Assessment of Sexual Health Risk Factors among Deaf American Sign Language (ASL) Users
1
2
2
2-4
Erica Heiman, MD, MS , Alicia Lane-Outlaw, BS , Sharon Haynes, LMSW , Michael McKee, MD, MPH
1 Department of Internal Medicine, University of California, Davis Medical Center, Sacramento, CA
2 Deaf Health Community Committee, Rochester, NY
3 Department of Family Medicine, University of Rochester School of Medicine and Dentistry, Rochester, NY
4 National Center for Deaf Health Research, University of Rochester School of Medicine and Dentistry, Rochester, NY
Background
• The number of Americans who use American Sign
Language (ASL) as a primary language is approximately
500,000.
• Members of the Deaf community face barriers to
prevention and treatment of medical illnesses due to low
access to high-quality health information in ASL and poor
cultural and language concordance with health care
providers.
• Previous studies suggest that Deaf ASL users struggle with
poorer sexual health knowledge than the general
population but little is known if Deaf ASL users engage in
riskier sexual behaviors.
Objectives
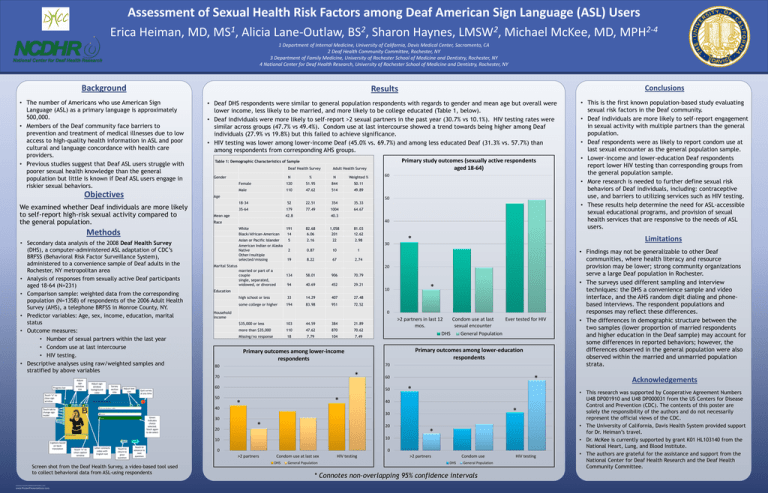
• Deaf DHS respondents were similar to general population respondents with regards to gender and mean age but overall were
lower income, less likely to be married, and more likely to be college educated (Table 1, below).
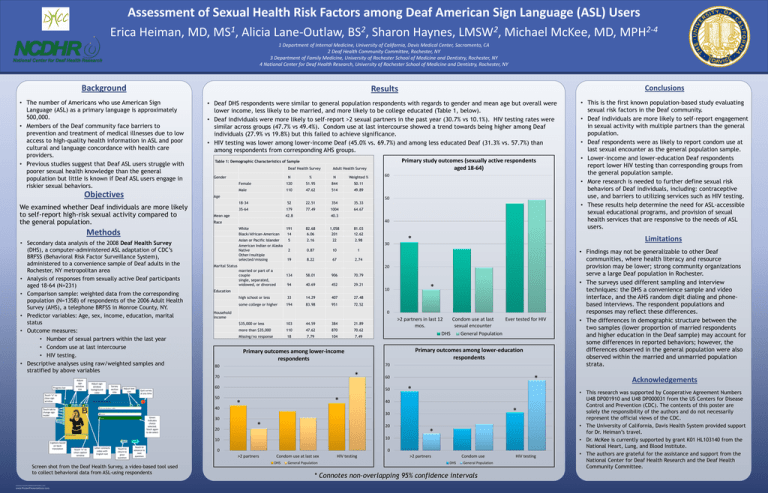
• Deaf individuals were more likely to self-report >2 sexual partners in the past year (30.7% vs 10.1%). HIV testing rates were
similar across groups (47.7% vs 49.4%). Condom use at last intercourse showed a trend towards being higher among Deaf
individuals (27.9% vs 19.8%) but this failed to achieve significance.
• HIV testing was lower among lower-income Deaf (45.0% vs. 69.7%) and among less educated Deaf (31.3% vs. 57.7%) than
among respondents from corresponding AHS groups.
Deaf Health Survey
Adult Health Survey
N
%
N
Weighted %
Female
120
51.95
844
50.11
Male
110
47.62
514
49.89
Gender
18-34
52
22.51
354
35.33
35-64
179
77.49
1004
64.67
Mean age
42.8
Asian or Pacific Islander
American Indian or Alaska
Native
Other/multiple
selected/missing
191
14
82.68
6.06
1,058
201
81.03
12.62
5
2.16
22
2.98
2
0.87
10
1
19
8.22
67
2.74
Marital Status
Survey
section
title
Adjust text
size
Touch “x” to
close sign
window
Quit survey
at any time
married or part of a
couple
single, separated,
widowed, or divorced
134
58.01
906
70.79
94
40.69
452
29.21
Captions based
on backtranslation
high school or less
33
14.29
407
27.48
some college or higher
194
83.98
951
72.52
0
Household
income
$35,000 or less
103
44.59
384
21.89
more than $35,000
110
47.62
870
70.62
Missing/no response
18
7.79
104
7.49
www.PosterPresentations.com
>2 partners in last 12
Condom use at last
Ever tested for HIV
mos.
sexual encounter
DHS
General Population
Primary outcomes among lower-education
respondents
Primary outcomes among lower-income
respondents
70
80
*
60
40
50
*
*
*
60
*
40
*
30
Green
indicates
choice
selected.
Touch again
to de-select
Touch “x” to
close caption
window
Letter connects
video with
English text
Touch to
return to
prior
question
Touch to
advance to
next
question
Screen shot from the Deaf Health Survey, a video-based tool used
to collect behavioral data from ASL-using respondents
RESEARCH POSTER PRESENTATION DESIGN © 2012
*
10
Education
50
Touch tab to
change sign
model
30
30
20
*
20
10
10
0
0
>2 partners
Condom use at last sex
DHS
General Population
HIV testing
• This is the first known population-based study evaluating
sexual risk factors in the Deaf community.
• Deaf individuals are more likely to self-report engagement
in sexual activity with multiple partners than the general
population.
• Deaf respondents were as likely to report condom use at
last sexual encounter as the general population sample.
• Lower-income and lower-education Deaf respondents
report lower HIV testing than corresponding groups from
the general population sample.
• More research is needed to further define sexual risk
behaviors of Deaf individuals, including: contraceptive
use, and barriers to utilizing services such as HIV testing.
• These results help determine the need for ASL-accessible
sexual educational programs, and provision of sexual
health services that are responsive to the needs of ASL
users.
Limitations
*
20
70
Progress bar
50
40
Methods
Adjust sign
window
background
color
60
40.3
Race
White
Black/African-American
• Secondary data analysis of the 2008 Deaf Health Survey
(DHS), a computer-administered ASL adaptation of CDC’s
BRFSS (Behavioral Risk Factor Surveillance System),
administered to a convenience sample of Deaf adults in the
Rochester, NY metropolitan area
• Analysis of responses from sexually active Deaf participants
aged 18-64 (N=231)
• Comparison sample: weighted data from the corresponding
population (N=1358) of respondents of the 2006 Adult Health
Survey (AHS), a telephone BRFSS in Monroe County, NY.
• Predictor variables: Age, sex, income, education, marital
status
• Outcome measures:
• Number of sexual partners within the last year
• Condom use at last intercourse
• HIV testing.
• Descriptive analyses using raw/weighted samples and
stratified by above variables
Primary study outcomes (sexually active respondents
aged 18-64)
Table 1: Demographic Characteristics of Sample
Age
We examined whether Deaf individuals are more likely
to self-report high-risk sexual activity compared to
the general population.
Adjust
sign
window
size
Conclusions
Results
*
>2 partners
Condom use
DHS
General Population
* Connotes non-overlapping 95% confidence intervals
HIV testing
• Findings may not be generalizable to other Deaf
communities, where health literacy and resource
provision may be lower; strong community organizations
serve a large Deaf population in Rochester.
• The surveys used different sampling and interview
techniques: the DHS a convenience sample and video
interface, and the AHS random digit dialing and phonebased interviews. The respondent populations and
responses may reflect these differences.
• The differences in demographic structure between the
two samples (lower proportion of married respondents
and higher education in the Deaf sample) may account for
some differences in reported behaviors; however, the
differences observed in the general population were also
observed within the married and unmarried population
strata.
Acknowledgements
• This research was supported by Cooperative Agreement Numbers
U48 DP001910 and U48 DP000031 from the US Centers for Disease
Control and Prevention (CDC). The contents of this poster are
solely the responsibility of the authors and do not necessarily
represent the official views of the CDC.
• The University of California, Davis Health System provided support
for Dr. Heiman’s travel.
• Dr. McKee is currently supported by grant K01 HL103140 from the
National Heart, Lung, and Blood Institute.
• The authors are grateful for the assistance and support from the
National Center for Deaf Health Research and the Deaf Health
Community Committee.