John Amson Capitman, PhD. Nickerson Professor of Health Policy
advertisement

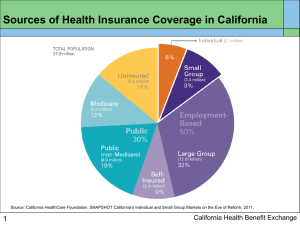
John Amson Capitman, PhD. Nickerson Professor of Health Policy Central Valley Health Policy Institute California State University, Fresno The 2009/2010 health reform debate Goals for Health Reform ◦ Underlying Philosophical arguments ◦ Continuous, Affordable, Universal, Sustainable Effective (CAUSE) PPAC (+ Reconciliation): Short-term changes PPAC (+ Reconciliation): Middle-term changes ◦ Low-income/uninsured ◦ Medicare ◦ Privately insured Assessing PPAC using the CAUSE goals Next Steps/ The “devil” in implementation detail Questions “Private sector dominant”/ Massachusetts model—approach from outset ◦ No serious debate of Universal/single payer plans ◦ No serious debate of goals for reform ◦ “Card not care” : “health reform” vs “health insurance reform” Successful lobbying by insurance and pharmaceutical industries August tea parties---astro-turf and manufactured rage House and Senate bills passed Reconciliation after presidential intervention Health care as: ◦ RIGHT ◦ PRIVILEDGE ◦ RESPONSIBILITY US historic compromise: All of the above US compromise: International comparisons IOM Report as basis Approach based on “real US health system” rather than political philosophy CAUSE and the goals for reform ◦ ◦ ◦ ◦ ◦ Continuous, Affordable, Universal, Sustainable Effective Failure of prevention adherence Most spending for chronic disease Unnecessary burden of poor management of chronic disease Unnecessary burden of preventable disease No breaks in coverage/primary care access Patient centered medical home Reimburse “cognitive services” Improved transition management About 50 million uninsured and about same number find it unaffordable/inadequate---about ¼ find health care unaffordable Health care costs biggest source of bankruptcy Employer coverage has decreased –unaffordable to many small businesses—limits mobility Keep total health care expense to 10% or less of pre-tax income for those within 500% of poverty Break link between employment and coverage Uninsured and inadequately insured have worse health outcomes, increase costs of care for all, increase unequal healthcare burden on lowincome communities Exclusion of demographic (e.g. “undocumented”, young adults) and need (e.g. behavioral health, community long-term care) groups increases overall system costs Universal access promotes efficiency and public health Remove demographic and need barriers to care Under current law and practice, Medicare goes broke next decade AND: health care grows ½ of economy reducing US global position Establish budget discipline for health care at national, state, and local levels Change reimbursement systems to promote prevention and efficiency Use financial transactions tax or FAT (financial activity tax) to finance health care Despite spending more, US has poorer health outcomes across life span Regional, race/ethnic, rural/urban, condition inequalities in care and outcomes Over-use of high cost/low efficacy services Low adherence to prevention recommendations Change reimbursement and tort laws to promote evidence-based and safe practice Change reimbursement and regulation to promote prevention and “cognitive” services Address health inequities through financing and regulatory changes Persons 23-26 remain on parents’ plan New federally-funded high risk pool Tax credit for small employers to purchase coverage Private insurance reforms (lifetime cap, cancellations, pre-existing conditions for children, preventive services with no co-pay, reporting on loss ratio and cost increase) Medicaid expanded to 133% of FPL. Establish state exchange (uninsured/insured but unaffordable 133-400 %FPL, small business employees) for legal residents. Subsidized coverage with total exposure less than 10% of pre-tax for 133-200% FPL, but less affordable. Increased Medicaid rates Demonstrations, start-up funds, training funds to improve safety-net capacity and effectiveness Reduced subsidy for Medicare Advantage plans— Medicare solvent for 15 years Donut hole in Part D closed by 2020—short-term asssistance Immediate benefit improvements ◦ ◦ ◦ ◦ ◦ Annual physical No co-pay for preventive services Improves primary care reimbursement Transitional care benefits Bundled payments and other reimbursement reform demonstrations Comparative effectiveness and payment review commissions Individual mandate to hold qualifying insurance Phased-in reforms (guaranteed issue, community rating, maximum out-of-pocket) apply to employer and individual markets Establishes level of exposure, loss ratios, minimum benefits etc. for qualifying plans Tort reforms Medical home demonstration Comparative effectiveness research Oversight for premium increases GRADE Rational Continuous C 1) Reduces risk of dropped coverage, 2) fewer uninsured for job change, 3) only demonstration on patient-centered medical home, 4) no co-pay for prevention, 5) inadequate payment reform Affordable B 1) Makes health care affordable for under 200% FPL, 2) Does not ensure affordability for 200400% FPL, 3) Does not limit growth of private premiums for 400+ FPL Universal C 1) Excludes “undocumented” 2) Unaffordable coverage may reduce enrollment below 95% estimate, 3) Rural initiatives/safety net expansions/disparity initiatives may not improve access Sustainable D 1) Extend Medicare solvency by 6 years, 2) Helps states expand Medicaid, 3) Some effort to “bend costs curve” but not enough, 4) No budget discipline for health care Effective C 1) Commissions and demonstrations to improve effectiveness, 2) Better consumer information 3) public health/healthy community initiatives, 4) health care safety and quality initiatives 1) PPAC leaves health care profit motive intact. ◦ ◦ ◦ Insurers will seek to limit (unprofitable) enrollment and coverage Pharmaceutical and other private health care will seek cost increases Ineffective, high-technology procedures will be pushed How will CA ensure that abuses actually stop? Can CA develop public options? Can CA institute additional practice and payment changes? 2) PPAC leaves undocumented uninsured (at least 200,000 in SJV) a state and local responsibility. How will CA and local government respond? 3) PPAC increases MediCal eligibility, expands Healthy Families, and creates Exchange but leaves much flexibility in benefits design and administrative process. How will CA manage new beneficiaries? How will CA expand safety net services to meet new demand? 4) PPAC will slow but not limit premium rate hikes. What else can CA do to keep health care affordable? 5) PPAC will promote comparative effectiveness knowledge but not require practice change. How can CA promote adoption of evidence-based practice? How can CA promote patient-centered medical home and disease management?