Not A Reject – A Falsely Elevated Cardiac Troponin in... Transplant Recipient Nicholas Wettersten, MD; Kathleen Tong, MD
advertisement

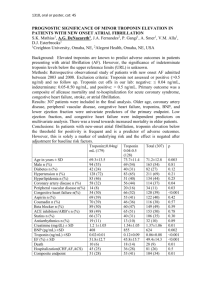
Not A Reject – A Falsely Elevated Cardiac Troponin in a Heart Transplant Recipient Nicholas Wettersten, MD; Kathleen Tong, MD University of California, Davis Medical Center; Sacramento, CA Investigational Studies Introduction Medications • • • • • Mycophenolate 360 mg BID • Fludrocortisone 0.1 mg daily Tacrolimus 3.5 mg BID • Duloextine 30 mg daily Carvedilol 3.125 mg BID • Mirtazapine 30 mg qhs Aspirin 81 mg daily • Lamotrigine 75 mg daily Trimethoprim/Sulfamethoxazole 160/800 mg M, W, F Past Medical History • • • • • Catecholamine Mediated Polymorphic Ventricular Tachycardia Orthotopic Heart Transplantation (with daclizumab induction) Asthma Polysubstance Abuse Mood Disorder, NOS Family History • Non-contributory Social History • Smokes 0.5-1 packs every day for 5 years • Occasional alcohol use • Intermittent use of marijuana and methamphetamine after transplantation Physical Exam Blood pressure: 112/50 mmHg; Heart Rate: 70/min General: No acute distress. Cardiac exam: Regular rate and rhythm, S1 and S2 Lung exam: Clear to auscultation bilaterally Extremities: No edema or cyanosis Luminescent Signal No Troponin Present Heterophilic Antibody Found Steroid Burst Started “Capture” Antibody Repeat Biopsy 30 Troponin 20 10 9/2/12 8/2/12 7/2/12 6/2/12 5/2/12 4/2/12 3/2/12 2/2/12 1/2/12 12/2/11 11/2/11 10/2/11 9/2/11 8/2/11 7/2/11 6/2/11 5/2/11 Confirmed Interference 4/2/11 “Signal” Antibody Heterophilic Antibody First Cardiac Catheterization and Biopsy 0 History • A 23 year old man presented with chest pain to an outside ER where his first troponin was <0.01 ng/ml and he was transferred to our institution for further evaluation • Five years prior he had undergone orthotopic heart transplantation for catecholamine mediated polymorphic ventricular tachycardia • Post-transplant he displayed maladaptive behavior with intermittent compliance to immunosuppressive therapy and frequent presentations to Emergency Rooms (ER) with syncope and chest pain. Evaluations did not identify any cause for these recurrent symptoms. 40 3/2/11 Case Presentation Troponin I/T Molecule 50 2/2/11 • • To recognize the implications of a positive troponin in a heart transplant patient To learn how heterophilic antibodies interfere with immunoassays To learn other causes of interference in the troponin assay Repeat Catheterization, Biopsy, and more Steroids 1/2/11 • 60 12/2/10 Learning Objectives Average Troponin Value For Date of Evaluation Troponin Measured (ng/ml) In cardiac transplant medicine, an elevated troponin may be a sign of organ rejection. This may prompt invasive testing and increased immunosuppression with significant risks and side effects. This series of events stems from a positive troponin, which can sometimes be falsely elevated. Assay Container Date of Evaluation Graph displaying mean troponin value measured during different presentations to our hospital. Highlighted on graph are key events. Cardiac Catheterization 11/11: No coronary artery disease Endomyocardial Biopsy 11/11: Mild to moderate rejection Tacrolimus level: 5.7 (target 8.5-10) Endomyocardial Biopsy 12/11: Mild chronic rejection Cardiac Catheterization 3/12: No coronary artery disease Endomyocardial Biopsy 3/12: Mild chronic rejection Tacrolimus level: 12.5 Troponin - UCD: 40.33 ng/ml; Heterophil Antibody Block: 0.06 ng/ml Troponin - UCD : 1.41 ng/ml; Other Hospital (different assay): <0.01 ng/ml Multiple echocardiograms over admissions showed preserved LV function Clinical Course • 11/11: Initial troponin 22.9 ng/ml, patient underwent cardiac catheterization and endomyocardial biopsy and tacrolimus level measured. Augmentation of immunosuppression deferred after discussion with transplant center. • 12/11: Repeat endomyocardial biopsy at transplant institution • 1/12: Elevated troponin, steroid burst of prednisone 60 mg started • 3/12: Troponin higher than measurable, repeat cardiac catheterization and endomyocardial biopsy performed and second steroid burst started • 5/12: Troponin measured 40 ng/ml, suspicion of assay interference and sample sent for testing with a heterophilic antibody blocking reagent, which measured troponin at 0.06 ng/ml strongly suggesting heterophilic antibody interference. • 7/12: Presented to outside ER with troponin of 0.1 ng/ml then 0.04 ng/ml. Transferred to UC Davis. Troponin measured 1.4 ng/ml. Sample sent to first hospital for measurement. No troponin detected confirming interference. Potentially Interfering Conditions Causing False Positive Troponin Heterophilic Antibodies Alkaline Phosphatase Fibrin Inadequate Washing Hemolysis Macrotroponin Rheumatoid Factor Infection with Legionella Table Conditions and substances that can interfere with troponin assay and cause a false positive. Figure Left: Example of normal immunoassay function with troponin captured by one antibody and a second antibody binds captured troponin to signal presence. Right: With a heterophilic antibody, it can bind both capture and signal antibody making it seem troponin is present when it is not. Discussion • Elevated cardiac troponin in a heart transplant recipient may be from: • Ischemia • Rejection with injury of vasculature and ischemia • Rejection with injury to myocardium • Troponin is measured by an immunoassay • Immunoassays commonly use a “two-site sandwich” • A “capture” antibody binds troponin floating in serum • A “signal” antibody is added and binds the captured troponin to signal the presence of troponin • The intensity of light emitted correlates with the amount of troponin present • Immunoassays are prone to various forms of interference • Multiple different substances and conditions have been shown to cause false positive troponins (see Table) • It is estimated between 0.4 and 3.1% of troponin measurements are false positives • A heterophilic antibody describes a type of antibody that displays weak and non-specific binding, often with broad reactivity • Sometimes they display stronger targeted binding, often in individuals previously exposed to a specific antigen • Provoking factors that can induce a heterophilic antibody include: • Clinical therapeutics • Blood transfusions • Vaccinations • Exposure to animals • Ingestions • The patient had Daclizumab, a humanized mouse anti-interleukin-2receptor antibody, at time of transplantation potentially inducing heterophilic antibodies • This case highlights the need to consider laboratory interference when other clinical parameters do not support laboratory results References • McNeil A. The trouble with Troponin. Heart, lung & circulation. 2007;16 Suppl 3:S13-16. • McClennen S, Halamka JD, Horowitz GL, Kannam JP, Ho KK. Clinical prevalence and ramifications of falsepositive cardiac troponin I elevations from the Abbott AxSYM Analyzer. Am J Cardiol. May 1 2003;91(9): 1125-1127. • Fleming SM, O'Byrne L, Finn J, Grimes H, Daly KM. False-positive cardiac troponin I in a routine clinical population. Am J Cardiol. May 15 2002;89(10):1212-1215. • Kricka LJ. Human anti-animal antibody interferences in immunological assays. Clinical chemistry. Jul 1999;45(7):942-956. • Garcia-Mancebo ML, Agullo-Ortuno MT, Gimeno JR, Navarro-Martinez MD, Ruiz-Gomez J, Noguera-Velasco JA. Heterophile antibodies produce spuriously elevated concentrations of cardiac Troponin I in patients with Legionella pneumophila. Clinical biochemistry. Jun 2005;38(6):584-587.

![Anti-Cardiac Troponin C antibody [12G3] ab10245 Product datasheet 1 Abreviews 2 Images](http://s2.studylib.net/store/data/012743017_1-6280d857c670e9b06dd3ff32e4e3ba81-300x300.png)