulation Program Rate model explains kinetic disorders Hypokinetic disorders: Hyperkinetic disorders: Parkinson’s disease Dystonia, hemiballism, HD Delong, TINS 1990:13, 281‐285 UC Davis Deep Brain Stimulation Program Focused excitation/surround inhibition model of BG function I N D I R E C T D I R E C T Mink Prog Neurobiol 1996 H Y P E R D I R E C T Nambu Neurosci Res 2002 UC Davis Deep Brain Stimulation Program Rate model provided the rationale for basal ganglia surgery in PD • Loss of DA input to striatum – Direct pathway is underactive – Indirect pathway is overactive – NET: Excess inhibition of thalamocortical relay • Nuclei that are overactive in PD – STN (driving the GPi) – GPi (inhibiting the thalamus) X X UC Davis Deep Brain Stimulation Program GPi and STN are overactive in PD Loss of dopaminergic activity results in disinhibition of the STN and GPi STN GPi normal: PD: UC Davis Deep Brain Stimulation Program DBS Surgery for PD • Indications – – – – Clear diagnosis of idiopathic PD Continued good motor response to dopamine Motor fluctuations and dyskinesias from meds Independent ambulation in best “on” state • Contraindications – – – – Dementia Age > 80years (?) Poor function in best “on” state Poor MD/patient relationship • Unilateral/bilateral – Cognitive status, laterality of symptoms UC Davis Deep Brain Stimulation Program Goals of DBS surgery • Primum non nocere! – “elective” operation AXIAL PLANE Brain Brain Orientation Orientation • Accurate implantation Zona incerta STN – Location, location, location – Awake, stereotactic surgery 1) 2) 3) SNc SNr Medial lemniscal pathway Red nucleus CN III CN III nerve roots nerve roots Oculomotor Oculomotor nucleus nucleus CNIIIIII ofofCN Indirect targeting Direct targeting Physiological targeting – Microelectrode recording/mapping – Test stimulation • Adjustable, reversible system UC Davis Deep Brain Stimulation Program DBS Surgery Steps 1) Indirect targeting 2) Direct targeting 3) Physiological targeting UC Davis Deep Brain Stimulation Program Indirect Targeting Develop 3D coordinate system Define AC, PC, and 3 midline points 3D map with MCP at 0,0,0mm UC Davis Deep Brain Stimulation Program Indirect Targeting Select target based on atlas data Vectors STN X (lateral) 12mm Y (ant/post) ‐3mm Z (sup/inf) ‐4mm UC Davis Deep Brain Stimulation Program Direct Targeting Revise based on direct visualization, internal landmarks Along anterior edge of red nucleus on axial 3mm lateral to edge of red nucleus 2mm below superior edge of red nucleus UC Davis Deep Brain Stimulation Program Direct Targeting Select entry point and trajectory Entry ‐ Avoid cortical veins ‐ Enter crest of gyrus ‐ Burr hole location Trajectory ‐ ‐ ‐ ‐ Avoid sulci Avoid ventricle Avoid subependyma Avoid major parenchymal vessels UC Davis Deep Brain Stimulation Program Day of surgery… Merge Head frame placed Localizer box with MRI using local used for CT – plan anesthesia provides fiducials Patient placed in comfortable position, then sedated UC Davis Deep Brain Stimulation Program DBS Surgery Prepped and draped. Incision and burr hole placed. Stereotactic head frame set to proper coordinates mER with patient awake UC Davis Deep Brain Stimulation Program Physiological Targeting: mER Subthalamic nucleus (STN) Globus pallidus internus (GPi) Goal: Dorsolateral motor territory of STN Goal: Posterior motor territory of GPi ‐‐ leg area is medial ‐‐ arm area is lateral ‐‐ leg area is dorsal/medial ‐‐ arm area is ventral/lateral UC Davis Deep Brain Stimulation Program Physiological Targeting: Test Stimulation Subthalamic nucleus (STN) Globus pallidus internus (GPi) UC Davis Deep Brain Stimulation Program Interpreting STN Test Stimulation Error Structures Side effect Too lateral IC: CBT IC: CST Dysarthria Tonic contractions FEF fibers Contra gaze dev CN3 Red nucleus Diplopia Paresthesia, flush Limbic STN Personality Too medial Too posterior Too anterior Zona incerta STN Med Lemnisc Parasthesia SNc SNr IC: CST IC: CBT Tonic contractions Dysarthria Hypothalam Flushing Medial lemniscal pathway Red nucleus CN III CN III nerve roots nerve roots Oculomotor Oculomotor nucleus nucleus ofofCN CNIIIIII UC Davis Deep Brain Stimulation Program Intraoperative Imaging: iCT Standard OR, equipment, surgical technique; awake surgery with mER UC Davis Deep Brain Stimulation Program Post‐implantation MRI Subthalamic nucleus (STN) Globus pallidus internus (GPi) UC Davis Deep Brain Stimulation Program Hospital stay: 1 night UC Davis Deep Brain Stimulation Program Stimulator Implantation Outpatient surgery (same day discharge, general anesthesia) UC Davis Deep Brain Stimulation Program Clinic follow‐up for programming Physician programmer monopolar C+/1‐ Bipolar 0‐/1+ Patient programmer Contacts/monopolar/bipolar Voltage Frequency Pulsewidth UC Davis Deep Brain Stimulation Program Benefits of DBS for PD ~ 30% improvement in motor scores ~ 40% improvement in ADL scores ~ 50% reduction in PD medication needs DBS is typically as effective as “best” dopamine response… Likely to improve: Tremor Rigidity (tightness) Bradykinesia (slowness) Dystonia Dyskinesia* Unlikely to improve: • Gait instability / falls • Freezing of gait • Speech • Swallow • Cognitive deficits UC Davis Deep Brain Stimulation Program Risks of DBS surgery • Infection: 5‐10% • ICH/hemorrhage: 2‐4% • Neurological deficit: <1% from Starr PA and Silay C, 2008 UC Davis Deep Brain Stimulation Program