The Rise of the Family Doctor
advertisement

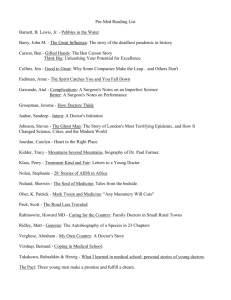
From Cradle to Grave: Term 2, Lecture 1 The Rise of the Family Doctor Lecture themes and outline THEMES/QUESTIONS • The consolidation of a medical profession? • The rise of the family doctor? OUTLINE • Definitions/criteria of ‘profession’ • Changes in medical practice in the C19th - Medical education - Licensing of practitioners • Reform of medical practice - 1815 Apothecaries Act - 1858 Medical Act • The medical profession in the late C19th - GPs, public offices, consultants - Problems for the profession: overstocking, competition, public image • The emergence of a family doctor? Professionalisation - definition from S.E. Shortt (1983)* ‘A process by which a heterogenous collection of individuals is gradually recognised, by both themselves and other members of society, as constituting a relatively homogenous and distinct occupational group’. *‘Physicians, science, and status: issues in the professionalization of Anglo American medicine in the nineteenth century’, Medical history, Vol. 27, No. 1. (Jan. 1983), pp. 51-68. A medical profession: relevant criteria 1. The possession of a body of highly specialized knowledge: we expect doctors to have a deep knowledge, acquired through long training in medical school. A doctor’s qualifications prove that he or she has completed this training to the standards required of the profession. 2. Professional unity and a strong ethos of public service: we do not expect doctors to compete with one another for patients by advertising their services or by offering cutprice practice. We do expect practitioners to co-operate when caring for patients, and to always work for the patients’ best interests. 3. A monopoly of practice: only members of the medical profession can call themselves doctors. We distinguish between orthodox medical practitioners and those who offer alternative forms of medical treatment by calling them practitioners of ‘complementary’ or ‘alternative’ medicine. 4. Professional autonomy: medical practice is based on highly specialist knowledge, which is not shared with the general public. Therefore, only doctors can judge whether other doctors are trained to a suitable standard and are competent to practice. 5. High social status: doctors earn high salaries and also enjoy a special social respect. Situation in early 19th century 1. No collective power: divisions between physicians, surgeons and apothecaries (tripartite structure) 2. Variety of routes to a medical licence – licensing bodies corrupt and irrelevant 3. Beginning of new division within the medical profession – general practitioners and consultants 4. Competitive medical marketplace 5. Public perceptions varied – doctors depicted as money grubbing or unskilled Argued modern medical profession emerged c.1840-1880 John Hunter (1728 -1793) Quack doctor open for business. Coloured etching by G.M. Woodward, 1802 Medical Reform (1) 1815 Apothecaries Act • License of the Society of Apothecaries (LSA) needed to practice as an apothecary: apprenticeship, academic courses, hospital experience and examination. Separated apothecary from retail druggist – ‘surgeonapothecary’ • By 1848 most practitioners held multiple qualifications: LSA, MRCS (Membership of the Royal College of Surgeons), medical degree and midwifery licence. c.15,000 GPs in England and Wales by 1848. • Became basis of general practice of medicine - already by 1820s division between GPs and consultants began to be laid down. Medical Journals: pressure for reform, Lancet 1823; Provincial Medical and Surgical Journal 1840, BMJ 1857 Sir Astley Cooper (1768-1841) Lancet attacked system of hospital appointments and consultant posts as corrupt. e.g. Bransby Cooper, appointed to Guys Hospital as nephew of Astley Cooper (Astley Cooper earned c.£1,000 a year) The Cooper’s Adz!! Versus the Lancet!!, 1828. Cooper is shown being stabbed in the bottom, not just for comic effect but also as an allusion to his botched operation to remove a bladder stone for which he was sued Sir Charles Hastings (1794-1866), founder of the British Medical Association (originally called the Provincial Medical and Surgical Association 1832) Renamed BMA 1855 Medical Reform (2) 1858 Medical Act Created single medical register Equal recognition of all practitioners General Medical Council – upheld standards, education, ethics, practice 1886 Medical Amendment Act – all medical students required to have qualifications in surgery, midwifery and medicine Limitations • Still multiple routes to qualification • Quacks and irregulars still practised • Period of great upheaval and competition between doctors Irvine Loudon Medical Care and the General Practitioner (Oxford: Clarendon Press, 1986), pp. 298-301 Ivan Waddington The Medical Profession in the Industrial Revolution (Dublin: Gill and Macmillan, Humanities Press, 1984), pp.138-52. Five career patterns for doctors (Anne Digby, Making a Medical Living: Doctors and Patients in the English Market for Medicine, 1720-1911, CUP,1999): 1. The ‘classic’ GP who practised general medicine amongst a mix of social classes. 2. The GP/surgeon who practised general medicine and had a part-time appointment as a surgeon in a small hospital 3. The GP/specialist, who worked as a general practitioner but also did some consulting work in one area of medicine, such as obstetrics. 4. GPs who became consultants, men who started their careers in general medicine but switched to full-time consulting. 5. The ‘pure’ consultants, who belonged to prestigious medical institutions, held posts in major hospitals and had a private practice. Problems of medical profession • ‘Overstocking’ of medical profession. More doctors qualifying in 19thC – though middleclass providing new market, too many doctors. • Medical Societies set up to regulate intraprofessional ethics and to combat unqualified practice,e.g.Huddersfield Medico-Ethical Society est.1852 • Female practitioners – seen as source of competition though numbers low. • Professional standing – image poor (body snatching). The BMA Secret Remedies Campaign, 1909 Elizabeth Garrett Anderson (1836-1917) • First woman to qualify in medicine in Britain • LSA 1865 • Specialised in treatment of women and children – advocate of women doctor and women’s rights more broadly • Set up New Hospital for Women and Children 1872 BURKE AND HARE – GRAVE ROBBERS Luke Fildes, Physician watching over a Sick Child, 1893 Family practitioner 20thC general practice • Going to doctor now most commonly shared experience – in Britain access to GP increasingly seen as right from introduction of National Insurance 1911 and confirmed by NHS • Early 20thC most patients saw doctor in their own homes or doctors’ parlour, many would also carry out small surgical operations at local cottage hospital, most also practised midwifery • NHS expelled last GPs from hospitals, but GPs got the patients (specialists the hospitals) – redefined role to refer patients • Home visits common early in the 20thC – in 1908 Harry Roberts, Hackney GP, saw 80 patients at home a day. By 1970s home visits fell to c.8-15 daily, and now extremely rare. Conclusion Did the 19th century see the emergence of a modern profession? YES….By the late 19th century meets many of criteria of a profession: unity, educational standards, GMC, register, regulation, medical press BUT…. • Mixed route to medical qualification • Intra-professional tensions e.g. hospital vs. public posts, generalists vs. specialists • Unqualified still practising and popular with the public NOT CONSOLIDATED PROFESSIONALISATION – this has to wait until 20thC which saw more clear cut split between GPs and hospital specialists Meaning of medical practice/idea of family doctor • Site of practice changed significantly – GP until late C20th associated much more with home setting, knew patients, practices smaller • In last quarter of C20th GPs practices complex and large – investment in equipment and staff • Trend accelerated since NHS market imposed in 1989-90, though remain purveyors of public service (very few private GPs) • Doctor-initiated and medical content of consultation increased and patient-initiated and social content decreased