MEdiCAL tRAining WitHoUt RiSK Published by the Faculty Development Office
advertisement
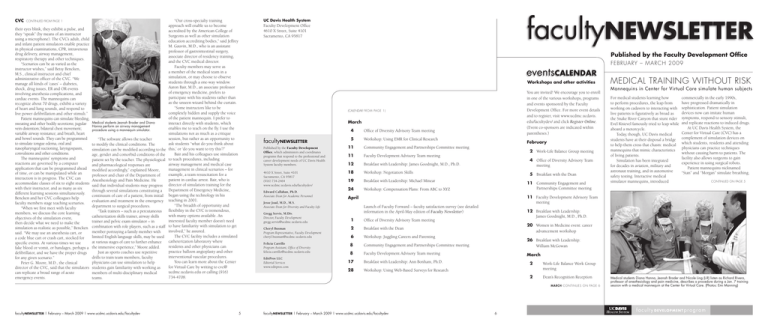
CVC continued from page 1 their eyes blink, they exhibit a pulse, and they “speak” (by means of an instructor using a microphone). The CVC’s adult, child and infant patient simulators enable practice in physical examinations, CPR, intravenous drug delivery, airway management, respiratory therapy and other techniques. “Scenarios can be as varied as the instructor wishes,” said Betsy Bencken, M.S., clinical instructor and chief administrative officer of the CVC. “We manage all kinds of ‘cases’ – diabetes, shock, drug issues, ER and OR events involving anesthesia complications, and cardiac events. The mannequins can recognize about 70 drugs, exhibit a variety of heart and lung sounds, and respond to live power defibrillation and other stimuli.” Patient mannequins can simulate bleeding, sweating and other bodily secretions; jugular vein distention; bilateral chest movement; variable airway resistance; and breath, heart and bowel sounds. They can be programmed to simulate tongue edema, oral and nasopharyngeal suctioning, laryngospasm, convulsions and other conditions. The mannequins’ symptoms and reactions are governed by a computer application that can be programmed ahead of time, or can be manipulated while an interaction is in progress. The CVC can accommodate classes of six to eight students with their instructor, and as many as six different learning sessions simultaneously. Bencken and her CVC colleagues help faculty members stage teaching scenarios. “When we first meet with faculty members, we discuss the core learning objectives of the simulation event, then decide what we need to make the simulation as realistic as possible,” Bencken said. “We may use an anesthesia cart, or a code blue cart or crash cart, stocked for specific events. At various times we use fake blood or vomit, or bandages, perhaps a defibrillator, and we have the proper drugs for any given scenario.” Peter G. Moore, M.D., the clinical director of the CVC, said that the simulators can replicate a broad range of acute emergency events. Medical students Jeanah Brader and Diana Hanna perform an airway management procedure using a mannequin simulator. “The software allows the teacher to modify the clinical conditions. The simulation can be modified according to the age, gender and comorbid conditions of the patient set by the teacher. The physiological and pharmacological responses are modified accordingly,” explained Moore, professor and chair of the Department of Anesthesiology and Pain Medicine. He said that individual students may progress through several simulations constituting a continuum of care of a patient, from initial evaluation and treatment in the emergency department to surgical procedures. “Task trainers – such as a percutaneous catheterization skills trainer, airway skills trainer and pelvic exam simulator – in combination with role players, such as a staff member portraying a family member with limited English language skills, may be used at various stages of care to further enhance the immersive experience,” Moore added. Just as sports coaches use repetitive drills to train team members, faculty physicians can use simulation to help students gain familiarity with working as members of multi-disciplinary medical teams. UC Davis Health System “Our cross-specialty training approach will enable us to become accredited by the American College of Surgeons as well as other simulation education accrediting bodies,” said Jeffrey M. Gauvin, M.D., who is an assistant professor of gastrointestinal surgery, associate director of residency training, and the CVC medical director. Faculty members may serve as a member of the medical team in a simulation, or may choose to observe students through a one-way window. Aaron Bair, M.D., an associate professor of emergency medicine, prefers to participate with his students rather than as the unseen wizard behind the curtain. “Some instructors like to be completely hidden and supply the voice of the patient mannequin. I prefer to interact directly with students, which enables me to teach on the fly. I use the simulations not as much as a critique session, but rather as an opportunity to ask students “what do you think about this,’ or ‘do you want to try this’?” Bair and his colleagues use simulation to teach procedures, including airway management and medical case management in clinical scenarios – for example, a team resuscitation for a patient in cardiac arrest. Bair, who is director of simulation training for the Department of Emergency Medicine, began using the technology in his teaching in 2001. “The breadth of opportunity and flexibility in the CVC is tremendous, with many options available. An interested faculty member doesn’t need to have familiarity with simulation to get involved,” he assured. The CVC facility includes a simulated catheterization laboratory where residents and other physicians can practice balloon angioplasty and other interventional vascular procedures. You can learn more about the Center for Virtual Care by writing to cvc@ ucdmc.ucdavis.edu or calling (916) 734-4708. Faculty Development Office 4610 X Street, Suite 4101 Sacramento, CA 95817 Published by the Faculty Development Office FEBRUARY – MARCH 2009 Workshops and other activities You are invited! We encourage you to enroll in one of the various workshops, programs and events sponsored by the Faculty Development Office. For more event details and to register, visit www.ucdmc.ucdavis. edu/facultydev/ and click Register Online. (Event co-sponsors are indicated within parentheses.) (Calendar from page 1) March facultyNewsletter Published by the Faculty Development Office, which administers and coordinates programs that respond to the professional and career development needs of UC Davis Health System faculty members. 4610 X Street, Suite 4101 Sacramento, CA 95817 (916) 734-2464 www.ucdmc.ucdavis.edu/facultydev/ Edward Callahan, Ph.D. Associate Dean for Academic Personnel Jesse Joad, M.D., M.S. Associate Dean for Diversity and Faculty Life Gregg Servis, M.Div. Director, Faculty Development gregg.servis@ucdmc.ucdavis.edu 4 Office of Diversity Advisory Team meeting 5 Workshop: Using EMR for Clinical Research February 11 Community Engagement and Partnerships Committee meeting 11 Faculty Development Advisory Team meeting 12 Breakfast with Leadership: James Goodnight, M.D., Ph.D. 4 Office of Diversity Advisory Team meeting 18 Workshop: Negotiation Skills 5 Breakfast with the Dean 19 Breakfast with Leadership: Michael Minear 24 Workshop: Compensation Plans: From ABC to XYZ 2 Work-Life Balance Group meeting 11 Community Engagement and Partnerships Committee meeting Launch of Faculty Forward – faculty satisfaction survey (see detailed information in the April-May edition of Faculty Newsletter) Office of Diversity Advisory Team meeting Cheryl Busman Program Representative, Faculty Development cheryl.busman@ucdmc.ucdavis.edu 2 Breakfast with the Dean 6 Workshop: Juggling Careers and Parenting Felicia Carrillo Program Assistant, Office of Diversity felicia.carrillo@ucdmc.ucdavis.edu 8 Community Engagement and Partnerships Committee meeting 26 Breakfast with Leadership: William McGowan 8 Faculty Development Advisory Team meeting March 17 Breakfast with Leadership: Ann Bonham, Ph.D. 28 Workshop: Using Web-Based Surveys for Research 5 facultyNewsletter | February – March 2009 | www.ucdmc.ucdavis.edu/facultydev commercially in the early 1990s, have progressed dramatically in sophistication. Patient simulation devices now can imitate human symptoms, respond to sensory stimuli, and replicate reactions to induced drugs. At UC Davis Health System, the Center for Virtual Care (CVC) has a complement of simulation devices on which students, residents and attending physicians can practice techniques without causing harm to patients. The facility also allows surgeons to gain experience in using surgical robots. Patient mannequins nicknamed “Stan” and “Morgan” simulate breathing, continued on page 5 20 Women in Medicine event: career advancement workshop 2 Work-Life Balance Work Group meeting 2 Dean’s Recognition Reception MARCH continues on page 6 facultyNewsletter | February – March 2009 | www.ucdmc.ucdavis.edu/facultydev For medical students learning how to perform procedures, the leap from working on cadavers to interacting with live patients is figuratively as broad as the Snake River Canyon that stunt rider Evel Knievel famously tried to leap while aboard a motorcycle. Today, though, UC Davis medical students have at their disposal a bridge to help them cross that chasm: medical mannequins that mimic characteristics of living patients. Simulation has been integrated for decades in aviation, military and astronaut training, and in automotive safety testing. Interactive medical simulator mannequins, introduced 12 Breakfast with Leadership: James Goodnight, M.D., Ph.D. 1 EditPros LLC Editorial Services www.editpros.com Mannequins in Center for Virtual Care simulate human subjects 11 Faculty Development Advisory Team meeting April MEDICAL TRAINING WITHOUT RISK 6 Medical students Diana Hanna, Jeanah Brader and Nicole Ling (L-R) listen as Richard Rivera, professor of anesthesiology and pain medicine, describes a procedure during a Jan. 7 training session with a medical mannequin at the Center for Virtual Care. (Photos: Emi Manning) officevisit P E DI AT R I C I A N S E R V E S L O W - IN C O M E K ID S STEP HAN IE WA LTON , M. D . , F. A . A . P Stephanie A. Walton, M.D., F.A.A.P., spent several years as a pediatric emergency physician, but these days she’s attending to a practice that is no less urgent than the demands of a pediatric emergency department. Now in private practice in Sacramento, Walton caters to urban patients whose access to medical care has been inconsistent or previously lacking. Her father, Dr. Vernon Walton – the first African-American pediatrician in Sacramento – established Walton Pediatrics in the 1960s. Stephanie oversees the practice’s business operations and sees patients, yet finds time to also serve as a volunteer clinical faculty member for the UC Davis Health System. Born in Fresno and reared in Sacramento, she obtained her M.D. degree from Howard University College of Medicine, where she became a clinical instructor, then assistant professor in pediatrics. She served as the director of ambulatory pediatrics at Howard University Hospital, where she completed her pediatric residency. Walton then moved to Children’s Hospital of Oakland, where she underwent fellowship training in pediatric emergency medicine. She began a career as an attending pediatric emergency physician at Los Angeles Children’s Hospital, Sunrise Children’s Hospital in Las Vegas and then Maricopa County Hospital in Phoenix. Her plans changed in 1998, however, when Vernon asked Stephanie to join him following the death of his practice partner. In addition to practicing alongside her father, she also works with her mother, Velma Walton, a registered nurse who serves as nurse manager of Walton Pediatrics. Stephanie is the practice’s medical director now that Vernon is semi-retired. Walton Pediatrics has 20 employees, including two other pediatricians and a pediatric nurse practitioner. The general pediatric practice has two offices – on East Southgate Drive in South Sacramento, and on Scripps Drive near CSU Sacramento. Patients include more than 4,000 Medi-Cal recipients. Walton intends to relocate the practice to the former Urban League Building at 3501 Broadway in Oak Park following eventual renovation of that structure. “Low-income kids come with a different set of problems than those patients of affluence,” she explained. “They often receive less preventative care than other kids; I see children who have poor dentition because they lack proper dental care, or kids who are obese because of a poor, high-fat diet. Many mothers are single, young and uneducated.” Walton knows her patients and their parents well, and talks about them with deep fondness. “One foster mom already had adopted two boys with medical problems. Then she came in with three more foster kids – siblings who she took into her home because she didn’t want to break facultyNewsletter | February – March 2009 | www.ucdmc.ucdavis.edu/facultydev facultyrounds viewpoint A welcome to new faculty colleagues By Claire Pomeroy, DEAN Donald M. Bers them up. The kids had been homeless on the street with their parents, who were schizophrenic. That foster mother eventually adopted the additional three kids,” Walton said. “I have one African-American foster mom who adopted a blond drug-addicted baby, two Hispanic kids and one AfricanAmerican kid. I derive my greatest sense of satisfaction from taking care of undeserved low-income kids.” Despite the caseload, Walton accepted an invitation to serve as a clinical instructor for the School of Medicine. Walton serves as a preceptor for thirdyear students. “Having worked all along at teaching institutions with residents and students, I enjoy having the teaching role again in private practice,” Walton said. Pediatric nephrologist Lavjay Butani, co-instructor of record for the third-year pediatric clerkship, said students tell him that Walton embodies selflessness and dedication to the community. Butani said students have described her as “compassionate, warm and approachable,” as “very inspirational,” and as an “excellent educator, pediatrician and mentor.” Walton Pediatrics runs the St. Hope Student Health Center at Sacramento Charter High School, in cooperation with HealthNet of California. “I volunteer my time, and receive payment only if we are able to bill a patient’s insurance,” Walton explained. She also is co-owner of Pediatric Urgent Care of Sacramento, an after-hours pediatric medical clinic near Methodist Hospital of Sacramento. “I once specialized in emergency medicine,” Walton said. ‘Now, serving the underserved, low-income child is my specialty.” advisoryteams Activities of the Faculty Development Office are guided by the recommendations of two advisory teams: Este Geraghty Faculty Development Advisory Team Each edition of the Faculty Newsletter introduces faculty colleagues who recently joined the UC Davis Health System family. Watch for more new clinical and research staff members in the next issue. Pharmacologist Donald Bers investigates cardiac function Donald M. Bers, Ph.D., distinguished professor and chair of the Department of Pharmacology, holds the Joseph Silva Endowed Chair for Cardiovascular Research. He studies the molecular and cellular activity involved in regulating cardiac function, especially the role of calcium in mediating electrical, contractile and signaling pathways in the heart. He is investigating changes that these systems undergo during heart failure and arrhythmias, and seeks to develop therapeutic strategies and computational models of electrical and signaling systems in the heart. Bers has been a Wellcome/FASEB visiting professor and the James DePauw endowed professor and physiology chair at Loyola University Chicago. He is an associate editor for the Journal of Molecular and Cellular Cardiology. Este Geraghty uses GIS to analyze health problems Newly board-certified in public health, Este Geraghty, M.D., M.S., M.P.H., C.P.H., supervises residents in the outpatient medicine clinics and on the medicine wards and general medicine consult service. Geraghty is conducting research in spatial epidemiology and geographic information systems (GIS), which involves spatial and geographic distribution of disease and/or exposures. GIS software performs spatial analysis and creates maps and diagrams to present data. Geraghty, an assistant professor of clinical internal medicine, is creating exposure prediction models for ambient pollutants, pollens and mold spores. 2 By using these models to adjust for confounding, she hopes to determine whether aerial pesticide spraying for West Nile virus correlated with respiratory irritation from the pesticide. Other new colleagues • April W. Armstrong, M.D., director of the Teledermatology Program, received her board certification in dermatology in November. Armstrong, an assistant professor of dermatology, is conducting clinical research in teledermatology, medication adherence and patient education. • The director of the Microbiology Laboratory in the Department of Medical Pathology and Laboratory Medicine is Chris Polage, M.D., an assistant professor of clinical pathology. Polage, a specialist in medical microbiology with board certifications in anatomic pathology, clinical pathology and medical microbiology, is investigating novel and more rapid approaches to diagnose infectious diseases. He is a scholar in the Mentored Clinical Research Training Program at UC Davis and is actively involved in projects to improve the diagnosis of Clostridium difficile infection and to develop point-of-care testing devices to diagnose bacteremia and fungemia. SIMULATION TECHNOLOGY IS A POWERFUL TEACHING TOOL Traditional medical training subscribed to the old adage “see one, do one, teach one.” Today at UC Davis, we embrace the concept of fully-demonstrated competence before a trainee interacts with a real patient. This new philosophy is possible due to new, cutting-edge learning venues like our Center for Virtual Care. At the center, students practice skills ranging from peripheral IV insertion to cardiac catheterization to team-based resuscitation. So, when they encounter clinical scenarios in the hospital or clinics, they have the expertise and confidence they need to provide the very best patient care. • Richard W. Dehn, M.P.A., is a certified physician assistant who performs medical workforce research. His studies have included ways to quantify the numbers and types • Thomas Sanchez, M.D., an of medical providers available to assistant professor of radiology, medically underserved populations. is a fellowship-trained pediatric Dehn, a clinical professor in the radiologist who has a particular Department of Family and Community interest in pediatric neuroradiology Medicine, is program director of and musculoskeletal imaging. He has the Family Nurse Practitioner and submitted several articles describing Physician Assistant Program (FNP/PA), common abdominal tumors in as well as a clinician in the UCDMC children to Contemporary Diagnostic family practice center. Radiology and on MRI imaging of • Statistician Chin-Shang Li, Ph.D., musculoskeletal trauma in children to an adjunct associate professor in the the MRI Clinics of North America, all Department of Public Health Sciences’ of which will be published in 2009. Division of Biostatistics, is studying • Anu Sinha, M.D., an assistant clinical lack-of-fit tests and zero-inflated professor of anesthesiology and pain Poisson models. A lack-of-fit test medicine, performs general anesthesia is conducted to determine whether and works in the liver transplant a postulated parametric model is program. He is board-certified by the appropriate. He also has expertise American Society of Anesthesiologists in cure models, semiparametric and by the California Society of and nonparametric regression, and generalized linear models. Anesthesiologists. facultyNewsletter | February – March 2009 | www.ucdmc.ucdavis.edu/facultydev New studies reveal that students who train using simulation have better patient outcomes. It’s not surprising, then, that accrediting bodies such as the LCME are starting to expect incorporation of simulation experiences into the curriculum. Helping tomorrow’s physicians gain “hands-on” experience – without ever putting a patient’s health in danger – is a powerful new approach to teaching and learning. Simulation technologies are dramatically changing the way we train health professions students. This training is valuable and effective for all the members of our health-care teams. Our high-tech mannequins can simulate complex situations that require 3 the attention of interdisciplinary groups of health professionals. Medical students, nursing students and other trainees can stand side-by-side to learn the critical importance of real-time collaboration in the clinical setting. Notably, this approach perfectly aligns with our emphasis on interprofessional education in our medical and nursing schools. Even health providers with decades of experience can learn something new by exploring our Center for Virtual Care. The robotic surgery simulator, for example, allows surgeons to make small incisions and use remote-controlled surgical tools. This technology supports minimally invasive surgery, resulting in less trauma, less pain, minimal scarring, faster recovery and shorter hospital stays. By exploring simulation technology, we have access to new ways to teach, to practice clinical skills and to do research. And this is just the beginning. At UC Davis Health System, we are even developing new simulation tools and techniques that will help future generations of health-care providers and their patients. Simulated patient experiences help empower both today’s and tomorrow’s health-care teams. If you haven’t already, I encourage you to take a formal tour of the Center for Virtual Care to learn more about the benefits of simulation technology. To schedule a tour, call (916) 734-4708. facultyNewsletter | February – March 2009 | www.ucdmc.ucdavis.edu/facultydev Gregg Servis, M.Div., Office of Faculty Development and Diversity Jesse Joad, M.D., M.S., Office of Faculty Development and Diversity Chuck Bevins, M.D., Ph.D., Medical Microbiology and Immunology Kathy DeRiemer, Ph.D., M.P.H., Public Health Sciences Tonya Fancher, M.D., M.P.H., Internal Medicine Jeff Gauvin, M.D., Surgery Estella Geraghty, M.D., M.S., M.P.H., Internal Medicine W. Ladson Hinton, M.D., Psychiatry and Behavioral Sciences Keith Lau, M.D., Pediatrics Jamie Ross, M.D., Internal Medicine Mark Sutter, M.D., Emergency Medicine Vicki Wheelock, M.D., Neurology Office of Diversity Advisory Team Jesse Joad, M.D., M.S., Office of Faculty Development and Diversity Gregg Servis, M.Div., Office of Faculty Development and Diversity Elizabeth Abad, Alumni and Development Officer, Health Sciences Advancement Susan DeMarois, Government and Community Relations James Forkin, Postbaccalaureate Program Coordinator, Office of Medical Education Darin Latimore, M.D., Office of Faculty Development and Diversity Russell Lim, M.D., Psychiatry and Behavioral Sciences José Morfin, M.D., Internal Medicine Marbella Sala, Executive Operations Manager, Center for Reducing Health Disparities Andreea Seritan, M.D., Psychiatry and Behavioral Sciences Pam Stotlar-McAuliffe, Manager, Continuing Medical Education Hendry Ton, M.D., Psychiatry Michelle Villegas-Frazier, Team Lead, Office of Diversity Bold type indicates team coordinators 4 officevisit P E DI AT R I C I A N S E R V E S L O W - IN C O M E K ID S STEP HAN IE WA LTON , M. D . , F. A . A . P Stephanie A. Walton, M.D., F.A.A.P., spent several years as a pediatric emergency physician, but these days she’s attending to a practice that is no less urgent than the demands of a pediatric emergency department. Now in private practice in Sacramento, Walton caters to urban patients whose access to medical care has been inconsistent or previously lacking. Her father, Dr. Vernon Walton – the first African-American pediatrician in Sacramento – established Walton Pediatrics in the 1960s. Stephanie oversees the practice’s business operations and sees patients, yet finds time to also serve as a volunteer clinical faculty member for the UC Davis Health System. Born in Fresno and reared in Sacramento, she obtained her M.D. degree from Howard University College of Medicine, where she became a clinical instructor, then assistant professor in pediatrics. She served as the director of ambulatory pediatrics at Howard University Hospital, where she completed her pediatric residency. Walton then moved to Children’s Hospital of Oakland, where she underwent fellowship training in pediatric emergency medicine. She began a career as an attending pediatric emergency physician at Los Angeles Children’s Hospital, Sunrise Children’s Hospital in Las Vegas and then Maricopa County Hospital in Phoenix. Her plans changed in 1998, however, when Vernon asked Stephanie to join him following the death of his practice partner. In addition to practicing alongside her father, she also works with her mother, Velma Walton, a registered nurse who serves as nurse manager of Walton Pediatrics. Stephanie is the practice’s medical director now that Vernon is semi-retired. Walton Pediatrics has 20 employees, including two other pediatricians and a pediatric nurse practitioner. The general pediatric practice has two offices – on East Southgate Drive in South Sacramento, and on Scripps Drive near CSU Sacramento. Patients include more than 4,000 Medi-Cal recipients. Walton intends to relocate the practice to the former Urban League Building at 3501 Broadway in Oak Park following eventual renovation of that structure. “Low-income kids come with a different set of problems than those patients of affluence,” she explained. “They often receive less preventative care than other kids; I see children who have poor dentition because they lack proper dental care, or kids who are obese because of a poor, high-fat diet. Many mothers are single, young and uneducated.” Walton knows her patients and their parents well, and talks about them with deep fondness. “One foster mom already had adopted two boys with medical problems. Then she came in with three more foster kids – siblings who she took into her home because she didn’t want to break facultyNewsletter | February – March 2009 | www.ucdmc.ucdavis.edu/facultydev facultyrounds viewpoint A welcome to new faculty colleagues By Claire Pomeroy, DEAN Donald M. Bers them up. The kids had been homeless on the street with their parents, who were schizophrenic. That foster mother eventually adopted the additional three kids,” Walton said. “I have one African-American foster mom who adopted a blond drug-addicted baby, two Hispanic kids and one AfricanAmerican kid. I derive my greatest sense of satisfaction from taking care of undeserved low-income kids.” Despite the caseload, Walton accepted an invitation to serve as a clinical instructor for the School of Medicine. Walton serves as a preceptor for thirdyear students. “Having worked all along at teaching institutions with residents and students, I enjoy having the teaching role again in private practice,” Walton said. Pediatric nephrologist Lavjay Butani, co-instructor of record for the third-year pediatric clerkship, said students tell him that Walton embodies selflessness and dedication to the community. Butani said students have described her as “compassionate, warm and approachable,” as “very inspirational,” and as an “excellent educator, pediatrician and mentor.” Walton Pediatrics runs the St. Hope Student Health Center at Sacramento Charter High School, in cooperation with HealthNet of California. “I volunteer my time, and receive payment only if we are able to bill a patient’s insurance,” Walton explained. She also is co-owner of Pediatric Urgent Care of Sacramento, an after-hours pediatric medical clinic near Methodist Hospital of Sacramento. “I once specialized in emergency medicine,” Walton said. ‘Now, serving the underserved, low-income child is my specialty.” advisoryteams Activities of the Faculty Development Office are guided by the recommendations of two advisory teams: Este Geraghty Faculty Development Advisory Team Each edition of the Faculty Newsletter introduces faculty colleagues who recently joined the UC Davis Health System family. Watch for more new clinical and research staff members in the next issue. Pharmacologist Donald Bers investigates cardiac function Donald M. Bers, Ph.D., distinguished professor and chair of the Department of Pharmacology, holds the Joseph Silva Endowed Chair for Cardiovascular Research. He studies the molecular and cellular activity involved in regulating cardiac function, especially the role of calcium in mediating electrical, contractile and signaling pathways in the heart. He is investigating changes that these systems undergo during heart failure and arrhythmias, and seeks to develop therapeutic strategies and computational models of electrical and signaling systems in the heart. Bers has been a Wellcome/FASEB visiting professor and the James DePauw endowed professor and physiology chair at Loyola University Chicago. He is an associate editor for the Journal of Molecular and Cellular Cardiology. Este Geraghty uses GIS to analyze health problems Newly board-certified in public health, Este Geraghty, M.D., M.S., M.P.H., C.P.H., supervises residents in the outpatient medicine clinics and on the medicine wards and general medicine consult service. Geraghty is conducting research in spatial epidemiology and geographic information systems (GIS), which involves spatial and geographic distribution of disease and/or exposures. GIS software performs spatial analysis and creates maps and diagrams to present data. Geraghty, an assistant professor of clinical internal medicine, is creating exposure prediction models for ambient pollutants, pollens and mold spores. 2 By using these models to adjust for confounding, she hopes to determine whether aerial pesticide spraying for West Nile virus correlated with respiratory irritation from the pesticide. Other new colleagues • April W. Armstrong, M.D., director of the Teledermatology Program, received her board certification in dermatology in November. Armstrong, an assistant professor of dermatology, is conducting clinical research in teledermatology, medication adherence and patient education. • The director of the Microbiology Laboratory in the Department of Medical Pathology and Laboratory Medicine is Chris Polage, M.D., an assistant professor of clinical pathology. Polage, a specialist in medical microbiology with board certifications in anatomic pathology, clinical pathology and medical microbiology, is investigating novel and more rapid approaches to diagnose infectious diseases. He is a scholar in the Mentored Clinical Research Training Program at UC Davis and is actively involved in projects to improve the diagnosis of Clostridium difficile infection and to develop point-of-care testing devices to diagnose bacteremia and fungemia. SIMULATION TECHNOLOGY IS A POWERFUL TEACHING TOOL Traditional medical training subscribed to the old adage “see one, do one, teach one.” Today at UC Davis, we embrace the concept of fully-demonstrated competence before a trainee interacts with a real patient. This new philosophy is possible due to new, cutting-edge learning venues like our Center for Virtual Care. At the center, students practice skills ranging from peripheral IV insertion to cardiac catheterization to team-based resuscitation. So, when they encounter clinical scenarios in the hospital or clinics, they have the expertise and confidence they need to provide the very best patient care. • Richard W. Dehn, M.P.A., is a certified physician assistant who performs medical workforce research. His studies have included ways to quantify the numbers and types • Thomas Sanchez, M.D., an of medical providers available to assistant professor of radiology, medically underserved populations. is a fellowship-trained pediatric Dehn, a clinical professor in the radiologist who has a particular Department of Family and Community interest in pediatric neuroradiology Medicine, is program director of and musculoskeletal imaging. He has the Family Nurse Practitioner and submitted several articles describing Physician Assistant Program (FNP/PA), common abdominal tumors in as well as a clinician in the UCDMC children to Contemporary Diagnostic family practice center. Radiology and on MRI imaging of • Statistician Chin-Shang Li, Ph.D., musculoskeletal trauma in children to an adjunct associate professor in the the MRI Clinics of North America, all Department of Public Health Sciences’ of which will be published in 2009. Division of Biostatistics, is studying • Anu Sinha, M.D., an assistant clinical lack-of-fit tests and zero-inflated professor of anesthesiology and pain Poisson models. A lack-of-fit test medicine, performs general anesthesia is conducted to determine whether and works in the liver transplant a postulated parametric model is program. He is board-certified by the appropriate. He also has expertise American Society of Anesthesiologists in cure models, semiparametric and by the California Society of and nonparametric regression, and generalized linear models. Anesthesiologists. facultyNewsletter | February – March 2009 | www.ucdmc.ucdavis.edu/facultydev New studies reveal that students who train using simulation have better patient outcomes. It’s not surprising, then, that accrediting bodies such as the LCME are starting to expect incorporation of simulation experiences into the curriculum. Helping tomorrow’s physicians gain “hands-on” experience – without ever putting a patient’s health in danger – is a powerful new approach to teaching and learning. Simulation technologies are dramatically changing the way we train health professions students. This training is valuable and effective for all the members of our health-care teams. Our high-tech mannequins can simulate complex situations that require 3 the attention of interdisciplinary groups of health professionals. Medical students, nursing students and other trainees can stand side-by-side to learn the critical importance of real-time collaboration in the clinical setting. Notably, this approach perfectly aligns with our emphasis on interprofessional education in our medical and nursing schools. Even health providers with decades of experience can learn something new by exploring our Center for Virtual Care. The robotic surgery simulator, for example, allows surgeons to make small incisions and use remote-controlled surgical tools. This technology supports minimally invasive surgery, resulting in less trauma, less pain, minimal scarring, faster recovery and shorter hospital stays. By exploring simulation technology, we have access to new ways to teach, to practice clinical skills and to do research. And this is just the beginning. At UC Davis Health System, we are even developing new simulation tools and techniques that will help future generations of health-care providers and their patients. Simulated patient experiences help empower both today’s and tomorrow’s health-care teams. If you haven’t already, I encourage you to take a formal tour of the Center for Virtual Care to learn more about the benefits of simulation technology. To schedule a tour, call (916) 734-4708. facultyNewsletter | February – March 2009 | www.ucdmc.ucdavis.edu/facultydev Gregg Servis, M.Div., Office of Faculty Development and Diversity Jesse Joad, M.D., M.S., Office of Faculty Development and Diversity Chuck Bevins, M.D., Ph.D., Medical Microbiology and Immunology Kathy DeRiemer, Ph.D., M.P.H., Public Health Sciences Tonya Fancher, M.D., M.P.H., Internal Medicine Jeff Gauvin, M.D., Surgery Estella Geraghty, M.D., M.S., M.P.H., Internal Medicine W. Ladson Hinton, M.D., Psychiatry and Behavioral Sciences Keith Lau, M.D., Pediatrics Jamie Ross, M.D., Internal Medicine Mark Sutter, M.D., Emergency Medicine Vicki Wheelock, M.D., Neurology Office of Diversity Advisory Team Jesse Joad, M.D., M.S., Office of Faculty Development and Diversity Gregg Servis, M.Div., Office of Faculty Development and Diversity Elizabeth Abad, Alumni and Development Officer, Health Sciences Advancement Susan DeMarois, Government and Community Relations James Forkin, Postbaccalaureate Program Coordinator, Office of Medical Education Darin Latimore, M.D., Office of Faculty Development and Diversity Russell Lim, M.D., Psychiatry and Behavioral Sciences José Morfin, M.D., Internal Medicine Marbella Sala, Executive Operations Manager, Center for Reducing Health Disparities Andreea Seritan, M.D., Psychiatry and Behavioral Sciences Pam Stotlar-McAuliffe, Manager, Continuing Medical Education Hendry Ton, M.D., Psychiatry Michelle Villegas-Frazier, Team Lead, Office of Diversity Bold type indicates team coordinators 4 officevisit P E DI AT R I C I A N S E R V E S L O W - IN C O M E K ID S STEP HAN IE WA LTON , M. D . , F. A . A . P Stephanie A. Walton, M.D., F.A.A.P., spent several years as a pediatric emergency physician, but these days she’s attending to a practice that is no less urgent than the demands of a pediatric emergency department. Now in private practice in Sacramento, Walton caters to urban patients whose access to medical care has been inconsistent or previously lacking. Her father, Dr. Vernon Walton – the first African-American pediatrician in Sacramento – established Walton Pediatrics in the 1960s. Stephanie oversees the practice’s business operations and sees patients, yet finds time to also serve as a volunteer clinical faculty member for the UC Davis Health System. Born in Fresno and reared in Sacramento, she obtained her M.D. degree from Howard University College of Medicine, where she became a clinical instructor, then assistant professor in pediatrics. She served as the director of ambulatory pediatrics at Howard University Hospital, where she completed her pediatric residency. Walton then moved to Children’s Hospital of Oakland, where she underwent fellowship training in pediatric emergency medicine. She began a career as an attending pediatric emergency physician at Los Angeles Children’s Hospital, Sunrise Children’s Hospital in Las Vegas and then Maricopa County Hospital in Phoenix. Her plans changed in 1998, however, when Vernon asked Stephanie to join him following the death of his practice partner. In addition to practicing alongside her father, she also works with her mother, Velma Walton, a registered nurse who serves as nurse manager of Walton Pediatrics. Stephanie is the practice’s medical director now that Vernon is semi-retired. Walton Pediatrics has 20 employees, including two other pediatricians and a pediatric nurse practitioner. The general pediatric practice has two offices – on East Southgate Drive in South Sacramento, and on Scripps Drive near CSU Sacramento. Patients include more than 4,000 Medi-Cal recipients. Walton intends to relocate the practice to the former Urban League Building at 3501 Broadway in Oak Park following eventual renovation of that structure. “Low-income kids come with a different set of problems than those patients of affluence,” she explained. “They often receive less preventative care than other kids; I see children who have poor dentition because they lack proper dental care, or kids who are obese because of a poor, high-fat diet. Many mothers are single, young and uneducated.” Walton knows her patients and their parents well, and talks about them with deep fondness. “One foster mom already had adopted two boys with medical problems. Then she came in with three more foster kids – siblings who she took into her home because she didn’t want to break facultyNewsletter | February – March 2009 | www.ucdmc.ucdavis.edu/facultydev facultyrounds viewpoint A welcome to new faculty colleagues By Claire Pomeroy, DEAN Donald M. Bers them up. The kids had been homeless on the street with their parents, who were schizophrenic. That foster mother eventually adopted the additional three kids,” Walton said. “I have one African-American foster mom who adopted a blond drug-addicted baby, two Hispanic kids and one AfricanAmerican kid. I derive my greatest sense of satisfaction from taking care of undeserved low-income kids.” Despite the caseload, Walton accepted an invitation to serve as a clinical instructor for the School of Medicine. Walton serves as a preceptor for thirdyear students. “Having worked all along at teaching institutions with residents and students, I enjoy having the teaching role again in private practice,” Walton said. Pediatric nephrologist Lavjay Butani, co-instructor of record for the third-year pediatric clerkship, said students tell him that Walton embodies selflessness and dedication to the community. Butani said students have described her as “compassionate, warm and approachable,” as “very inspirational,” and as an “excellent educator, pediatrician and mentor.” Walton Pediatrics runs the St. Hope Student Health Center at Sacramento Charter High School, in cooperation with HealthNet of California. “I volunteer my time, and receive payment only if we are able to bill a patient’s insurance,” Walton explained. She also is co-owner of Pediatric Urgent Care of Sacramento, an after-hours pediatric medical clinic near Methodist Hospital of Sacramento. “I once specialized in emergency medicine,” Walton said. ‘Now, serving the underserved, low-income child is my specialty.” advisoryteams Activities of the Faculty Development Office are guided by the recommendations of two advisory teams: Este Geraghty Faculty Development Advisory Team Each edition of the Faculty Newsletter introduces faculty colleagues who recently joined the UC Davis Health System family. Watch for more new clinical and research staff members in the next issue. Pharmacologist Donald Bers investigates cardiac function Donald M. Bers, Ph.D., distinguished professor and chair of the Department of Pharmacology, holds the Joseph Silva Endowed Chair for Cardiovascular Research. He studies the molecular and cellular activity involved in regulating cardiac function, especially the role of calcium in mediating electrical, contractile and signaling pathways in the heart. He is investigating changes that these systems undergo during heart failure and arrhythmias, and seeks to develop therapeutic strategies and computational models of electrical and signaling systems in the heart. Bers has been a Wellcome/FASEB visiting professor and the James DePauw endowed professor and physiology chair at Loyola University Chicago. He is an associate editor for the Journal of Molecular and Cellular Cardiology. Este Geraghty uses GIS to analyze health problems Newly board-certified in public health, Este Geraghty, M.D., M.S., M.P.H., C.P.H., supervises residents in the outpatient medicine clinics and on the medicine wards and general medicine consult service. Geraghty is conducting research in spatial epidemiology and geographic information systems (GIS), which involves spatial and geographic distribution of disease and/or exposures. GIS software performs spatial analysis and creates maps and diagrams to present data. Geraghty, an assistant professor of clinical internal medicine, is creating exposure prediction models for ambient pollutants, pollens and mold spores. 2 By using these models to adjust for confounding, she hopes to determine whether aerial pesticide spraying for West Nile virus correlated with respiratory irritation from the pesticide. Other new colleagues • April W. Armstrong, M.D., director of the Teledermatology Program, received her board certification in dermatology in November. Armstrong, an assistant professor of dermatology, is conducting clinical research in teledermatology, medication adherence and patient education. • The director of the Microbiology Laboratory in the Department of Medical Pathology and Laboratory Medicine is Chris Polage, M.D., an assistant professor of clinical pathology. Polage, a specialist in medical microbiology with board certifications in anatomic pathology, clinical pathology and medical microbiology, is investigating novel and more rapid approaches to diagnose infectious diseases. He is a scholar in the Mentored Clinical Research Training Program at UC Davis and is actively involved in projects to improve the diagnosis of Clostridium difficile infection and to develop point-of-care testing devices to diagnose bacteremia and fungemia. SIMULATION TECHNOLOGY IS A POWERFUL TEACHING TOOL Traditional medical training subscribed to the old adage “see one, do one, teach one.” Today at UC Davis, we embrace the concept of fully-demonstrated competence before a trainee interacts with a real patient. This new philosophy is possible due to new, cutting-edge learning venues like our Center for Virtual Care. At the center, students practice skills ranging from peripheral IV insertion to cardiac catheterization to team-based resuscitation. So, when they encounter clinical scenarios in the hospital or clinics, they have the expertise and confidence they need to provide the very best patient care. • Richard W. Dehn, M.P.A., is a certified physician assistant who performs medical workforce research. His studies have included ways to quantify the numbers and types • Thomas Sanchez, M.D., an of medical providers available to assistant professor of radiology, medically underserved populations. is a fellowship-trained pediatric Dehn, a clinical professor in the radiologist who has a particular Department of Family and Community interest in pediatric neuroradiology Medicine, is program director of and musculoskeletal imaging. He has the Family Nurse Practitioner and submitted several articles describing Physician Assistant Program (FNP/PA), common abdominal tumors in as well as a clinician in the UCDMC children to Contemporary Diagnostic family practice center. Radiology and on MRI imaging of • Statistician Chin-Shang Li, Ph.D., musculoskeletal trauma in children to an adjunct associate professor in the the MRI Clinics of North America, all Department of Public Health Sciences’ of which will be published in 2009. Division of Biostatistics, is studying • Anu Sinha, M.D., an assistant clinical lack-of-fit tests and zero-inflated professor of anesthesiology and pain Poisson models. A lack-of-fit test medicine, performs general anesthesia is conducted to determine whether and works in the liver transplant a postulated parametric model is program. He is board-certified by the appropriate. He also has expertise American Society of Anesthesiologists in cure models, semiparametric and by the California Society of and nonparametric regression, and generalized linear models. Anesthesiologists. facultyNewsletter | February – March 2009 | www.ucdmc.ucdavis.edu/facultydev New studies reveal that students who train using simulation have better patient outcomes. It’s not surprising, then, that accrediting bodies such as the LCME are starting to expect incorporation of simulation experiences into the curriculum. Helping tomorrow’s physicians gain “hands-on” experience – without ever putting a patient’s health in danger – is a powerful new approach to teaching and learning. Simulation technologies are dramatically changing the way we train health professions students. This training is valuable and effective for all the members of our health-care teams. Our high-tech mannequins can simulate complex situations that require 3 the attention of interdisciplinary groups of health professionals. Medical students, nursing students and other trainees can stand side-by-side to learn the critical importance of real-time collaboration in the clinical setting. Notably, this approach perfectly aligns with our emphasis on interprofessional education in our medical and nursing schools. Even health providers with decades of experience can learn something new by exploring our Center for Virtual Care. The robotic surgery simulator, for example, allows surgeons to make small incisions and use remote-controlled surgical tools. This technology supports minimally invasive surgery, resulting in less trauma, less pain, minimal scarring, faster recovery and shorter hospital stays. By exploring simulation technology, we have access to new ways to teach, to practice clinical skills and to do research. And this is just the beginning. At UC Davis Health System, we are even developing new simulation tools and techniques that will help future generations of health-care providers and their patients. Simulated patient experiences help empower both today’s and tomorrow’s health-care teams. If you haven’t already, I encourage you to take a formal tour of the Center for Virtual Care to learn more about the benefits of simulation technology. To schedule a tour, call (916) 734-4708. facultyNewsletter | February – March 2009 | www.ucdmc.ucdavis.edu/facultydev Gregg Servis, M.Div., Office of Faculty Development and Diversity Jesse Joad, M.D., M.S., Office of Faculty Development and Diversity Chuck Bevins, M.D., Ph.D., Medical Microbiology and Immunology Kathy DeRiemer, Ph.D., M.P.H., Public Health Sciences Tonya Fancher, M.D., M.P.H., Internal Medicine Jeff Gauvin, M.D., Surgery Estella Geraghty, M.D., M.S., M.P.H., Internal Medicine W. Ladson Hinton, M.D., Psychiatry and Behavioral Sciences Keith Lau, M.D., Pediatrics Jamie Ross, M.D., Internal Medicine Mark Sutter, M.D., Emergency Medicine Vicki Wheelock, M.D., Neurology Office of Diversity Advisory Team Jesse Joad, M.D., M.S., Office of Faculty Development and Diversity Gregg Servis, M.Div., Office of Faculty Development and Diversity Elizabeth Abad, Alumni and Development Officer, Health Sciences Advancement Susan DeMarois, Government and Community Relations James Forkin, Postbaccalaureate Program Coordinator, Office of Medical Education Darin Latimore, M.D., Office of Faculty Development and Diversity Russell Lim, M.D., Psychiatry and Behavioral Sciences José Morfin, M.D., Internal Medicine Marbella Sala, Executive Operations Manager, Center for Reducing Health Disparities Andreea Seritan, M.D., Psychiatry and Behavioral Sciences Pam Stotlar-McAuliffe, Manager, Continuing Medical Education Hendry Ton, M.D., Psychiatry Michelle Villegas-Frazier, Team Lead, Office of Diversity Bold type indicates team coordinators 4 CVC continued from page 1 their eyes blink, they exhibit a pulse, and they “speak” (by means of an instructor using a microphone). The CVC’s adult, child and infant patient simulators enable practice in physical examinations, CPR, intravenous drug delivery, airway management, respiratory therapy and other techniques. “Scenarios can be as varied as the instructor wishes,” said Betsy Bencken, M.S., clinical instructor and chief administrative officer of the CVC. “We manage all kinds of ‘cases’ – diabetes, shock, drug issues, ER and OR events involving anesthesia complications, and cardiac events. The mannequins can recognize about 70 drugs, exhibit a variety of heart and lung sounds, and respond to live power defibrillation and other stimuli.” Patient mannequins can simulate bleeding, sweating and other bodily secretions; jugular vein distention; bilateral chest movement; variable airway resistance; and breath, heart and bowel sounds. They can be programmed to simulate tongue edema, oral and nasopharyngeal suctioning, laryngospasm, convulsions and other conditions. The mannequins’ symptoms and reactions are governed by a computer application that can be programmed ahead of time, or can be manipulated while an interaction is in progress. The CVC can accommodate classes of six to eight students with their instructor, and as many as six different learning sessions simultaneously. Bencken and her CVC colleagues help faculty members stage teaching scenarios. “When we first meet with faculty members, we discuss the core learning objectives of the simulation event, then decide what we need to make the simulation as realistic as possible,” Bencken said. “We may use an anesthesia cart, or a code blue cart or crash cart, stocked for specific events. At various times we use fake blood or vomit, or bandages, perhaps a defibrillator, and we have the proper drugs for any given scenario.” Peter G. Moore, M.D., the clinical director of the CVC, said that the simulators can replicate a broad range of acute emergency events. Medical students Jeanah Brader and Diana Hanna perform an airway management procedure using a mannequin simulator. “The software allows the teacher to modify the clinical conditions. The simulation can be modified according to the age, gender and comorbid conditions of the patient set by the teacher. The physiological and pharmacological responses are modified accordingly,” explained Moore, professor and chair of the Department of Anesthesiology and Pain Medicine. He said that individual students may progress through several simulations constituting a continuum of care of a patient, from initial evaluation and treatment in the emergency department to surgical procedures. “Task trainers – such as a percutaneous catheterization skills trainer, airway skills trainer and pelvic exam simulator – in combination with role players, such as a staff member portraying a family member with limited English language skills, may be used at various stages of care to further enhance the immersive experience,” Moore added. Just as sports coaches use repetitive drills to train team members, faculty physicians can use simulation to help students gain familiarity with working as members of multi-disciplinary medical teams. UC Davis Health System “Our cross-specialty training approach will enable us to become accredited by the American College of Surgeons as well as other simulation education accrediting bodies,” said Jeffrey M. Gauvin, M.D., who is an assistant professor of gastrointestinal surgery, associate director of residency training, and the CVC medical director. Faculty members may serve as a member of the medical team in a simulation, or may choose to observe students through a one-way window. Aaron Bair, M.D., an associate professor of emergency medicine, prefers to participate with his students rather than as the unseen wizard behind the curtain. “Some instructors like to be completely hidden and supply the voice of the patient mannequin. I prefer to interact directly with students, which enables me to teach on the fly. I use the simulations not as much as a critique session, but rather as an opportunity to ask students “what do you think about this,’ or ‘do you want to try this’?” Bair and his colleagues use simulation to teach procedures, including airway management and medical case management in clinical scenarios – for example, a team resuscitation for a patient in cardiac arrest. Bair, who is director of simulation training for the Department of Emergency Medicine, began using the technology in his teaching in 2001. “The breadth of opportunity and flexibility in the CVC is tremendous, with many options available. An interested faculty member doesn’t need to have familiarity with simulation to get involved,” he assured. The CVC facility includes a simulated catheterization laboratory where residents and other physicians can practice balloon angioplasty and other interventional vascular procedures. You can learn more about the Center for Virtual Care by writing to cvc@ ucdmc.ucdavis.edu or calling (916) 734-4708. Faculty Development Office 4610 X Street, Suite 4101 Sacramento, CA 95817 Published by the Faculty Development Office FEBRUARY – MARCH 2009 Workshops and other activities You are invited! We encourage you to enroll in one of the various workshops, programs and events sponsored by the Faculty Development Office. For more event details and to register, visit www.ucdmc.ucdavis. edu/facultydev/ and click Register Online. (Event co-sponsors are indicated within parentheses.) (Calendar from page 1) March facultyNewsletter Published by the Faculty Development Office, which administers and coordinates programs that respond to the professional and career development needs of UC Davis Health System faculty members. 4610 X Street, Suite 4101 Sacramento, CA 95817 (916) 734-2464 www.ucdmc.ucdavis.edu/facultydev/ Edward Callahan, Ph.D. Associate Dean for Academic Personnel Jesse Joad, M.D., M.S. Associate Dean for Diversity and Faculty Life Gregg Servis, M.Div. Director, Faculty Development gregg.servis@ucdmc.ucdavis.edu 4 Office of Diversity Advisory Team meeting 5 Workshop: Using EMR for Clinical Research February 11 Community Engagement and Partnerships Committee meeting 11 Faculty Development Advisory Team meeting 12 Breakfast with Leadership: James Goodnight, M.D., Ph.D. 4 Office of Diversity Advisory Team meeting 18 Workshop: Negotiation Skills 5 Breakfast with the Dean 19 Breakfast with Leadership: Michael Minear 24 Workshop: Compensation Plans: From ABC to XYZ 2 Work-Life Balance Group meeting 11 Community Engagement and Partnerships Committee meeting Launch of Faculty Forward – faculty satisfaction survey (see detailed information in the April-May edition of Faculty Newsletter) Office of Diversity Advisory Team meeting Cheryl Busman Program Representative, Faculty Development cheryl.busman@ucdmc.ucdavis.edu 2 Breakfast with the Dean 6 Workshop: Juggling Careers and Parenting Felicia Carrillo Program Assistant, Office of Diversity felicia.carrillo@ucdmc.ucdavis.edu 8 Community Engagement and Partnerships Committee meeting 26 Breakfast with Leadership: William McGowan 8 Faculty Development Advisory Team meeting March 17 Breakfast with Leadership: Ann Bonham, Ph.D. 28 Workshop: Using Web-Based Surveys for Research 5 facultyNewsletter | February – March 2009 | www.ucdmc.ucdavis.edu/facultydev commercially in the early 1990s, have progressed dramatically in sophistication. Patient simulation devices now can imitate human symptoms, respond to sensory stimuli, and replicate reactions to induced drugs. At UC Davis Health System, the Center for Virtual Care (CVC) has a complement of simulation devices on which students, residents and attending physicians can practice techniques without causing harm to patients. The facility also allows surgeons to gain experience in using surgical robots. Patient mannequins nicknamed “Stan” and “Morgan” simulate breathing, continued on page 5 20 Women in Medicine event: career advancement workshop 2 Work-Life Balance Work Group meeting 2 Dean’s Recognition Reception MARCH continues on page 6 facultyNewsletter | February – March 2009 | www.ucdmc.ucdavis.edu/facultydev For medical students learning how to perform procedures, the leap from working on cadavers to interacting with live patients is figuratively as broad as the Snake River Canyon that stunt rider Evel Knievel famously tried to leap while aboard a motorcycle. Today, though, UC Davis medical students have at their disposal a bridge to help them cross that chasm: medical mannequins that mimic characteristics of living patients. Simulation has been integrated for decades in aviation, military and astronaut training, and in automotive safety testing. Interactive medical simulator mannequins, introduced 12 Breakfast with Leadership: James Goodnight, M.D., Ph.D. 1 EditPros LLC Editorial Services www.editpros.com Mannequins in Center for Virtual Care simulate human subjects 11 Faculty Development Advisory Team meeting April MEDICAL TRAINING WITHOUT RISK 6 Medical students Diana Hanna, Jeanah Brader and Nicole Ling (L-R) listen as Richard Rivera, professor of anesthesiology and pain medicine, describes a procedure during a Jan. 7 training session with a medical mannequin at the Center for Virtual Care. (Photos: Emi Manning) CVC continued from page 1 their eyes blink, they exhibit a pulse, and they “speak” (by means of an instructor using a microphone). The CVC’s adult, child and infant patient simulators enable practice in physical examinations, CPR, intravenous drug delivery, airway management, respiratory therapy and other techniques. “Scenarios can be as varied as the instructor wishes,” said Betsy Bencken, M.S., clinical instructor and chief administrative officer of the CVC. “We manage all kinds of ‘cases’ – diabetes, shock, drug issues, ER and OR events involving anesthesia complications, and cardiac events. The mannequins can recognize about 70 drugs, exhibit a variety of heart and lung sounds, and respond to live power defibrillation and other stimuli.” Patient mannequins can simulate bleeding, sweating and other bodily secretions; jugular vein distention; bilateral chest movement; variable airway resistance; and breath, heart and bowel sounds. They can be programmed to simulate tongue edema, oral and nasopharyngeal suctioning, laryngospasm, convulsions and other conditions. The mannequins’ symptoms and reactions are governed by a computer application that can be programmed ahead of time, or can be manipulated while an interaction is in progress. The CVC can accommodate classes of six to eight students with their instructor, and as many as six different learning sessions simultaneously. Bencken and her CVC colleagues help faculty members stage teaching scenarios. “When we first meet with faculty members, we discuss the core learning objectives of the simulation event, then decide what we need to make the simulation as realistic as possible,” Bencken said. “We may use an anesthesia cart, or a code blue cart or crash cart, stocked for specific events. At various times we use fake blood or vomit, or bandages, perhaps a defibrillator, and we have the proper drugs for any given scenario.” Peter G. Moore, M.D., the clinical director of the CVC, said that the simulators can replicate a broad range of acute emergency events. Medical students Jeanah Brader and Diana Hanna perform an airway management procedure using a mannequin simulator. “The software allows the teacher to modify the clinical conditions. The simulation can be modified according to the age, gender and comorbid conditions of the patient set by the teacher. The physiological and pharmacological responses are modified accordingly,” explained Moore, professor and chair of the Department of Anesthesiology and Pain Medicine. He said that individual students may progress through several simulations constituting a continuum of care of a patient, from initial evaluation and treatment in the emergency department to surgical procedures. “Task trainers – such as a percutaneous catheterization skills trainer, airway skills trainer and pelvic exam simulator – in combination with role players, such as a staff member portraying a family member with limited English language skills, may be used at various stages of care to further enhance the immersive experience,” Moore added. Just as sports coaches use repetitive drills to train team members, faculty physicians can use simulation to help students gain familiarity with working as members of multi-disciplinary medical teams. UC Davis Health System “Our cross-specialty training approach will enable us to become accredited by the American College of Surgeons as well as other simulation education accrediting bodies,” said Jeffrey M. Gauvin, M.D., who is an assistant professor of gastrointestinal surgery, associate director of residency training, and the CVC medical director. Faculty members may serve as a member of the medical team in a simulation, or may choose to observe students through a one-way window. Aaron Bair, M.D., an associate professor of emergency medicine, prefers to participate with his students rather than as the unseen wizard behind the curtain. “Some instructors like to be completely hidden and supply the voice of the patient mannequin. I prefer to interact directly with students, which enables me to teach on the fly. I use the simulations not as much as a critique session, but rather as an opportunity to ask students “what do you think about this,’ or ‘do you want to try this’?” Bair and his colleagues use simulation to teach procedures, including airway management and medical case management in clinical scenarios – for example, a team resuscitation for a patient in cardiac arrest. Bair, who is director of simulation training for the Department of Emergency Medicine, began using the technology in his teaching in 2001. “The breadth of opportunity and flexibility in the CVC is tremendous, with many options available. An interested faculty member doesn’t need to have familiarity with simulation to get involved,” he assured. The CVC facility includes a simulated catheterization laboratory where residents and other physicians can practice balloon angioplasty and other interventional vascular procedures. You can learn more about the Center for Virtual Care by writing to cvc@ ucdmc.ucdavis.edu or calling (916) 734-4708. Faculty Development Office 4610 X Street, Suite 4101 Sacramento, CA 95817 Published by the Faculty Development Office FEBRUARY – MARCH 2009 Workshops and other activities You are invited! We encourage you to enroll in one of the various workshops, programs and events sponsored by the Faculty Development Office. For more event details and to register, visit www.ucdmc.ucdavis. edu/facultydev/ and click Register Online. (Event co-sponsors are indicated within parentheses.) (Calendar from page 1) March facultyNewsletter Published by the Faculty Development Office, which administers and coordinates programs that respond to the professional and career development needs of UC Davis Health System faculty members. 4610 X Street, Suite 4101 Sacramento, CA 95817 (916) 734-2464 www.ucdmc.ucdavis.edu/facultydev/ Edward Callahan, Ph.D. Associate Dean for Academic Personnel Jesse Joad, M.D., M.S. Associate Dean for Diversity and Faculty Life Gregg Servis, M.Div. Director, Faculty Development gregg.servis@ucdmc.ucdavis.edu 4 Office of Diversity Advisory Team meeting 5 Workshop: Using EMR for Clinical Research February 11 Community Engagement and Partnerships Committee meeting 11 Faculty Development Advisory Team meeting 12 Breakfast with Leadership: James Goodnight, M.D., Ph.D. 4 Office of Diversity Advisory Team meeting 18 Workshop: Negotiation Skills 5 Breakfast with the Dean 19 Breakfast with Leadership: Michael Minear 24 Workshop: Compensation Plans: From ABC to XYZ 2 Work-Life Balance Group meeting 11 Community Engagement and Partnerships Committee meeting Launch of Faculty Forward – faculty satisfaction survey (see detailed information in the April-May edition of Faculty Newsletter) Office of Diversity Advisory Team meeting Cheryl Busman Program Representative, Faculty Development cheryl.busman@ucdmc.ucdavis.edu 2 Breakfast with the Dean 6 Workshop: Juggling Careers and Parenting Felicia Carrillo Program Assistant, Office of Diversity felicia.carrillo@ucdmc.ucdavis.edu 8 Community Engagement and Partnerships Committee meeting 26 Breakfast with Leadership: William McGowan 8 Faculty Development Advisory Team meeting March 17 Breakfast with Leadership: Ann Bonham, Ph.D. 28 Workshop: Using Web-Based Surveys for Research 5 facultyNewsletter | February – March 2009 | www.ucdmc.ucdavis.edu/facultydev commercially in the early 1990s, have progressed dramatically in sophistication. Patient simulation devices now can imitate human symptoms, respond to sensory stimuli, and replicate reactions to induced drugs. At UC Davis Health System, the Center for Virtual Care (CVC) has a complement of simulation devices on which students, residents and attending physicians can practice techniques without causing harm to patients. The facility also allows surgeons to gain experience in using surgical robots. Patient mannequins nicknamed “Stan” and “Morgan” simulate breathing, continued on page 5 20 Women in Medicine event: career advancement workshop 2 Work-Life Balance Work Group meeting 2 Dean’s Recognition Reception MARCH continues on page 6 facultyNewsletter | February – March 2009 | www.ucdmc.ucdavis.edu/facultydev For medical students learning how to perform procedures, the leap from working on cadavers to interacting with live patients is figuratively as broad as the Snake River Canyon that stunt rider Evel Knievel famously tried to leap while aboard a motorcycle. Today, though, UC Davis medical students have at their disposal a bridge to help them cross that chasm: medical mannequins that mimic characteristics of living patients. Simulation has been integrated for decades in aviation, military and astronaut training, and in automotive safety testing. Interactive medical simulator mannequins, introduced 12 Breakfast with Leadership: James Goodnight, M.D., Ph.D. 1 EditPros LLC Editorial Services www.editpros.com Mannequins in Center for Virtual Care simulate human subjects 11 Faculty Development Advisory Team meeting April MEDICAL TRAINING WITHOUT RISK 6 Medical students Diana Hanna, Jeanah Brader and Nicole Ling (L-R) listen as Richard Rivera, professor of anesthesiology and pain medicine, describes a procedure during a Jan. 7 training session with a medical mannequin at the Center for Virtual Care. (Photos: Emi Manning)