posterior cortical atrophy PCA SuPPoRt GRouP www.pcasupport.ucl.ac.uk
advertisement

posterior cortical atrophy PCA support group www.pcasupport.ucl.ac.uk newsletter Welcome to the [PCA] Support Group Welcome to the PCA Support Group Newsletter. There have been two PCA Support Group meetings since the last newsletter was published. Following a change of venue, made necessary in light of the number of people who confirmed their likely attendance, we found ourselves on 22 January 2013, in a rather formal lecture theatre in the Institute of Neurology….fitted with all mod cons, including an examination couch…but not the most ‘cosy’ of venues to date! Having braved the snow and freezing temperatures, we welcomed Barbara Pointon MBE as a guest speaker to our carers’ meeting, along with two of our own group members who kindly prepared and delivered very informative presentations. Barbara spoke about her experiences as a carer for her husband Malcolm in a talk entitled: ‘Offering enlightened care and support to people with dementia’. Barbara is the widow of Malcolm Pointon, who was diagnosed with Alzheimer’s disease at the age of 51 and died in 2007. She knows first-hand the struggle that many Newsletter Issue 16, June 2013 people face to achieve the necessary care for people with dementia and has contributed to the debate on appropriate dementia care at many levels. Currently very active as a Government adviser on dementia and an advocate for dementia care, she is quoted as saying: “I now feel I might be in a position not to just whinge about problems but to do something to put things right - it’s such a wonderful legacy.” For her work campaigning for better care of those with Alzheimer’s disease, Barbara was included in the Queen’s Birthday Honours of June 2006 and awarded the MBE. Her presentation to the group was based on one which she has given in many venues and to multiple audiences. Roger Kelly and Peter Ledger are both members of the PCA Support Group and we are grateful to them for the information they shared at the meeting, sadly, borne out of personal experience. Roger Kelly provided an informative guide to the maze one must negotiate in “Non Means Tested Benefits”. Peter Ledger followed by presenting a very personal account of his journey through MEF myrtle ellis fund supporting rare dementia The PCA Support Group is generously supported by the Myrtle Ellis Fund, as part of The National Brain Appeal (Charity number 290173). For more information on the work of the Fund or to make your own contribution to the running costs of the PCA Support Group, please contact the Foundation on 020 3448 4724 1 intro cont’ the process of recognising the need for nursing home care and indeed then finding appropriate such care for his wife Margaret; “Identifying a Care/Nursing Home and accessing State Benefits - a personal experience.” A ‘PCA Research Update’ was presented by research fellows from the Dementia Research Centre: Tim Shakespeare, Ross Paterson and Keir Yong, followed by question and answer session. Details of the research they described are included in this newsletter. The meeting was enriched by the provision of written diary accounts from Bill McCammon and David Moon. Bill’s wife Pat sadly passed away in 2012 and we thank him for his candid sharing of the events during the two years prior to her death in July 2012. David cares for his wife Pat at home and above all, wanted to share the value he and Pat have enjoyed as a result of a dictaphone recording they made about their lives together. After lunchtime refreshments, we reconvened in smaller groups to contribute to a discussion about the particular service and care needs of younger people with dementia and, more specifically, with PCA. This discussion was preceded by a brief explanation from Robert Holman, a mental health commissioning officer in the London Borough of Camden, about the care commissioning process that exists there. Feedback from the discussions was shared at the meeting and will be collated, together with feedback from similar styled sessions that have since been conducted with other young onset dementia support groups. To quote David: “About a year ago, when Pat was still very lucid, we sat down with a little dictaphone and made a 20 minute recording about our lives together. I acted like an interviewer but basically we talked about all we could remember about our lives together. How we met, our marriage, jobs, homes, children, holidays, Pat’s books and so on. The final report will be made available via the support group networks. Having recently been to visit an inspiring team of people at a ‘Young People with Dementia’ group in West Berkshire, I am very excited at the prospect of a regional PCA support group meeting in Wokingham in the autumn. This meeting would be supported by staff as well as patient representatives and could hopefully be scheduled on a regular basis. More details to follow in the next newsletter, but do visit www.ypwd.info in the meantime for more information about this group. The recording has proved to be a lifeline and I must have used it a hundred times. Whenever Pat ‘loses it’ I play the tape and nine times out of ten it brings her back. She even participates by intervening and joining the discussion again as we listen. The technique has brought her back to ‘reality’ time and time again. I STRONGLY recommend this to all carers who care for someone who is still sufficiently lucid. It will prove invaluable to them in the coming months”. The results of the ‘My Requests’ workshop which Steve Lines facilitated during the Feb 2012 meeting have now been collated and incorporated into a new PCA support group leaflet: ‘Living with PCA’. There will be copies available at the July meeting. Alternatively, visit the website to download or contact Jill if you would like to receive one via post. Both diary accounts are available to read in this newsletter, with the kind permission of Bill and David. The 22 March 2013 meeting saw a welcome return to Wilkins Old Refectory, where despite one or two PA system difficulties (for which I apologise), we engaged in a somewhat more interactive presentation style than has previously been the case. 2 intro cont’ I have been encouraged on several counts recently, following my engagement with local and charitable organisations for visually impaired people. It would seem that there are a plethora of local, often volunteer-led services that provide a range of valuable facilities: recording local newspapers in an audio format; providing volunteers who will visit a person in their own home and assist with tasks that require visual accuracy; and completing paperwork or reading necessary documents. Forthcoming Meetings 5 July 2013: Wilkins Old Refectory, UCL, Gower St, London, WC1E 6BT. Time: 11.00am-2.30pm. Coffee available from 10.30am. Lunch included. Map details overleaf. Living Well with Cortical Visual Loss The agenda includes a presentation by Jane Norman, Director, Young Dementia UK Homes, the sister charity of Young Dementia UK. She outlines their plans to build a new home for young people with dementia in Oxfordshire, incorporating an ‘extra care’ model to provide individual apartments for around 12 people. Researchers at the Dementia Research Centre have submitted a grant application regarding the development of aids and strategies for helping people with dementia-related visual impairment including PCA. It would be useful to use this meeting to engage in further discussion to gather ideas about what would be most useful to patients and carers. 20 Sept 2013: Carers’ Only Meeting, Seminar Room, Dementia Research Centre, 8-11 Queen Sq, London WC1N 3BG: Time: 11am – 2pm. Lunch included. November 2013: Date and venue to be confirmed 21 March 2014: Wilkins Old Refectory, UCL, Gower St, London, WC1E 6BT. Time: 11.00am-2.30pm. Coffee available from 10.30am. Apparently, many of these local initiatives were established after the First World War, when the blinding effects of mustard gas became a very real and tragic consequence for many returning soldiers. My route into many of these services has been via the helpline at the RNIB accessed via helpline@ rnib.org.uk or by calling 0303 123 9999. We look forward to welcoming you to the next support group meeting on 5 July 2013, details of which are listed below and to receiving any contributions you may wish to make to future editions of the newsletter. Jill Walton 3 directions Directions for forthcoming meetings Wilkins Old Refectory, University College London, Gower Street, London WC1E 6BT Underground travelling from south to north stop outside Warren The closest underground stations to UCL are Street station, about five minutes’ walk from UCL. Euston Square on the Circle, Metropolitan and Services to these stops include route numbers: 10, Hammersmith and City Lines, Goodge Street 14, 24, 29, 73, 134, 390. on the Northern Line and Warren Street on the London Buses Infoline: 020 7222 1234 Northern and Victoria Lines. British Rail London Underground Infoline: 020 7222 1234. London has many mainline rail stations. Most London Underground - Did you know that you of these are a short journey away from UCL, can ring London Underground Customer Services with the stations at Euston, King’s Cross and St on 0845 330 9880 the day before you are due Pancras being within easy walking distance. to use a service? They arrange for someone to British Rail Infoline: 0845 748 4950. meet you in the entrance area of the station at Parking which your journey begins, accompany you down UCL Helpline 020 7974 4651 or 020 7974 4655 to the platform and onto your train. They then (Staffed Monday -Friday 9.00 am to 5.00pm) radio ahead to an official at the relevant station to We are very conscious that travelling to and assist with any required platform changes or take around London can seem a daunting prospect. you up to ground level. Be aware that pre-booked travel is generally Buses cheaper than tickets purchased on the day UCL’s Gower Street site is served by many and that the Myrtle Ellis Fund provides help Transport for London bus routes. Buses travelling with travel costs where required. Contact Jill for from north to south stop in Gower Street, further details. immediately outside UCL’s main gate, while those 4 your contributions Blog spots Pam O’Donnell attended the last support group meeting via Skype and is keen to promote activity on various blog spots. She writes: “This is the guest blog site for Scientific America .The blog just started and they have been posting looking for information: http://blogs.scientificamerican.com/mind-guest-blog/ Two of my tips for caregivers got posted on a blog: http://unfrazzle.blogspot.com/2013/02/tips-from-fellow-caregivers.html Attached is a story from 2006 about Dee Bingham and her Dr: Bradley Boeve the Chair of Behavioural Neurology at Mayo: http://www.keloland.com/newsdetail.cfm/posterior-cortical-atrophy/?id=49126” 5 your contributions cont’ Depression in carers This BBC report from the Royal College of General Practitioners may be of interest: http://www.bbc.co.uk/news/health-22478706 NB Please also see the article by Susie Henley later in this newsletter, which is the summary of a presentation she recently gave. Personal Independence Payment to replace DLA You can make a claim for Disability Living Allowance (DLA) until 10 June 2013. From this date, you will have to make a claim for Personal Independence Payment (PIP) instead. This is because PIP replaces DLA for new claimants from 10 June 2013. Personal Independence Payments involve a more objective assessment, with a face-to-face consultation with an independent health professional for most people and include regular reviews so individuals continue to get the right support. PIP is based on an assessment of individual need. It will not consider what impairment an individual has, labelling them simply on this basis. Instead it will consider how their impairment affects their life, considering their ability to carry out a range of everyday activities. Information will be gathered from the individual, as well as healthcare and other professionals who work with and support them. Most people will be asked to a face-to-face consultation with an independent health professional as part of the assessment process. The health professional will ask questions about the claimant’s circumstances, their health condition or disability and how this affects their daily life. For more information visit: https://www.gov.uk/.../introducing-personal-independence-payment 6 your contributions cont’ ‘Access to work’ grants An Access to Work grant helps pay for practical support so you can do your job. You may be able to apply if you have a disability, health or mental health condition. The money you get can pay for things like: specialist equipment, travel when you can’t use public transport and a communicator at a job interview. How much you get depends on your circumstances. You won’t have to pay any money back and it won’t affect your other benefits. Laura Knight has recently applied for the grant for her father and writes: “This information might be useful for some people who can still contribute to the workplace, but can’t drive and struggle with certain tasks. We are currently going through the process with dad and so far they have been really good and have offered to pay for taxis to work, digital voice recorders and voice activated software and even a support worked to come in a couple of hours to help dad with tasks he struggles with.” The website to visit for more information is www.gov.uk/access-to-work/overview Tinted lenses Following on from previous newsletter comments regarding the potential value of tinted lenses for people with PCA, Pam O Donnell has provided the following 2 website references, which answer some of the questions raised in respect of how different coloured lenses affect vision: www.trails.com/how_8622_select-sunglasses-fishing.html http://www.wileyx.com/catalogs/pdfs/2012_Motorcycle_Brochure.pdf In general, amber and yellow lenses filter out blue light to increase contrast and improve your ability to focus in hazy conditions. Pink lenses improve contrast and depth perception by absorbing light in foggy or gray conditions. Gray lenses sacrifice contrast to allow for accurate colour perception. Brown lenses combine the advantages of gray and amber lenses, but to a lesser degree than the originals. Purple and blue lenses attract low-contrast blue light, so they’re only useful in fashion settings. However, the exact effect of colour lenses in PCA remains to be tested. 7 dementia and carers The impact of a diagnosis of dementia on carers Dr Susie Henley is a research and clinical psychologist at the Dementia Research Centre, UCL. At a recent meeting she spoke about the complex process of accepting a diagnosis of dementia in a friend or family member. She listed some of the processes this inevitably entails and also used the session to explain a new counselling service which she is to be a part of, which will offer a series of counselling sessions for people diagnosed with dementia at the National Hospital for Neurology and Neurosurgery. Whilst this service will not in the first instance be available to all, it is hoped that results will show that people who receive the counselling service benefit from it in a significant way, and that a case can be made to roll the service out more widely. Coming to a peer support group is one way of realising that it is normal to feel like this, and that many other carers also have those feelings from time to time. Sometimes you can manage these feelings by finding some time to yourself, or letting off steam with a friend, or going out for a walk, but if they become overwhelming and stop you from getting on with what you want to do, there are lots of options that have been shown to be helpful. Susie’s talk embraced the impact of a dementia diagnosis on carers and some resources that carers might find useful. There are over 670,000 carers for people with dementia in the UK and the amount of free care they give saves the state around £8 billion. Often carers experience difficulty in getting a diagnosis for the person with dementia, because the symptoms aren’t well-recognised, and then find they are “left alone” after diagnosis when in fact they really need on-going support and information. And whilst it can be a relief finally to be given a name for what’s going on, it can also be very upsetting and make the future seem uncertain. Your GP should be able to refer you to a form of counselling, of which there are different types to suit different people, and your GP should also be able to discuss whether some medication might help lift your mood, particularly if you feel very down or worried. More and more research is focusing on carers and their needs. Key messages are that carers need on-going support after diagnosis, and that healthcare professionals must recognise that the needs of the carer and the person with dementia change all the time. Susie touched a bit on the social dilemmas that arise when you care for someone with dementia – friends and neighbours often can’t see that anything is wrong, don’t understand what help you might need, or in the later stages just assume that there’s no point visiting. She suggested that it is important not to assume that everyone will react like this though, as this can put you off asking for any sort of help; do try to ask friends and neighbours for what you need and see what the result is. The emotional impact of dementia is also hard – many people go through a wealth of feelings from guilty, angry and annoyed, to sad and despairing. National guidelines for carers (NICE) now say that all carers should have an assessment of their needs (which includes assessing for and treating psychological distress if necessary), and should be given education about dementia, peer-support groups and information about benefits and legal matters. Ideally a lot of this initial information should be provided by an NHS clinic, although feedback from carers shows that services really vary in how much they understand about dementia and what information they can offer. Susie listed a number of websites, both NHS and voluntary, that have information about 8 dementia and carers cont’ legal, financial, and social support that is available. The importance of peer support groups came up several times, and was reinforced during the meeting as the most useful answers to questions people had at the end of the talk were from the other carers there; and it is great that people feel able to share their experiences with each other at the meetings. Susie has also given her permission to reprint this letter which was published in the Times on April 23 2013 . It was writtten by her in response to an article the previous week citing Dr Chris Fox of UEA saying that there was really no point diagnosing dementia early as it just meant people lived in misery. 9 more news Update from Down Under By Terry Barnett You may remember reading in a previous newsletter about our contact with a group of people with PCA in Australia, and their attempts to start a support group akin to the model we have trialled with our group. Terry Barnett was the founder member of this group, after first contacting us approximately 2 years ago following his wife’s diagnosis of PCA. Terry writes: “I have now had around 40 PCA-connected people make contact with me via the pcaaustralia website. We are gradually finding people but the same problems of geographic spread and different stages of the disease mean forming support groups is difficult. Still, we are moving in the right direction. So I worked with her and she made contact with Dr Seb and your information, and now we have it. It is not that the information on it is new but finally having a reference to PCA on the Alz Aust website (nothing existed previously) is a breakthrough. It will also be an extremely helpful tool for staff in Care Provider facilities who can at last have something put straight into their hands.” One major breakthrough has been the development of a Help Sheet for PCA within Alzheimer’s Australia. Just fortunately a Researcher in Alz Aust is a friend of my daughter We are looking forward to touching base with Terry and his wife during a forthcoming trip to the UK. You may be interested to visit their website at and wanted to do something for us and PCA. www.pcaaustralia.org PCA Website day; of those, approximately 7 have visited the new website before, whilst 8 of them have not and so are regarded as new enquirers. The new PCA support group website format allows us to see how many people are visiting it. At the moment there are around 15 people visiting it every 10 research update Research Updates: The following summaries are synopses of the presentations given by Tim, Keir and Ross at the meeting on 22 March 2013. Tim Shakespeare We hope that by collecting this information and trying our best to measure it, we can better communicate the problems that people with PCA face to other people. Also, by following people up and seeing how these things change over time, we hope to get a better picture of the effects of Posterior Cortical Atrophy at different stages. This should help us answer common questions about how the disease progresses and when people experience different symptoms. I presented initial results from a questionnaire that we give to people who know someone with PCA well, usually a friend or a relative. The questionnaire has lots of questions about different symptoms and tries to build a picture of the things that people with PCA have difficulty with. By doing this with people over subsequent years we hope to get a better picture of the stages of PCA. The questionnaire we use was developed by a group in Cambridge and has questions that fit Keir Yong into different categories, such as everyday skills, orientation to time and place, memory and mood. I am currently doing a PhD focusing on dyslexia in PCA, with a particular emphasis on using what we know of problems in vision and reading to inform the development of computer-based aids that may facilitate reading in PCA. At the moment I am looking at how altering the presentation of text can help avoid problems reported by individuals with PCA when reading, such as losing their place on the page, skipping lines or finding it hard focusing on the appropriate word in a sentence. We found that only a small proportion of the people with PCA that we asked about had frequent problems with their mood and less awareness of their own abilities. However, when we asked about everyday skills, things like making a hot drink and shopping, the proportion of people who had a reduced ability was very high. Often, a little bit of assistance is needed with many kinds of activities. When we compare the results from people with Posterior Cortical Atrophy with those from people who have what we call typical Alzheimer’s disease – where memory is affected first - we find that a greater number of people with typical Alzheimer’s disease have problems with memory, awareness and mood – but a slightly lower proportion have severe problems with everyday skills. The original questionnaire didn’t have any questions about vision, so we added some extra questions about visual perception, Ross Paterson As a PhD student focusing on Young Onset Alzheimer’s disease I discussed a study I am involved in setting up. Later this year we will be recruiting individuals to a new study into early onset Alzheimer’s disease (individuals with symptoms before the age of 65 years without a known genetic cause). We already know that Alzheimer’s disease can cause different problems in individuals with symptom onset at an early age compared with those whose symptoms begin later on in life: in particular we know that some patients with young onset Alzheimer’s disease have much more prominent problems with vision rather than day-to-day memory. We suspect that there are other such variants and this study will allow us to explore the clinical and neuropsychological features, brain imaging signatures and cerebrospinal ability to use numbers, and language. In these categories, a much greater proportion of people with PCA had severe deficits than in the other kinds of questions we asked, and this suggests is that it’s really important to assess visual perception, as problems with this can make every day activities incredibly difficult. 11 research update fluid (CSF) profiles of Young-onset Alzheimer’s disease. This study, funded by Alzheimer’s Research UK through a very generous donation from Iceland Foods, will be one of the largest carried out to date and we hope will allow us to gain unique insights into how young onset Alzheimer’s disease affects individuals and their families. More generally we hope that this research will help us understand better the biological processes that cause Alzheimer’s disease. Drs Catherine Slattery and I are the researchers who will be running this study, supervised by Dr Jonathan Schott and Professor Nick Fox. For more information about the study, please contact us by email (c.slattery@ucl.ac.uk; r.paterson@ucl.ac.uk) or by telephone (0203 448 3856). 12 diary extracts Diary extracts As mentioned in the introduction to this newsletter, Bill McGammon and David Moon both contributed to the January meeting by providing access to diary extracts, outlining significant moments in the journey their wives have experienced as a result of PCA. With their permission, and as a result of the feedback we received from people who read them, we are reprinting them here, trusting that they will provide valuable insight for all of us affected by this condition in any way. David and his wife Pat have been members of the group since it was formed in 2007 - Pat lives at home with David in Norwich. Bill’s wife Mags died in July 2012, having also been a longstanding member of the group. Pat Moon – Diary extract Sept 13th- 24th 2012 together. How we met, our marriage, jobs, homes, children, holidays, Pat’s books and so on. Pat suffers from Posterior Cortical Atrophy (PCA), a rare brain condition. The following is a diary account which her husband David kept and records the everyday changes that he noticed in her over a 3-month period. The recording has proved to be a lifeline and I must have used it a hundred times. Whenever Pat ‘loses it’, I play the tape and nine times out of ten it brings her back. She even participates by intervening and joining the discussion again as we listen. The technique has brought her back to ‘reality’ time and again. “About a year ago, when Pat was still very lucid, we sat down with a little dictaphone and made a 20 minute recording about our lives together. I acted like an interviewer but basically we talked about all we could remember about our lives FROM SEPTEMBER 2012 Registered blind. Spatially disorientated – has no memory of any familiar spaces so cannot find her way from room to room in her own home. When in a room she is often unable to leave because she does not remember the way out (even in a space as small as a toilet) Can no longer conduct normal functions independently - e.g. dressing, washing etc (but thinks she can). Unable to use cutlery independently and cannot eat or drink very effectively. Pat cannot be left alone for more than about 1 minute – gets very anxious. For example, she might ask for a cup of tea but starts to call for help soon after I leave the room. Much weaker than at start of year and deteriorating fast. Cannot walk far, weak hands (lifting a full cup very difficult), very poor co-ordination. Can only just climb I STRONGLY recommend this to all carers who care for someone who is still sufficiently lucid. It will prove invaluable to them in the coming months”. the stairs at home (now limited to once a day at bedtime). Has had tendency to ‘lean’ very markedly, particularly when tired; almost topples over at times. Lean started to the right (for some weeks) then changed to the left. Presently it has become a ‘stoop’ – to the centre. Low mood persists, mornings usually worse. Often says she wants to die. Has a daily ‘memory loss’. Usually around 5 or 6 o’clock. Demands to know ‘why am I here?’ Denies that she is in her house and does not know who her husband is. (If I explain that I am her husband she can get quite aggressive and says that her husband has left her). When these episodes end, she has no memory of them happening. Most symptoms are unpredictable and complex, they can switch on quite suddenly. Occasional bouts of ‘insanity’ – attempts to run away but has no idea where she is and might even attempt to 13 diary extracts cont’ walk through walls or objects. Administration of Pat’s medications has become a fine art. Her symptoms have to be understood and monitored in order to provide appropriately and at timely (although irregular) intervals. Can mislead (not deliberately) – might insist that she came by helicopter for example. Usually thinks she can do anything as before – ‘I need a new pair of glasses’. Could be dangerous if she inadvertently fooled a stranger. Calling “help me” is becoming more common. Sometimes about the house to inanimate objects (which she cannot see), and sometime in the street. She has never articulated what sort help she wants. Very odd delusions or requests (asked to have a bath during lunch, for example). Seems to see odd things and stares towards nowhere – saw a baby on the table. Pat’s ‘out of it’ experiences are more frequent and seem to trip in and out for longer. She sometimes adopts a fixed stare with dilated pupils; at those times she has no idea who I am – and is afraid of me. Pat’s ‘vision’ is definitely worsening. Her brain’s interpretation of what her eyes can see is very loose. She is also losing skills in both gross and fine motor control. She can no longer manipulate a small object such as a pencil. She cannot eat without assistance except for ‘finger food’ (such as a grape). She tends to ‘shuffle’ a little so is prone to trip (we watch her very closely); if she stumbles she has little in the way of reacting to save herself. Pat’s motor skills and control are getting much worse. She cannot use a tissue effectively and sometimes has problems with clearing phlegm. Toileting has become a serious problem (not incontinence but she seems to have forgotten the process and always needs help). Once in bed Pat stays completely still and only moves when I take her to the toilet (usually about 4 times now). the pattern described for the September ‘diary’ – but the ‘out of it’ experiences are becoming more frequent (sometimes twice daily) and less predictable. She often gets an attack at around one o’clock in the afternoon – but, worst of all, they can happen in the night. Once she called for help and tried to get out of the room every five minutes from 11.00pm to 02.30am; a really bad night for both of us. We have had a ‘wet room’ installed and made a ground floor bedroom so we no longer have to go upstairs. Pat has been loaned a hospital bed by the O.T. – very useful. Pat always uses a wheelchair when we go out and has an indoor ‘shower chair’ (also from the O.T.) to move about at times. Her walking has become very weak and toileting is difficult. Another big change is that Sam (our son) has given up his full time work so that he can help us. He comes for two or three hours nearly every day – this is a massive help and pretty indispensible. Other members of our family come to stay whenever they can. SUMMARY for NOVEMBER More of the same although Pat is becoming weaker and less responsive. She can barely walk at all (just a shuffle and perhaps 30yards max) so the wheelchair is indispensible. Her mood is variable but she sinks into despondency for long periods. Still very unpredictable. Her temperament can change at mercurial speed; she can go from being quite docile to becoming hostile and aggressive within seconds. When she is hostile she does not recognise me and will oppose every suggestion or offer of help. She is on the verge of physical aggression and will sometime clutch at my clothing. However, her muscle control is very uncoordinated and she does no damage. Sometimes she will scream. More serious are the times when she stands up and starts to blunder about – this is also uncoordinated so can be controlled by ensuring that she is not likely to damage herself (not always easy). Her medication programme requires some SUMMARY for OCTOBER Pat’s condition is more or less repeating 14 diary extracts cont’ She is having even more serious ‘5.00 o’clock’ when she can be very difficult and inconsolable. She will aggressively deny that I am her husband and her delusions can be wide ranging now. She can have two quite serious events daily although on some days they might be minor episodes but more frequent. She might even wake up in that state of mind and recently one came on during her shower when she flatly refused to move for about 30 minutes. I am finding the best approach is to be very gentle and reassuring at all times; it is important not to argue as logic has no meaning to her. I try to change the subject or tell her that ‘David’ is away but will be back soon. I try to prepare her for the bad events (like dressing) by talking her through well in advance and going very slowly through the process. Pat always has the full dose of Respiderone (0.5mg in 4 doses). Lorazepam as required (normally 3x 0.5 but sometimes 4x) skilled evaluation of her ‘mood’ almost on an hourly basis. Sometimes I am able to get it just right but there seem to be no rules except to watch for the signs. She is taking the full dose of Respiderone (4 x 0.5mg) but not always using the maximum of Lorazepam (usually 1.5 mg only). Pat is suffering more delusions and certainly can no longer be unattended for more than 60 seconds before she starts to call for help. It would be impossible to cope without Sam and other members of the family. SUMMARY for DECEMBER Steady deterioration in abilities. Pat is virtually unable to do anything without help and can only be left unattended for a few seconds before she calls for help. Often calls for ‘David’ even when I am by her side. She will try to stand as soon as she realises she is alone – and then staggers about dangerously. Margaret McCammon’s Diary Mags had retired in June 2008 after working as a Legal Secretary for the past 30 years. She was diagnosed with PCA in November of the same year by Dr Peter Nestor at Addenbrooke’s Hospital, Cambridge (happy retirement, eh!). During testing, she touched type her name and address for him, no problem, and when read back had missed out 1 digit of postcode. It took her longer to correct that than typing the original. This was when we realised there was something amiss. She attended various research programmes early in 2009, and continued with annual visits to Dr Nestor’s clinic in June of each year. On her last visit in 2011, it was obvious that degeneration was starting to kick in and it was suggested that she should withdraw from Aricept as it did not seem to improve her situation. She wasn’t well enough to commute for follow up appointment in June 2012. She had managed quite well until I retired in June 2009, when it was now becoming quite obvious that she was struggling to cope on her own. She could open the freezer door but couldn’t think to turn her hand around to open fridge door. Found it impossible to work out 24hr clock on cooker and even began to have difficulty with the 12hr clock, she could see the hands but could not work out the time. Cooking was now out of the question as she would forget to turn off hob and it became too dangerous. Mags had to give up driving and as a passenger trying to enter car with left foot forward, proved impossible. She began to 15 diary extracts cont’ have difficulty locating the armchair, quite often sitting on arm first and sliding into position. Eventually she had to be guided into chair, as if left to her own devices would miss chair completely and land on floor, all due to lack of spatial awareness. This obviously applied to visits to the toilet. I purchased a lightweight transportable wheelchair as walking when shopping became very tiresome. When you are desperate you will try anything, acupuncture (10 sessions), brain gym (rhythmic movement training, wellness kinesiology), all to no avail. Margaret had attended two/three meetings of the PCA Support Group. time progressed we became aware that a wheelchair commode only fits over a conventional 15” high toilet. Never told this by installer at time. January 2012 Began the year having weekly visits from physiotherapist to help keep muscles supple, arranged by GP. March 2012 Attended East Anglia Driveability for assessment of swivel chair to aid entering/ exiting car. It was something we were seriously considering. It is a worthwhile option for long term use. Visit from Speech Therapist, as Mags was beginning to mumble her words at times. After several visits, the therapist concluded that there was not much she could do. She thought it a degenerating muscle problem that was the cause, which also affected her ability to eat. Information of findings given to GP. Visit from Sensory Support team, nothing they could do either. Visit from Social Care Assessor, who reported her findings to our GP. Visit from Occupational Therapist for assessment. Visit from Assistive Technology for assessment. Sufferers from Dementia normally have a plateau period. Mags was beginning to degenerate without plateauing at all. This was making it difficult to meet her needs as her condition was constantly changing. April 2012 Visit from Social Worker for assessment, as it was now becoming clear that help with care would be needed. As recommended by O/T, stairlift and bedroom ceiling hoist were installed. It was deemed inappropriate for me to lift Mags from bed to shower commode, due to risk of injuring my back and then who would look after her (at GPs insistence). It was becoming increasingly difficult for her to walk unaided. Mags was not happy on stair lift, very frightened (? due to spatial). There does not seem to be any equipment 2010 Was not a bad year as Mags seemed to have plateaued for most of it and we managed to have a bit of a social life. When on holiday in Lancs at Mags’ sister, she took a fainting turn in car. We took her to Burnley A&E; they had never heard of PCA and she was discharged. She took another turn at midnight. The paramedics were called, she was admitted to Blackburn Royal Infirmary and kept in for observation. Again, the hospital had never heard of PCA. Mags had another three episodes under their care. She was kept in for three days and prescribed Epilim, to control epilepsy, which she had never suffered from previously. After 48 hrs clear from any episodes, we drove home. On her annual visit to Addenbrooke’s, they suggested it would be safer to keep her on Epilim, rather than take a chance of another episode. November 2011 We converted our bathroom, extended shower cubicle area and removed shower tray to install a level access shower with wet room non-slip flooring and appropriate grab handles. Also anti-scalding thermostatic shower, as Mags could not be trusted to adjust controls by herself. This proved a good move. Beware: Made mistake of installing 18” higher toilet to make it easier for her. As 16 diary extracts cont’ available that can transfer a patient from wheelchair to stairlift and vice versa, only option is to be manually lifted. Assistive Technology brought alarm button on lanyard, large number telephone with three picture memo buttons and a movement sensor; didn’t find any of them much good at this stage. Also bought baby alarm monitor for downstairs with infrared camera placed in bedroom. Brilliant piece of equipment, enabling me to monitor her from downstairs. Visual and sound. Highly recommended. capable of doing it herself, wanted to take her home. My daughter Loraine , Mags’ sister Ann and I were sharing care from 9am to 10pm to ensure Mags had adequate food and drink. Loraine had to change her mum’s wet nappy as nurses were too busy at the time, simply not enough of them. We filled in booklet with regard to her drug dosage and frequency, this was totally ignored. On asking trolley nurse why she was giving Mags her ‘knock-out’ drugs at tea time and not supper time, she said I just give them out, I don’t know what they are for. Honestly, I didn’t swear. I complained to sister, who persuaded me to leave Mags there until Friday, as she was trying to initiate Continuous Health Care (CHC), which she can only do while patient under her care. Friday 8th: Mags came home, hospital issued medication in liquid form, as they found she now had difficulty swallowing tablets. Monday 11th: Hospital bed arrived. APS and Hospice@Home teams took over care for two weeks; very professional. Monday 18th: Mags was now under care of GP, Community Matron and Macmillan Nurse. Macmillan Nurse arrived for assessment. CHC assessor arrived, but did not think Mags met criteria. I was livid. How can she be under H@H team and not meet criteria? Tuesday 19th: After pressure from other three, CHC assessor admitted she called it wrong. Wednesday 20th: Mags 64th birthday. Family all here. I was not sure if she was aware it was her birthday. Friend telephoned to wish her happy birthday, last phone call Mags made. Friday 22nd: Visit from GP who is going on holiday for 3 weeks, doubted if Mag would be with us on his return; very sympathetic. He prescribed minimal dose morphine patches (12.5 um) to make her more comfortable. Monday 25th: Care was handed over to Saga Care. They were excellent, all of small team looking after her very well. She even May 2012 Further visit from OT, who had supplied a separate commode for downstairs toilet. Social Worker organised ‘one day respite care’ per week at nursing home. Mags was not happy there; lasted two visits. She was the only one in day centre; not much stimulation there. We then considered installing low profile front door with ramp for wheelchair access. Social Worker organised care twice a day for personal needs through Allied Care. First week, two carers x two visits per day equals 28 carers, we had 22 different faces. Not good for someone with dementia. Weeks 2 and 3 seem better with less personnel. June 2012 Were about to give go ahead to builder for ramp, but as degeneration began to move quite quickly, put on hold, eventually cancelled. Jubilee Monday: Visitors from Australia to see Mags. Jubilee Tuesday: Mags suffered from abdominal pains. Called out of hours service; not very helpful. Daughter called ambulance. Paramedics called out of hours doctor; did not have much success either. They decided to take her into hospital. Wednesday, Thursday: In hospital, no one had of heard of PCA, they had to ‘Google’ it. Hospital care was appalling, leaving jugs of water by her bedside, no one to decant into beaker to give her a drink, she was not 17 diary extracts cont’ feeding Mags and withhold all drink. We were to wet her mouth with a sponge type lollipop (supplied), occasionally dipped in pineapple juice which is full of enzymes to help stop any bacteria. Was this the beginning of the Liverpool Pathway? Nobody had said. Wed 11th: Stand in GP arrived to check on Mags. Patients at EOL stage should been seen at least once a fortnight by GP, as if not seen within final two weeks, there may be a need for post mortem. Are carers aware of this? I wasn’t. Last thing you would need. Friday 13th: Mags breathing quite heavily; checked her rate over 3 hours and maintained 36 breathes per minute. We were told it could go as low a 5 or 6. Saturday 14th: Shock, Mags passed away at 6 am this morning. Friday 20th: Mags’ funeral (birthday 20th June, funeral 20th July). joked and laughed with them. Thursday 28th: Visit from palliative consultant, as Mags ability even to swallow liquids was deteriorating; she prescribed medication administered through a syringe driver. Mag began to scream when being bed bathed, nurses thought this was due to muscle contraction. Doctor later told us this was because she was in a black space (disorientated) and when rolled over on side, thought she was falling. I wish we had known this at the time. Friday 29th: Community Matron visited to see all care was in place. July 2012 Wednesday 4th: Nursing Sister attended to fit syringe driver. She visits daily. Monday 9th: Nursing Sister attended to service syringe driver. Advised us to stop Summary We as a family, (son Alan, daughter Loraine and myself) realised that there was no way back for Mags. Although it was very sad for us, I know it was not sad for her. She was well aware of what lay ahead, and wanted no part of it. It was a sense of relief. Unfortunately, you can’t rectify the brain. Mags wasn’t daft and knew what was coming; there is no way that she would have wanted to live a life where she was going. Her main worry was who was going to iron my shirts, typical of her. She was an avid reader, but when she turned to page 2 and could not remember what was on page 1, that was sad. Being a Morse fanatic, never missed an episode, you can see how hopeless it was becoming for her when she could not follow the plot, or as she said “I have lost the plot”. In the end she never complained or got hysterical, and that was how she left us, peacefully drifting away in her sleep. Donations tell you how well she was regarded (with full house of 120+ at her funeral), totalling almost £1200: £500 to PCA Support Group, £500 to Alzheimer’s Society, £100 to church for someone in need at Christmas and remainder on Christmas Vouchers for THE carers who looked after her so well at the end. That’s what she would have wanted. Loraine, a teacher, had the chance of redundancy in summer of 2011 when Suffolk CC closed down middle schools, but opted for another position in a Secondary School. She bitterly regrets that decision, if she had known her mum had so little time left she would definitely have wanted to spend the last year with her. Loraine would sit at night holding her mum’s hand and talking to her for 3 hours at a time, not just her mum, her best friend, they did everything together. My son, Alan, couldn’t do this, seeing his mum for 5 mins at a time was about all he could handle. He now feels so guilty. He mustn’t, everyone is different. Both of them were very close to their mum, he particularly found it so hard to handle. In conclusion, don’t take any aggression or nasty remarks from your partner too seriously; let it go over your head. They are not saying it, it is this dreaded disease. I am afraid when you are diagnosed with PCA you become a member of “God’s waiting room”. Cherish what time you have together, life is short enough for us all. Good luck and wishing you all the time in the world together. Bill McCammon 18 and finally ... Alzheimers Show, London, April 2013 We were delighted to be able to represent the PCA Support Group at the recent Alzheimer’s Show in London. With over 2000 people passing through the doors, we had plenty of opportunity to talk to people and promote awareness of the groups we operate under the umbrella of the Myrtle Ellis Fund. Seb had been invited to speak about ‘Young Onset Dementia’ at one of the main show events. Checklist RADAR keys: national key scheme for toilets for disabled people. E-mail: radar@radar.org.uk Tel: 020 7250 3222 This checklist will remain a feature in forthcoming newsletters and can be added to as appropriate. It is a brief reminder and pointer to those services which may be of benefit for people with PCA. Please contact Jill if you require further information about any of these services. Blue badge parking permit: see our website for our factsheet and supporting statement RNIB: support and advice for people with sight loss. Tel 030 3123 9999 E-mail: helpline@rnib. org.uk Medic Alert or other identification networks Disabled Living Sites, which sell products designed to make daily living activities easier to manage. Of particular note is The Knork is a fork with wide, rounded and bevelled outer tines that will safely cut food like a knife, without a sharp edge to cut the mouth of the user. Visit www. livingmadeeasy.org.uk and www,asksara.org.uk Assessment of need: for patient and carer. Request one via your GP or directly via your local social service department: [Disability Living Allowance/Attendance Allowance/Council Tax Reduction] Advance Care Planning: the process of identifying the wishes and preferences of the person diagnosed, ensuring that people are aware of these Lasting Power of Attorney: needs to be established as soon as possible Admiral Nurse Service: information and support for family carers, people with dementia and professionals. Available locally in some areas for practical support but the helpline is open Message in a Bottle: a Lions scheme which combines a notification at your front door with the storage of vital information in a bottle in the fridge! Visit www.lions105d.org.uk/projects/ miab.html for information to all. Tel: 0845 257 9406 or email direct@ dementiauk.org 19 minutes PCA CARERS MEETING MINUTES: 22 JANUARY 2013; Gilliatt Lecture Theatre, Institute of Neurology, Queen Square, 1pm to 3.30pm Venue and attendees: 40 people attended in person, with 3 others (all from the UK) joining us has PCA. 2.2 Disability Living. The lowest amount is via Skype. This is a very encouraging number, £20.55, the middle award is £51.85 and so our meeting continued in the Gilliatt Lecture the highest award is £77.45. In addition, Theatre. We all felt we had gone back in time Mobility Allowance continues after the age to our student days! The acoustics etc. are, of of 65: so make sure you apply for it before course good - purpose built, though the steep 65, since you cannot apply if you are over steps would make it difficult if a number of elderly 65. carers were to attend. 2.3 Points to remember when filling out claim Programme: Our theme was “End of life care” forms: - Don’t under-estimate how you are we heard 3 personal accounts from Roger coping: describe the worst day. It is all too Kelly and Peter Ledger from our membership easy to make the best of things and not to along with Barbara Pointon MBE, an Alzheimer notice deterioration. Remember Night Care Champion, who is a government advisor on is triggered, if you are woken up more than behalf of the Alzheimer Association. twice per night. Ask yourself, if you would leave the person you are claiming for alone Welcome from Jill: 1.1 all night? Jill outlined the programme and added 2.4 In claiming for Mobility, you need to stress a brief history of Carers Meetings for the that the person cannot go out alone: benefit of newcomers. stress that they need help with steps and 1.2 A number of case histories written by think how far they can walk before they members were available at the meeting. become tired. Remember that severe sight Further copies may be obtained from Jill, as impairment automatically triggers the needed. highest rate for Mobility. 1.3 Data protection issues. Minutes will be 2.5 Blue Badge. Severe sight impairment taken and posted on the web site. Issues triggers an automatic Blue Badge. Drivers are recorded but no names are used, ferrying people with a Blue Badge do not except for those of the speakers. Speakers’ pay congestion tax. The badge holder can Power Point Presentations will be posted on register up to 2 vehicles of people who drive the website. them. 2.6 HM Revenue and Customs. A Blind Person’s 2Talk by Roger Kelly “Non means-tested allowance is £2,100. They are entitled to a benefits”. The main sources of such benefits are: half price TV. 2.7 NHS Continuing Health Care. Applying is Local Government, The Department of a long and complicated procedure with a Work and Pensions, HM Revenue and points system under various headings; it is Customs, TV Licensing and the NHS. Social processed in two stages over a period of Services were not included in this talk. months before a final decision is reached. 2.1 Local Government: Council Tax is There are 10 criteria is stage 1 including reduced by 25% on application. In effect, Cognition, Behaviour, Medication and carers are treated as being the only taxable Mobility each of which is assessed at 3 resident. Council tax reduction is if there levels. If you pass Stage 1, then Stage 2 is are only two of you in the property and one the Decision Support Tool (DST which has 20 minutes cont’ 12 criteria and up to six levels of severity legal position. It is vital to plan well in However, benefits can be substantial. In advance since the latter stages of PCA can one case the patient was given 3½ hours of progress suddenly. A scripted version of his help in the home paid for by the NHS and presentation is available to read at the end their carer are allowed 2 respite nights. of these minutes. All Care in a Nursing home can be fully Barbara Pointon’s talk, ‘Offering funded by NHS. Disability Living Allowance enlightened care and support to people will lapse after 28 days. Some Local Areas with dementia’.4.1 Barbara’s talk was based will provide an independent Health Budget on what she learnt in the final 6 years of where the carer becomes the client and her 10 years of living with her husband’s can administer the budget for professional Dementia. As a Dementia Champion, she Carers as an employer and thus pay at presented imaginative, pragmatic solutions around two thirds of the rate of an agencies to the problems of Dementia, championing charge. Organisations such as the Sussex not just the carer but also the sufferer, as an Independent Living Association will help individual. you with their contracts and administer their 4.2 Spotting tell-tale signs. A new fact does salaries and the tax involved. Currently, pilot not go into the memory – in Dementia, schemes are being monitored prior to being the brain no longer lays down a memory. rolled out nationally. If you stay at home When patients ask the same question may keep DLA if your PHB does not fully 5 times, each time is the first time. fund 24/7 care. Patients start to make mistakes in familiar 2.8 Final tips. It is vital to stress that the activities. 84% of Alzheimer sufferers have condition is unpredictable. Apply ASAP for visio-spatial problems. They can see, but help. In making applications, stress that this can’t interpret: hence misunderstanding is an ILLNESS. Do not be positive about how their environment. They get lost in familiar you are coping. Look forward to what will places, have problems telling the time happen: do not base your application on or finding rooms. They are aware of the past situation. this and get frustrated by mistakes. 2.9 Getting Help: A social worker should Their tracking of facts becomes faulty: be assigned to each case; in addition hence left and right get confused; art, Community Psychiatric nurses will help spelling and writing all become flawed. as will care home management, charity 4.3 It is vital to celebrate what they can do. workers and even your MP! Roger also Music, for example is stored in a separate offered advice to individual members based part of the brain, and continues to be on his experiences. enjoyed. An early diagnosis is vital to 2.10 Problems of money not coming to the carer preserve relationships. and a bank refusing to give a breakdown 4.4 Help with personal Care. Don’t rush. Allow of how it is being spent were raised from the patient their own pace. NHS Carers are the floor. Getting power of Attorney is highly allowed a disgustingly short amount of time desirable to prevent this happening. with patients. Limit choices and don’t try to normalize the situation: ask yourself who is 3 Talk by Peter Leger. Identifying a Care/ the problem for? Let it go and try instead to Nursing Home and accessing State benefits think laterally. 4.5 Memories of the past can be abruptly lost, 3.1 Peter spoke of his experiences as difficult, so respect the patient’s routine, they may time consuming and frustrating at each be reverting to childhood routines. Knowing stage: identifying a home, finding funding past history might explain their resistance to and how to access it, understanding the certain actions. 21 minutes cont’ 4.6 Strip washes are often preferred by the the Alzheimer Association. This booklet is elderly, who feel the cold more. Always filled out with a photo of the patient and reassure the patient – resist the urge to take basic personal details by the carer: it stays over. on the bedside locker in hospital giving 4.7 People with dementia can’t cope with more personal information to staff when the patient can’t do so. than one thing at once, background music helps concentration. Continuity of paid 4.13 Eating Weight loss is inevitable as the brain is losing control of extraction. Opening one’s carers leads to a familiar relationship. 4.8 Perceptual solutions. Leave the WC door mouth is a very trusting thing to do: hourly open: where there is an image, locate pureed food or thickened cold drinks by it near the handle. Floor needs to be a the teaspoonful are preferable to PEG (tube different colour from the WC. feeding). Coloured beakers (baby ones) are 4.9 Hiding and hoarding are never stealing. most easily perceived. Paraplegic routines Patients forget where they have hidden for excretion are preferable to resorting to a lost item. Wait for people to form a laxatives, which irritate the gut rather than question: simplify the response. helping failing muscles. Reduce medicines. 4.10 Actively involve family carers as expert Child-size doses are effective and have partners in all care settings. Patient may fewer side effects. Normal pain scales use childhood words for bodily functions are unreliable in dementia where sensory (eg. Number 2 = poo) Share these with the things have increased importance. When carer, so that they can meet the patient cognition, abstract thinking and the control halfway. Patient confidentiality may have of physical functions are lost, the things we to come second. The National Council for learned first as babies are still intact, our Palliative care and Carers UK can advise on psyche, our senses and our emotions. Use these issues and on difficult conversations. the senses: smile at patients, comfort with E.g. Booklet “What every Carer needs to touch, introduce stronger flavours, make know”. use of favourite tunes. Support the psyche: 4.11 Perplexing Behaviours. Feelings and Build positive emotions: Help the person to feel cherished. emotions give rise to behaviours: a reflection in a mirror may appear as 4.14 Dying It is important to establish final a stranger: TV can be real. Mistaking wishes early, bearing in mind that there are generations may simply be because the huge advances in palliative care. Make use patient is time travelling. See: “And still the of touch and music: help the person to feel Music plays” Graham Stokes (Hawker). See safe. Engage hands, head and heart to the also Leaflet 8 Caregiving Maxims. If people end. Competency is not enough. cannot enter our world, we must enter theirs: protect their feelings, ensure good physical care, personalize activities - people with dementia don’t do anything gladly. Beware of using anti-psychotic medicines. 4.12 The severe stage. If Alzheimer does take its full course, mobility will be lost: a hoist and a recliner (rather than a chair) will be needed. Forever Living products eg. Aloe Vera Jelly, help with skin problems. Admiral Nurses 0845 257 9406 can advise, as can direct@dementia.uk.org. See also the booklet “This is me” published by RCN and 22 Celia Heath, January 2013. minutes cont’ Notes from Peter Ledger’s presentation Paper given to the PCA Support Group 22nd Identifying a nursing home January 2013 Although from time to time Margaret and I had “Identifying a Care/Nursing home and discussed her condition, she has never had an accessing State Benefits – a personal insight into it and so I have had to make all the experience” decisions. My name is Peter Ledger, I live in Ipswich and I’m Throughout the five years when Margaret was still the husband of Margaret who was diagnosed at home I did give a lot of thought to what I would with PCA in 2006. do if I was no longer able to care for her on my For five years after the first diagnosis I cared for own. However, I didn’t do this in an organized, Margaret. During that time we were able to lead objective way and I dreaded the prospect. The a relatively full life. However, Margaret’s condition issue would go in and out of my mind and I deteriorated quite suddenly and in April 2011 I would think about certain scenarios and then the realized that I could no longer cope. I am not thought would drift out again. going pretend that this was anything other than In other words, I was sliding into my first and devastating at the time but I am reconciled to the biggest mistake. I found it impossible to confront reality that Margaret needs 24 hour nursing care. the reality of what was happening. So when The fact that I can say this is largely due my great the dreadful moment came I hadn’t done any good fortune in finding a nursing home where planning – other than arranging Enduring Power Margaret receives excellent care. of Attorney which proved to be an absolute saver. Jill’s brief was for me to talk about “about the Fortunately, we have a wonderful GP. I had experiences you have had in terms of finding, reason to call on his skill and support as settling and now caring for Margaret in a care Margaret’s condition deteriorated but I had no home setting.” So what I plan to do is just tell idea that he was keeping an eye on me as well you our story: how I went about finding a suitable as treating Margaret. He began to encourage home, what was involved in funding Margaret’s me, and eventually to hassle me, to consider care and in settling her in the home. respite care for Margaret. As he put it: “Peter, we Put like that the process sounds as though it was don’t want two of you falling over.” relatively straight forward. That was a wake up call. It wasn’t. As a result I did something I had dreaded – I I found the benefits system confusing and the roused myself and visited a care home. It was process of finding a home and accessing benefits a good thing I did. That evening I hit the buffers was difficult, time consuming and very frustrating. and the decision whether or not I could continue So my principal objective today is to try and to cope - and what to do if I couldn’t - was forced explain how I overcame what often appeared to on me. be obstacles put in my way. The following day Margaret moved, as an When Margaret had to move from our home into emergency admission, to the one home I had care I found myself confronted by four practical visited. Looking back I realize now that I it was issues (and here I am setting aside my own a close call. I had looked at just one home and emotional reaction): I happened to sense it was OK. I hate to think 1. identifying a home that I was happy with; what I would have done if I hadn’t made that one 2.What funding was available; visit. In truth I had only myself to blame. 3.how to access these benefits and The result was that I found myself having to work 4.The legal issues. things out at a time when I was in emotional turmoil. It’s not the best state of mind in which to discover the extent of your ignorance. 23 minutes cont’ So my first point is – however hard, don’t put of the Alzheimer’s Society and asked for her off making enquiries and finding out. I do not advice as to what I should expect. She was really pretend it is easy. It isn’t. But however much pain helpful. Her advice included: is involved, try and crank yourself up and start to • when assessing a home, make more than one prepare because it’s worth it. visit; • take someone else along so that you could The legal issues It soon became clear that Margaret needed full have a second opinion; • She pointed out that it’s a good start if a home time nursing care. So what started as “respite is happy for you to turn up “on spec” rather care” rapidly transformed into a search for a than insisting on an appointment. (In fairness, suitable nursing home. Again, this only served to all the homes I contacted expected me to just emphasize the extent of my ignorance and lack turn up). of preparation. • She also suggested that I should assess the The most important thing I had failed to realize residents as well as the home. How do they was what is involved when dealing with the appear? For example, clothes messed up by welfare and best interests of someone who no eating do not necessarily indicate neglect. It longer has capacity. could be that the home is trying to ensure the Fortunately, Parliament has given this a lot of resident maintains his/her independence. thought and the person suffering is heavily Alarm bells should ring, however, if the person protected, but you need to know who is involved is in the same state a day later. and why. The bottom line is - you can’t just move I’m fortunate in having a very supportive family someone in your care into a home: and group of friends. I talked about my concerns • Social Services need to be satisfied that they with them and this led to two lucky breaks. A do not have the capacity to take decisions friend mentioned that he knew a social worker themselves; who was “in and out of homes” and said he • The NHS Trust needs to be satisfied that the patient is eligible for the benefits available. • and in Margaret’s case, because mental would ask her opinion. Simultaneously, a school friend of one our sons phoned and offered his help. He is a GP in Suffolk and offered to speak health issues were involved, the Community to a friend in Ipswich. Unbeknown to me the Mental Health Team had to make a medical friend was an Ipswich GP. assessment so that the correct treatment and A week later I got the same advice from two third level of care could be identified. parties, neither of whom I had met. The words I didn’t know any of this nor did I know how to were almost identical: “tell your friend he could access these agencies. do no worse than look at Orwell Nursing Home”. Armed with the advice of two professionals I Finding a home visited the home twice, the second time with my Our GP kicked things off and put me in touch sister in law. We had already revisited together with Social Services. At the same time I asked his some of the other homes I had seen. She agreed advice on appropriate homes. with and reinforced my view that they didn’t fit the Unwittingly, I had stumbled on a path which was bill. Happily, however, she felt that Orwell Nursing to serve me well – I had started to network. Home would suit Margaret best, and so it proved. However, lack of preparation again caught me So getting a second opinion proved invaluable. I out. The two best homes were full. I visited three was reassured by the view of someone else that more but, although I had no idea what I was my own impression was right. looking for, I sensed that they weren’t right. Role of the Community Mental Health Team I had, however, got to know the local manager However, before I could move Margaret from the 24 minutes cont’ first care home I had to secure the agreement of accessing them. Social Services. Simultaneously, I had to arrange for her to be assessed by the Community Mental Funding Health Team. Again, our GP was key, putting Up to this point Margaret’s care was self-funded. me in touch with the Community Nurse and she She received Disability Living Allowance and a arranged for the CMHT to contact me. small state pension, both of which made a helpful It was at this point that I stumbled into the mesh contribution to the costs but they were still eye of bureaucracy. Margaret was suffering from watering – around £38,000 a year. bouts of acute anxiety but was no longer in the As soon as Margaret arrived at the Nursing Home care of our local GP surgery. The home was they applied on her behalf for Funded Nursing finding it difficult to cope with her and quickly Care. That’s the normal procedure. identified that she needed full time nursing But it took seven months and a lot of hassle care. However, it was over a month before before Margaret was awarded Funded Nursing Margaret was finally seen by a nurse, and then Care. Getting it was a marathon which included: a consultant, from the Community Mental Health • Endless phone calls, Team. • Dealing with 14 different people, What I discovered was that the CMHT only had • Attending an assessment, an assessment meeting once a week. Patients • And what seemed like endless delays. were added to the bottom of the list and were only reviewed when they got to the top. I must So how did I cut through this? say I was staggered by this – and still am. So I 1. By sticking to my rule that whatever happened, adopted a tactic of phoning the Team at intervals I would keep cool and try to win the sympathy of every four working days, i.e. enough to ensure of the person I was talking to. I always knew I they didn’t forget about Margaret but not so had made progress when someone said: “I tell frequently that I would annoy them and risk you what I’m going to do Mr Ledger…” losing their goodwill. And despite my anger 2.Networking like fury. As an example, one of and frustration, I made a determined effort to our neighbours works for Social Services and I stay cool and try to engage the sympathy of the asked her advice. What I didn’t know was that person who controlled the list. It may sound her daughter is also a social worker and she obvious but it paid dividends as I began to be told really knew the ropes. She was fantastic: what was happening. - Margaret also had to be assessed by a consultant in the Team and this led to more She gave me the name and address of the manager responsible at the PCT, - She also gave me a copy of the frustration and delay - he was in a different assessment form. This enabled me to roughly location with separate booking arrangements - work out Margaret’s score so that when I was but, once again, I stuck to my plan of persistence told Margaret hadn’t met the qualification combined with staying cool. score I was able to challenge this. However when Margaret got to the top of the - And most importantly, she told me about list, the CMHT swept into action. She was the second component of NHS Continuing assessed by two specialist nurses and then Healthcare. This was my most important monitored every few days, including one visit discovery. The second component picks over a weekend, and she was also seen by the up 100% of the nursing home costs. She consultant. mentioned in passing that “no one knows To summarize: I was staggered by the range about this, we are having to spend money to and depth of support services available to me publicize it”. Now there’s an admission. Until but frustrated by the difficulties in finding and then I had been worried stiff about how I would 25 minutes cont’ fund Margaret’s care. As soon as Margaret was awarded Funded finding. - Attending two assessments (Social Services Nursing Care I applied for the second component and NHS) and a third joint meeting between of Continuing Healthcare. As I have said, the two agencies. there’s a lot of ignorance surrounding this. The However, when it was made, the award was support for residents of nursing homes (ie people backdated to the date of the first assessment (not deemed to need nursing care) is covered by NHS the date I applied). Again, the process was very Continuing Healthcare. However, there are two frustrating but polite persistence paid off. components: My biggest ‘win’ was when I gained the sympathy 1. Funded Nursing Care - this applies to people of a nurse assessor. She was assigned to assess whose primary need for care must relate Margaret but was then promoted and had to to their health. It covers the costs of care pass the papers to yet another nurse assessor. provided either at home or in a nursing home. When I politely described the frustrations I had It pays for healthcare, such as services from encountered (actually I was beside myself) I heard a community nurse or specialist therapist, that wonderful sentence: “I tell you what I’m going and personal care, such as help with bathing, to do Mr Ledger…” and she decided to take back dressing and laundry. Anyone who is deemed the file. She turned out to be the best person I to require care in in a nursing home receives encountered and was tremendously helpful. this. There is no means test. The current rate So some general points arising from our is around £107 per week experience: 2.for those people who are deemed to require • Margaret is treated separately from me, so my full time care in a nursing home, as well as healthcare and personal care, the NHS will assets are NOT taken into account; • Continuing Healthcare (the second component) pay for care home fees, including board and pays the costs of the nursing home and is not accommodation. This is known as “the second subject to means testing; component” and is around £700 per week. • Don’t forget DLA. I advised the Dept of Work & Pensions when Margaret was awarded Here is a link to a good document on one of the Continuing Healthcare and then Funded NHS websites: Nursing Care. DLA wasn’t withdrawn until after http://www.nhs.uk/chq/Pages/2392. aspx?CategoryID=68 But although I applied as soon as Margaret was awarded NHS-Funded Nursing Care it took a further eight months for the second component of Continuing Healthcare to be awarded. This involved: - Dealing with yet another group of people; - Being told at one point that Margaret didn’t qualify, only to discover that a mistake had been made which added another month to the delay. And the mistake was staggering – the nurse assessor had simply added up the scores incorrectly. If I hadn’t seen the assessment form beforehand and roughly worked out Margaret’s likely score I would she had been awarded Funded Nursing Care and it only stopped a month after the award kicked in. Settling Margaret in the Care Home Perhaps this is more about settling myself and being happy that I have done my best for Margaret. Emotionally it was a very difficult for both of us. Paradoxically, however, Margaret’s condition helped her as she became less aware of her surroundings. That left me. Gradually I got used to the idea and what helped was: 1. Visiting every day; 2.Timing my visits for mealtimes. This gives me something to do and helps the staff; 3.Recognizing that Margaret and I are now part of a new community which is made up of other not have been in a position to challenge the residents and their families. Getting to know 26 minutes cont’ them, “sharing the problem”, has helped; are trying their best. They are under-resourced 4.Getting to know the staff, making sure that I and it’s not their fault that the system works so know their names, showing interest in them. badly. Allow them the benefit of doubt – it will In short, becoming friends with them; help win friends (and my goodness, you need 5.Making a contribution where I can, for example I wrote to the Council and got them to friends!) • Apply for benefits in good time; the process regularly inspect the road to the Nursing Home and persuaded them to make it a priority in involves running a marathon; • Network like fury – use every contact you bad weather. have (GP, Alzheimer’s Society, family, friends, acquaintances) and follow every lead – the Summary best information I received came from the most To summarize: • Make plans in advance. It is natural to put unexpected sources; • ABOVE ALL be persistent and stay cool. things off, but try not to. Making plans, however painful the process, will pay big I hope that this has been helpful and that I dividends; haven’t told you what you know already. • Recognize that the people you are dealing with 27 minutes cont’ PCA SUPPORT GROUP, SPECIFIC CARE NEEDS. 22 MARCH 2013; Wilkins Old Refectory, University College London. PCA Research Updates with opportunities for Questions and Small Group Sessions to discuss the specific needs and requirements of people facing a diagnosis of PCA Venue: We are again very grateful to UCL for the considerable variation in individuals, PCA use of these facilities. It is an ideal venue, well patients retain self-awareness and memory placed for access by public transport. skills much more than people with typical Attendees and Welcome: Jill welcomed 62 Alzheimer’s. attendees including 5 attending via Skype Questions from Ohio, Melbourne, Chester, Cambridge, 2.1 Does the diagnosis itself make a difference Northampton and Exeter. It was lovely to meet to behaviour? At present this has not been new members: we hope you enjoyed the meeting researched. The questionnaire was used and felt at ease with us: we look forward to you 5-6 years after diagnosis; there are plans joining us again and becoming old members! to repeat it at different intervals during the Seb sent his apologies; he is attending a meeting course of the illness. in Sweden. Members of the National PCA team 2.2 Does age affect the results? At present, wore green badges for easy identification during groups are mixed but we have plans to the 2 discussion sessions and hence could also separate age groups. be approached during the informal sessions 2.3 How do drugs affect the results? This before the meeting and during lunch. We hasn’t been looked at yet, but part of the thanked Grace Bulmer in her absence for her half questionnaire asks about what medications marathon fundraising efforts on behalf of the PCA patients are taking, so they should be able support group. Please visit http://www.justgiving. to look at whether there are any differences com/graceandtom between people on different medication or no medication. Programme: Tim Shakespeare on the 2.4 Can you collect information from more Cambridge Behavioural Inventory people, including working with other 1.1 Tim gave a presentation on the Cambridge research groups? At the moment, different Behavioural Inventory, which is a research groups in different parts of the questionnaire given to a friend or relative, world tend to use different tests, but designed to map the progress of the through the International Working Party on deterioration of skills in PCA sufferers PCA, the team hope to communicate the compared with more typical, memory-led results of their studies, so other groups can Alzheimer sufferers. So far around 30 carers use the same tests, if they’re found to be have filled out the questionnaire and there useful. are plans to roll it out more widely. 2.5 Question via Skype: are coloured lenses 1.2 The skills involved were, orientation, self- helpful? There is some evidence that care, memory, awareness), disinhibition yellow or blue lenses can be effective (loss of the ability to stop yourself doing for people with dyslexia, but there has things you should not do). Vision, numbers been very little research about this in and language skills were added later, PCA. It is something that Seb has plans to because these represent the strongest investigate. Please see the comment in the differences between PCA and typical ‘My Contributions’ section of this newsletter. Alzheimer’s disease. Although there is 2.6 Are there any useful I-phone apps? 28 minutes cont’ Some people have suggested using such. there is worth in collecting as many voice recognition, for example ‘Siri’. Voice types of sample as possible from people, recognition one is not yet fully developed, in case future tests mean that we are able and may still be difficult to use, hence not to retrospectively examine samples for completely useful for people with PCA. Jill biomarkers. Hence the request for people to suggests visiting www.dlf.org.uk/sara and provide urine samples at some clinic visits! parkinsons.org.uk for information on the 3.8 Does sense of smell play a role? Loss of new ‘EasyCall’ app. the sense of smell is an early symptom of Parkinson’s disease. Ross Patterson: Update on Aspects of Medical 3.9 How long are biological samples kept? Research into Neurology. The issue of consent needs to be clarified: 3.1 Speaking as a “medical” doctor, Ross the Royal College of Pathology has issued identified 5 important new strands in in new guidelines for consent being kept with research: International Collaboration, The samples. Samples kept at -70° can be Study of Genetic Factors, The Study of used, but proteins degrade if repeatedly Imaging, Multimodal Investigations, and thawed. Samples taken after 2008 are of The Importance of Cerebrospinal Fluid. higher quality, as improved containers have 3.2 International Developments: July 2012 saw the first international meeting of 38 been used. 3.10 Can the causes of PCA be confirmed after clinicians from 239 institutions worldwide death? PCA is a clinical syndrome which with a view standardizing terminology and applies in life. However, a post mortem to pooling and sharing resources. examination can confirm protein contents, 3.3 Genetic factors: There are currently very the presence of plaques etc. Such samples disparate associations involving genomes and genetic factors. The availability of are hugely valuable. 3.11 Questions from Skype re new drugs and worldwide blood samples represents a vital how far they can help (NB Not all of these step forward in such research. are licensed in the UK) Jill gets lots of 3.4 Research into Early Onset PCA i.e. in the questions re the value of taking vitamin 40’s 50’s and 60’s has been started with a supplements but cannot recommend them sample of 50 participants and 25 controls per se. Basically if they are helping, are not using MRI scans, neuro-psychological and doing harm and are not overpriced, some epidemiological testing. patients choose to continue with them. Very 3.5 Research into Cerebrospinal fluid: This few have been through stringent clinical fluid surrounds the brain and spinal cord studies, which makes proving their efficacy and hence is in direct contact with the very difficult. Anecdotal evidence then tends brain itself. It is hoped that this research to preside. SouvenaidDanone is a nutrient will elucidate the biological mechanisms cocktail which claims to improve memory involved and aid diagnosis. It can be used in people with Alzheimer’s disease: There to measure the individual’s response to are mixed views so far from users: some drug treatment. people have been helped. . Resveratrol, 3.6 Questions Can this fluid be used to rule a natural compound found in red wine, out other diseases? Yes, it can be used grape skins, blueberries, pomegranates to rule out cancer and certain types of and several other plants, has been found inflammation and is being used in other to benefit health in a myriad of ways and is areas. another example of a compound which it 3.7 Can a bio marker be found for PCA? This is difficult at the moment to comment upon is the subject of research at present. As scientifically. 29 minutes cont’ 3.12 Food Supplements are not regulated by NICE reading the individual letters. 4.6 Comment via Skype: the use of a 3.13 Aricept and Memantine are licensed in the background colour, particularly pink, can help. UK and are useful for Alzheimer’s: there is no specific evidence on the separate effects 4.7 Is there a connection between childhood dyslexia and PCA? This is not yet known. for PCA. 3.14 Medics in the USA have suggested using 4.8 What is the effect on opticians’ tests? a double dose. Is there any information on PCA sufferers cannot read top letters, they the efficacy of this? This is not known. are better with smaller ones. Their restricted 3.15 At what stage does Aricept become no vision means they can focus on individual longer useful? The policy at the National is letters: however there is a variation in the to continue with it, for as long as it is seen to consistency of perception – it can be erratic. be helping. There is sometimes a case to be made for trialing a period without Aricept. Small group session to discuss patients’ needs and service requirements following PCA Keir Yong: Acquired dyslexia in PCA. diagnosis. 4.1 Reading problems and difficulties in the 5.1 This was introduced by Robert Holman, perception of letters are amongst the early Care Commissioner from LB Camden, symptoms of PCA. Keir’s current research based on a project to assess the needs of is concerned with the reading of whole younger people with dementia The Camden passages. initiative has established the following 4.2 PCA sufferers can have poor peripheral vision, are often visually disorientated, perceived needs. 1 Sufferers need personalized and and may experience visual crowding (an consistent care: a series of new people excessive integration of visual information) coming in to provide care is disturbing. which may contribute to problems losing 2 The raising of awareness in all their place when reading a page or concerned. People’s concept of focusing on the relevant part of text. dementia is based on symptoms 4.3 Developing reading aids for PCA: there have been 11 participants so far. Accuracy observed in 80 and 90 year olds. 3There is a big need to better understand was increased from 56% to 95% when early onset dementia and hence to reading text displayed words at a time listen specifically to patients’ needs, so rather than all-at-once. Participants tended that they can be collated for the Clinical to find reading easier and more pleasant Commission. when using this method of reading. 4.4 The project seeks learn more about be fed to other Commissioners across London and ultimately nation-wide. perceptual manipulations which might facilitate reading in PCA and to begin 4Results from the questionnaires will 5The young onset group need more development of a computer-based aid next physical activities. Examples of good year. practice come from Cambridgeshire and 4.5 Questions. Why do PCA sufferers find Hampshire, where monthly walks and lunches have been very successful. it impossible to read phone numbers? Some PCA sufferers have great difficulty and sharing resources. with this because they need to look at numbers individually, on top of often having 7Data protection issues are a major concern in providing services. specific problems in processing numerical information. In reading words it is possible 6Boroughs should consider combining 8Comment via Skype: Employers need to be informed. perceiving the word as a whole rather than 30 minutes cont’ 5.2 We broke in to small groups of between activities in town and countryside, especially 6 and 8, with the aim of answering the question: What are the specific care for those with early onset dementia. 5.10 Feedback documents need to be available and service needs of people with PCA? in a general generic form from all support Feedback will be collated from similar groups. There should be a user friendly exercises with people across the different recognizable web site for all dementias. dementia groups. There will of course be detailed feedback via the newsletter in due course. The minutes contain a brief summary of the main points of today’s ideas. 5.3 General conclusions from Group 1. Other groups shared these - extra ideas are minuted separately. Patients and carers felt seriously alone with their diagnosis, which can be brusque and contain little introduction to the condition and scant explanation. They feel marginalized. Delays and poor liaison between agencies and departments, particularly with the GP are serious issues. There is a strong feeling that departments sit on files for too long. There is a need for everyone involved to understand medical terms, to know what lies ahead, and what the stages of the illness are. Driving was singled out as an area where advice and information is badly needed. 5.4 Personalised advice is very important e.g. in the area of handling money and personal spending. 5.5 Length of time in arriving at a diagnosis is a source of distress: there is a long route to the specialist’s opinion. 5.6 The lack of coherence between the local authority and the medical team is a minefield. There is a perceived need for a personal psychiatric nurse to explain what is happening or should happen. Allied to this is the need to have an overview of exactly what is available centrally, in one’s locality and in those nearby. 5.7 Hope is important: a bare diagnosis alone can be cold. 5.8 A single person is valuable to guide the sufferer throughout their illness. 5.9 There is a need for suitable leisure 31 Celia Heath




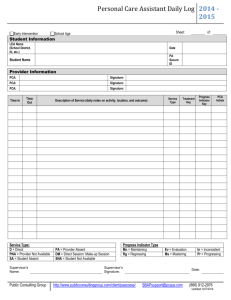
![See our handout on Classroom Access Personnel [doc]](http://s3.studylib.net/store/data/007033314_1-354ad15753436b5c05a8b4105c194a96-300x300.png)