Identifying cortical visual dysfunction in Posterior Cortical Atrophy Timothy J. Shakespeare
advertisement
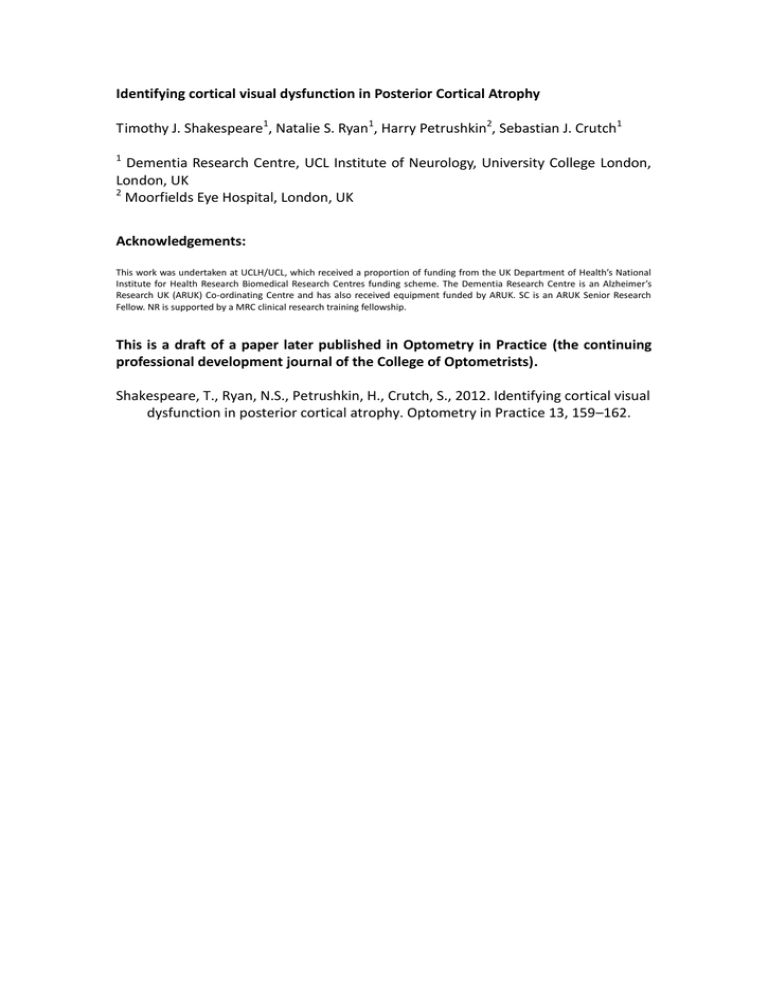
Identifying cortical visual dysfunction in Posterior Cortical Atrophy Timothy J. Shakespeare1, Natalie S. Ryan1, Harry Petrushkin2, Sebastian J. Crutch1 1 Dementia Research Centre, UCL Institute of Neurology, University College London, London, UK 2 Moorfields Eye Hospital, London, UK Acknowledgements: This work was undertaken at UCLH/UCL, which received a proportion of funding from the UK Department of Health’s National Institute for Health Research Biomedical Research Centres funding scheme. The Dementia Research Centre is an Alzheimer’s Research UK (ARUK) Co-ordinating Centre and has also received equipment funded by ARUK. SC is an ARUK Senior Research Fellow. NR is supported by a MRC clinical research training fellowship. This is a draft of a paper later published in Optometry in Practice (the continuing professional development journal of the College of Optometrists). Shakespeare, T., Ryan, N.S., Petrushkin, H., Crutch, S., 2012. Identifying cortical visual dysfunction in posterior cortical atrophy. Optometry in Practice 13, 159–162. Abstract Posterior Cortical Atrophy is a degenerative condition most frequently caused by Alzheimer’s disease leading to atrophy of the occipital and parietal cortices. Though often considered to be a rare condition, PCA is likely under diagnosed. Its existence is not well recognised and unusual early symptoms may be misattributed to anxiety or malingering. Early complaints include reading difficulties or problems localising or identifying objects, and patients often first consult an optometrist or ophthalmologist for primary investigation of the problem. This provides the opportunity to highlight from the outset that the problem is likely to be due to higher cortical dysfunction and to recommend a neurological referral. Detailed neurological and neuropsychological assessment along with an MRI scan will aid diagnosis. Current symptomatic treatment and future disease modifying therapies rely on early and accurate diagnosis, reinforcing the need for better awareness of the condition. Introduction Posterior cortical atrophy (PCA) is an early-onset dementia syndrome in which cortical degeneration leads to perceptual dysfunction. It is most commonly, although not exclusively caused by Alzheimer’s disease (AD). Unlike ‘typical’ amnestic AD, the histopathological burden (amyloid plaques and neurofibrillary tangles) is in the parietal and occipital lobes (Levine, Lee, & Fisher, 1993; Tang-Wai et al., 2004) causing brain shrinkage (atrophy) in these regions (see Figure 1) and corresponding deficits in visuospatial and visuoperceptual processing (Lehmann et al., 2011), whilst episodic memory and insight are relatively preserved (Tang-Wai et al., 2004). PCA is often referred to as the visual variant of AD or biparietal AD. The earliest symptoms of PCA often relate to vision, so patients often consult their optometrist prior to seeking medical attention via their GP. In a number of cases, an abnormal visual field test and history of cortical visual dysfunction in the absence of significant eye disease has alerted the optometrist to the possibility of a neurological disorder, resulting in a fast track to accurate diagnosis. In some cases, if an eye examination is normal, or reveals only mild cataracts that would not usually cause significant visual dysfunction, patients may be reassured and discharged. As their symptoms persist, they may subsequently receive a diagnosis of anxiety, depression or malingering. Early diagnosis and referral to a neurologist are crucial for effective treatment and care in PCA, as with other dementias (Leifer, 2003). How do people with PCA present to an optometrist? Typical early symptoms include difficulties with reading; patients may lose their place at the end of a line or find that the words appear to float off the paper. They may complain of difficulty locating objects, they mis-reach for, or are unable to find objects that are right in front of them. They may also have trouble judging distance, depth and volume. This manifests with problems when driving such as clipping wing mirrors or veering out of the lane. They may perceive patterns on the road or floor as threedimensional. Patients may walk into low objects and become lost in both new and familiar environments. Negotiating stairs, escalators and shiny floors is often particularly taxing. Early non-visual symptoms include difficulty with other parietal lobe functions such as calculation, spelling and praxis. A small proportion of patients with PCA experience visual hallucinations and/or motor deficits similar to those seen in Parkinson’s disease. A minority of patients also develop problems in language production - particularly reduced or slowed speech and impaired naming. In contrast to these deficits, episodic memory and insight into the condition remain relatively spared until late into the disease process, as does general cognitive reasoning. What causes PCA? Alzheimer’s disease is the most common underlying pathology, but cases due to Lewy body disease and Cortico-Basal Degeneration (CBD) have been described (Renner et al., 2004; Tang-Wai et al., 2004). Visual hallucinations and Parkinsonian features may be associated with PCA due to Lewy body disease, whilst asymmetric Parkinsonism may be suggestive of CBD. In practice, Alzheimer’s disease and Lewy body pathology often co-occur at post mortem (Hamilton, 2000). Whilst exact prevalence and incidence of PCA are unknown, a study of AD patients at a UK specialist centre reported 5% with a visual presentation (Snowden et al., 2007). This is likely to be an underestimation of the prevalence in the population due to poor awareness of the condition. The age of disease onset in PCA (typically late 50s and early 60s; McMonagle, Deering, Berliner, & Kertesz, 2006; Mendez, Ghajarania, & Perryman, 2002) tends to be earlier than that of tAD, but may range from 40 to 86 years (Tang-Wai et al., 2004). Patients with PCA also differ in terms of genetic risk. The ApoE ε4-allele is associated with a greater risk of typical AD, however studies show lower frequency of the ε4-allele in patients with PCA than typical AD (Schott et al., 2006; Snowden et al., 2007). Despite the young age at onset, PCA presentations of familial AD have not been reported (Ryan & Rossor, 2010). If there is a family history, genetic testing for mutations in the prion protein gene may sometimes be considered as early visual processing deficits may occur in some forms of familial prion disease. How is PCA diagnosed? Diagnostic criteria for PCA are show in Table 1. Visual acuity and examination of the eye tend to be normal in PCA (Lee & Martin, 2004). Visual field tests often show areas of reduced visual sensitivity, particularly bilateral constriction, but not complete visual loss (Lee & Martin, 2004). Interpretation of these results should be undertaken with caution as a reduced effective field of vision (Mannan, Kennard, & Husain, 2009) and spatial disorientation may contribute to poor performance, and results are often inconsistent and unreliable. Similarly, the Ishihara colour plates have reduced validity in PCA as the requirements of intact form and number perception are not met. The Cortical Visual Screening Test (CORVIST; James-Galton, Plant, & Warrington, 2001) has a number of tests that aid the diagnosis of a cortical visual disturbance, such as shape discrimination, shape detection, dot counting and fragmented numbers. Simply asking whether a patient can see fragmented letters can immediately suggest a visuoperceptual deficit (see Figure 2). PCA can be differentiated from cortical visual loss due to stroke by the insidious onset of symptoms in the history and lack of acute episode. If PCA is suspected, referral to a Neurologist with an interest in dementia is recommended. Typical investigations include formal neuropsychology testing and an MRI scan. As PCA patients tend to be relatively young, investigations to exclude reversible causes of dementia may be undertaken, including blood tests, EEG and sometimes lumbar puncture. In specialist centres, analysis of cerebrospinal fluid levels of the proteins tau and amyloid-β can support an underlying diagnosis of AD (Baumann et al., 2010). Patients with PCA often derive significant symptomatic benefit from treatment with a cholinesterase inhibitor. A multi-disciplinary team approach is imperative to ensure that appropriate support is provided. They must be advised to inform the DVLA of their diagnosis of PCA and it may be appropriate for them to be registered as partially sighted. Conclusion PCA is a dementia syndrome characterised by impaired processing of visual stimuli with relatively preserved memory and an early age of onset. Patients may be referred to an optometrist, and it is important to rule out ocular disease as the cause of the problem, and ensure that long or short sightedness is corrected as far as possible. The prognosis for PCA is thought to be similar to typical AD although there are no formal estimates of disease duration and variation in clinical phenotype towards the end stages. Early diagnosis enables the patient and family to plan for the future, and improves the chance of effective treatment, which will be especially important as new therapies with the potential for disease modification are developed in the future. References Baumann, T. P., Duyar, H., Sollberger, M., Kuhle, J., Regeniter, A., Gomez-Mancilla, B., Schmidtke, K., et al. (2010). CSF-tau and CSF-Abeta(1-42) in posterior cortical atrophy. Dementia and geriatric cognitive disorders, 29(6), 530-3. Hamilton, R. L. (2000). Lewy bodies in Alzheimer’s disease: a neuropathological review of 145 cases using alpha-synuclein immunohistochemistry. Brain pathology, 10(3), 378-84. James-Galton, M., Plant, G., & Warrington, E. (2001). The cortical vision screening test (CORVIST). London: Thames Valley Test Company. Lee, A. G., & Martin, C. O. (2004). Neuro-ophthalmic findings in the visual variant of Alzheimer’s disease. Ophthalmology, 111(2), 376-80. Lehmann, M., Crutch, S. J., Ridgway, G. R., Ridha, B. H., Barnes, J., Warrington, E. K., Rossor, M. N., et al. (2011). Cortical thickness and voxel-based morphometry in posterior cortical atrophy and typical Alzheimer’s disease. Neurobiology of aging, 32(8), 1466-76. Leifer, B. P. (2003). Early diagnosis of Alzheimer’s disease: clinical and economic benefits. Journal of the American Geriatrics Society, 51(5 Suppl Dementia), S281-8. Levine, D. N., Lee, J. M., & Fisher, C. M. (1993). The visual variant of Alzheimer’s disease: a clinicopathologic case study. Neurology, 43(2), 305-13. Mannan, S. K., Kennard, C., & Husain, M. (2009). The role of visual salience in directing eye movements in visual object agnosia. Current biology, 19(6), R2478. McMonagle, P., Deering, F., Berliner, Y., & Kertesz, A. (2006). The cognitive profile of posterior cortical atrophy. Neurology, 66(3), 331-8. Mendez, M. F., Ghajarania, M., & Perryman, K. M. (2002). Posterior cortical atrophy: clinical characteristics and differences compared to Alzheimer’s disease. Dementia and geriatric cognitive disorders, 14(1), 33-40. Renner, J. A., Burns, J. M., Hou, C. E., McKeel, D. W., Storandt, M., & Morris, J. C. (2004). Progressive posterior cortical dysfunction: a clinicopathologic series. Neurology, 63(7), 1175-80. Ryan, N. S., & Rossor, M. N. (2010). Correlating familial Alzheimer’s disease gene mutations with clinical phenotype. Biomarkers in medicine, 4(1), 99-112. Schott, J. M., Ridha, B. H., Crutch, S. J., Healy, D. G., Uphill, J. B., Warrington, E. K., Rossor, M. N., et al. (2006). Apolipoprotein e genotype modifies the phenotype of Alzheimer disease. Archives of neurology, 63(1), 155-6. Snowden, J. S., Stopford, C. L., Julien, C. L., Thompson, J. C., Davidson, Y., Gibbons, L., Pritchard, A., et al. (2007). Cognitive phenotypes in Alzheimer’s disease and genetic risk. Cortex, 43(7), 835-45. Tang-Wai, D. F., Graff-Radford, N. R., Boeve, B. F., Dickson, D. W., Parisi, J. E., Crook, R., Caselli, R. J., et al. (2004). Clinical, genetic, and neuropathologic characteristics of posterior cortical atrophy. Neurology, 63(7), 1168-74. Table 1. Diagnostic criteria for PCA (from Mendez et al. 2002) 1. Core diagnostic features (all must be present) a) Insidious onset and gradual progression b) Presentation with visual complaints with intact primary visual functions c) Evidence of predominant complex visual disorder on examination d) Elements of Balint’s syndrome e) Visual agnosia f) Dressing apraxia g) Environmental disorientation h) Proportionally less impaired deficits in memory and verbal fluency i) Relatively preserved insight with or without depression 2. Supportive diagnostic features a) Presenile onset b) Alexia c) Elements of Gerstmann’s syndrome d) Ideomotor apraxia e) Physical examination within normal limits f) Investigations Neuropsychology: predominantly impaired perceptual deficits Brain imaging: predominantly occipitoparietal abnormality (especially on functional neuroimaging) with relative sparing of frontal and mesiotemporal regions Figure 1 A. Sagittal T1 MRI sections of typical AD and PCA patients, with arrows indicating significant hippocampal (tAD) and parietal (PCA) atrophy. B. Regional percentage differences in cortical thickness in PCA compared with typical AD for the left and right hemisphere (from Lehmann et al., 2009). Colour scale represents magnitude of cortical thickness difference. Red and yellow (positive values) represent lower cortical thickness in PCA subjects compared with tAD, whilst dark to light blue (negative values) represent greater cortical thickness. Figure 2 Example stimuli used in neuropsychological testing of PCA. The stimulus on the left is a fragmented letter, a test of visuoperceptual ability. On the right is a number location stimulus, used to test visuospatial ability. The participant must say which number is in the same place as the dot.