A MeASuRe of SAtISfActIon faculty Published by the Faculty Development Office

FACUltY contInued fRoM PAge 1 improvements to enhance faculty job satisfaction and retention. The survey also offers every faculty member the ability to contribute to a national dialogue of vital importance to the discipline of academic medicine,” Servis said.
Faculty satisfaction is the beating heart of the Faculty Forward program.
The program is given a sense of urgency by a nationally publicized study showing that 70 percent of physicians who vacate positions do so for reasons other than retirement, illness, death or termination. That disturbing 70 percent figure, determined by the Medical Group
Management Association and the healthcare executive placement firm Cejka
Search, largely reflects job dissatisfaction in one respect or another — unhappiness with compensation, work schedules, promotional opportunities or other factors.
Such departures take a heavy toll at teaching hospitals. Research has revealed that annual faculty turnover costs at academic medical centers can exceed
$3 million in recruitment, retraining and related expenses.
“We absolutely want and need our faculty members to be productive and happy in their careers, but we can’t work on that unless we know what they seek,”
Joad said. “We are counting on the results of the Faculty Forward survey to help us conceive and make changes to better support them.”
The AAMC-COACHE Medical
Faculty Job Satisfaction Survey questions encompass 13 topic domains: appointment and demographic information; nature of work; climate, culture and collegiality; collaboration; mentoring; feedback; promotion; pay and compensation; benefits and family policies; faculty recruitment and retention; institutional decision-making, governance and operations; clinical practice; and global satisfaction.
“Through participation in Faculty
Forward, medical schools can refine their understanding of what drives job satisfaction among their faculty, obtain valuable benchmarking data to peer institutions and to the national cohort, and strengthen institutional capacity to identify, implement and sustain efforts to improve faculty satisfaction,” explained
Euphia Smith, director of Faculty Forward at AAMC.
The 10-week survey period will begin on April 6, after AAMC and COACHE send instructional e-mail messages directly to
UC Davis faculty members. The survey, conducted through a secure Web portal, requires about 30 minutes to complete.
Edward Callahan acknowledges that faculty members’ time is precious, but urges all to participate.
“We can only get as much good out of this process as people are willing to put into it. If you take the time to share your heartfelt thoughts, we can all benefit. This survey will enable us to keep an ear close to the ground to help us shape the kind of work environment we collectively want,”
Callahan said.
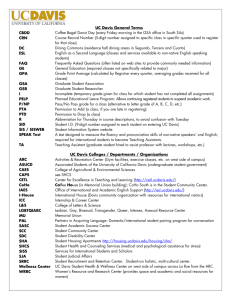
Edward Callahan, Jesse Joad and Gregg Servis
(L-R), who comprise the executive committee of the health system’s Faculty Forward task force, as they finalize survey planning documents.
(Photo: Trudi Banko )
William T. Mallon, AAMC’s director of organizational learning and research, affirmed that the privacy of respondents will be maintained in all published and written data resulting from the study.
“Faculty names and e-mail address are gathered and stored on a secure technology platform. Data will be reported only when responses can be aggregated in cells of five respondents or more, so that individual faculty cannot be identified,” Mallon said. Using an encrypted electronic identifier, AAMC will randomly select one UC Davis faculty survey participant to receive a
$2,000 certificate for personal faculty development.
Mallon strongly encourages broad participation.
“The survey was designed to generate a report of actionable diagnoses—not simply interesting data. The reports that institutions will receive will 1) provide institutional leaders with data to leverage workplace improvements; 2) help both prospective and current faculty ask better questions and make informed decisions about their workplace; and
3) generate ideas from faculty that enrich and expand the range of possible improvements to work environments,”
Mallon said.
Sarah Bunton, AAMC senior research analyst, said that the benchmarking reports will include a “dashboard report” presenting an overview of various dimensions of job satisfaction and dissatisfaction among faculty at the medical school.
“The report will include a comprehensive statistical report of the strengths and weaknesses of the institution’s faculty work environments as perceived by the faculty,” Bunton said.
“Data are presented by satisfaction levels, thematic clusters, appointment type, department and other variables. Finally, this report includes a comparison of the school’s results to peer institutions as well as to national data.”
During the second and third years,
AAMC will coordinate learning and idea-sharing opportunities through Web seminars, break-out sessions at national meetings, on-site visits and workshops.
Servis said that UC Davis survey results and comparative data will be disseminated to faculty members.
UC Davis Health system
Faculty Development Office
4610 X Street, Suite 4101
Sacramento, CA 95817 faculty
Newsletter
Published by the Faculty Development
Office , which administers and coordinates programs that respond to the professional and career development needs of UC Davis Health
System faculty members.
4610 X Street, Suite 4101
Sacramento, CA 95817
(916) 734-2464 www.ucdmc.ucdavis.edu/facultydev/
Edward Callahan, Ph.D.
Associate Dean for Academic Personnel
Jesse Joad, M.D., M.S.
Associate Dean for Diversity and Faculty Life
Gregg Servis, M.Div.
Director, Faculty Development gregg.servis@ucdmc.ucdavis.edu
Cheryl Busman
Program Representative, Faculty Development cheryl.busman@ucdmc.ucdavis.edu
Felicia Carrillo
Program Assistant, Office of Diversity felicia.carrillo@ucdmc.ucdavis.edu
EditPros LLC
Editorial Services www.editpros.com
(cALendAR fRoM PAge 1)
April
23 Workshop: Leading a Terrific Small-Group Discussion (OME)
27 Workshop: Improving Your Exams – Writing Vignette Questions (OME)
28 Workshop: Using Web-Based Surveys for Research
30 Workshop: Discussion in Large Groups – Using Team-Based Learning (OME)
13
13
14
19
May
4
6
8
Work-Life Balance Work Group meeting
Office of Diversity Advisory Team meeting
Workshop: Career Defining Moments – Expect the Unexpected (CTSC)
Community Partnerships Committee meeting
Faculty Development Advisory Team meeting
New Faculty Orientation
Safe Zone Training
20 Workshop: Crucial Conversations
June
1
24
Workshop: Juggling Careers and Parenting
Workshop: Time Management Skills (CTSC)
Event co-sponsors
CTSC: Clinical Translational Science Center
FDO: Faculty Development Office
OME: Office of Medical Education faculty Newsletter | April – May 2009 | www.ucdmc.ucdavis.edu/facultydev 5 faculty Newsletter | April – May 2009 | www.ucdmc.ucdavis.edu/facultydev 6 workshops and other activities
You are invited! We encourage you to enroll in one of the various workshops, programs and events sponsored by the Faculty
Development Office. For more event details and to register, visit www.ucdmc.ucdavis.
edu/facultydev/ and click Register Online .
(Event co-sponsors are indicated within parentheses.)
April
1 Office of Diversity Advisory Team meeting
2 Breakfast with the Dean
6 Launch of Faculty Forward faculty satisfaction survey (FDO)
6 Work-Life Balance Work Group meeting
8 Community Partnerships Committee meeting
8 Faculty Development Advisory Team meeting
14 Workshop: Using the Audience
Response System (OME)
17 Breakfast with Leadership: Ann
Bonham, Ph.D.
20 Workshop: Improving Your Exams
– Question Quality and Scoring (OME)
21 Workshop: How to Do Effective
Student-Centered Clinical Teaching
(OME)
APRIL contInueS on PAge 6
Published by the Faculty Development Office
APRIL – MAY 2009
A MeASuRe of SAtISfActIon
‘Faculty Forward’ survey seeks opinions from entire faculty
All UC Davis Health System faculty members who work half-time or more will soon receive an invitation to participate in a survey through which they may anonymously assess their work environment and job satisfaction, influence important evolutionary changes in the institution — and perhaps win a $2,000 voucher for professional development.
The health system has signed on as one of 25 “founding partner” medical schools participating in an inaugural nationwide project called Faculty
Forward: The Alliance for Advancing the Academic Medicine Workplace.
Administered by the Association of
American Medical Colleges (AAMC),
Faculty Forward will generate national benchmarking data to help participating institutions improve faculty satisfaction, retention and vitality.
AAMC developed the faculty satisfaction survey instrument and diagnostic benchmarking tool jointly with the Collaborative on
Academic Careers in Higher Education
(COACHE) at the Harvard Graduate
School of Education.
UC Davis and the Stanford
University School of Medicine are the only California medical institutions participating in the Faculty Forward program, the most ambitious opinion census ever conducted among academic medicine professionals. Dean Claire
Pomeroy championed UC Davis’ participation in Faculty Forward, which Gregg Servis, director of faculty development, and Cheryl Busman, program representative in the Faculty
Development Office, set into motion. A
15-member task force consisting of UC
Davis Health System administrators, senior and junior clinical and teaching faculty members, and academic staff
April 6 members has been convened to develop
UC Davis-specific questions and monitor the survey process. The task force operates under the direction of an executive committee composed of co-chairs Gregg Servis and Jesse Joad, associate dean for diversity and faculty life, and Edward Callahan, associate dean for academic personnel.
“We view Faculty Forward as a mechanism to guide UC Davis in creating overall and department-specific contInued on PAge 5
office visit williAM G. CUsHArD, M.D.
MARKS 40-YeAR VoLunteeR MILeStone
The names of many medical specialties are enigmatic to the lay public, and that’s a hindrance that has pervaded the 45-year medical career of William Green Cushard
Jr., M.D.
“Endocrinologists have an image problem. Most people don’t know what an endocrinologist is,” said
Cushard, who operates a practice called
Endocrine Associates on Scripps Drive in Sacramento. “I tell most patients that I am a doctor who treats diabetes, thyroid problems and hormone imbalances.”
In his practice, Cushard devotes considerable time to patient education.
“People tend to think of hormones only as sex hormones, so I explain that hormones are chemical signals sent through the bloodstream as a means by which one part of the body can control another part,” Cushard said.
Because education is so significant in Cushard’s practice, he naturally was attracted to a tangential role. He has served as a volunteer clinical professor of medicine in the UC Davis Division of
Endocrinology, Clinical Nutrition and
Vascular Medicine for nearly 40 years, predating the establishment of his own practice by two years.
Cushard accepted his volunteer clinical faculty appointment in September
1969, while in military service as a staff endocrinologist at the rank of captain, assigned to David Grant Medical Center at
Travis Air Force base.
“I was fresh out of residency training at the Hospital of the University of
Pennsylvania, and I wanted to continue my academic activities,” said Cushard, who obtained his M.D. degree from the
University of Maryland in 1964.
Cushard instructs UC Davis medical students in the endocrine portion of year one and internal medicine courses. He also has worked with medical residents, interns and fellows.
“My interaction with students does not project from a fixed, annually repeating, schedule. I am rather a utility man in the department responding to serve as needed,” Cushard explained. “This year,
I will be discussion leader in a workshop on polycystic ovary syndrome.” He often places his clinical discussions within a philosophical context. “While teaching students about the physiology and biochemistry underlying clinical problems,
I remind them to preserve the dignity of every patient by treating each with courtesy and respect.”
Cushard’s entry into the realm of medicine was in answer to a metaphysical calling.
“The moment of epiphany occurred when I was a college undergraduate. It was early March, still chilly, with clumps of snow yet lingering on the shady side of trees, yellow forsythia already in bloom, and big, white, puffy clouds drifting across the blue sky,” Cushard recalled.
“A presence came to me, unseen but ineluctable, bearing the information that
I was going to go to medical school and become a doctor. It was an order from
The General that I never questioned, in spite of my surprise. Within days I changed my major and signed up for premedical courses.”
Cushard said he has consistently derived benefits from his participation as a volunteer clinical faculty member.
“I have enjoyed the experiences, but beyond that, being challenged by younger people in training has forced me to produce the right answer. I discovered that kept me academically fresh. It still does,” Cushard said.
He has served on a California
Department of Motor Vehicles advisory panel on the safety of diabetic drivers who are susceptible to treatment-induced hypoglycemia. He also fulfilled two terms as an editorial reviewer for the journal
Endocrine Practice .
Cushard enjoys listening to music ranging in genre from bluegrass to grand opera, but is modest about his musical abilities; he admits to annoying his wife,
Jacquie, by “playing the classical guitar badly.” He also is an amateur radio operator with the call sign KC6TBF, and he and Jacquie are competitive runners and avid skiers.
“I have been married to the same woman for 39 1/2 years. We have four fine sons who are all college-educated, married, have jobs and their own homes, and yet we still do things together. I am the luckiest man in the world,” Cushard concluded.
faculty Newsletter | April – May 2009 | www.ucdmc.ucdavis.edu/facultydev 2 faculty rOUNDs
A weLcoMe to new fAcuLtY coLLeAgueS
Michelle A. James John P. Livoni
Each edition of the Faculty Newsletter introduces faculty colleagues who recently joined the UC Davis
Health System family. Watch for more new clinical and research staff members in the next issue.
Michelle James specializes in pediatric upper-limb surgery
Orthopaedic surgeon Michelle A.
James, M.D., a pediatric upper-limb specialist, devotes her clinical practice to treatment of congenital malformations, brachial plexus birth palsy and other neuromuscular conditions, and reconstruction of upper limbs of patients with spinal cord injuries.
James is a professor of clinical orthopaedic surgery at UC Davis and UC
San Francisco; chief of the UC Davis
Division of Pediatric Orthopaedics; and chief of orthopaedic surgery at
Shriners Hospital for Children Northern
California. She is board-certified in orthopaedic surgery, with a certificate of added qualification in hand surgery. She is deputy editor of the Journal of Hand
Surgery, and is researching hand function in children with congenital malformations and neuromuscular conditions.
John livoni is health system’s only radiology ‘B reader’
Diagnostic radiologist John P. Livoni,
M.D., M.P.H., who obtained his medical degree from UC Davis and was a faculty member here before entering private practice, has returned as a clinical professor in the Department of Radiology, where he has become assistant chair for clinical affairs.
The National Institute for Occupational
Safety and Health certified him as a “B
Reader,” qualifying him to interpret chest
X-rays for pneumoconioses and other occupational lung diseases. He is one of only two B Readers in the Sacramento area, and the only one in the UC Davis
Health System. B Reader certification requires testing every four years at the
Appalachian Laboratory for Occupational
Safety and Health in West Virginia.
Other new colleagues
• Julie Bossuyt, D.V.M., Ph.D., an assistant professor in residence in the Department of Pharmacology, is investigating the cellular and molecular mechanisms that govern cardiac function and how they become disordered in heart disease.
She is studying the role of protein kinase D signaling in the regulation of myocardial contraction, hypertrophy and cardiac remodeling.
• Denis M. Dwyre, M.D., an assistant professor of pathology and laboratory medicine, practices hematopathology, transfusion medicine and apheresis.
He is board-certified in clinical pathology and internal medicine, and subspecialty boarded in hematopathology and transfusion medicine. He is conducting clinical research in hematopathology and transfusion medicine.
• Interventional radiologist Craig
Glaiberman, M.D., an assistant professor of radiology, performs angiographies, arterial and venous interventions, biliary interventions, portal hypertension procedures, interventional oncology, dialysis interventions, embolization, drainages and central venous access procedures.
He is researching the use of medical simulation technology in training, and was included in the Best Doctors in
America list in 2007–08.
• Maha Najeeb Haddad, M.D., an assistant professor of pediatric nephrology, sees outpatients for conditions ranging from simple kidney disorders to illnesses requiring chronic dialysis or transplantation.
Board-certified in pediatrics and pediatric nephrology, she performs in-house consultations for patients, including those in pediatric intensive care who require acute dialysis.
She is shifting her focus to teaching and training medical students and residents.
• Pietro Invernizzi, M.D., Ph.D., an assistant adjunct professor in the
Division of Rheumatology, Allergy and Clinical Immunology, is studying the pathogenesis of primary biliary cirrhosis. He is concentrating on the role of genetic factors in development of the disease, and in understanding whether bile ducts play an active role or are innocent victims of the autoimmune aggression.
• Robert M. Tamurian, M.D., an assistant professor of orthopaedic surgery, is chief of orthopaedic oncology. Certified by the American
Board of Orthopaedic Surgery, he is a fellow of the American Academy of Orthopaedic Surgeons, and was named among America’s Top
Orthopaedic Surgeons in 2007 and
2008. His research encompasses clinical trials for optimal adjuvant therapy in soft-tissue sarcomas; radiation effects on soft-tissue healing; effects of radiation on bacterial shedding in mesenchymal tissue; and biomechanics of bone metastasis.
faculty Newsletter | April – May 2009 | www.ucdmc.ucdavis.edu/facultydev 3 view
POiNt
BY cLAIRe PoMeRoY, deAn whY YouR PARtIcIPAtIon In
‘fAcuLtY foRwARd’ IS IMPoRtAnt
Faculty satisfaction is crucial to creating the collaborative culture that has allowed us to thrive in recent years, helping us achieve a leadership role in academic medicine. But we know there are always opportunities to improve!
Therefore, I was pleased to announce during the State of the Health
System Address in January that we are participating in a faculty satisfaction initiative called Faculty Forward.
And now, our health system needs your input to continue moving this project forward.
All faculty members with 50 percent or greater appointments are being e-mailed a link to the online survey as part of a three-year study aimed at improving faculty satisfaction, retention and vitality.
UC Davis is proud to be one of the first 25 medical schools participating in this effort.
The survey instrument was developed by the AAMC and the Collaborative on
Academic Careers in Higher Education at the Harvard Graduate School of
Education. It will provide an objective and standardized method to measure satisfaction levels. Importantly, responses will be confidential, and the data collected will be aggregated and kept anonymous.
The results will allow us to understand what drives faculty satisfaction at our institution and benchmark that information with peer institutions. In addition, the results will guide training and learning opportunities that will make our health system an even more vibrant place for you to do your work.
Research and our own experiences emphasize how important it is to continually invest in faculty satisfaction.
According to the AAMC, medical schools lose half of their faculty to other institutions or to private settings within a decade. The cumulative effects of those departures are costly, with studies showing annual turnover costs exceeding $3 million per school. More importantly, turnover can have significant impacts on institutional performance, culture and morale.
Not only do we want to continue to retain and recruit dynamic faculty members, but we also want to make sure that each of you has the tools and resources you need to succeed.
To ensure that we realize those goals, a 15-member, health-system-wide task force will oversee this initiative and deliver recommendations based on the survey’s findings.
But again, we need your help. I encourage each of you to view the survey as a special opportunity to share your opinions and insights about how we can make our health system the best place for you to accomplish your important work in research, education, clinical care and community engagement.
Together, we can ensure that our health system remains a “destination of choice” for our world-class cadre of current – and future – faculty members.
advisory teams
Activities of the Faculty Development
Office are guided by the recommendations of two advisory teams:
Faculty Development
Advisory team
Gregg Servis, M.Div., Office of Faculty
Development and Diversity
Jesse Joad, M.D., M.S., Office of Faculty
Development and Diversity
Chuck Bevins, M.D., Ph.D., Medical
Microbiology and Immunology
Kathy DeRiemer, Ph.D., M.P.H., Public
Health Sciences
Tonya Fancher, M.D., M.P.H., Internal
Medicine
Jeff Gauvin, M.D., Surgery
Estella Geraghty, M.D., M.S., M.P.H.,
Internal Medicine
W. Ladson Hinton, M.D., Psychiatry and
Behavioral Sciences
Keith Lau, M.D., Pediatrics
Jamie Ross, M.D., Internal Medicine
Mark Sutter, M.D., Emergency Medicine
Vicki Wheelock, M.D., Neurology
Office of Diversity
Advisory team
Jesse Joad, M.D., M.S., Office of Faculty
Development and Diversity
Gregg Servis, M.Div., Office of Faculty
Development and Diversity
Elizabeth Abad, Alumni and Development
Officer, Health Sciences Advancement
Susan DeMarois, Government and
Community Relations
James Forkin, Postbaccalaureate Program
Coordinator, Office of Medical Education
Darin Latimore, M.D., Office of Faculty
Development and Diversity
Russell Lim, M.D., Psychiatry and
Behavioral Sciences
José Morfin, M.D., Internal Medicine
Marbella Sala, Executive Operations Manager,
Center for Reducing Health Disparities
Andreea Seritan, M.D., Psychiatry and
Behavioral Sciences
Pam Stotlar-McAuliffe, Manager,
Continuing Medical Education
Hendry Ton, M.D., Psychiatry
Michelle Villegas-Frazier, Team Lead,
Office of Diversity
Bold type indicates team coordinators faculty Newsletter | April – May 2009 | www.ucdmc.ucdavis.edu/facultydev 4
office visit williAM G. CUsHArD, M.D.
MARKS 40-YeAR VoLunteeR MILeStone
The names of many medical specialties are enigmatic to the lay public, and that’s a hindrance that has pervaded the 45-year medical career of William Green Cushard
Jr., M.D.
“Endocrinologists have an image problem. Most people don’t know what an endocrinologist is,” said
Cushard, who operates a practice called
Endocrine Associates on Scripps Drive in Sacramento. “I tell most patients that I am a doctor who treats diabetes, thyroid problems and hormone imbalances.”
In his practice, Cushard devotes considerable time to patient education.
“People tend to think of hormones only as sex hormones, so I explain that hormones are chemical signals sent through the bloodstream as a means by which one part of the body can control another part,” Cushard said.
Because education is so significant in Cushard’s practice, he naturally was attracted to a tangential role. He has served as a volunteer clinical professor of medicine in the UC Davis Division of
Endocrinology, Clinical Nutrition and
Vascular Medicine for nearly 40 years, predating the establishment of his own practice by two years.
Cushard accepted his volunteer clinical faculty appointment in September
1969, while in military service as a staff endocrinologist at the rank of captain, assigned to David Grant Medical Center at
Travis Air Force base.
“I was fresh out of residency training at the Hospital of the University of
Pennsylvania, and I wanted to continue my academic activities,” said Cushard, who obtained his M.D. degree from the
University of Maryland in 1964.
Cushard instructs UC Davis medical students in the endocrine portion of year one and internal medicine courses. He also has worked with medical residents, interns and fellows.
“My interaction with students does not project from a fixed, annually repeating, schedule. I am rather a utility man in the department responding to serve as needed,” Cushard explained. “This year,
I will be discussion leader in a workshop on polycystic ovary syndrome.” He often places his clinical discussions within a philosophical context. “While teaching students about the physiology and biochemistry underlying clinical problems,
I remind them to preserve the dignity of every patient by treating each with courtesy and respect.”
Cushard’s entry into the realm of medicine was in answer to a metaphysical calling.
“The moment of epiphany occurred when I was a college undergraduate. It was early March, still chilly, with clumps of snow yet lingering on the shady side of trees, yellow forsythia already in bloom, and big, white, puffy clouds drifting across the blue sky,” Cushard recalled.
“A presence came to me, unseen but ineluctable, bearing the information that
I was going to go to medical school and become a doctor. It was an order from
The General that I never questioned, in spite of my surprise. Within days I changed my major and signed up for premedical courses.”
Cushard said he has consistently derived benefits from his participation as a volunteer clinical faculty member.
“I have enjoyed the experiences, but beyond that, being challenged by younger people in training has forced me to produce the right answer. I discovered that kept me academically fresh. It still does,” Cushard said.
He has served on a California
Department of Motor Vehicles advisory panel on the safety of diabetic drivers who are susceptible to treatment-induced hypoglycemia. He also fulfilled two terms as an editorial reviewer for the journal
Endocrine Practice .
Cushard enjoys listening to music ranging in genre from bluegrass to grand opera, but is modest about his musical abilities; he admits to annoying his wife,
Jacquie, by “playing the classical guitar badly.” He also is an amateur radio operator with the call sign KC6TBF, and he and Jacquie are competitive runners and avid skiers.
“I have been married to the same woman for 39 1/2 years. We have four fine sons who are all college-educated, married, have jobs and their own homes, and yet we still do things together. I am the luckiest man in the world,” Cushard concluded.
faculty Newsletter | April – May 2009 | www.ucdmc.ucdavis.edu/facultydev 2 faculty rOUNDs
A weLcoMe to new fAcuLtY coLLeAgueS
Michelle A. James John P. Livoni
Each edition of the Faculty Newsletter introduces faculty colleagues who recently joined the UC Davis
Health System family. Watch for more new clinical and research staff members in the next issue.
Michelle James specializes in pediatric upper-limb surgery
Orthopaedic surgeon Michelle A.
James, M.D., a pediatric upper-limb specialist, devotes her clinical practice to treatment of congenital malformations, brachial plexus birth palsy and other neuromuscular conditions, and reconstruction of upper limbs of patients with spinal cord injuries.
James is a professor of clinical orthopaedic surgery at UC Davis and UC
San Francisco; chief of the UC Davis
Division of Pediatric Orthopaedics; and chief of orthopaedic surgery at
Shriners Hospital for Children Northern
California. She is board-certified in orthopaedic surgery, with a certificate of added qualification in hand surgery. She is deputy editor of the Journal of Hand
Surgery, and is researching hand function in children with congenital malformations and neuromuscular conditions.
John livoni is health system’s only radiology ‘B reader’
Diagnostic radiologist John P. Livoni,
M.D., M.P.H., who obtained his medical degree from UC Davis and was a faculty member here before entering private practice, has returned as a clinical professor in the Department of Radiology, where he has become assistant chair for clinical affairs.
The National Institute for Occupational
Safety and Health certified him as a “B
Reader,” qualifying him to interpret chest
X-rays for pneumoconioses and other occupational lung diseases. He is one of only two B Readers in the Sacramento area, and the only one in the UC Davis
Health System. B Reader certification requires testing every four years at the
Appalachian Laboratory for Occupational
Safety and Health in West Virginia.
Other new colleagues
• Julie Bossuyt, D.V.M., Ph.D., an assistant professor in residence in the Department of Pharmacology, is investigating the cellular and molecular mechanisms that govern cardiac function and how they become disordered in heart disease.
She is studying the role of protein kinase D signaling in the regulation of myocardial contraction, hypertrophy and cardiac remodeling.
• Denis M. Dwyre, M.D., an assistant professor of pathology and laboratory medicine, practices hematopathology, transfusion medicine and apheresis.
He is board-certified in clinical pathology and internal medicine, and subspecialty boarded in hematopathology and transfusion medicine. He is conducting clinical research in hematopathology and transfusion medicine.
• Interventional radiologist Craig
Glaiberman, M.D., an assistant professor of radiology, performs angiographies, arterial and venous interventions, biliary interventions, portal hypertension procedures, interventional oncology, dialysis interventions, embolization, drainages and central venous access procedures.
He is researching the use of medical simulation technology in training, and was included in the Best Doctors in
America list in 2007–08.
• Maha Najeeb Haddad, M.D., an assistant professor of pediatric nephrology, sees outpatients for conditions ranging from simple kidney disorders to illnesses requiring chronic dialysis or transplantation.
Board-certified in pediatrics and pediatric nephrology, she performs in-house consultations for patients, including those in pediatric intensive care who require acute dialysis.
She is shifting her focus to teaching and training medical students and residents.
• Pietro Invernizzi, M.D., Ph.D., an assistant adjunct professor in the
Division of Rheumatology, Allergy and Clinical Immunology, is studying the pathogenesis of primary biliary cirrhosis. He is concentrating on the role of genetic factors in development of the disease, and in understanding whether bile ducts play an active role or are innocent victims of the autoimmune aggression.
• Robert M. Tamurian, M.D., an assistant professor of orthopaedic surgery, is chief of orthopaedic oncology. Certified by the American
Board of Orthopaedic Surgery, he is a fellow of the American Academy of Orthopaedic Surgeons, and was named among America’s Top
Orthopaedic Surgeons in 2007 and
2008. His research encompasses clinical trials for optimal adjuvant therapy in soft-tissue sarcomas; radiation effects on soft-tissue healing; effects of radiation on bacterial shedding in mesenchymal tissue; and biomechanics of bone metastasis.
faculty Newsletter | April – May 2009 | www.ucdmc.ucdavis.edu/facultydev 3 view
POiNt
BY cLAIRe PoMeRoY, deAn whY YouR PARtIcIPAtIon In
‘fAcuLtY foRwARd’ IS IMPoRtAnt
Faculty satisfaction is crucial to creating the collaborative culture that has allowed us to thrive in recent years, helping us achieve a leadership role in academic medicine. But we know there are always opportunities to improve!
Therefore, I was pleased to announce during the State of the Health
System Address in January that we are participating in a faculty satisfaction initiative called Faculty Forward.
And now, our health system needs your input to continue moving this project forward.
All faculty members with 50 percent or greater appointments are being e-mailed a link to the online survey as part of a three-year study aimed at improving faculty satisfaction, retention and vitality.
UC Davis is proud to be one of the first 25 medical schools participating in this effort.
The survey instrument was developed by the AAMC and the Collaborative on
Academic Careers in Higher Education at the Harvard Graduate School of
Education. It will provide an objective and standardized method to measure satisfaction levels. Importantly, responses will be confidential, and the data collected will be aggregated and kept anonymous.
The results will allow us to understand what drives faculty satisfaction at our institution and benchmark that information with peer institutions. In addition, the results will guide training and learning opportunities that will make our health system an even more vibrant place for you to do your work.
Research and our own experiences emphasize how important it is to continually invest in faculty satisfaction.
According to the AAMC, medical schools lose half of their faculty to other institutions or to private settings within a decade. The cumulative effects of those departures are costly, with studies showing annual turnover costs exceeding $3 million per school. More importantly, turnover can have significant impacts on institutional performance, culture and morale.
Not only do we want to continue to retain and recruit dynamic faculty members, but we also want to make sure that each of you has the tools and resources you need to succeed.
To ensure that we realize those goals, a 15-member, health-system-wide task force will oversee this initiative and deliver recommendations based on the survey’s findings.
But again, we need your help. I encourage each of you to view the survey as a special opportunity to share your opinions and insights about how we can make our health system the best place for you to accomplish your important work in research, education, clinical care and community engagement.
Together, we can ensure that our health system remains a “destination of choice” for our world-class cadre of current – and future – faculty members.
advisory teams
Activities of the Faculty Development
Office are guided by the recommendations of two advisory teams:
Faculty Development
Advisory team
Gregg Servis, M.Div., Office of Faculty
Development and Diversity
Jesse Joad, M.D., M.S., Office of Faculty
Development and Diversity
Chuck Bevins, M.D., Ph.D., Medical
Microbiology and Immunology
Kathy DeRiemer, Ph.D., M.P.H., Public
Health Sciences
Tonya Fancher, M.D., M.P.H., Internal
Medicine
Jeff Gauvin, M.D., Surgery
Estella Geraghty, M.D., M.S., M.P.H.,
Internal Medicine
W. Ladson Hinton, M.D., Psychiatry and
Behavioral Sciences
Keith Lau, M.D., Pediatrics
Jamie Ross, M.D., Internal Medicine
Mark Sutter, M.D., Emergency Medicine
Vicki Wheelock, M.D., Neurology
Office of Diversity
Advisory team
Jesse Joad, M.D., M.S., Office of Faculty
Development and Diversity
Gregg Servis, M.Div., Office of Faculty
Development and Diversity
Elizabeth Abad, Alumni and Development
Officer, Health Sciences Advancement
Susan DeMarois, Government and
Community Relations
James Forkin, Postbaccalaureate Program
Coordinator, Office of Medical Education
Darin Latimore, M.D., Office of Faculty
Development and Diversity
Russell Lim, M.D., Psychiatry and
Behavioral Sciences
José Morfin, M.D., Internal Medicine
Marbella Sala, Executive Operations Manager,
Center for Reducing Health Disparities
Andreea Seritan, M.D., Psychiatry and
Behavioral Sciences
Pam Stotlar-McAuliffe, Manager,
Continuing Medical Education
Hendry Ton, M.D., Psychiatry
Michelle Villegas-Frazier, Team Lead,
Office of Diversity
Bold type indicates team coordinators faculty Newsletter | April – May 2009 | www.ucdmc.ucdavis.edu/facultydev 4
office visit williAM G. CUsHArD, M.D.
MARKS 40-YeAR VoLunteeR MILeStone
The names of many medical specialties are enigmatic to the lay public, and that’s a hindrance that has pervaded the 45-year medical career of William Green Cushard
Jr., M.D.
“Endocrinologists have an image problem. Most people don’t know what an endocrinologist is,” said
Cushard, who operates a practice called
Endocrine Associates on Scripps Drive in Sacramento. “I tell most patients that I am a doctor who treats diabetes, thyroid problems and hormone imbalances.”
In his practice, Cushard devotes considerable time to patient education.
“People tend to think of hormones only as sex hormones, so I explain that hormones are chemical signals sent through the bloodstream as a means by which one part of the body can control another part,” Cushard said.
Because education is so significant in Cushard’s practice, he naturally was attracted to a tangential role. He has served as a volunteer clinical professor of medicine in the UC Davis Division of
Endocrinology, Clinical Nutrition and
Vascular Medicine for nearly 40 years, predating the establishment of his own practice by two years.
Cushard accepted his volunteer clinical faculty appointment in September
1969, while in military service as a staff endocrinologist at the rank of captain, assigned to David Grant Medical Center at
Travis Air Force base.
“I was fresh out of residency training at the Hospital of the University of
Pennsylvania, and I wanted to continue my academic activities,” said Cushard, who obtained his M.D. degree from the
University of Maryland in 1964.
Cushard instructs UC Davis medical students in the endocrine portion of year one and internal medicine courses. He also has worked with medical residents, interns and fellows.
“My interaction with students does not project from a fixed, annually repeating, schedule. I am rather a utility man in the department responding to serve as needed,” Cushard explained. “This year,
I will be discussion leader in a workshop on polycystic ovary syndrome.” He often places his clinical discussions within a philosophical context. “While teaching students about the physiology and biochemistry underlying clinical problems,
I remind them to preserve the dignity of every patient by treating each with courtesy and respect.”
Cushard’s entry into the realm of medicine was in answer to a metaphysical calling.
“The moment of epiphany occurred when I was a college undergraduate. It was early March, still chilly, with clumps of snow yet lingering on the shady side of trees, yellow forsythia already in bloom, and big, white, puffy clouds drifting across the blue sky,” Cushard recalled.
“A presence came to me, unseen but ineluctable, bearing the information that
I was going to go to medical school and become a doctor. It was an order from
The General that I never questioned, in spite of my surprise. Within days I changed my major and signed up for premedical courses.”
Cushard said he has consistently derived benefits from his participation as a volunteer clinical faculty member.
“I have enjoyed the experiences, but beyond that, being challenged by younger people in training has forced me to produce the right answer. I discovered that kept me academically fresh. It still does,” Cushard said.
He has served on a California
Department of Motor Vehicles advisory panel on the safety of diabetic drivers who are susceptible to treatment-induced hypoglycemia. He also fulfilled two terms as an editorial reviewer for the journal
Endocrine Practice .
Cushard enjoys listening to music ranging in genre from bluegrass to grand opera, but is modest about his musical abilities; he admits to annoying his wife,
Jacquie, by “playing the classical guitar badly.” He also is an amateur radio operator with the call sign KC6TBF, and he and Jacquie are competitive runners and avid skiers.
“I have been married to the same woman for 39 1/2 years. We have four fine sons who are all college-educated, married, have jobs and their own homes, and yet we still do things together. I am the luckiest man in the world,” Cushard concluded.
faculty Newsletter | April – May 2009 | www.ucdmc.ucdavis.edu/facultydev 2 faculty rOUNDs
A weLcoMe to new fAcuLtY coLLeAgueS
Michelle A. James John P. Livoni
Each edition of the Faculty Newsletter introduces faculty colleagues who recently joined the UC Davis
Health System family. Watch for more new clinical and research staff members in the next issue.
Michelle James specializes in pediatric upper-limb surgery
Orthopaedic surgeon Michelle A.
James, M.D., a pediatric upper-limb specialist, devotes her clinical practice to treatment of congenital malformations, brachial plexus birth palsy and other neuromuscular conditions, and reconstruction of upper limbs of patients with spinal cord injuries.
James is a professor of clinical orthopaedic surgery at UC Davis and UC
San Francisco; chief of the UC Davis
Division of Pediatric Orthopaedics; and chief of orthopaedic surgery at
Shriners Hospital for Children Northern
California. She is board-certified in orthopaedic surgery, with a certificate of added qualification in hand surgery. She is deputy editor of the Journal of Hand
Surgery, and is researching hand function in children with congenital malformations and neuromuscular conditions.
John livoni is health system’s only radiology ‘B reader’
Diagnostic radiologist John P. Livoni,
M.D., M.P.H., who obtained his medical degree from UC Davis and was a faculty member here before entering private practice, has returned as a clinical professor in the Department of Radiology, where he has become assistant chair for clinical affairs.
The National Institute for Occupational
Safety and Health certified him as a “B
Reader,” qualifying him to interpret chest
X-rays for pneumoconioses and other occupational lung diseases. He is one of only two B Readers in the Sacramento area, and the only one in the UC Davis
Health System. B Reader certification requires testing every four years at the
Appalachian Laboratory for Occupational
Safety and Health in West Virginia.
Other new colleagues
• Julie Bossuyt, D.V.M., Ph.D., an assistant professor in residence in the Department of Pharmacology, is investigating the cellular and molecular mechanisms that govern cardiac function and how they become disordered in heart disease.
She is studying the role of protein kinase D signaling in the regulation of myocardial contraction, hypertrophy and cardiac remodeling.
• Denis M. Dwyre, M.D., an assistant professor of pathology and laboratory medicine, practices hematopathology, transfusion medicine and apheresis.
He is board-certified in clinical pathology and internal medicine, and subspecialty boarded in hematopathology and transfusion medicine. He is conducting clinical research in hematopathology and transfusion medicine.
• Interventional radiologist Craig
Glaiberman, M.D., an assistant professor of radiology, performs angiographies, arterial and venous interventions, biliary interventions, portal hypertension procedures, interventional oncology, dialysis interventions, embolization, drainages and central venous access procedures.
He is researching the use of medical simulation technology in training, and was included in the Best Doctors in
America list in 2007–08.
• Maha Najeeb Haddad, M.D., an assistant professor of pediatric nephrology, sees outpatients for conditions ranging from simple kidney disorders to illnesses requiring chronic dialysis or transplantation.
Board-certified in pediatrics and pediatric nephrology, she performs in-house consultations for patients, including those in pediatric intensive care who require acute dialysis.
She is shifting her focus to teaching and training medical students and residents.
• Pietro Invernizzi, M.D., Ph.D., an assistant adjunct professor in the
Division of Rheumatology, Allergy and Clinical Immunology, is studying the pathogenesis of primary biliary cirrhosis. He is concentrating on the role of genetic factors in development of the disease, and in understanding whether bile ducts play an active role or are innocent victims of the autoimmune aggression.
• Robert M. Tamurian, M.D., an assistant professor of orthopaedic surgery, is chief of orthopaedic oncology. Certified by the American
Board of Orthopaedic Surgery, he is a fellow of the American Academy of Orthopaedic Surgeons, and was named among America’s Top
Orthopaedic Surgeons in 2007 and
2008. His research encompasses clinical trials for optimal adjuvant therapy in soft-tissue sarcomas; radiation effects on soft-tissue healing; effects of radiation on bacterial shedding in mesenchymal tissue; and biomechanics of bone metastasis.
faculty Newsletter | April – May 2009 | www.ucdmc.ucdavis.edu/facultydev 3 view
POiNt
BY cLAIRe PoMeRoY, deAn whY YouR PARtIcIPAtIon In
‘fAcuLtY foRwARd’ IS IMPoRtAnt
Faculty satisfaction is crucial to creating the collaborative culture that has allowed us to thrive in recent years, helping us achieve a leadership role in academic medicine. But we know there are always opportunities to improve!
Therefore, I was pleased to announce during the State of the Health
System Address in January that we are participating in a faculty satisfaction initiative called Faculty Forward.
And now, our health system needs your input to continue moving this project forward.
All faculty members with 50 percent or greater appointments are being e-mailed a link to the online survey as part of a three-year study aimed at improving faculty satisfaction, retention and vitality.
UC Davis is proud to be one of the first 25 medical schools participating in this effort.
The survey instrument was developed by the AAMC and the Collaborative on
Academic Careers in Higher Education at the Harvard Graduate School of
Education. It will provide an objective and standardized method to measure satisfaction levels. Importantly, responses will be confidential, and the data collected will be aggregated and kept anonymous.
The results will allow us to understand what drives faculty satisfaction at our institution and benchmark that information with peer institutions. In addition, the results will guide training and learning opportunities that will make our health system an even more vibrant place for you to do your work.
Research and our own experiences emphasize how important it is to continually invest in faculty satisfaction.
According to the AAMC, medical schools lose half of their faculty to other institutions or to private settings within a decade. The cumulative effects of those departures are costly, with studies showing annual turnover costs exceeding $3 million per school. More importantly, turnover can have significant impacts on institutional performance, culture and morale.
Not only do we want to continue to retain and recruit dynamic faculty members, but we also want to make sure that each of you has the tools and resources you need to succeed.
To ensure that we realize those goals, a 15-member, health-system-wide task force will oversee this initiative and deliver recommendations based on the survey’s findings.
But again, we need your help. I encourage each of you to view the survey as a special opportunity to share your opinions and insights about how we can make our health system the best place for you to accomplish your important work in research, education, clinical care and community engagement.
Together, we can ensure that our health system remains a “destination of choice” for our world-class cadre of current – and future – faculty members.
advisory teams
Activities of the Faculty Development
Office are guided by the recommendations of two advisory teams:
Faculty Development
Advisory team
Gregg Servis, M.Div., Office of Faculty
Development and Diversity
Jesse Joad, M.D., M.S., Office of Faculty
Development and Diversity
Chuck Bevins, M.D., Ph.D., Medical
Microbiology and Immunology
Kathy DeRiemer, Ph.D., M.P.H., Public
Health Sciences
Tonya Fancher, M.D., M.P.H., Internal
Medicine
Jeff Gauvin, M.D., Surgery
Estella Geraghty, M.D., M.S., M.P.H.,
Internal Medicine
W. Ladson Hinton, M.D., Psychiatry and
Behavioral Sciences
Keith Lau, M.D., Pediatrics
Jamie Ross, M.D., Internal Medicine
Mark Sutter, M.D., Emergency Medicine
Vicki Wheelock, M.D., Neurology
Office of Diversity
Advisory team
Jesse Joad, M.D., M.S., Office of Faculty
Development and Diversity
Gregg Servis, M.Div., Office of Faculty
Development and Diversity
Elizabeth Abad, Alumni and Development
Officer, Health Sciences Advancement
Susan DeMarois, Government and
Community Relations
James Forkin, Postbaccalaureate Program
Coordinator, Office of Medical Education
Darin Latimore, M.D., Office of Faculty
Development and Diversity
Russell Lim, M.D., Psychiatry and
Behavioral Sciences
José Morfin, M.D., Internal Medicine
Marbella Sala, Executive Operations Manager,
Center for Reducing Health Disparities
Andreea Seritan, M.D., Psychiatry and
Behavioral Sciences
Pam Stotlar-McAuliffe, Manager,
Continuing Medical Education
Hendry Ton, M.D., Psychiatry
Michelle Villegas-Frazier, Team Lead,
Office of Diversity
Bold type indicates team coordinators faculty Newsletter | April – May 2009 | www.ucdmc.ucdavis.edu/facultydev 4
FACUltY contInued fRoM PAge 1 improvements to enhance faculty job satisfaction and retention. The survey also offers every faculty member the ability to contribute to a national dialogue of vital importance to the discipline of academic medicine,” Servis said.
Faculty satisfaction is the beating heart of the Faculty Forward program.
The program is given a sense of urgency by a nationally publicized study showing that 70 percent of physicians who vacate positions do so for reasons other than retirement, illness, death or termination. That disturbing 70 percent figure, determined by the Medical Group
Management Association and the healthcare executive placement firm Cejka
Search, largely reflects job dissatisfaction in one respect or another — unhappiness with compensation, work schedules, promotional opportunities or other factors.
Such departures take a heavy toll at teaching hospitals. Research has revealed that annual faculty turnover costs at academic medical centers can exceed
$3 million in recruitment, retraining and related expenses.
“We absolutely want and need our faculty members to be productive and happy in their careers, but we can’t work on that unless we know what they seek,”
Joad said. “We are counting on the results of the Faculty Forward survey to help us conceive and make changes to better support them.”
The AAMC-COACHE Medical
Faculty Job Satisfaction Survey questions encompass 13 topic domains: appointment and demographic information; nature of work; climate, culture and collegiality; collaboration; mentoring; feedback; promotion; pay and compensation; benefits and family policies; faculty recruitment and retention; institutional decision-making, governance and operations; clinical practice; and global satisfaction.
“Through participation in Faculty
Forward, medical schools can refine their understanding of what drives job satisfaction among their faculty, obtain valuable benchmarking data to peer institutions and to the national cohort, and strengthen institutional capacity to identify, implement and sustain efforts to improve faculty satisfaction,” explained
Euphia Smith, director of Faculty Forward at AAMC.
The 10-week survey period will begin on April 6, after AAMC and COACHE send instructional e-mail messages directly to
UC Davis faculty members. The survey, conducted through a secure Web portal, requires about 30 minutes to complete.
Edward Callahan acknowledges that faculty members’ time is precious, but urges all to participate.
“We can only get as much good out of this process as people are willing to put into it. If you take the time to share your heartfelt thoughts, we can all benefit. This survey will enable us to keep an ear close to the ground to help us shape the kind of work environment we collectively want,”
Callahan said.
Edward Callahan, Jesse Joad and Gregg Servis
(L-R), who comprise the executive committee of the health system’s Faculty Forward task force, as they finalize survey planning documents.
(Photo: Trudi Banko )
William T. Mallon, AAMC’s director of organizational learning and research, affirmed that the privacy of respondents will be maintained in all published and written data resulting from the study.
“Faculty names and e-mail address are gathered and stored on a secure technology platform. Data will be reported only when responses can be aggregated in cells of five respondents or more, so that individual faculty cannot be identified,” Mallon said. Using an encrypted electronic identifier, AAMC will randomly select one UC Davis faculty survey participant to receive a
$2,000 certificate for personal faculty development.
Mallon strongly encourages broad participation.
“The survey was designed to generate a report of actionable diagnoses—not simply interesting data. The reports that institutions will receive will 1) provide institutional leaders with data to leverage workplace improvements; 2) help both prospective and current faculty ask better questions and make informed decisions about their workplace; and
3) generate ideas from faculty that enrich and expand the range of possible improvements to work environments,”
Mallon said.
Sarah Bunton, AAMC senior research analyst, said that the benchmarking reports will include a “dashboard report” presenting an overview of various dimensions of job satisfaction and dissatisfaction among faculty at the medical school.
“The report will include a comprehensive statistical report of the strengths and weaknesses of the institution’s faculty work environments as perceived by the faculty,” Bunton said.
“Data are presented by satisfaction levels, thematic clusters, appointment type, department and other variables. Finally, this report includes a comparison of the school’s results to peer institutions as well as to national data.”
During the second and third years,
AAMC will coordinate learning and idea-sharing opportunities through Web seminars, break-out sessions at national meetings, on-site visits and workshops.
Servis said that UC Davis survey results and comparative data will be disseminated to faculty members.
UC Davis Health system
Faculty Development Office
4610 X Street, Suite 4101
Sacramento, CA 95817 faculty
Newsletter
Published by the Faculty Development
Office , which administers and coordinates programs that respond to the professional and career development needs of UC Davis Health
System faculty members.
4610 X Street, Suite 4101
Sacramento, CA 95817
(916) 734-2464 www.ucdmc.ucdavis.edu/facultydev/
Edward Callahan, Ph.D.
Associate Dean for Academic Personnel
Jesse Joad, M.D., M.S.
Associate Dean for Diversity and Faculty Life
Gregg Servis, M.Div.
Director, Faculty Development gregg.servis@ucdmc.ucdavis.edu
Cheryl Busman
Program Representative, Faculty Development cheryl.busman@ucdmc.ucdavis.edu
Felicia Carrillo
Program Assistant, Office of Diversity felicia.carrillo@ucdmc.ucdavis.edu
EditPros LLC
Editorial Services www.editpros.com
(cALendAR fRoM PAge 1)
April
23 Workshop: Leading a Terrific Small-Group Discussion (OME)
27 Workshop: Improving Your Exams – Writing Vignette Questions (OME)
28 Workshop: Using Web-Based Surveys for Research
30 Workshop: Discussion in Large Groups – Using Team-Based Learning (OME)
13
13
14
19
May
4
6
8
Work-Life Balance Work Group meeting
Office of Diversity Advisory Team meeting
Workshop: Career Defining Moments – Expect the Unexpected (CTSC)
Community Partnerships Committee meeting
Faculty Development Advisory Team meeting
New Faculty Orientation
Safe Zone Training
20 Workshop: Crucial Conversations
June
1
24
Workshop: Juggling Careers and Parenting
Workshop: Time Management Skills (CTSC)
Event co-sponsors
CTSC: Clinical Translational Science Center
FDO: Faculty Development Office
OME: Office of Medical Education faculty Newsletter | April – May 2009 | www.ucdmc.ucdavis.edu/facultydev 5 faculty Newsletter | April – May 2009 | www.ucdmc.ucdavis.edu/facultydev 6 workshops and other activities
You are invited! We encourage you to enroll in one of the various workshops, programs and events sponsored by the Faculty
Development Office. For more event details and to register, visit www.ucdmc.ucdavis.
edu/facultydev/ and click Register Online .
(Event co-sponsors are indicated within parentheses.)
April
1 Office of Diversity Advisory Team meeting
2 Breakfast with the Dean
6 Launch of Faculty Forward faculty satisfaction survey (FDO)
6 Work-Life Balance Work Group meeting
8 Community Partnerships Committee meeting
8 Faculty Development Advisory Team meeting
14 Workshop: Using the Audience
Response System (OME)
17 Breakfast with Leadership: Ann
Bonham, Ph.D.
20 Workshop: Improving Your Exams
– Question Quality and Scoring (OME)
21 Workshop: How to Do Effective
Student-Centered Clinical Teaching
(OME)
APRIL contInueS on PAge 6
Published by the Faculty Development Office
APRIL – MAY 2009
A MeASuRe of SAtISfActIon
‘Faculty Forward’ survey seeks opinions from entire faculty
All UC Davis Health System faculty members who work half-time or more will soon receive an invitation to participate in a survey through which they may anonymously assess their work environment and job satisfaction, influence important evolutionary changes in the institution — and perhaps win a $2,000 voucher for professional development.
The health system has signed on as one of 25 “founding partner” medical schools participating in an inaugural nationwide project called Faculty
Forward: The Alliance for Advancing the Academic Medicine Workplace.
Administered by the Association of
American Medical Colleges (AAMC),
Faculty Forward will generate national benchmarking data to help participating institutions improve faculty satisfaction, retention and vitality.
AAMC developed the faculty satisfaction survey instrument and diagnostic benchmarking tool jointly with the Collaborative on
Academic Careers in Higher Education
(COACHE) at the Harvard Graduate
School of Education.
UC Davis and the Stanford
University School of Medicine are the only California medical institutions participating in the Faculty Forward program, the most ambitious opinion census ever conducted among academic medicine professionals. Dean Claire
Pomeroy championed UC Davis’ participation in Faculty Forward, which Gregg Servis, director of faculty development, and Cheryl Busman, program representative in the Faculty
Development Office, set into motion. A
15-member task force consisting of UC
Davis Health System administrators, senior and junior clinical and teaching faculty members, and academic staff
April 6 members has been convened to develop
UC Davis-specific questions and monitor the survey process. The task force operates under the direction of an executive committee composed of co-chairs Gregg Servis and Jesse Joad, associate dean for diversity and faculty life, and Edward Callahan, associate dean for academic personnel.
“We view Faculty Forward as a mechanism to guide UC Davis in creating overall and department-specific contInued on PAge 5
FACUltY contInued fRoM PAge 1 improvements to enhance faculty job satisfaction and retention. The survey also offers every faculty member the ability to contribute to a national dialogue of vital importance to the discipline of academic medicine,” Servis said.
Faculty satisfaction is the beating heart of the Faculty Forward program.
The program is given a sense of urgency by a nationally publicized study showing that 70 percent of physicians who vacate positions do so for reasons other than retirement, illness, death or termination. That disturbing 70 percent figure, determined by the Medical Group
Management Association and the healthcare executive placement firm Cejka
Search, largely reflects job dissatisfaction in one respect or another — unhappiness with compensation, work schedules, promotional opportunities or other factors.
Such departures take a heavy toll at teaching hospitals. Research has revealed that annual faculty turnover costs at academic medical centers can exceed
$3 million in recruitment, retraining and related expenses.
“We absolutely want and need our faculty members to be productive and happy in their careers, but we can’t work on that unless we know what they seek,”
Joad said. “We are counting on the results of the Faculty Forward survey to help us conceive and make changes to better support them.”
The AAMC-COACHE Medical
Faculty Job Satisfaction Survey questions encompass 13 topic domains: appointment and demographic information; nature of work; climate, culture and collegiality; collaboration; mentoring; feedback; promotion; pay and compensation; benefits and family policies; faculty recruitment and retention; institutional decision-making, governance and operations; clinical practice; and global satisfaction.
“Through participation in Faculty
Forward, medical schools can refine their understanding of what drives job satisfaction among their faculty, obtain valuable benchmarking data to peer institutions and to the national cohort, and strengthen institutional capacity to identify, implement and sustain efforts to improve faculty satisfaction,” explained
Euphia Smith, director of Faculty Forward at AAMC.
The 10-week survey period will begin on April 6, after AAMC and COACHE send instructional e-mail messages directly to
UC Davis faculty members. The survey, conducted through a secure Web portal, requires about 30 minutes to complete.
Edward Callahan acknowledges that faculty members’ time is precious, but urges all to participate.
“We can only get as much good out of this process as people are willing to put into it. If you take the time to share your heartfelt thoughts, we can all benefit. This survey will enable us to keep an ear close to the ground to help us shape the kind of work environment we collectively want,”
Callahan said.
Edward Callahan, Jesse Joad and Gregg Servis
(L-R), who comprise the executive committee of the health system’s Faculty Forward task force, as they finalize survey planning documents.
(Photo: Trudi Banko )
William T. Mallon, AAMC’s director of organizational learning and research, affirmed that the privacy of respondents will be maintained in all published and written data resulting from the study.
“Faculty names and e-mail address are gathered and stored on a secure technology platform. Data will be reported only when responses can be aggregated in cells of five respondents or more, so that individual faculty cannot be identified,” Mallon said. Using an encrypted electronic identifier, AAMC will randomly select one UC Davis faculty survey participant to receive a
$2,000 certificate for personal faculty development.
Mallon strongly encourages broad participation.
“The survey was designed to generate a report of actionable diagnoses—not simply interesting data. The reports that institutions will receive will 1) provide institutional leaders with data to leverage workplace improvements; 2) help both prospective and current faculty ask better questions and make informed decisions about their workplace; and
3) generate ideas from faculty that enrich and expand the range of possible improvements to work environments,”
Mallon said.
Sarah Bunton, AAMC senior research analyst, said that the benchmarking reports will include a “dashboard report” presenting an overview of various dimensions of job satisfaction and dissatisfaction among faculty at the medical school.
“The report will include a comprehensive statistical report of the strengths and weaknesses of the institution’s faculty work environments as perceived by the faculty,” Bunton said.
“Data are presented by satisfaction levels, thematic clusters, appointment type, department and other variables. Finally, this report includes a comparison of the school’s results to peer institutions as well as to national data.”
During the second and third years,
AAMC will coordinate learning and idea-sharing opportunities through Web seminars, break-out sessions at national meetings, on-site visits and workshops.
Servis said that UC Davis survey results and comparative data will be disseminated to faculty members.
UC Davis Health system
Faculty Development Office
4610 X Street, Suite 4101
Sacramento, CA 95817 faculty
Newsletter
Published by the Faculty Development
Office , which administers and coordinates programs that respond to the professional and career development needs of UC Davis Health
System faculty members.
4610 X Street, Suite 4101
Sacramento, CA 95817
(916) 734-2464 www.ucdmc.ucdavis.edu/facultydev/
Edward Callahan, Ph.D.
Associate Dean for Academic Personnel
Jesse Joad, M.D., M.S.
Associate Dean for Diversity and Faculty Life
Gregg Servis, M.Div.
Director, Faculty Development gregg.servis@ucdmc.ucdavis.edu
Cheryl Busman
Program Representative, Faculty Development cheryl.busman@ucdmc.ucdavis.edu
Felicia Carrillo
Program Assistant, Office of Diversity felicia.carrillo@ucdmc.ucdavis.edu
EditPros LLC
Editorial Services www.editpros.com
(cALendAR fRoM PAge 1)
April
23 Workshop: Leading a Terrific Small-Group Discussion (OME)
27 Workshop: Improving Your Exams – Writing Vignette Questions (OME)
28 Workshop: Using Web-Based Surveys for Research
30 Workshop: Discussion in Large Groups – Using Team-Based Learning (OME)
13
13
14
19
May
4
6
8
Work-Life Balance Work Group meeting
Office of Diversity Advisory Team meeting
Workshop: Career Defining Moments – Expect the Unexpected (CTSC)
Community Partnerships Committee meeting
Faculty Development Advisory Team meeting
New Faculty Orientation
Safe Zone Training
20 Workshop: Crucial Conversations
June
1
24
Workshop: Juggling Careers and Parenting
Workshop: Time Management Skills (CTSC)
Event co-sponsors
CTSC: Clinical Translational Science Center
FDO: Faculty Development Office
OME: Office of Medical Education faculty Newsletter | April – May 2009 | www.ucdmc.ucdavis.edu/facultydev 5 faculty Newsletter | April – May 2009 | www.ucdmc.ucdavis.edu/facultydev 6 workshops and other activities
You are invited! We encourage you to enroll in one of the various workshops, programs and events sponsored by the Faculty
Development Office. For more event details and to register, visit www.ucdmc.ucdavis.
edu/facultydev/ and click Register Online .
(Event co-sponsors are indicated within parentheses.)
April
1 Office of Diversity Advisory Team meeting
2 Breakfast with the Dean
6 Launch of Faculty Forward faculty satisfaction survey (FDO)
6 Work-Life Balance Work Group meeting
8 Community Partnerships Committee meeting
8 Faculty Development Advisory Team meeting
14 Workshop: Using the Audience
Response System (OME)
17 Breakfast with Leadership: Ann
Bonham, Ph.D.
20 Workshop: Improving Your Exams
– Question Quality and Scoring (OME)
21 Workshop: How to Do Effective
Student-Centered Clinical Teaching
(OME)
APRIL contInueS on PAge 6
Published by the Faculty Development Office
APRIL – MAY 2009
A MeASuRe of SAtISfActIon
‘Faculty Forward’ survey seeks opinions from entire faculty
All UC Davis Health System faculty members who work half-time or more will soon receive an invitation to participate in a survey through which they may anonymously assess their work environment and job satisfaction, influence important evolutionary changes in the institution — and perhaps win a $2,000 voucher for professional development.
The health system has signed on as one of 25 “founding partner” medical schools participating in an inaugural nationwide project called Faculty
Forward: The Alliance for Advancing the Academic Medicine Workplace.
Administered by the Association of
American Medical Colleges (AAMC),
Faculty Forward will generate national benchmarking data to help participating institutions improve faculty satisfaction, retention and vitality.
AAMC developed the faculty satisfaction survey instrument and diagnostic benchmarking tool jointly with the Collaborative on
Academic Careers in Higher Education
(COACHE) at the Harvard Graduate
School of Education.
UC Davis and the Stanford
University School of Medicine are the only California medical institutions participating in the Faculty Forward program, the most ambitious opinion census ever conducted among academic medicine professionals. Dean Claire
Pomeroy championed UC Davis’ participation in Faculty Forward, which Gregg Servis, director of faculty development, and Cheryl Busman, program representative in the Faculty
Development Office, set into motion. A
15-member task force consisting of UC
Davis Health System administrators, senior and junior clinical and teaching faculty members, and academic staff
April 6 members has been convened to develop
UC Davis-specific questions and monitor the survey process. The task force operates under the direction of an executive committee composed of co-chairs Gregg Servis and Jesse Joad, associate dean for diversity and faculty life, and Edward Callahan, associate dean for academic personnel.
“We view Faculty Forward as a mechanism to guide UC Davis in creating overall and department-specific contInued on PAge 5