n. EMPLOYEE BENEFITS FOR GENERAL PRACTITIONERS: TEN RULES THAT EVERY
advertisement

EMPLOYEE BENEFITS FOR GENERAL
PRACTITIONERS: TEN RULES THAT EVERY
ATTORNEY SHOULD KNOW ABOUT ERISA
by Jayne Elizabeth Zanglein°
I.
n.
m.
IV.
V.
VI.
VII.
VIII.
IX.
X.
XI.
INTRODUCTION................................
RULE #1: ERISA TRUMPS EVERYTHING-ALMOST ANY
STATE LAW CAUSE OF ACTION You CAN THINK OF WILL
BE PREEMPTED BY ERISA
RULE #2: WITH RESPECT TO REMEDIES, PARTICIPANTS ARE
WORSE OFF Now THAN THEY WERE BEFORE ERISA
WAS ENACTED
RULE #3: THERE IS AN EXCEPTION FOR EVERY RULESOME CLAIMS ARE NOT PREEMPTED BY ERISA
RULE #4: SOMETIMES THE FIFTH CIRCUIT WILL ApPLY
FEDERAL COMMON LAW TO A VOID THE EFFECTS OF
PREEMP110N . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . ..
RULE #5: "As CONGRESS GIVETH, CONGRESS
TAKETH AWAY"-SELF-FuNDED WELFARE PLANS GET
AWAY WITH ALMOST ANYTHING . . . . . . . . . . . . . . . . . ..
RULE #6: DISCRIMINATION UNDER ERISA REQUIRES
SPECIFIC INTENT BY THE EMPLOYER TO INTERFERE WITH
ERISA BENEFITS
RULE #7: ONLY PARTICIPANTS, BENEFICIARIES, AND
FIDUCIARIES, BUT NOT INTENDED BENEFICIARIES, HAVE
STANDING TO SUE UNDER ERISA
RULE #8: UNDER MOST PLANS, THE PLAN ADMINISTRATOR
WILL HAvE DISCRETIONARY AUTHORITY TO CONSTRUE THE
TERMS OF THE PLAN, AND THEREFORE, THE STANDARD OF
REVIEW WILL BE ABUSE OF DISCRETION
RULE #9: FACTUAL DETERMINATIONS BY A PLAN
ADMINISTRATOR ARE REVIEWED FOR ABUSE OF
DISCRETION REGARDLESS OF PLAN LANGUAGE
RULE #10: ADVISORS WHO Do NOT HAVE AUTHORITY
AND CONTROL OVER PLAN ASSETS AND WHO Do NOT
RENDER REGULAR INVESTMENT ADVICE TO THE PLAN ARE
NOT FIDUCIARIES . . . . . . . . . . . . . . . . . . . . . . . . . . . . ..
580
580
582
585
587
590
593
596
599
603
605
• Associate Dean and Professor of Law. Texas Tech Univenity School of Law. B.M.E.• Berldee
College of Music. 1975; J.D., State Univenity of New York at Buffalo. 1980.
579
HeinOnline -- 26 Tex. Tech L. Rev. 579 1995
580
XII.
TEXAS TECH LAW REVIEW
[Vol. 26:579
CONCLUSION AND FINAL RULE. . . . . . . . . . . . . . . . . . . .. 607
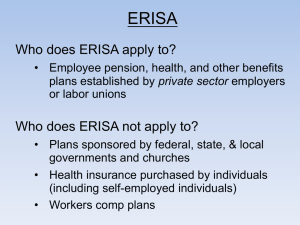
I. INTRODUCTION
This article, written on the eve of the twentieth anniversary of the
Employee Retirement Income Security Act (' 'ERISA' '), is a primer for nonERISA attorneys. Because ERISA is a complex statute that constantly
changes, it may seem fonnidable to some practitioners. After all, at least
according to legend, ERISA is an acronym for Every Ridiculous Idea Since
Adam. 1 But with a little guidance, ERISA issues that frequently arise in
general practice can be handled with confidence. Fortunately, the Fifth
Circuit's 1993-1994 tenn offers a good outline of issues for attorneys who
do not frequently work in this area.
II. RULE #1: ERISA TRUMPS EVERYTHING-ALMOST ANy STATE LAW
CAUSE OF ACTION You CAN THINK OF WILL BE PREEMPTED BY ERISA
ERISA preempts all state laws that relate to an employee benefit plan.2
The United States Supreme Court has broadly construed the preemption
clause, noting that it is "conspicuous for its breadth.,,3 As the Seventh
Circuit Court of Appeals stated: "Congress has blotted out (almost) all state
law on the subject of pensions, so [that] a complaint about pensions [or welfare
plans] rests on federal law no matter what label its author attaches.,,4 The
Fifth Circuit has noted that "[t]his sweeping preemption of state law is
consistent with Congress's decision to create a comprehensive, unifonn
federal scheme for the regulation of employee benefit plans.' ,s
1. One ridiculous idea that pops to mind is section 89. an amendment to the Internal Revenue
Code that sparked more controversy than any other ERISA legislation. Act of Oct. 22, 1986, 100 Stat.
2494 (repealed 1989); see Reform Bills Make Similar Mistakes as Section 89. Former Tax Aide Says, 19
BNA PENSION & BENBFITS REP. 448, 448 (Mar. 16, 1992). It was eventually abandoned after
implementation proved impossible. See id. at 448.
2. Employee Retirement Income Sewrity Act ("ERISA") § 514(a). 29 U.S.C. § 1144(a) (1988);
see District of Columbia v. Greater Washington Bd. of Trade, _ U.S. _' - ' 113 S. CL 580,583, 121
L. Ed. 2d 513, 520 (1992); Ingersoll-Rand Co. v. McClendon, 498 U.S. 133, 139 (1990); Pilot Life Ins.
Co. v. Dedeaux, 481 U.S. 41, 45-47 (1987); Shaw v. Delta Air Lines Inc., 463 U.S. 85,96-97 (1983).
ERISA's definition of an "employee benefit plan" includes pension and welfare plans. 29 U.S.C. §
1002(3) (1988).
3. FMC Corp. v. Holliday, 498 U.S. 52, 56-58 (1990); see also Shaw, 463 U.S. at 96
(recognizing breadth of ERISA's preemption) ; Alessi v. Raybestos-Manhattan, Inc., 451 U.S. 504, 52425 (1981) (finding New Iersey statute to be within the bounds of ERISA); Christopher v. Mobil Oil
Corp., 950 F.2d 1209, 1218 (5th Cir.) (recognizing broad interpretation of ERISA's preemption
provisions), cert. denied, _ U.S. --' 113 S. CL 68, 121 L Ed. 2d 35 (1992).
4. Bartholet v. Reishauer A.G. (Zurich), 953 F.2d 1073, 1075 (7th Cir. 1992).
5. Corcoran v. United HealthCare, Inc., 965 F.2d 1321, 1329 (5th Cir.), cert. denied, _ U.S.
--' 113 S. Ct. 812, 121 LEd. 2d 684 (1992); see McClendon, 498 U.S. at 142; Dedeaux, 481 U.S. at
45-46.
HeinOnline -- 26 Tex. Tech L. Rev. 580 1995
1995]
EMPLOYEE BENEFITS
581
Although there is absolutely no doubt that ERISA preempts all state law
claims that relate to an employee benefit plan (with some exceptions for
insurance, banking, securities,6 and general criminal laws?), courts decide
hundreds of ERISA preemption cases each year. The number of preemption
cases is startling, given that the law is well settled in this area. s For
example, this term, the Fifth Circuit decided six preemption cases. 9 In
Anderson v. Electronic Data Systems Corp.,1° the Fifth Circuit noted,
"[We] are hardly writing on a clean slate, as the subject of federal
preemption under ERISA has generated a wealth of jurisprudence. "11 Yet,
the issue keeps reappearing, as if plaintiffs believe that by sheer force of
repetition, the law will change. More likely, plaintiffs' attorneys believe that
if given just the right sympathetic facts, judges might ignore preemption and
rule with the heart instead of the mind. 12
This is unlikely to happen. The Fifth Circuit has heard numerous
ERISA cases about hapless participants who have been wronged by
unscrupulous employers or insurers. In fact, the Fifth Circuit has dubbed
these hapless participants as "betrayed without a remedy. "13 The Fifth
Circuit has been reluctant to expand federal common law under ERISA to
provide remedies for these remediless participants. For example, in
Corcoran v. United HealthCare, inc.,14 the Fifth Circuit preempted a
lawsuit brought by a grieving couple for the wrongful death of their unborn
child. 15 The couple alleged that the fetus's death was caused by a negligent medical decision made by a utilization review company.16 The Fifth
Circuit held that ERISA preempted the wrongful death claim and said that
"[t]he acknowledged absence of a remedy under ERISA's civil enforcement
6. 29 U.S.C. § 1144(b)(2)(A) (1988).
7. Id. § 1144(b)(4).
8. Of course, there are always cases of first impression. However, most of the cases discussed
in this article relate to routine preemption issues which courts have previously addressed.
9. Anderson v. Electronic Data Sys. Corp., 11 F.3d 1311 (5th Cir. Jan.), cert. denied, _
U.S.
_, 115 S. Ct. 55, 130 L. Ed. 2d 14 (1994); Bulks v. Amerada Hess Corp., 8 F.3d 301 (5th Cir. Dec.
1993); Perdue V. Burger King Corp., 7 F.3d 1251 (5thCir. Dec. 1993); Epps v. NCNB Texas, 7 F.3d44 (5th
Cir. Oct. 1993); NGS Am., Inc., v. Barnes, 998 F.2d 296 (5th Cir. Aug. 1993); Tingle v. Pacific Mut.Ins.
Co., 996 F.2d 105 (5th Cir. July 1993).
10. 11 F.3d 1311 (5th Cir. Jan. 1994).
11. Id.atI313.
12. In Smith v. Hartford Insurance Group, 6 F.3d 131 (3d Cir. 1993), Judge Hutchinson, in a
dissenting opinion, commented: "Logic may be the law's tool but its heart is justice, and the public's
demand for concrete justice will not be contained by the straitjacket of inflexible rules." Id. at 146
(Hutchinson, J., dissenting).
13. Degan v. Ford Motor Co., 869 F.2d 889, 895 (5th Cir. 1989).
14. 965 F.2d 1321, 1333 (5th Cir.), cert. denied, _
U.S. _,113 S. Ct. 812, 121 L. Ed. 2d
684 (1992).
15. Id. at 1331.
16. Id. at 1326.
HeinOnline -- 26 Tex. Tech L. Rev. 581 1995
582
TEXAS TECH LAW REVIEW
[Vol. 26:579
scheme ... does not alter our conclusion.';17 The court held that "[w]hile
we are not unmindful of the fact that our interpretation of the preemption
clause leaves a gap in remedies within a statute intended to protect
participants in employee benefit plans, the lack of an ERISA remedy does
not affect a preemption analysis.',18 Likewise, in Hansen v. Continental
Insurance CO.,19 the Fifth Circuit held that "ERISA's preemption provision
bars state law causes of action even though such preemption may leave a
victim ... without a remedy,',20
III. RULE #2: WITH RESPECT TO REMEDIES, PARTICIPANTS ARE WORSE
OFF Now THAN THEY WERE BEFORE ERISA WAS ENACTED
Although it seems unfair that participants are worse off with respect to
remedies than they were twenty years ago before the passage of ERISA, this
is the current state of the law. 21 Before ERISA, plaintiffs had a full range
of remedies to choose from under state and federal law. After ERISA, as
interpreted by the Supreme Court, plaintiffs have fewer remedies. 22 ERISA
does not provide for extra-contraetual23 or punitive damages,24 so there
is little to deter an unscrupulous employer or insurer. Basically, ERISA
allows a participant to sue to recover an unpaid benefit,25 but does not
allow any other monetary damages.2Ci In some cases, the participant cannot
directly receive any recovery. For example, where a participant alleges a
breach of fiduciary duty, any recovery goes to the plan, not the individual.27
This lack of remedies is exacerbated by the preemption of state law claims.
In suits for negligence,28 violation of the Deceptive Trade Practices Aet,29
intentional infliction of emotional distress,30 misrepresentation,31 tortious
17.
18.
Jd. at 1333.
Jd. (citations omitted).
19. 940 F.2d 971 (5th Cir. 1991).
20. Jd. at 979.
21. See Labor Department Reviews Cases in Effort to Help Determine Law. 21 BNA PENSION
& BBNEfITS REp. 1689. 1689 (Sept. 12. 1994).
22. See Jayne Zanglein. Closing the Gap: Safeguarding Participants' Rights by Expanding the
Federal Common Law of ERlSA. 72 WASH. U. LQ. 671 (1994). for a more detailed analysis of this
problem.
23. Massachusetts Mut. llie Ins. Co. v. Russell. 473 U.S. 134. 148 (1985).
24. Jd.
25. 29 U.S.C. § 1102(a)(1)(B) (1988).
26. Mertens v. Hewitt Assoc., _ U.S. -..J -..J 113 S. Ct. 2063. 2066-68. 124 L Ed. 2d 161.
167-69 (1993).
27. Russell. 473 U.S. at 144.
28. E.g., Ramirez v. Intercontinental Hotels, 890 F.2d 7(1.). 762-63 (5th Cir. 1989).
29. E.g .• id.
.
30. E.g .• Burks. 8 F.3d at 305; Brown v. Southwestern Bell Tel. Co., 901 F.2d 1250. 1254 (5th
Cir. 1990).
31. E.g .• Degan, 869 F.2d at 893.
HeinOnline -- 26 Tex. Tech L. Rev. 582 1995
1995]
EMPLOYEE BENEFITS
583
interference,32 unfair claims practices,33 breach of contract,34 wrongful
death,3s and wrongful discharge,36 ERISA preempts state law without
providing an adequate remedy.
For example, this term in Anderson v. Electronic Data Systems, Corp.,
the Fifth Circuit held that Anderson's claim that he was demoted and
discharged for refusing to violate ERISA and for whistleblowing was
preempted by ERISA. 3? The Fifth Circuit relied on Ingersoll-Rand Co. v.
McClendon,38 in which the Supreme Court held that a law "relates to" an
ERISA plan, and is therefore preempted, "if it has a connection with or
reference to such a plan...39 The Fifth Circuit held that Anderson's
wrongful discharge claim was preempted because it was "based on his
refusals to carry out violations of ERISA."4O Because Anderson's claim
depended on the existence of a pension plan, it "relate[d] to" an ERISA
plan and was preempted.41 The court also noted that a state cause of
action for wrongful discharge would conflict with the antidiscrimination rule
found in ERISA section 510.42 The court said that "such a finding of
preemption does not hinge on whether ERISA provides the remedy the
plaintiff seeks or any remedy at all for the alleged wrong.' ,43
At first blush, the preemption of Anderson's wrongful discharge case
might appear logical because he mentioned ERISA in his original complaint.
However. Anderson was not an ERISA case. It was a wrongful discharge
case for which Anderson might have recovered substantial damages, if
successful. Under ERISA, however, extra-contractual or punitive damages
are unavailable, so the only remedy would have been for Anderson to return
32.
E.g., Kuhl v. Lincoln Nat'l Health Plan, Inc., 999 F.2d 298,302·03 (8th Cir. 1993), cerr.
U.S.
, Il4 S. Ct. 694, 126 L Ed. 2d 661 (1994).
3~E.g., ~e v. Connecticut Gen. Life Ins. Co., 867 F.2d 489, 493-94 (9th Cir. 1988), cert.
denied, 492 U.S. 906 (1989).
34. E.g., Kuhl, 999 F.2d at 302-03; Cromwell v. Equicor-Equitable HCA Corp., 944 F.2d 1272,
1275 (6th Cir. 1991); Powell v. Chesapeake & Potomac Tel Co., 780 F.2d 419, 421-22 (4th Cir. 1985),
cert. denied, 476 U.S. Il70 (1986); Shaw v. InCI Ass'n of Machinists & Aerospace Workers Pension
Plan, 563 F. Supp. 653, 658-59 (C.D. Cal. 1983), affd, 750 F.2d 1458 (9th Cir.), cert. denied, 471 U.S.
Il37 (1985).
35. E.g., Corcoran, 965 F.2d at 1333.
36. E.g., Anderson, II F.3d at 1314.
37. Id. Anderson alleged that he was discharged for refusing to sign pension checks without the
approval of the trustees and for refusing to write minutes for meetings that he did not attend. Id. at 1312.
Anderson alleged that such actions would have violated ERISA. Id. Later, Anderson amended his
complaint and deleted all references to ERISA. Id. at 1313.
38. 498 U.S. 133 (1990).
39. Id. at 139 (quoting Shaw, 463 U.S. at 96-97).
40. Anderson, II F.3d at 1314.
41. Id.
42. 29 U.S.C. § 1140 (1988).
43. Anderson, II F.3d at 1314.
denied,
HeinOnline -- 26 Tex. Tech L. Rev. 583 1995
584
TEXAS TECH LAW REVIEW
[Vol. 26:579
to work for an employer who he believed was dishonest and who fired him
for blowing the whistle.
In Burks v. Amerada Hess COrp.,44 the Fifth Circuit held that an
employee's claim for intentional infliction of emotional distress arising from
a wrongful termination was preempted by ERISA. 45 Originally, Burks
filed a complaint alleging that he had been wrongfully fired in retaliation for
filing a worker's compensation claim.46 In his original complaint, Burks
alleged that as a result of his discharge, he lost pension and medical benefits
that he otherwise would have accrued,47 Later, he amended the complaint
to delete any references to the loss of pension and medical benefits. but still
alleged that his employer improperly denied his long-term disability
benefits.48
The Fifth Circuit preempted Burk's claim for intentional infliction of
emotional distress, stating that the claim was preempted because it was
based on the employer's alleged denial of long-term disability benefits.49
The court noted: "This is not a case in which the loss of benefits is merely
an element in damages related to a claim for wrongful discharge.' ,so The
court expressed its displeasure that Burks engaged in "forum manipulation.' ,51 The court found that Burks engaged in an obvious and somewhat
frantic maneuver to avoid federal jurisdiction.52 The court stymied Burks'
attempt at forum manipulation by denying his motion to remand. 53
In Epps v. NCNB Texas,S4 the Fifth Circuit noted that "[w]hen a court
must refer to an ERISA plan to determine the plaintiff's retirement benefits
and compute the damages claimed, the claim relates to an ERISA plan.' ,55
The court held that even though Epps did not mention ERISA or specifically
refer to an employee benefit plan in his complaint, his claim for breach of
obligation to pay severance benefits was preempted.56 The court determined that preemption was appropriate because Epps sued to recover' 'loss
of pension and retirement benefits which would have accrued and vested"
44.
8 F.3d 301 (5th Cir. Dec. 1993).
45.
46.
47.
48.
[d. at 304-OS.
[d. at 303.
[d.
[d.
49. [d. at 305. The court held that "[a] state [law] cause of action for emotional distress arising
from the denial of employee benefits determines when an employer can and cannot terminate an
employee's benefits," [d.
50. [d. The court explained that "[a] claim that unlawful termination resulted in loss of benefits
is not preempted by ERISA," [d. at 306.
51. [d.
52. [d.
53. [d.
54. 7 F.3d 44 (5th Cir. Oct. 1993).
55. [d. at 45 (citing Christopher, 950 F.2d at 1218-20).
56. [d.
HeinOnline -- 26 Tex. Tech L. Rev. 584 1995
1995]
EMPLOYEE BENEFITS
585
if the employer had not breached the employment contract. S7 The court
held that because it would have been required to refer to the pension plan
to calculate the damages claimed, the claim was preempted.58 Likewise,
in Perdue v. Burger King COrp.,59 the court held that a common law fraud
claim was preempted "because the only damages recoverable under the
claim 'relate[d] to' the value of severance benefits" under an employee
benefit plan.60
IV. RULE #3: THERE IS AN EXCEPTION FOR EVERY RULE-SOME
CLAIMS ARE NOT PREEMPTED BY ERISA
Caution, however. For every rule, there is an exception! Not all state
causes of action will be preempted. Occasionally, the Fifth Circuit will hold
that a state law claim is not preempted because it does not "relate to" a
plan. This term, in Perdue, the court held that ERISA did not preempt a
claim for breach of an agreement to confer a franchise because it did not
relate to a plan.61
Similarly, in Weaver v. Employers Underwriters, Inc.,62 the Fifth
Circuit held that ERISA did not preempt the claims of an independent
contractor who was neither a participant nor a beneficiary and thus not a
person traditionally protected under ERISA. Jimmy Weaver was hired by
Malcolm Rodrigues as a saw hand to fell lumber for an unincorporated
logging business. 63 Rodrigues identified Weaver as a subcontractor for
purposes of federal income tax and social security taxes. 64 Rodrigues
became a member of a multi-employer medical plan that provided benefits
to Rodrigues and his employees.65 The plan covered all employees who
worked an average of one or more hours a week. 66
Weaver was injured by a falling tree. 67 He applied for and began
receiving benefits under the plan. 68 Later, Rodrigues informed the insurer
that Weaver was not an employee and payments ceased.69 The insurer
57. Id.
58. Id.
59. 7 F.3d 1251 (5th Cir. Dec. 1993).
60. Id. at 1255-56.
61. Id. at 1256.
62. 13 F.3d 172, 176 (5th Cir. Feb.), cerr. denied, _
866 (1994).
63. Id. at 173.
64. Id. at 174.
65. Id.
66. Id.
67. Id.
68. Id.
69. Id.
U.S. - ' 114 S. Ct. 2137. 128 L. Ed. 2d
HeinOnline -- 26 Tex. Tech L. Rev. 585 1995
586
TEXAS TECH LAW REVIEW
[Vol. 26:579
negotiated a lump sum settlement with Weaver?O Weaver was dissatisfied
with the settlement and sued Rodrigues, the insurer, and an insurance
adjuster. Weaver alleged, among other things, violation of the Texas
Deceptive Trade Practices Act due to false, misleading, and deceptive
practices in the settlement of his claim, violation of the Texas Insurance
Code due to the alleged grossly inadequate settlement, duress, bad faith,
conspiracy to deceive, and negligence in failing to provide a safe workplace
and safe equipment.71 The district court preempted all of Weaver's claims
except those relating to unsafe working conditions and inadequate equipment
and held that Weaver had no standing to bring an ERISA claim.72
Weaver appealed, arguing that as an independent contractor, he was
covered by the plan, but that the portion of the plan that covered nonemployees was not an ERISA plan; therefore, his claims were not preempted.73 The Fifth Circuit acknowledged that a Rhode Island district court
"ha[d] held that a plan can be divided into ERISA and non-ERISA portions. ,,74 The court held that ERISA did not preempt Weaver's claims, but
declined to rule, however, on the issue of whether a plan may be split into
ERISA and non-ERISA parts.7S
The court held that ERISA preempts state law claims if two factors are
present: "(1) the state law claims address areas of exclusive federal
concern, such as the right to receive benefits under the terms of an ERISA
plan; and (2) the claims directly affect the relationship between the
traditional ERISA entities - the employer, the plan and its fiduciaries, and
the participants and beneficiaries.' ,76
Both factors must be present. The court held that the second factor was
not present here: the claims of an independent contractor do not "directly
affect the relationship between the traditional ERISA entities.',n Weaver
was not a participant in the plan because he was not an employee.78
ERISA defines a participant as:
[A]ny employee or former employee of an employer, or any member or
former member of an employee organization, who is or may become
eligible to receive a benefit of any type from an employee benefit plan
which covers employees of such employer or members of such organiza-
70.
71.
72.
73.
74.
1993».
[d.
[d.
[d.
[d. at 174-75.
•
[d. at 175 (citing Kelly v. Blue Cross & Blue Shield, 814 F. Supp. 220, 227-29 (D. R.I.
75. Weaver. 13 F.3d at 175.
76.
Cir. 1990)
77.
78.
[d. at 176 (citing Memorial Hasp. Sys. v. Northbrook Life Ins. Co.• 904 F.2d 236, 245 (5th
(footnotes omitted».
[d.
[d.
HeinOnline -- 26 Tex. Tech L. Rev. 586 1995
1995]
EMPLOYEE BENEFITS
587
lion, or whose beneficiaries may be eligible to receive any such benefit79
This definition clearly focuses on the employer-employee relationship.
Weaver was an independent contractor, not an employee; therefore, he could
not be a participant.80
The court also ruled that Weaver was not a beneficiary.81 ERISA
defines a beneficiary as "a person designated by a participant, or by the
tenns of an employee benefit plan, who is or may become entitled to a
benefit thereunder... 82 Weaver did not fall within this definition of
beneficiary.83
The court noted that the claims of a nonparticipant and nonbeneficiary
such as Weaver "do not affect the relationship between the traditional
ERISA entities" and are not preempted. 84 As previously noted, individuals
are better off, in some respects, if they are not covered by ERISA.
V. RULE #4: SOMETIMES THE FIFrH CIRCUIT WILL ApPLY FEDERAL
COMMON LAW TO AVOID THE EFFECTS OF PREEMPTION
In Brandon v. Travelers Insurance CO.,8S a case of first impression
with surprising results, the Fifth Circuit applied federal common law to
detennine that an ex-spouse was not entitled to receive benefits under a life
insurance plan even though she was designated as a beneficiary under the
tenns of the plan.
The court's opinion took some strange turns and twists. First (and
predictably), the court held that ERISA preempts state laws relating to the
transfer of property on divorce. 86 The court held that ERISA preempts a
Texas Family Code provision87 that requires a life insurance plan participant to redesignate an ex-spouse after divorce in order to maintain that exspouse as the designated beneficiary.88
Richard Brandon designated his wife, Wanda, as a beneficiary of a life
insurance policy offered through his employer.89 At the time of the
designation, the Brandons were separated.90 Richard told Wanda that she
79.
80.
81.
82.
83.
29 U.S.C. § 1002(1) (1988).
Weaver. 13 F.3d at 176.
Id. at 177.
29 U.S.C. § 1002(8) (1988).
Weaver, 13 F.3d at 177.
84.
Id.
18 F.3d 1321 (5th Cir. Apr. 1994).
Id. at 1326.
TEX. FAM. CODE ANN. § 3.632 (Vernon 1993).
Brandon, 18 F.3d at 1326.
Id. at 1323.
Id.
85.
86.
87.
88.
89.
90.
HeinOnline -- 26 Tex. Tech L. Rev. 587 1995
588
TEXAS TECH LAW REVIEW
[Vol. 26:579
would remain the designated beneficiary even if they divorced. 9l The
Brandons divorced. 92 According to the divorce decree, each spouse would
separately retain his or her own employment benefits.93 The divorce decree
specifically divested Wanda of all rights in any "benefit program existing by
reason of [Richard's] past, present or future employment. "94 The Brandons
were on friendly terms and continued to socialize.9s Richard aid not change
his designation of Wanda as his beneficiary.96 When Richard died, his
employer notified Wanda that she was the designated beneficiary.97 Wanda
applied for the life insurance benefit. 98 Later, Wanda discovered that the
benefit had been paid to Richard's brother, Gary, who was listed as a
contingent beneficiary.99 Richard's employer paid Gary because Richard
had not redesignated Wanda as his beneficiary after the divorce, as required
by Texas Family Code section 3.632. 100 Wanda sued. 101 The district
court held that Wanda was not entitled to the life insurance because the
divorce decree, which determined her rights, divested her of those benefits. 102
The plan required the employer to "pay the insurance proceeds to the
designated beneficiary unless for specified reasons the administrator
determine[d] that the contingent beneficiary should be paid. ,,103 Therefore, under the terms of the plan, Wanda, as the designated beneficiary,
should have been entitled to the benefit
The Fifth Circuit rejected the employer's contention that the Texas
Family Code requires a redesignation of an ex-spouse after divorce to
maintain the ex-spouse as the designated beneficiary of a life insurance
policy.l04 The court held that ERISA preempts the Texas Family Code
provision because that provision "relates to" an employee benefit plan. lOS
So far, so good. But here's where the case took some swprising turns.
Next, the court considered whether ERISA controlled exclusively or whether
federal common law applied. lOO The court noted that the circuit courts
Id.
92. Id.
93. Id.
94. Id.
95. Id.
96. Id.
97. Id.
98. Id.
99. Id.
100. Id.
101. Id.
102. Id.
103. Id. at 1324.
104.· Id. at 1324-25.
105. Id. at 1325; see supra text accompanying notes 2-20 for a mon: exh8l1stive diSalSSion of
preemption.
106. Brandon, 18 F.3d at 1325.
91.
HeinOnline -- 26 Tex. Tech L. Rev. 588 1995
1995]
EMPLOYEE BENEFITS
589
have taken two different approaches. 107 Some, like the Sixth Circuit,
apply strict statutory construction. IDS Other courts, like the Seventh and
Eighth Circuits, look to federal common law to achieve a more equitable
result. I09
The court· first examined the strict statutory construction approach
adopted by the Sixth Circuit in McMillan v. Parrot. IlO ERISA section
404(a)(l)(D) requires a plan administrator to administer the plan "in
accordance with the documents and instruments governing the plan. ,,111
The Sixth Circuit held that ERISA section 404(a)(l)(D) requires plan
administrators to follow plan documents, and when a conflict arises between
plan documents and a divorce decree, the plan documents govem. 112 The
Sixth Circuit reasoned that the "clear statutory command, together with the
plan provisions, answer the question; the documents control, and those name
[the ex-wife]. ,,113
Next. the Fifth Circuit examined the more liberal approach taken by the
Seventh Circuit in Fox Valley & Vicinity Construction Workers Pension
Fund v. Brown 1l4 and the Eighth Circuit in Lyman Lumber Co. v. Hill. ll5
Those courts examined whether" a valid, specific waiver of benefits in the
divorce decree" had occurred and whether the court could give effect to this
waiver under federal common law. 116 In Fox Valley, the Seventh Circuit
looked to Illinois family law which provided that a divorce decree will not
affect pension rights unless the decree specifically tenninated those
rights. 117 The court held that "the ability of a spouse to waive rights to
a benefit through a specific waiver in a divorce settlement has been recognized by many [state] courts and we adopt that rule for purposes of
ERISA. "liS
The Fifth Circuit adopted the reasoning of Fox Valley and applied the
Texas Family Code's "presumption of waiver absent redesignation
following divorce. ,,119 However, the court cautioned that "any waiver of
107. [d.
108. [d. at 1325-26 (citing McMillan v. Parrott. 913 F.2d 310 (6th Cir. 1990».
109. [d. at 1326 (citing Fox Valley & Vicinity Constr. Workers Pension Fund v. Brown, 897 F.2d
275 (7th Cir.) (en bane). cert. denied. 498 U.S. 820 (1990); Lyman Lumber Co. v. Hill, 877 F.2d 692
(8th Cir. 1989».
110. 913 F.2d 310 (6th Cir, 1990).
11 I. 29 U.S.c. § 1100(a)(I)(O) (1988 & Supp. V 1993).
112. Brandon. 18 F.3d at 1325.
113. [d. at 1326 (quoting McMillan, 913 F.2d at 311).
114. 897 F.2d 275. 280 (7th Cir.) (en bane). cert. denied. 498 U.S. 820 (1990).
115. 877 F.2d 692 (8th Cir. 1989).
116. Brandon. 18 F.3d at 1326.
117. [d. (citing Fox Valley. 897 F.2d at 281-82).
118. [d. (citing Fox Valley. 897 F.2d at 281).
119. Jd.
HeinOnline -- 26 Tex. Tech L. Rev. 589 1995
590
TEXAS TECH LAW REVIEW
[Vol. 26:579
ERISA benefits [must] be explicit, voluntary, and made in good faith. "120
The court found that Wanda Brandon had explicitly and voluntarily waived,
in good faith, her right to the insurance proceeds, even though she did not
attend the divorce proceedings: "The divorce decree was a bona fide
waiver of her rights to the insurance policy proceeds and we are bound to
cany out the provisions of the agreement signed by the parties.' ,121
Therefore, Wanda was not entitled to the proceeds of the life insurance.
As a strong advocate of the application of federal common law to fill
in the gaps in ERISA,122 I applaud the use of federal common law to
achieve more equitable results in ERISA cases. However, it seems strange
that Brandon applied federal common law since ERISA clearly provides that
the plan documents control and since the attorneys involved in the case
should have known the effect of ERISA on divorce decrees and qualified
domestic relations orders. 123 What was unusual in Brandon was that the
court used federal common law to clearly act against the wishes of the
participant and the beneficiary to reach an unintended and contrived result.
Brandon presents a case where the beneficiary wins under a preemption
analysis and then loses when the court applies federal common law.
Meanwhile, plaintiffs like Anderson who are discharged for whistleblowing
are "betrayed without a remedy," lost in the black hole left by federal
preemption and inadequate remedies. The moral: It is difficult for a participant or a beneficiary to win in the Fifth Circuit.
VI. RULE #5: "As CONGRESS GIVETH, CONGRESS TAKETH
AWAy"I24_S ELF-F'UNDED WELFARE PLANS GET AWAY WITH ALMOST
ANYTHING
Self-funded employee benefit welfare plans (Le., medical plans) exist
in the best of all possible worlds. They are not required to comply with
state-mandated benefit laws, and they are exempt from state laws relating
to taxes and fees.
ERISA's preemption clause contains an "insurance savings clause"125
that provides that nothing in ERISA "shall be construed to exempt or
relieve any person from any law of any state which regulates insurance,
120. ld. at 1327.
121. ld.
122. See Jayne Zanglein. Closing the Gap: Safeguarding Participants' Rights by Expanding the
Federal C011l1TlOn lAw of ERISA. 72 WASH. U. L.Q. 671 (1994) for a more detailed analysis of this
problem.
123. In fact, it is possible that an astlne lawyer might have advised Richard Brandon not to worry
about the redesignation of Wanda as his designated beneficiary because ERISA preempts the Texas
Family Code provision.
124. NGS Am., Inc. v. Bames. 998 F.2d 296 (5th Cir. Aug. 1993).
125. 29 U.S.C. § 1144(b)(2)(A) (1988).
HeinOnline -- 26 Tex. Tech L. Rev. 590 1995
1995]
EMPLOYEE BENEFITS
591
banking, or securities."126 In Metropolitan Life Insurance Co. v. Massachusetts,127 the Supreme Court held that a state law that required insurance
companies to provide mandated mental health benefits fell within the
insurance savings clause and was not preempted by ERISA. 128 However,
the Court noted that insured plans and self-funded plans are subject to
different regulation because of ERISA's deemer clause. 129 The deemer
clause provides that ERISA plans should not be deemed to be insurance
companies. 130 The effect of the deemer clause is that insured plans are
subject to state insurance regulation, but self-funded plans are not.
In NGS American, Inc. v. Barnes,l3l the Fifth Circuit held that ERISA
preempts article 21.07-6 of the Texas Insurance Code as applied to
administrators of self-funded ERISA plans. 132 Article 21.07-6 imposes
regulations, fees, and taxes on self-funded ERISA plans and their administrators. 133 The Fifth Circuit described a two-pronged test that determines
whether a state insurance law is saved from preemption by ERISA's savings
clause. l34 First, the court must determine if the statute meets a common
sense defmition of insurance regulation. 13S Second, the court must
consider three factors: "(1) whether the state statute spreads the policyholder's risk; (2) whether the state statute is an integral part of the policy
relationship between the insurer and the insured; and (3) whether the
practice is limited to entities within the insurance industry. ,,136 If the
statute meets the first prong and all three parts of the second prong, the
statute falls within ERISA's savings clause and is not preempted. 137
The court applied the test to article 21.07_6. 138 Because the Commissioner of Insurance had conceded that plan administrators of self-insured
plans subject to regulation under article 21.07-6 perform no risk-bearing
function, the court concluded that the first part of the second prong of the
126.
Id.
127.
471 U.S. 724 (1985).
128. Id. at 744.
129. Id. at 747. Employers may fund medical benefits in two ways: self-insure or purchase
insurance. NGS Am., 998 F.2d at 298. In Metropolitan Life Insurance Co., the Supreme Court held that
insured plans are subject to regulation by state insurance laws, but self-funded plans are noL
Metropolitan Life Ins. Co., 471 U.S. at 739-47.
130. 29 U.S.c. § I I44(b)(2)(B) (1988).
131. 998 F.2d 296 (5th Cir. Aug. 1993).
132. Id. at 300; see also Self-Insurance Institute of Am. Inc. v. Korioth, 993 F.2d 479 (5th Cir.
June 1993) (involving a challenge to article 21.07-6).
133. TEX. INS. CODB ANN. art. 21.07-6 (Vemon 1986 & Supp. 1994).
134. NGS Am., 998 F.2d at 299.
135. Id.
136. Id.
137. Id.
138. Id.
HeinOnline -- 26 Tex. Tech L. Rev. 591 1995
592
TEXAS TECH LAW REVIEW
[Vol. 26:579
test could not be met: the law did not spread risk among policyholders. 139
Therefore, the plan could not fall within ERISA's savings clause. 140
Next, the court rejected the Commissioner's argument that article
21.07-6 does not "relate to" an employee benefit plan because it applies to
both insured and self-funded plans. 141 Article 21.07-6 provides that the
Commissioner may review the fmancial records of the administrator and
may examine all written agreements between the plan and its insurers. 142
The statute also allows the Commissioner to audit the administrator's books
and records. 143 The court held that it was just these types of "burdens of
complying with conflicting state regulations that Congress sought to
eliminate by enacting ERISA. ,,144 The court held that the statute "related
to" an employee benefit plan and, therefore. was preempted by ERISA. 145
Tingle v. Pacific Mutual Insurance CO.,146 another preemption case
involving the insurance savings clause, might be subtitled "The Case of the
$71,300 Girdle." Mrs. Tingle injured her back while attempting to put on
her girdle. 147 She was operated on for a herniated disk and incurred
$71,300 in medical expenses. 148
Her husband submitted her claims to Pacific Mutual Insurance
Company ("Pacific") for payment. 149 Pacific investigated Mrs. Tingle's
139. The court did not evaluate whether any other parts of the test had been met. Id.
140. Id.
141. Id.
142. Id. at 299-300.
143. Id. at 300.
144. Id. (citing Shaw. 463 U.S. at 105).
145. NGS Am., 998 F.2d at 300. The court noted that the Commissioner could still enforce
article 21.07-6 against third party administrators of non-ERISA governed insurance plans, or against third
party administrators of both ERISA and non-ERISA govemed plans in their capacity as administrators
of non-ERISA governed plans. Id.
Another case this tenn dealt with Texas Insurance Code article 21.07-6. In Self-lnsuranL:e Institute
of America. Inc. v. Korioth. the Fifth Circuit held that a California not-for-profit trade association
organized to advance the self-insurance industry had standing to challenge article 21.07-6. 993 F.2d 479,
484-85 (5th Cir. June 1993). The court relied on Hunt v. Washington Apple Advertising Commission,
432 U.S. 333 (I9n), in which the Supreme Court held that a trade group has associational standing to
sue when: (a) its members would otherwise have standing to sue in their own right; (b) the interests it
seeks to protect are gennane to the organization's purpose; and (c) neither the claim asserted nor the
relief requested requires the participation of individual members in the lawsuit. Korioth, 993 F.2d at 484
(citing Hunt, 432 U.S. at 343). The court also relied on Data Processing Service Organization v. Camp,
in which the Supreme Court held that "a plaintiff that seeks standing to maintain an action alleging
violations of a federal statute must: (i) suffer injury in fact; and (ii) fall within the zone of interest
protected by the statute." Id. (relying on Camp, 397 U.S. 150 (1970». The Fifth Circuit held that the
association's members had been affected by article 21.07-6 and were within ERISA's zone of interests.
Id. The court noted that because the association's members were considered fiduciaries under Texas law,
they constituted an enumerated party under section 502. Id. The court held that the trade association
had associational standing to bring the case. Id. at 484-85.
146. 996 F.2d 105 (5th Cir. July 1993).
147. Id. at 106.
148. Id.
149. Id.
HeinOnline -- 26 Tex. Tech L. Rev. 592 1995
1995]
EMPLOYEE BENEFITS
593
medical history and discovered some discrepancies between her medical
history and her insurance enrollment fonns. ISO Pacific denied her claims
and retroactively cancelled the policy, alleging that misrepresentations were
made on the enrollment fonn. lsl Tingle sued. ls2
The Fifth Circuit held that ERISA preempts a Louisiana state law that
allows an insurer to refuse payment because of a false statement in an
application fonn if the statement was made with actual intent to deceive or
to materially affect acceptance of risk or hazard assumed by the insurer. ls3
The court held that the statute did not fall within ERISA's insurance savings
clause, and, therefore, was preempted. lS4
The court looked at the two-pronged test set forth in Metropolitan
1SS
Life.
The court held that because the statute did not have the effect of
spreading policyholders' risks, it did not meet the first prong of the test. IS6
The court noted that "[a]lthough the statute does shift the burden of
innocent misrepresentations (the legal risks) onto the insurer, it does not
spread the risk of insurance (health) coverage for which the parties
contracted. "157 Therefore, the statute was preempted. 1S8
VII. RULE #6: DISCRIMINATION UNDER ERISA REQUIRES SPECIFIC
INTENT BY THE EMPLOYER TO INTERFERE WITH ERISA BENEFITS
Section 510 of ERISA prohibits an employer from discharging,
expelling, or discriminating "against a participant ... for the purpose of
interfering with the attainment of any right to which such participant may
become entitled under the plan .... ' '159 The Fifth Circuit has frequently
held that although an employer's conduct might appear to be discriminatory,
it is not discriminatory per se simply because it adversely affects a class of
participants or because it is motivated by the employer's desire to cut costs
under the plan. 160 For example. in McGann v. H & H Music CO.,161 the
Fifth Circuit held that an employer did not violate section 510 when it
150. Jd.
151. Jd.
152. Jd.
153. Jd. at 108; see LA. REv. STAT. ANN. § 22:619 (West 1978 & Supp. 1994).
154. Tingle, 996 F.2d at 108.
155. Jd. at 107-09.
156. Id. at 108.
157. Id.
158. Id.
159. 29 U.S.C. § 1140 (1988).
160. But see Stephen Allen Lynn, P.e. Employee Profit Sharing Plan & Trost v. Stephen Allen
Lynn, P.C., 25 F.3d 280, 284 (5th Cir. 1994) (holding that across-the-board plan amendments that
prevented a sole proprietor's estranged wife from becoming a beneficiary violated section 510).
161. 946 F.2d 401 (5th Cir.), cerro denied, _
U.S. _ ' 113 S. CL 482, 121 L. Ed. 2d 387
(1992).
HeinOnline -- 26 Tex. Tech L. Rev. 593 1995
594
TEXAS TECH LAW REVIEW
[Vol. 26:579
reduced medical benefits for participants with AIDS.162 The court noted
that in enacting ERISA, Congress did not require the vesting of medical
benefits so as to encourage employers to create medical plans. 163 Furthermore, the court held that section 510 requires proof of specific intent to
discriminate against the plaintiff, rather than general allegations that the
employer's action adversely affected a particular class of participants!64
Later, in Unida v. Levi Strauss & CO.!6S the Fifth Circuit held that an
employer's decision to close a plant to avoid increased employee benefits
costs was not sufficient to prove that the employer violated section 510 of
ERISA. 166
This term, in Perdue v. Burger King Corp., the Fifth Circuit reiterated
that specific intent is required to prove discrimination under ERISA. I67
In April 1989, Burger King Corporation ("BKC") eliminated several
management tiers including all Franchise Area Manager positions.168 At
the same time, BKC created the Burger King Job Elimination Program, a
severance plan that offered severance benefits to "any full-time employee
who loses his job as a result of a job elimination plan or reduction in a
workforce."169 Perdue, a Franchise Area Manager, was given the option of
either staying on with BKC as a Franchise Operations Manager or receiving
a severance benefit under the program.170 He decided to remain with
BKC and become the Franchise Operations Manager. l71
At the time Perdue switched positions, he owed BKC $1,000 for
unused travel advances. 172 He contacted the BKC accounting department
and advised them that Bushey, the regional operations vice president, had
authorized an extension until September for the repayment of travel
funds. 173 When the accounting department contacted Bushey for verification, he said that he had not authorized an extension. 174 Bushey and
Perdue met to discuss the advance on July 31, 1989. 175 Perdue denied
telling the accounting office that an extension had been authorized. 176 He
told Bushey that he had called the accounting office to tell them that he was
162. /d. at 408.
163. /d. at 407 (citing Moore v. Metropolitan Life Ins. Co., 856 F.2d 488. 492 (2d Cir. 1988)).
164. /d. at 408.
165. 986 F.2d 970 (5th Cir. 1993).
166. /d. at 980.
167. 7 F.3d 1251. 1255 (5th Cir. Dec. 1993).
168. /d. at 1252.
169. /d.
170. /d.
171. /d. at 1252-53.
172. /d. at 1253.
173. /d.
174. /d.
175.
/d.
176. /d.
HeinOnline -- 26 Tex. Tech L. Rev. 594 1995
1995]
EMPLOYEE BENEFITS
595
unable to obtain an extension. 177 Bushey, no longer believing that Perdue
was trustworthy, terminated Perdue. 178
Perdue requested severance benefits. 179 BKC denied benefits because
the termination was not the result of a reduction in force or a job elimination program. 180 Perdue sued, alleging, among other things, that BKC
violated section 510 of ERISA by inducing him to accept the Franchise
Operations Manager position and then terminating him under the pretext of
just cause. 181 More specifically, Perdue alleged "that the misunderstanding
surrounding the travel advance provided the pretext for terminating Perdue's
employment ,,182 The district court refused "to consider [the] 'suspect'
circumstances surrounding his termination," and Perdue appealed. 183
The Fifth Circuit rejected Perdue's claim. l84 The court noted that
section 510 of ERISA "is concerned with acts taken against employees to
prevent rights from ripening. The prohibitions under the statute do not
extend per se to an employer who retains an employee so as to avoid
payment of severance benefits under an ERISA plan.' ,185
The court held that under ERISA section 510, a plaintiff is "required
to demonstrate that the employer discharged the claimant 'with the specific
intent of interfering with ... ERISA benefits." ,186 The court held that
BKC did not violate ERISA section 510 for two reasons. First, Perdue
offered no evidence that Bushey either induced Perdue to accept the other
position or terminated his employment "with the specific intent of
interfering with Perdue's attainment of rights under the Program.,,187
Second, at the time that Perdue was terminated, he no longer had any rights
under the Severance Program because he had accepted another position with
BKC. 188
177. [d.
178. [d.
179. [d.
180. [d.
181. [d.
182. [d.
183. [d.
184. [d.
185. [d.
186. [d.
at 1255.
at 1255 n.lI.
at 1255.
(citations omitted).
(citing Simmons v. Willcox. 911 F.2d 1077. 1081-82 (5th Cir. 1990); Clark v.
Resistoflex Co.• 854 F.2d 762. 770 (5th Cir. 1988)).
187. Perdue. 7 F.3d at 1255.
188.
[d.
HeinOnline -- 26 Tex. Tech L. Rev. 595 1995
596
TEXAS TECH LAW REVIEW
[Vol. 26:579
VIII. RULE #7: ONLY PARTICIPANTS, BENEFICIARIES, AND FIDUCIARIES,
BUT NOT INTENDED BENEFICIARIES, HAVE STANDING TO SUE UNDER
ERISA
Section 502 of ERISA grants participants, beneficiaries, fiduciaries, and
the Department of Labor standing to sue to redress a violation of ERISA.189
Participants,190 beneficiaries,191 and fiduciaries l92 are carefully defined
in ERISA and are identified as possible plaintiffs. The Fifth Circuit has
been reluctant to expand section 502 beyond this list of enumerated
plaintiffs.
In Coleman v. Champion International Corp.,193 the Fifth Circuit held
that a self-professed "intended beneficiary" (Coleman) did not have
standing to sue his father's (Charlie Coleman) pension fund to change the
type of retirement benefit his father was scheduled to receive at retirement. 194 Charlie Coleman reached age 55, early retirement age under the
plan, in July of 1986. 195 Charlie Coleman died the following March. 196
At the time of his death, Charlie Coleman was divorced. 197 He had not
remarried. 198 He was no longer employed by Champion International and
was entitled at any time to elect to start receiving his pension.199 Under
the plan, he could elect various optional forms of payments such as a tenyear certain, which would guarantee that he would receive benefits for his
lifetime.2oo However, if he died before ten years had elapsed, the payment
for the remaining years would be paid to a designated beneficiary.201
189. 29 U.S.C. § 1132(a)(I)-(5) (1988 & Supp. V 1993).
190. ERISA section 3(7) defines a participant as an "employee or former employee of an
employer, or any member or former member of an employee organization, who is or may become
eligible to receive a benefit of any type from an employee benefit plan which covers employees of such
employer or members of such organization, or whose beneficiaries may be eligible to receive any such
benefiL" 29 U.S.C. § 1002(7) (1988).
191. ERISA section 3(8) defines a beneficiary as "a person designated by a participant. or by
the terms of an employee benefit plan, who is or may become entitled to a benefit thereunder." 29
U.S.C. § 1002(8) (1988).
192. Under ERISA section 3(21), "a person is a fiduciary with respect to a plan to the extent (i)
he exercises any discretionary authority or discretionary control respecting management of such plan or
exercises any authority or control respecting management or disposition of its assets, (ii) he renders
investment advice for a fee or ... other property of such plan, or has any authority or responsibility to
do so, or (iii) he has any discretionary authority or discretionary responsibility in the achninistration of
such plan." 29 U.S.C. § lOO2(21)(A) (1988).
193. 992 F.2d 530 (5th Cir. June 1993).
194. ld. at 534.
195. ld. at 532.
196. ld.
197. ld..
198. ld.
199. ld.
200. ld.
201. ld.
HeinOnline -- 26 Tex. Tech L. Rev. 596 1995
1995]
EMPLOYEE BENEFITS
597
Charlie Coleman did not elect any optional form of payment, such as a tenyear certain, and he did not designate a beneficiary to receive benefits under
an optional form of payment. 202 Instead, he would receive a lifetime
annuity by default, with payments to begin once he retired. 203
The pension plan provided that if an unmarried terminated vested
participant, such as Charlie Coleman, died before he started receiving
benefits, the plan would pay no pension benefits.204 When Charlie
Coleman died, no benefits were paid, and his son sued to recover his
father's benefits?05
The court noted that the son clearly was not a participant or fiduciary
as defined by ERISA. 206 Coleman's only chance to establish standing
would be if he could prove he was a beneficiary under ERISA. 207 ERISA
section 3(8) defines "beneficiary" as "a person designated by a participant,
or by the terms of any employee benefit plan, who is or may become
entitled to a benefit thereunder.' ,208 Coleman did not satisfy this defInition because his father had not designated him as a beneficiary and the plan
did not name him as a beneficiary.209 Coleman argued that if the plan had
advised his father that his pension benefits would be forfeited unless he
selected an optional form of benefit, Charlie Coleman would have designated his son as his beneficiary.210 The court described this argument as
"speculative at best. "211 The court said: "[W]e do not agree that the
mere possibility that one could potentially have been named beneficiary is
sufficient to confer status under" section 502. 212
The plan defmed "beneficiary" as "anyone or more of the persons
comprising the group consisting of the participant's spouse, the participant's
descendants, the participant's parents or the participant's heirs at law ... of
. . . the estate of such deceased participant. . . .' ,213 The court rejected
Coleman's argument that because he was "Charlie Coleman's descendant,
heir at law, and the representative of Charlie Coleman's estate," he was a
beneficiary' under section 502. 214 The court explained that under the plan,
a Retirement Committee could designate a beneficiary from the group of
possible beneficiaries only if at the time of the participant's death, death
202.
203.
204.
205.
206.
2CY7.
208.
209.
210.
211.
212.
213.
214.
Jd.
Jd.
Jd.
Jd.
Jd. at 533.
Jd.
29 U.S.C. § 1002(8) (1988).
Coleman, 992 F.2d at 533.
Jd. at 533 n.6.
Jd.
Jd.
Jd. at 533.
Jd.
HeinOnline -- 26 Tex. Tech L. Rev. 597 1995
TEXAS TECH LAW REVIEW
598
[Vol. 26:579
benefits were payable and the participant had failed to elect an alternate
payment option and had failed to name a beneficiary.2lS However,
because no benefits were payable at the time of Charlie Coleman's death,
the Retirement Committee was not authorized to name a beneficiary from
the liSt.216 Therefore, Coleman was not a beneficiary as defined by
ERISA and had no standing to sue,217
The court refused to expand the section 502 list of enumerated
plaintiffs, citing its previous holding that •• [w]here Congress has defined the
parties who may bring a civil action founded on ERISA, we are loathe to
ignore the legislature's specificity. Moreover, our previous decisions have
hewed to a literal construction of [section 502(a)]. ,,218 The court held that
"[a]bsent clear Congressional expression that non-enumerated parties such
as the appellant have standing to sue under ERISA, we decline to confer
such standing.' ,219
The court distinguished Christopher v. Mobil Oil COrp.,220 where the
court "restored ERISA standing to individuals who once had standing but
were divested of that standing because of the ERISA violations of their
employer, ,,221 In Christopher, a group of employees alleged that their
employer had wrongfully induced them to retire and that but for this
inducement they would have remirined participants and would have retained
standing to sue?22 The court noted in Coleman that "Coleman never had
standing to sue under ERISA since he was neither a plan participant nor a
beneficiary. ,,223 Thus, Christopher was not controlling. 224
215.
216.
217.
218.
Id.
Id. at 534.
Id.
Id. (citing Jamail. Inc. v. Ca!penters Dist. Council of Houston Pension & Welfare Trosts,
954 F.2d 299,302 (5th Cir. 1992); Hennann Hosp. v. MEBA Medical & Benefits Plan. 845 F.2d 1286,
1289 (5th Cir. 1988». In Yancy v. American PetrojifID, Inc., the court refused to grant standing to a
plaintiff who did not meet the statutory definition of "participant.' , 768 F.2d 7m, 708 (5th Cir. 1985);
see also Joseph v. New Orleans Elec. Pension & Retirement Plan, 754 F.2d 628,630 (5th Cir.) (holding
that plaintiffs lacked standing because they were not "participants" within the meaning of ERISA), cert.
denied, 474 U.S. 1006 (1985).
219. Coleman, 992 F.2d at 534.
220. 950 F.2d 1209 (5th Cir.), cerl. denied, _ U.S. --J 113 S. Ct. 68, 121 1.. Ed. 2d 35 (1992).
221. Coleman, 992 F.2d at 535.
222. Id. In Firestone Tire & Rubber Co. v. Bruch, the Supreme Court held that the tenn
"participant" in section 502 referred to "fonner employees who 'have ... a reasonable expectation of
retuming to covered employment' or who have a 'colorable claim' to vested benefits." 489 U.S. 101,
118 (1989). In Christopher, the Fifth Circuit stated that "it would seem ... logical to say that but for
the employer's amduct alleged to be in violatioo of ERISA, the employee would be a current employee
with a reasonable expectation of receiving benefits, and the employer should not be able through its own
malfeasance to defeat the employee's standing." 950 F.2d at 1221.
223. Coleman, 992 F.2d at 535.
224. Id.
HeinOnline -- 26 Tex. Tech L. Rev. 598 1995
1995]
EMPLOYEE BENEFITS
599
IX. RULE #8: UNDER MOST PLANS, THE PLAN ADMINISTRATOR WILL
HAVB DISCRETIONARY AUTHORITY TO CONSTRUE THE TERMS OF THE
PLAN, AND THEREFORE, THE STANDARD OF REVIEW WILL BE ABUSE OF
DISCRETION
.
In Firestone Tire & Rubber Co. v. Bruch,22S the Supreme Court
articulated the standard of review for a denial of employee benefits:
[A] denial of benefits challenged under § [502](a)(1)(B) is to be reviewed
under a de novo standard unless the benefit plan gives the administrator
or fiduciary discretionary authority to detennine eligibility for benefits or
to construe the tenns of the plan. . . . Of course, if a benefit plan gives
discretion to an administrator or fiduciary who is operating under a
conflict of interest, that conflict must be weighed as a "facto[r] in
detennining whether there is an abuse of discretion." 226
To avoid the uncertainty and expenses involved in de novo review, most
plans give the plan administrator discretionary authority to construe the
plan's terms.
The Fifth Circuit consistently applies a two-part test to determine if a
plan administrator has abused his or her discretion.227 First, the court
determines whether the administrator's decision was "legally correct...228
To determine if the decision was legally correct, the court considers three
factors: (1) whether the plan administrator has uniformly construed the
plan; (2) whether the administrator's interpretation of the plan is consistent
with a fair reading of the plan; and (3) whether the administrator's
interpretation results in any unanticipated costs.229
If the court determines that the administrator's interpretation of the plan
is legally incorrect, the court must then decide whether the administrator
abused its discretion. no Under the second step of the two-part test, the
court considers the following factors in determining if the administrator
abused its discretion: "(1) whether the [administrator's] interpretation is
internally consistent with the remainder of the plan; (2) whether the
[administrator's] interpretation comports with any relevant regulations
formulated by appropriate administrative agencies; (3) whether the factual
225.
489 U.s. 101 (1989).
226. Id. at 115.
227. The Fifth Cirroit has held that this two-part test is not required in every case. See Duhon
v. Texaco. Inc.• 15 F.3d 1302. 1306 (5th Cir. Feb. 1994). For example, in Duhon, the administrator
clearly did not abuse his discretion; thus, the two-part analysis was unnecessary. Id. at 1307 n.7.
228. Jones v. Sonat Inc. Master Employee Benefits Plan Admin. Comm.• 997 F.2d 113 (5th Cir.
Aug. 1993).
229. Id. at 115; see Wildbur v. ARCO Oem. Co., 974 F.2d 631, 637-38 (5th Cir. 1992); Jordan
v. Cameron Iron Works, Inc., 900 F.2d 53, 56 (5th Cir.). cert. denied. 498 U.S. 939 (1990).
230. SOMt Inc.• 997 F.2d at 116.
HeinOnline -- 26 Tex. Tech L. Rev. 599 1995
600
TEXAS TECH LAW REVIEW
[Vol. 26:579
background supports the [administrator's] detennination; and (4) any
inferences of lack of good faith on the [administrator's] part .. 231
Where a potential conflict of interest exists between the plan and the
participant, the court will scrutinize the decision more carefully: a review
will be "more penetrating the greater ... the suspicion of partiality, [and]
less penetrating the smaller that suspicion.' ,232
Duhon v. Texaco, Inc. 233 presented the Fifth Circuit with "a rather
typical question pertaining to ERISA benefits:" a claim that benefits were
improperly denied. 234 Clifford Duhon was employed by Texaco Trading
and Transportation, Inc. until he became disabled. 235 He began receiving
benefits under Texaco's disability plan.236 Under the tenns of the plan,
Duhon would receive benefits for the first twenty-four months following his
separation from work if he was unable to perfonn the nonnal duties of his
regular job or a comparable one.237 After twenty-four months, disability
payments would cease if Duhon was .. able to perfonn any job for which he
[was, or had become,] qualified by training, education, or experience.,,238
After twenty-four months, Duhon was evaluated by three doctors to
detelIDine whether his disability benefits should continue. 239 Duhon's
family doctor concluded that Duhon was pelIDanently disabled from working
as a truck driver. 240 Texaco's doctor of choice agreed that Duhon was
pennanently disabled and that Duhon should not drive trucks or lift heavy
objects.241 The third doctor, an orthopedist selected by Texaco, concluded
that Duhon had degenerative lumbar disc disease and that Duhon could not
"squat, stoop, bend, or lift more than twenty-five pounds... 242 The
orthopedist agreed that Duhon could not wort as a truck driver but said that
Duhon could do "sedentary to light wort... 243
Texaco's plan administrator and chief medical officer reviewed
Duhon's medical records and decided that Duhon was no longer eligible for
disability benefits. 244 Duhon's appeal, challenging the denial of benefits,
231.
232.
denied. 493
233.
234.
235.
236.
237.
238.
239.
240.
241.
242.
243.
244.
Jd.; see Wildbur. 974 F.2d at 638.
Lowry v. Bankers Life & Casualty Retirement Plan. 871 F.2d 522. 525 n.6 (5th Cir.). cerro
U.S. 852 (1989).
15 F.3d 1302 (5th Cir. Feb. 1994).
Jd. at 1304.
Jd.
Jd.
Jd.
Jd.
Jd.
Jd.
Jd.
Jd.
Jd.
Jd.
HeinOnline -- 26 Tex. Tech L. Rev. 600 1995
1995]
EMPLOYEE BENEFITS
601
was denied. 245 Duhon then sued Texaco and the plan administrator. 246
The trial court ordered Texaco to continue paying the disability benefits.247
Texaco appealed. 24s
Because the plan granted discretionary authority to the Texaco plan
administrator,249 the Fifth Circuit held that the administrator's decision was
subject to review under the abuse of discretion standard.250 The court
declined to follow the elaborate two-prong test adopted in Wildbur v. ARCO
Chemical CO.,251 stating that the test was not required in a case such as
Duhon's where the administrator clearly did not abuse his discretion. 252
The court rejected Duhon's argument that the administrator abused his
discretion by interpreting the plan language "any job for which he ... is or
may become qualified" to include any job that required only "sedentary to
light work" for which Duhon was otherwise qualified. 253 Duhon argued
that no evidence had been presented that "he [could] actually perfonn any
identifiable job.,,254 The court stated that:
It was not an abuse of discretion for the pIan administrator to conclude
that a sixty-five year old man with a high school diploma and plenty of
experience in the work-a-day world, although unable to squat, stoop, bend,
or lift more than twenty-five pounds, would be able to perform the
functions of some identifiable job. Indeed, to fmd otherwise would be
blindly and deliberately to ignore a common-and uncontested-truth:
people in their sixties and seventies who have similar physical and job
limitations ... are employed and employable throughout the workplace
today.2.5S
Next, the court considered whether the plan administrator abused his
discretion by denying benefits without obtaining the expert testimony of a
vocational rehabilitation expert to detennine if Duhon was capable of
perfonning other work. 256 The court refused to burden plan administrators
with a rule that would require them to consider vocational rehabilitation
245. Id.
246. Id.
247. The Fifth Circuit held that the trial court's award of disability benefits was emmeous. Id.
at 1309 n.7. The trial court should have remanded "the case to the plan administrator with instructions
to take additional evidence." Id.
248. Id.
249. The plan stated that "[t]he decisions of the Plan Administrator shall be final and conclusive
with respect to every question which may arise relating to either the interpretation or administration of
this Plan." Id. at 1305.
250.
Id.
251.
974 F.2d 631 (5th Cir. 1992).
Duhon, 15 F.3d at 1307.
252.
253. Id.
254. Id.
255. Id. at 1308.
256. Id.
HeinOnline -- 26 Tex. Tech L. Rev. 601 1995
602
TEXAS TECH LAW REVIEW
[Vol. 26:579
evidence to avoid an abuse of discretion charge.2S7 Instead, the court
determined that a case-by-case examination should be conducted to
determine whether a plan administrator abused its discretion by failing to
obtain the opinion of a vocational rehabilitation expert.2S8
The court concluded that in Duhon's case the plan administrator did not
abuse its discretion by failing to obtain the opinion of a vocational rehabilitation expert. 2S9 The court noted that "[g]iven ... [the] undemanding [plan]
language and the medical evidence in this case, the plan administrator could
competently determine disability without vocational testimony.' '260
Judge Johnson dissented. 261 He criticized the majority for avoiding
the real issue: Whether the plan administrator was required to ·specifically
determine if Duhon was qualified or could become qualified to perform a
job.262 Judge Johnson also criticized the majority for not analyzing the case
under the Wildbur two-step test. 263 He noted that the "application of the
two-step process in plan-interpretation cases is mandatory.' ,264 Judge
Johnson argued that Texaco had failed to meet its burden of proving that
Duhon "[was, or had become,] qualified [to perform a job] by training,
education. or experience.' ,265 Applying the first part of the two-step test,
Judge Johnson concluded that Texaco's deletion of this qualification
requirement was" anything but a •fair reading' of the plan. ,,266 Specifically,
Judge Johnson explained that Texaco's interpretation of the plan was
"anything but reasonable," as it ignored the plan's requirement that the
participant must either be capable of performing a job or have the ability to
become qualified to perform a job.267 Judge Johnson noted:
[W]hile it is true that Mr. Duhon is a high school graduate, the fact of the
matter is that many moons have passed since his graduation in 1947.
Nothing in the record reveals that Mr. Duhon ever used or honed any of
the skills he gained in school - whether reading, writing, or otherwise. 268
Therefore, Judge Johnson disagreed with the majority's conclusion that the
administrator did not abuse his discretion. 269
257.
258.
259.
260.
[d. at 1309.
[d.
[d.
[d.
261. [d. at 1310 (Johnson., J., dissenting).
262. [d.
263. [d. at 1310-11.
264.
265.
266.
267.
268.
[d. at 1310.
[d. at 1311.
[d.
See id. at 1312.
[d. at 1313.
269. [d.
HeinOnline -- 26 Tex. Tech L. Rev. 602 1995
1995]
EMPLOYEE BENEFITS
603
Under Firestone, if the plan does not give the administrator discretionary
authority, the court must review the administrator's decision de novo. 270
In Ramsey v. Colonial Life Insurance Co. of America,271 the court reviewed
the administrator's denial of benefits de novo because the plan did not give
the administrator discretion. 272
William Ramsey, Jr. was paralyzed from the neck down. 273 He was a
dependent under his wife's medical plan. 274 After receiving coverage under
this plan for two and a half years, the insurer discontinued coverage.275
Ramsey sued.276
The court interpreted the policy to require the insurer to continue
Ramsey's medical coverage.277 The court noted that the plan language
was clear, but even if it was ambiguous, any ambiguity would be construed
in favor of the insured under the doctrine of contra proferentem.278 The
court reiterated that:
Any burden of uncertainty created by careless or inaccurate drafting of the
summary must be placed on those who do the drafting, and who are most
able to bear that burden, and not on the individual employee, who is
powerless to affect the drafting of the summary or the policy and ill
equipped to bear the fmandal hardship that might result from a misleading
or confusing document. 279
The court construed any ambiguities against the insurer and held that
Ramsey was entitled to continued medical coverage.280
X. RULE #9: FACTUAL DETERMINATIONS BY A PLAN ADMINISTRATOR
ARE REVIEWED FOR ABUSE OF DISCRETION REGARDLESS OF PLAN
LANGUAGE
In Southern Farm Bureau Life Insurance Co. v. Moore,281 the Fifth
Circuit noted that in Firestone, the Supreme Court did not address the
applicable standard for review of a factual determination made by a plan
270.
271.
272
Firestone Tire & Rubber Co. v. Broch, 489 U.S. 101. 115 (1989).
12 F.3d 472 (5th Cir. Jan. 1994).
[d. at 478.
[d. at 473.
273.
274. [d.
275. [d.
276. [d.
277.
[d. at 479.
278. [d.; see Hansen v. Continental Ins. Co.• 940 F.2d 971, 982 (5th Cir. 1991); cf. Wise v. El
Paso Natural Gas Co., 986 F.2d 929, 938 (5th Cir. 1993) (stating that rules of constNctiOll announced
in Hansen "mandate that we adopt the most pro-beneficiary interpretation' .), cert. denied, _ U.S._,
114 S. Ct. 196, 126 L. Ed. 2d 154 (1993).
279. Ramsey, 12 F.3d at 479 (quoting Hansen, 940 F.2d at 982).
280. [d.
281.
993 F.2d 98 (5th Cir. June 1993).
HeinOnline -- 26 Tex. Tech L. Rev. 603 1995
604
TEXAS TECH LAW REVIEW
[Vol. 26:579
administrator. 282 In Pierre v. Connecticut General Life Insurance CO.,283
the Fifth Circuit held that an administrator's factual detennination should be
reviewed for abuse of discretion. 284 Under ERISA, a plan administrator
is a fiduciary.28S As a fiduciary, the administrator "possesses inherent
discretion through a statutory grant of authority to control and manage the
operation of the plan.' ,286 This result avoids the potential problem of
courts "supplant[ing] plan administrators, through de novo review, as
resolvers of mundane and routine fact disputes.' ,287
Applying Pierre, the Fifth Circuit ruled in Moore that the district court
erred in reviewing de novo the plan administrator's factual detenninations. 288 Not only may the court consider "the evidence that was available to the plan administrator" in evaluating the administrator's factual
detenninations, but the court also may consider additional evidence that was
not available to the administrator in reviewing the plan administrator's
interpretation of the plan. 289
The court looked to Texas law to detennine whether the plan administrator's refusal to pay accidental death benefits to Mrs. Moore was
proper.290 The plan excluded coverage for death that resulted from or was
contributed to by a disease or infinnity of the body.291 Southern Farm
Bureau denied benefits to Mrs. Moore, claiming that her husband's death in
an automobile wreck was caused by loss of consciousness triggered by a
brain tumor. 292
The court held that the administrator did not abuse his discretion when
he detennined, on the basis of three medical reports, the autopsy report, a
newspaper article, and the death certification, that the brain tumor, a bodily
disease, caused or contributed to Mr. Moore's death. 293 The court held
282. /d. at 100.
283. 932 F.2d 1552 (5th Cir.). cert. denied, _ U.S. _ ' 112 S. a. 453. 116 L. Ed. 2d 470
(1991).
284. /d. at 1562.
285. 29 C.F.R. § 2509.75-8(0-3) (1993).
286. Moore, 993 F.2d at 101.
287. /d.
288. /d. The trial court applied a de novo standard of review because the administrator did not
notify the claimant that the claim had been denied. /d. The Fifth Circuit noted that Department of Labor
regulations provide that if a claim is not denied, it will be deemed denied. /d. (referring to 29 C.F.R. §
2560.503-1(h)(l),(4». The Fifth Circuit held that the standard is the same regardless of whether the
claim is actually denied or deemed denied. /d. The Fifth Circuit reviewed the administrator's factual
detennination under an arbitrary and capricious standard. /d.
289. /d. at 102. The court also noted that under Firestone, since the plan administrator apparently
did not have discretionary authority to interpret the plan, the plan administrator's interpretation of the
plan should be reviewed de novo. /d. at 101.
290. /d.
291. /d.
292 /d. at 100.
293. /d. at 103.
HeinOnline -- 26 Tex. Tech L. Rev. 604 1995
1995]
EMPLOYEE BENEFITS
605
that this evidence was sufficient to support the plan administrator's
detennination that the accident was a result of Mr. Moore's brain tumor.294
XI. RULE #10: ADVISORS WHO Do NOT HAVE AUTHORITY AND
CONTROL OVER PLAN ASSETS AND WHO Do NOT RENDER REGULAR
INVESTMENT ADVICE TO THE PLAN ARE NOT FIDUCIARIES
In Sch/oege/ v. Boswe//,295 the Fifth Circuit held that an insurance
agent who purchased life insurance on behalf of a pension plan was not a
fiduciary.296 In 1977, Boswell, an insurance agent, purchased two ordinary
life insurance policies insuring the life of a plan participant. 297 The plan
paid insurance commissions for ten years until the plan realized that the
insurance policies violated the Internal Revenue Code,298 which requires
death benefits to be •• incidental" to the primary purpose of providing
retirement benefits.299 The plan cashed in the insurance policies and sued
Boswell for breach of fiduciary duties under ERISA. 300
ERISA section 3(21)(A) provides that a person is a fiduciary with
respect to the plan:
to the extent (i) he exercises any discretionary authority or discretionary
control respecting management of such plan or exercises any authority or
control respecting management or disposition of its assets, (ii) he renders
investment advice for a fee or other compensation, direct or indirect, with
respect to any moneys or other property of such plan, or has any authority
or responsibility to do so, or (iii) he has any discretionary authority or
discretionary responsibility in the administration of such plan?01
The plan argued that Boswell had effective control over the plan's
investments because the trustee relied on Boswell's expertise and long-term
relationship with the plan in deciding to purchase the life insurance.302
294.
295.
(1993).
[d.
994 F.2d 266 (5th Cir. July), cert. denied, _
U.S. _, 114 S. Ct. 440, 126 L. Ed. 2d 374
296. [d. at 273.
297. [d. at 269.
298.
Treas. Reg. § 1.401-1(b)(1)(ii) (1993).
299. Boswell, 994 F.2d at 270.
300. [d. at 268.
301. 29 U.S.C. § lOO2(21)(A) (1988).
302. ERISA's legislative history provides:
While the ordinary functions of consultants and advisers to employee benefit plans (other than
investment advisers [which are covered in subsection (ii) of the applicable statutory
definitionl) may not be considered as fiduciary functions, it must be recognized that there will
be situations where such consultants and advisers may because of their special expertise, in
effect, be exercising discretionary authority or control with respect to the management or
administration of such plan or some authority or control regarding its assets. 10 such cases,
they are to be regarded as having assumed fiduciary obligations within the meaning of the
applicable defmition.
HeinOnline -- 26 Tex. Tech L. Rev. 605 1995
606
TEXAS TECH LAW REVIEW
[Vol. 26:579
The court noted that although a court may look at a professional service
provider to detennine if the professional exceeded the scope of his ordinary
functions, "mere influence over the trustee's investment decisions, however,
is not effective control over plan assets.' ,303 More than just urging the
purchase of insurance products is required: "To satisfy the 'authority or
control' element under [ERISA section 3(21)(i)], the Plaintiffs must
demonstrate that Boswell caused trustee Eastland to relinquish his independent discretion in investing the plan's funds. ,,304 The court concluded that
"Boswell made an investment proposal, not an investment decision.' ,30S
Next, the court detennined that Boswell did not fall within the
definition of fiduciary described in ERISA section 3(21)(ii) as a person who
gives investment advice. 306 Under Department of Labor regulations,
Boswell would have been a fiduciary if he met two conditions: (1) he made
recommendations as to the purchase or sale of property, and (2) either (a)
he had discretionary control or authority with respect to purchasing property
for the plan or (b) he rendered individualized investment advice based on
the particular needs of the plan on a regular basis to the plan pursuant to a
mutual agreement that such advice would serve as the primary basis for the
plan's investment decisions. 307
The court held that the first requirement of the Department of Labor
regulation was met since Boswell "made recommendations as to the
advisability of purchasing life insurance. ' ,308 However, the second
H.R. CONF. REp. No. 1280, 93d Cong., 2d Sess. 323 (1974), reprinted in 1974 U.S.C.C.A.N. 5038, 5103.
303. Boswell, 994 F.2d at 271; see American Fed'n of Unions Local 102 Health & Welfare Fund
v. Equitable Life Assurance Soc'y of the United States, 841 F.2d 658, 664 (5th Cir. 1988).
304. Boswell, 994 F.2d at 271.
305. Id. at 272.
306.
Id.
307. 29 C.F.R. § 251O.3-21(c)(1) (1993) provides:
A person shall be deemed to be rendering "investment advice" to an employee benefit plan,
within the meaning of [29 U.S.C. § lOO2(21)(A)(ii)), only if:
(i) Such person renders advice to the plan as to the value of securities or other property, or
makes recommendation as to the advisability of investing in, purchasing, or selling securities
or other property; and
(ii) Such person either directly or indirectly (e.g., through or together with any affiliate}(A) Has discretionlllY authority or control, whether or not pursuant to agreement, arrangement
or understanding, with respect to purchasing or selling securities or other property for the
plan; or
(B) Renders any advice described in paragraph (c)(I)(i) of this section on a regular basis to
the plan pursuant to a mutual agreement, arrangement or IDIderstanding, written or otherwise,
between such person and the plan or a fiducilllY with respect to the plan, that such services
will serve as a primlllY basis for investment decisions with respect to plan assets, and that
such person will render individualized investment advice to the plan based on the particular
needs of the plan regarding such matters as, among other things, investment policies or
strategy, overall portfolio composition, or diversification of plan investments.
Id.
308.
Boswell, 994 F.2d at 272.
HeinOnline -- 26 Tex. Tech L. Rev. 606 1995
1995]
EMPLOYEE BENEFITS
607
requirement was not met because Boswell did not have discretionary
authority or control with respect to the plan's purchase of the life insurance
policies. 309 Moreover, Boswell did not render investment advice to the
fund on a regular basis and did not have an agreement that his advice
"would serve as the primary basis for the plan's investment decisions.'o3lo
The court noted that at trial, the trustee testified "that he did not 'seek
[Boswell] out and ask advice' but that, if Boswell approached him, he 'was
willing to listen.',,311 The court held that "[t]his falls far short of the type
of relationship described in the DOL Regulation.' ,312 Therefore, the court
concluded that Boswell was not a fiduciary.313
XII.
CONCLUSION AND FINAL
RULE
Sometimes, ERISA is confusing even to ERISA attorneys. When
ERISA issues seem overwhelming, take comfort in the thought that you are
probably not the only one who is confused. The final rule for non-ERISA
attorneys is: When ERISA matters get too complex or confusing, call an
ERISA attorney.
Good luck handling ERISA cases and have fun celebrating ERISA's
twentieth anniversary.
309.
310.
311.
312.
313.
Id. at 273.
Id.
Id.
Id.
Id.
HeinOnline -- 26 Tex. Tech L. Rev. 607 1995
j
j
j
j
j
j
j
j
j
j
j
j
j
j
j
HeinOnline -- 26 Tex. Tech L. Rev. 608 1995
j
j