I Q R
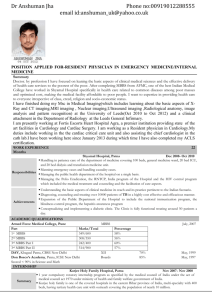
advertisement

UCL MEDICAL SCHOOL INTERNAL QUALITY REVIEW MBBS Self Evaluative Statement Contents Page Introduction 2 Educational Organisational Structures 2 1. STUDENTS, STAFF AND LEARNING RESOURCES 2 1.1 Student Profile 1.2 Student Profile Trends 1.3 Academic Staff Profile 1.4 Non-Academic Support Staff Profile 1.5 RAE Assessment 1.6 Learning Resources 2 3 6 7 7 7 2. QUALITY MONITORING & ENHANCEMENT FRAMEWORK 9 2.1 Student Input and Feedback 2.2 Staff Support 2.3 Recruitment and Reception of Students 2.4 Student Support 2.5 The Teaching Function and Process 2.6 Programme Design, Operation and Review 2.7 Assessment of Student Performance 10 10 12 13 14 15 18 3. SELF-ANALYSIS 21 3.1 Approach to Self-analysis 3.2 Historical Note 3.3 What the Students Say 3.4 Planning, Structure, Content and Assessment 3.5 Areas Supporting the MBBS Programme 3.6 Resources 3.7 Additional Areas of Good Practice 3.8 Summary – Change and Opportunity 21 21 22 23 25 26 26 27 MBBS IQR Document Register 29 MBBS Programme SES 2010 Introduction This Self Evaluative Statement (SES) follows the structure given in the Academic Manual guidelines found on the UCL IQR website, with reference to the Gold Book. Additional evidence to support statements made in this document are accessible through hypertext where possible or listed in the document register and available at: http://www.ucl.ac.uk/medicalschool/quality/priv This process runs in parallel with the professional regulatory requirement of the GMC which covers similar ground, albeit in a different format. These processes have coincided in 2010. We have incorporated a small amount of evidence prepared for the GMC return. However this entire report has been written exclusively for the IQR panel. In order to understand the MBBS programme and its regulation we advise the IQR panel to familiarise themselves with the requirements of the GMC and we would therefore be grateful if the panel would read, in conjunction with this document, the following: Tomorrow’s Doctors: Outcomes and standards for undergraduate medical education (2009) UCLMS GMC Enhanced Return 2010 (Part A & Part B and Annex 1) th UCLMS GMC Enhanced Return 2010 ((Part C and Annex 2)– to be posted on the website on 16 March 2010 (Panel members will be notified via Rob Traynor) Educational Organisational Structures IQR panel member may wish to be aware of the following documents that provide an overview of the MBBS programme administration. Organograms FBS Graduate and UG Programme Academic and Welfare Leads FBS MBBS Module and Assessment Leads FBS MBBS Teaching Committee and Sub Committees MBBS & Graduate Programme Management Manuals 1. 2. 3. 4. Management - leadership roles & responsibilities Committees - structure, remit & membership Exam Boards - policy, structure, remit & membership Administration - structure & responsibilities (31 pages) (32 pages) (35 pages) (15 pages) Panel members are also advised that useful supporting information is available on the following web pages: A-Z Policies and Regulations Medical School Administration: Service Standards 1. STUDENTS, STAFF AND LEARNING RESOURCES 1.1 Student Profile The profile of students is displayed in tables 1.2.1 and 1.2.2 The number of students admitted to the programme is determined by quotas for funding, nationally agreed with the Department of Health (the former Medical Workforce Standing Advisory Committee) which allow for: There are 330 students entering Year 1 of MBBS programme (Portico course UBMMEDSING01) of whom: approx 290 enrol on a 6 year programme which includes a compulsory iBSc either between years 2 and 3 or between years 3 and 4 approx 40 graduate entrants enrol on a 5 year programme with exemption from the iBSc SES IQR MBBS 2010 2 of 29 55 students transferring into Year 3 of the MBBS programme (block 4 of Portico UBMMEDSING01) from Oxbridge and completing a 3 year programme Up to 10 students registering for an MBPhD in any year and who are selected just prior to entry to Year 3 of A100 and who may include students who entered the 6 year programme, the 5 year programme, the 3 year programme, and up to 4 students each year who transfer into Year 3 from other medical schools. We have, therefore, 4 separate cohorts of students gaining the MBBS award each year, each of which entered at a different point and so currently appear in different entry statistics: Cohort Portico code UBMMEDSING01 Starting block UBMMEDSING01 Descriptor Approx no. of student entering i 6 year MBBS Block 1 290 ii 5 year MBBS Block 1 iii 3 year MBBS Block 4 iv 8 year MBPhD Block 1 and Block 4 School leaver entrants who take an intercalated BSc in block 3, 4, or 5 Graduate entrants taking a 5 year through-course (exempt from iBSc) Oxbridge transfers entering in Year 3 of MBBS (block 4) Students awarded a joint MBBS and PhD on completion of thesis can transfer back into cohort (i) or (ii) Max no. graduates per year 40 55 10 of whom up to 4 are new entrants to UCL 389 Entry qualifications A wide range of entry qualifications are accepted although the majority of students enter with A levels. From 2010, the standard academic offer will rise to AAA+, or IB 38+ points. It is hoped this will help to minimise early Entry qualification (entrants) 2006-7 (n=327) 2007-8 (n=327) 2008-9 (n=337) AAAA, AAAB, AABB, AAA Majority 201 235 AAAAAA 2 2 2 AAAAA 5 9 6 AAB 26 29 28 International Baccalaureate 10 13 22 (mean grade point 40) Graduate entrants: BA BSc Masters PhD 46 st 9 (1 x 1 , 8 x 2:1) st 27 (5 x 1 , 22 x 2:1) 9 1 48 0 st 33 (7 x 1 , 26 x 2:1) 10 2 29 0 st 23 (3 x 1 , 20 x 2:1) 5 1 attrition from the course. 1.2 Student Profile Trends The Medical School has identified certain trends regarding the profiles of applicants and students: There has been an increase in the following areas:(i) (ii) (iii) (iv) the number of applicants and students with disabilities; the number of entrants with dependants; the upper age of admitted students; the range of nationalities of applicants and students (all continents represented); There is also a progressing increase in the proportion of state school entrants (currently 62%), approaching their representation amongst applicants. There has been a reduction in the number of suitable graduate applicants and therefore a decline in the number of graduate entrants in the past two years. SES IQR MBBS 2010 3 of 29 1.2.1 Student Profile - Males Category Year 1 (09/10 entry) Application Intake With declared disability EU/UK Non-EU Total White British White Irish White Other Mixed - White & Black Caribbean Mixed - White & Black African Ethnicity Mixed - White & Asian Other Mixed Asian/Asian British - Indian Asian/Asian British - Pakistani Asian/Asian British - Bangladeshi Asian/Asian British - Other Asian Black/Black British - Caribbean Black/Black British - African Black/Black British – Black Other Chinese Any Other Not stated MBBS Male Current student numbers Year 2 Year 3 Year 4 Year 5 Year 6 31 1058 234 3 137 8 145 7 170 8 178 7 141 11 152 8 186 9 197 9 179 10 189 5 139 6 145 390 87 89 79 97 93 70 1 7 1 1 2 2 1 1 1 32 16 5 4 7 7 7 4 4 2 3 3 1 6 162 15 27 19 28 36 26 61 5 10 5 3 7 5 27 1 4 6 4 1 4 96 4 11 6 9 19 9 3 1 53 4 4 3 4 2 4 2 41 42 358 1 6 4 9 1 3 4 9 6 6 16 6 17 10 7 8 6 6 8 SES IQR MBBS 2010 4 of 29 1.2.2 Student Profile - Females Category Year 1 09/10 entry) Application Intake With declared disability EU/UK Non-EU Total White British White Irish White Other Mixed - White & Black Caribbean Mixed - White & Black African Ethnicity Mixed - White & Asian Other Mixed Asian/Asian British - Indian Asian/Asian British - Pakistani Asian/Asian British - Bangladeshi Asian/Asian British - Other Asian Black/Black British - Caribbean 31 1301 270 1571 Chinese Any Other Not stated Year 6 3 132 15 147 74 5 183 13 196 104 10 153 8 161 72 14 168 14 172 100 2 183 11 194 92 1 4 1 3 1 4 21 4 4 2 3 2 7 5 2 5 5 3 2 21 19 28 20 25 25 2 2 4 3 5 7 1 5 2 5 3 1 2 6 2 5 7 15 13 23 10 2 2 1 1 1 6 6 11 Black/Black British - African Black/Black British – Black Other 141 8 149 85 MBBS Female Current student numbers Year 2 Year 3 Year 4 Year 5 2 8 11 5 6 156 1 11 5 6 13 7 8 9 8 10 11 1 11 10 2 13 5 4 18 9 2 SES IQR MBBS 2010 5 of 29 Widening participation There is a range of widening participation initiatives specifically aimed at increasing diversity of applicants to the MBBS, reaching unrepresented groups and supporting non-traditional students once they arrive. These are described in the document: Widening Participation in the MBBS Programme. In summary, these include: Target Medicine; Dick Whittington Summer School: interview, BMAT and personal statement guidance and support; The Camden and Islington Tutoring Scheme; Use of head teachers in interviews; UCL Ambassadors; Public engagement projects: the Reel Film Festival, Open Minds, Sexpression, Saving London’s Lives; Financial resources; The student welfare system (disability and peer support). 1.3 Academic Staff Profile Leadership of MBBS programme The MBBS programme is led by the Vice Dean and Director of Medical Education (Professor Jane Dacre) who reports directly to the Vice Provost for Health, Professor Sir John Tooke. The programme is supported by a range of academics based in FLS and FBS, and NHS staff. No individual works exclusively for the programme. The majority of academic staff based in FBS are also practising NHS clinicians. The number of full-time equivalent staff with leadership roles in the programme is approximately 7 (mostly at senior lecturer or professor level) (see: document: 0910 MBBS Leadership PAs and Medical Student Admin for IQR. Division of Medical Education Leadership roles for, and management of, the MBBS programme are overseen by the Division of Medical Education (DoME) although DoME does not receive direct funding for the programme. The majority of leadership post holders are members of staff in other Divisions in SLMS or are NHS staff with sessional arrangements with the Medical School. DoME academic staff, however, do make a significant contribution to the programme. Estimates of their time dedicated to the MBBS programme are as follows: 0.6 FTEs for Professor Dacre, 0.5 FTEs for Professor David Bender (Sub Dean and Director of Studies, Phase1), 3.5 senior lecturer FTEs, 0.8 lecturer FTEs, 1.4 clinical training fellows. DoME’s supporting roles provide consistency to the complex, integrated programme and include staff development, research related to medical teaching and learning, leading on peer tutoring, professional communication and ethics, and the three Clinical Skills Centres. DoME has close links with CALT, the London Postgraduate Deaneries (for medicine) and the GMC, through its internationally renowned work on assessment. (See DoME website). Other teaching staff In addition to SLMS academic staff, the following are involved in teaching UCL medical students: Clinical staff at: The Royal Free, University College and the Whittington Hospitals NHS Trusts Seven district general hospitals in south east England Approximately 300 GP practices spread throughout the UK A number of Mental Health Trusts and non-NHS psychiatric service providers A range of smaller NHS and voluntary sector providers These are listed in the spreadsheet: Clinical Providers for UCL medical students. The programme employs 54 professional development tutors, working 10 days per year who also act as academic advisors for Phase 1 students. The majority are GPs, with the rest drawn from a range of relevant fields. SES IQR MBBS 2010 6 of 29 Full lists of academic, welfare and module leads are available on the website as follows: Principal MBBS Academic Leads Module Leads MBBS Welfare and Admissions Leads FBS MBBS Module and Assessment Leads Staff with responsibilities within the MBBS programme also contribute to a wide range of College activities including, for example, membership of the following committees or working groups: Academic Board, Academic Committee, QMEC, Keys Skills, Camden Academy, e-learning, ESCILTA, etc.. 1.4 Non-Academic Support Staff Profile Support staff are drawn from Medical Student Administration, DoME and some academic divisions, and NHS Trusts. The Medical Student Administration programme support (including the MBPhD programme and Foundation School management during the first year post-graduation) totals 34 FTEs of staff time (see 0910 MBBS Leadership PAs and Medical Stud Admin for (IQR). For a full list of administrative support staff see: Current Student Administration post holders: In addition to staff within Medical Student Administration the following administrative support is provided through DoME: approximately 2.5 FTEs administrator and clerical staff plus 6 FTE for Technical Clinical Skills Centre staff. 1.5 RAE Assessment Academic members of staff contributing to the MBBS programme were entered in the RAE through their host Divisions within the Faculties of Biomedical and Life Sciences. Professor Jane Dacre acted as a 2008 RAE Panel Member for UOA 45 (Education). 1.6 Learning Resources Students are based mainly at the Bloomsbury campus for the first two years of the MBBS programme. In the third year, they continue to attend some teaching sessions within the UCL Bloomsbury campus, but spend the majority of their time at the three central NHS Trusts; the Royal Free, the Whittington and University College Hospital. In the fourth and final years, they are attached to a range of district general hospitals (DGHs), two general practices (out of a total of around 300) as well attending some sessions on one of the three main campuses (Royal Free, Whittington or Bloomsbury). The required learning resources vary from year to year, and the standard of provision can also vary. For the most part, students have access to adequate learning resources and facilities including libraries, computers, lecture theatres and seminar rooms although capacity is stretched by the size of the year cohorts (330-380) and this limits options for enhancing our teaching and assessments methods. Relevant SLMS and MBBS Facilities and Resources Committees (FRC) are collaborating to ensure current and future needs are met. Mechanisms are being developed to ensure that the MBBS FRC can initiate improvements, replacements and innovations. Lecture rooms & teaching spaces and rooms There is constant pressure on teaching space within the UCL campus given the restrictions of being in the centre of the capital and the number of listed buildings. Consequently there is only one lecture theatre on the Bloomsbury campus that can hold the entire cohort of Year 1 and 2 students, and only one lecture in the whole of UCL (under Royal Free NHS Trust management, in Hampstead) that can hold the entire cohort of Years 3-5. Laboratories and Dissecting Room There are two dry laboratories and three wet laboratories in the Cruciform Building and an additional dry laboratory in the Anatomy Building. The Cruciform laboratories are mostly equipped to a high standard, although SES IQR MBBS 2010 7 of 29 some of the equipment is in need of replacement. The laboratories are shared with Life Sciences courses and are used very heavily throughout the teaching year. Further development of non-lecture teaching is hampered by the lack of sufficient dry laboratories. The dissection room will hold half the class at a time. It has an excellent collection of potted specimens, and while it is moderately well equipped, it is in need of investment in air conditioning and new audio-visual equipment. It is used by a number of courses in anatomy in addition to medical teaching. Management of the dissection room has recently passed from the former Department of Anatomy to a faculty committee chaired by the Dean of Life Sciences. Computers & Information Technology Students have access to computing facilities on all the main campuses and at all NHS sites and are able to access the UCL email and Moodle resources. Students are generally satisfied with the level of access they have although at certain times capacity can not cope with the cohort size. Access to clinical systems in the noncentral NHS trusts is more variable. A full list of all e-learning resources has now been compiled on a single site. E-learning support is of the highest standard and is consolidated by the development of an E-learning advisory group and the appointment of a Learning Technology Adviser. There is a need for a large computer cluster room (seating 200 students) for use for on-line assessments and examinations. Teaching resources at clinical sites The Medical School has written agreements with all sites providing teaching. These agreements define the duties and responsibilities of the NHS Trusts providing training for medical student clinical training. Responsibilities incorporate the minimum standards for the provision of facilities and learning resources. Insufficient teaching space in the new UCH building was problematic for some years and raised serous concerns with the GMC. The site Sub Dean has worked closely with UCLH NHS Trust and made substantial improvements to the availability of appropriate facilities to support undergraduate learning. With the NHS trusts, especially the DGHs, a shortfall in the provision of the agreed resources is often a result of misdirection of SIFT funding within the trust, and can usually be resolved through negotiation with the trust’s finance department. 1. 2. 3. 4. 5. 6. Learning & Development Agreement between NHS London & Health Service Bodies Service Level Agreement between NHS London & UCLMS Letter of Agreement for between Medical School & Community Based Undergraduate Teaching 09-10 Letter of Agreement between Medical School & Small Providers of Undergraduate Teaching 09-10 Standard Tripartite Service Level Agreement- NHS London Medical School-NHS body 08-09 Community Based Teaching Standards Medical School & Community Based Teacher 2009-10 Clinical skills centres There is a clinical skills centre on each of the three central sites. These are well-equipped and staff provide excellent opportunities for learning. Clinical skills centres and their staff are essential for teaching as well as for the complex assessments required for medicine. The Clinical Skills Centres and their staff are predominantly funded via SIFT and therefore may be vulnerable following the implementation of the MPET review. Library provision Medical library services are provided at each of the three main campuses and at all the DGHs. Student feedback on libraries and the support provided by librarians is positive and as part of the annual QA processes, the QA Unit gathers feedback from the libraries to monitor whether they are receiving adequate financial support from the NHS trusts, allowing them to deliver the standards set in the SLA. The library at the Royal Free was recently refurbished to high specification. Funding for these services at central sites is complex, drawing on UCL, SIFT and other MADEL monies. SES IQR MBBS 2010 8 of 29 2. QUALITY MONITORING & ENHANCEMENT FRAMEWORK Description of the MBBS Programme QME Framework and its Articulation with Faculty- and InstitutionLevel QME Frameworks The General Medical Council has the statutory responsibility to set standards for basic medical education and to ensure that these standards are met. The subject benchmark statements for medicine are contained within the GMC document Tomorrow’s Doctors. The standards and learning outcomes contained within are based on current research evidence and best practice with regard to the education of medical professionals and the expectations of both patients and future employers. The Medical School underwent a full review through the GMC Quality Assurance of Basic Medical Education (QABME) procedures in 2004/2005. Following the requirements for the School listed in the resulting report (see Box 1, Section 3 of this SES), the Quality Assurance Unit was set up to ensure that the Medical School has a clear framework for organising quality management and quality control of an increasingly integrated programme in a complex and dynamic educational and service environment. The 2009 SLA between NHS London and the Medical School lays the responsibility for quality assurance and compliance with GMC requirements explicitly on the Medical School (and therefore, de facto, on UCL) The Quality Assurance Unit (QAU) within Medical Student Administration is academically led by the Sub Dean for Quality (0.2 FTE) who coordinates all its activities. As of January 2010 a further 0.2 FTE Senior Lecturer has joined to review and further develop student input and feedback. The role of the QAU is to ensure that high standards within teaching and learning processes for the undergraduate medical programme are recognised and rewarded, good practice is acknowledged and problems can be identified and addressed. The Unit has a key role in helping the MBBS programme interpret, respond to and reconcile the demands of its multiple stakeholders (students, staff, NHS providers and academic divisions) and ensuring its procedures and policies are compliant with the expectation of UCL, the GMC and NHS London. In order to fulfil this role, the QAU is responsible for co-ordinating the following: Internal monitoring of Medical School courses, modules and individual teachers through: o o o o o o o Development and dissemination of teaching standards / guidelines Student evaluation questionnaires (SEQs) QA / SIFT visits to NHS sites Liaison with student representatives Liaison with TPDU on staff development Overseeing the Reward and Recognition scheme (including the Top Teachers and Excellence in Medical Education awards) Promotion of peer review (this is the direct responsibility of the Academic Divisions) External monitoring Ensuring that procedures are established and maintained which allow the School to respond in a systematic and transparent manner to the regulatory requirements of the QAA (via UCL IQR and Annual Monitoring), the GMC and NHS London. The Medical School’s Quality Monitoring and Enhancement Committee (mQMEC) This committee oversees the activities of the QAU and identifies quality enhancement priorities for its curriculum committees and NHS providers. The committee reports to the MBBS Teaching Committee. The QA Unit works closely with the SIFT Office, TPDU, DoME, the three central NHS trusts and seven peripheral NHS trusts, the Sub Dean for Community (who is responsible for all GP placements), UCL Academic Services and committees throughout the Medical School. In response to the publication of the GMC’s Tomorrow’s Doctors 2009, the QAU will be piloting a system for gathering feedback from patients via hospital patient satisfaction surveys. Similarly, we are planning to pilot an employer's survey in order to gather feedback about the preparedness of our graduates. As we are net SES IQR MBBS 2010 9 of 29 exporters of graduates we would need to orchestrate an extensive survey of all foundation schools and their associated trusts. In discussion with the North Central Thames Foundation School (NCTFS), we have suggested to the GMC that such a survey is co-ordinated nationally as a joint enterprise between QABME, PMETB and medical school representatives. Current monitoring processes accurately identify areas of concern about, or risks to, the quality of any aspect of undergraduate medical education. We are planning to develop a Risk Register for the curriculum given the pressure on funding and the rapidly changing landscape that may mean some key providers closing, moving or altering services. The administrative operation of the MBBS programme is governed by a set of service standards available to all staff. 2.1 Student Input and Feedback Student input into the curriculum is extensive and aspires to best practice in higher education. The MBBS programme pioneered the use of online student evaluation questionnaires (SEQs) at UCL and currently gathers more than 20,000 responses per year. We are planning to improve the use of this data further by enhancing summaries, empowering student representatives, targeting SEQs, running more focus groups and improving access to SEQ data for all students and staff. There is very active student representation under the leadership of student union presidents, who in recent years have been dedicated and articulate advocates for their constituents. mQMEC ensures that student representatives and curriculum leads are informed and consulted regarding significant issues relevant to course quality monitoring and enhancement. Students sit on every curriculum committee, sub-committee and module management group, where ‘student issues’ are a standing item on all agendas. QA/SIFT site visit panels include a student representative. This involvement of students in educational reviews is considered best practice by the QAA and the NUS and actively welcomed by sites under review. In 2008-9, the QAU hosted a SSC in Educational Quality which resulted in a discussion paper Enhancing the student experience at UCL Medical School. A new senior lecturer with a special interest in developing the ‘student voice’ has recently joined the QAU. The formation of a Student Parliament is under discussion. A separate document detailing student feedback has been prepared for the IQR Panel: MBBS Student input and feedback (IQR) This document provides: 1. An overview of all mechanisms of student input 2. Summary of student evaluation questionnaires (SEQ) data for all Phases of the MBBS (2008-2009) 3. Longitudinal data - exit questionnaire data and national student survey (NSS 2004 – 2007) 4. A comparison with NSS data 2009 5. Summary of Student Staff Consultative Committee (SSCC) actions points (2007-2009) 6. Summary and response from MBBS to UCLU’s written submission to Institutional Audit 2008 National Workshops on Student Evaluation The QAU, in collaboration with the medical schools at Barts & The London and Hull York, has hosted two highly rated National Workshops on Student Evaluation. These events were supported by grants from UCL ESCILTA and the HEA Subject Centre for Medical Education. See: http://www.ucl.ac.uk/silva/medicalschool/quality/student-evaluation/ProgrammeFINAL.pdf 2.2 Staff Support Programme academic management Following the establishment of FBS and DoME in 2005 and the transfer of management of the MBBS programme to the Division of Medical Education in 2006, DoME and Medical Student Administration worked closely to ensure all committees with responsibilities for MBBS educational management aligned with College requirements. This involved a full review of the structures that had been set up at the time of the merger of the Royal Free and University College medical schools and the introduction of the new curriculum which remained divided across two faculties (FLS and FBS). The organisational charts for FBS as a whole and the MBBS programme are located on the Medical School website: SES IQR MBBS 2010 10 of 29 FBS Graduate and Undergraduate Programme Teaching Committees FBS MBBS Teaching Committee and Sub Committees Detailed guidance regarding the role of administrative staff in these structures are described in the Guide to Medical School MBBS Administration (4) Staff recruitment & induction Academic staff are appointed via their host academic divisions. The majority of administrative staff supporting the MBBS programme are recruited and appointed by Medical Student Administration and appointed by FBS Management in accordance with UCL HR. A few administrators are employed directly by an academic division or an NHS Trust. NHS Trusts are responsible for recruiting all their clinical teachers and deciding whether to include teaching in their job plans. Performance Academic staff (senior lecturer or above) are subject to the appraisal and staff review arrangements of UCL. Clinical academics, who are required to undergo an appraisal process agreed between the GMC and the Department of Health, undergo joint NHS/UCL appraisal annually under the Follet procedures. See: Appraisal Scheme - Clinical Senior Lecturers, Readers and Professors; Clinical teachers are appraised under the NHS appraisal scheme which includes a section on all teaching (not just of medical students). As a result of increased contact via the QA/SIFT visits and the undergraduate liaison committees, many NHS sites are now focusing on undergraduate teaching in appraisals and job-planning. Reward & recognition Formal reward and recognition for education and teaching within the UCL promotions process remains a challenge and SLMS is actively looking to devise criteria that define and capture excellence in medical education that would parallel the metric used for research-based promotion. Nonetheless a few staff have recently achieved promotion, in part, for their contribution to medical student education. These include: David Bender (to Professor), Alison Sturrock and Surinder Singh (to Senior Lecturer). Clinical staff can apply for NHS Clinical Excellence Awards (ACCEA) which in some areas reward education. In the past, major teaching hospitals awarded honorary UCL senior lecturer titles on all newly appointed staff. Most honorary academics are very proud of the title which, importantly, allows them access to electronic learning materials and library resources. There was, however, no process for monitoring the actual contribution of these appointees. The Medical School and Trusts have developed a robust system of appointment criteria, review and reappointment. Unfortunately UCL HR and the Medical School have been unable to resolve key issues related to these important appointments and therefore neither review nor new appointments for clinical teachers is currently taking place. The QAU is responsible for two informal reward and recognitions schemes:- Top Teachers (which are awarded on the basis of a student plebiscite) and the Excellence in Medical Education Awards. The latter are awarded on the basis of evaluation of an educational portfolio, and open to anyone involved in medical student teaching, not only UCL academics. Details of these can be found on the website. Recipients of UCL Provost’s Teaching Awards for contribution to the MBBS programme include David Bender (2007-8) and Ray Noble (2006-7). Staff development and training Academic staff have access to staff development through CALT and DoME’s TPDU. Teaching Improvement Project System, or TIPS courses offered are listed on http://www.ucl.ac.uk/dome/tips/courses . TIPS courses are funded through a special SIFT arrangement between DoME and a number NHS providers. As a result of the MPET funding review, the future of this programme and needs of medical teachers is under review. A separate paper outlining current approaches and challenges to staff development has been prepared. Faculty Development for Teachers on the MBBS Programme SES IQR MBBS 2010 11 of 29 Higher qualifications in education A number of key staff have teaching certificates or masters degrees education while other are currently enrolled in higher degree programmes. Many academics are also Fellows of the HEA and at least four individuals are undertaking a Doctorate in Education at the Institute of Education, including Deborah Gill and Anita Berlin. In 2010-11, DoME will welcome its first intake of students to a new UCL postgraduate Certificate in Clinical Education. 2.3 Recruitment and Reception of Students There continues to be considerable pressure on the available places for students to read Medicine. Applications for 2010 entry exceeded 2500 for a total of 330 places (nearly 8 applicants per place). Screening of qualifications includes assessment of application forms and use of Biomedical Admissions Test (BMAT) scores. All applications are read carefully by several people and an overall ‘priority’ score is assigned to each application. Candidates are then invited to interview in order of priority and interviewing continues until places are exhausted. This usually means that we invite 700 - 800 candidates to interview at UCL, between December and early March. This process is conducted by the Medical Admissions Officers and the Admissions Tutor in accordance with the selection procedure guidance published on the Medical School website and in the prospectus. Each selected candidate is interviewed by a panel of three interviewers. Panels are formed from a pool of over 250 interviewers, comprising academic members of staff, clinicians and laypersons. Lay interviewers include senior medical students, head teachers or other school representatives, careers advisers and healthcare administrators. The pool of lay interviewers includes individuals with disabilities. We endeavour to ensure that wherever possible, the panel of interviewers is balanced in terms of gender, profession, ethnicity, etc.. All interviewers receive structured training and are given guidance notes to ensure fairness. Interviewees have the opportunity to meet Admissions staff, including the Admissions Tutor, when visiting UCL for their interview, as well as joining a student-led guided campus tour, thus ensuring that all of their questions regarding academic matters, admissions or ‘student life’ can be addressed. Selection tool Description of assessment (e.g. academic qualities, personal qualities, ethical and professional behaviours) Use of this tool UCAS application form Academic qualifications, personal qualities (including motivation for medicine, evidence of teamwork, leadership and communications skills, study skills and outside interests). Academic profile is screened to ensure that entry requirements are met; personal statements and references are scrutinised in order to assess previous experience (work, volunteering, personal), motivation, study skills and other personal qualities. BMAT Assessment of scientific aptitude, critical thinking and written communication skills. BMAT allows us to identify potential in candidates irrespective of their background. The test includes an essay component, which is also used at interview. Comparison of scores of candidates with the average for the cohort – high scores strengthen an application. Scrutiny of essay to assess written English and ability to construct an argument. Interview Personal qualities and ethical and professional behaviour (including intellectual ability, motivation, understanding of a career in medicine, ability to express and defend opinions, awareness of relevant issues, attitude including integrity and flexibility, individual strengths, Interviewers score candidates for a set of criteria and make recommendations to the Admissions Tutor as to whether the candidate should receive an offer. SES IQR MBBS 2010 12 of 29 communication skills). The BMAT essay is used to provide a discussion topic. Additional documentation Academic qualifications, personal qualities. Candidates are given the opportunity to submit additional information to support their UCAS application (for example references or commentaries from work experience placements). Additional information is considered in order develop a more complete understanding of the candidate’s background and experience, particularly for graduates and mature applicants. 2.4 Student Support Personal Tutor and Medical Student Advisor Scheme Since 2004/2005, PDS tutors have been the pastoral tutor to members of their tutor group of approximately st nd fifteen 1 or 2 year students. The tutor helps to ensure academic and pastoral progress and support. Guidelines for this role for PDS tutors are circulated at tutor training. In Year 3, (the first clinical year) students will be assigned an advisor and expected to have four appointments over the course of this year. During Years 4 and 5, students are expected to have at least one appointment each year with their advisor in order that they can track their progress, potentially write them a reference, and give advice on foundation year applications. Welfare system There is a highly regarded welfare system for all medical students, offering both pastoral and academic support throughout the course and led by the Faculty Tutors. Welfare clinics are held on a daily basis at the three central sites with a balance of male and female, academic and clinical Welfare Tutors. For details please see Welfare Handbook and website. Over the last academic year, approximately 1,700 appointments were made for students in these clinics for welfare issues. The School’s ethos is to provide students in difficulty with easily accessible and flexible support through the overarching framework of the welfare system. The welfare provision has undergone extensive development over the last 5 years and is able to help students who have academic, personal, social or health problems. The service relies on both self-referrals and referrals by concerned staff where students may lack insight or motivation to address their difficulties. Key elements of the welfare system are: Close Supervision policy for students requiring extra support Student Support Cards for those who wish educational supervisors and/or examiners to be made aware of health or personal circumstances which might affect their performance Serious Concerns reporting system (via UCLMS Fitness to Practise forms) for student whose conduct has caused alarm during the course or in an assessment. Ultimately most students known to the welfare service will graduate with or without ongoing support. A few will be referred for a full Fitness to Practise procedure. The UCLMS welfare system, however, is not framed as a “Fitness to Practise" system. There is a clear overlap and link between pastoral and academic support and the fitness to practise process, but the ethos of the service is to emphasise support and encourage self-reporting and shared responsibility for students in difficulty. Preparation and progress of students away from College The largest part of a medical student’s time will be spent away from College on placements. One of the mainstays of preparation is ensuring both the public and the student are afforded adequate safeguards in terms of potential personal and health risks. Their professional responsibilities are emphasised in their PDS sessions where they are familiarised with the GMC document The Duties of a Doctor. Medical students are required to demonstrate that they are covered by a professional defence society, they have CRB clearance and that they know their immune status against a specified list of infectious diseases. In SES IQR MBBS 2010 13 of 29 future applicant will also need Independent Safeguarding Authority (ISA) clearance. These are explained in the Medical School A-Z Policies and Regulations Students’ commitment to their duties regarding these procedures is obtained when they sign the Student Agreement at the beginning of Year 1 and again in Year 3. NHS placements – hospital & GP A very strong emphasis is placed on ensuring student can access up to date joining instructions prior to placements and receiving the best possible induction on arrival. These are evaluated in the SEQs. Each hospital site has a named tutor or sub dean, and an undergraduate administrator for support and advice. Students on GP placements receive written web based information including access to evaluation by previous student. All students attend the academic department for a briefing prior to the placement. Students submit a Learning Needs Assessment checklist which is used for initial, mid-block and end-of-firm discussions. Overseas electives Nearly every final year student goes abroad for an 8 week medical elective. The procedures for screening placements and for preparing students are meticulous and include at least one personal interview and an occupational heath and insurance advice session for each of the 370+ final year students. Each student is given the personal mobile phone number of the Sub Dean for Electives prior to departure in case of emergency such as accident, theft or needle stick injury. Procedures for planning electives and staying safe are presented via detailed Factsheets. Student handbooks Every phase and module of the course has its own handbook which can be accessed via the website. In addition, the A-Z Policies and Regulations provides easily accessible and detailed advice in key areas. 2.5 The Teaching Function and Process The undergraduate medical course takes 6 years from entry to qualification with the degrees of MBBS and BSc (with the exception of graduate entrants and MBPhDs - see Student Profile, above). On the award of the UCL MBBS degree graduates are eligible for provisional registration with the GMC. This is followed by two years in foundation training posts. After the first foundation year graduates gain full registration with the GMC and after the second they begin specialist postgraduate training. The function of the programme is to produce highest possible calibre graduates who qualify for inclusion on the medical register. In order to achieve this, the entire programme must be approved by the GMC and comply with their published recommendations; Tomorrow’s Doctors. The recommendations cover all aspects of course content (through “outcomes for graduates”) and specify mandatory standards for the delivery of teaching, learning opportunities and assessment. The most recent edition of Tomorrow’s Doctors was published in September 2009 and is considerably more detailed than previous versions. All medical schools are required to be fully compliant with every outcome and standard by academic year 2011-12. In addition to the general expectations contained within Tomorrow’s Doctors each medical school has undergone a GMC review through the QABME procedures within the last 5 years. Overall, the provision at UCL was deemed satisfactory, however the GMC required the Medical School to address certain specific areas, and recommended changes in a number of others. Most, but not all, of these requirements have been addressed. Outstanding issues and the role of the ongoing Curriculum Review are addressed in Section 3, Self Analysis. It therefore follows that teaching function and processes of the MBBS programme are largely determined by the GMC’s graduate outcomes, standards and requirements. Nonetheless medical schools remain free to determine many aspects of their programme design in terms of overall pedagogic principles, timetabling, sequencing and sites of delivery. These are outlined in our Programme specification. SES IQR MBBS 2010 14 of 29 2.6 Programme Design, Operation and Review Programme aims Overarching aim: The MBBS programme aspires to educate the UCL Doctor: a highly competent and scientifically literate clinician, equipped to practise patient-centred medicine in a constantly changing modern world, with a foundation in the basic medical and social sciences. This vision is informed by research in education and the relevant sciences and is underpinned by the values of scholarship, rigour and professionalism. The focus is on the development of the student as a scientifically informed, socially responsible professional who, in turn, can serve the health needs of individuals and communities. Aims of the Programme: To ensure graduates are: Scientifically literate and clinically competent Ready to enter careers in any clinical speciality or in the biomedical sciences Capable of evidence-based practice Fit to practise clinically and / or conduct research legally and ethically with appropriate professionalism and attitudes FBS Teaching & Learning Strategy SES IQR MBBS 2010 15 of 29 Underlying Principles of the MBBS programme: Content: A coherent curriculum supporting acquisition of knowledge necessary to achieve excellence in clinical practice and clinical sciences. Programme design: In order to achieve our aims, there is an integrated 5 year, core programme of study, divided into three phases: Phase 1 (Years 1 and 2) Science and Medicine Phase 2 (Years 3 and 4) Science and Medical Practice Phase 3 (Year 5) Preparation for Practice All students who are not already graduates will intercalate a year to take a BSc degree in a basic or clinical science, history of medicine or another approved subject. This will normally be after the end of year 2, or sometimes after the end of Year 3. Vertical Spines and Modules There are also four vertical modules which run throughout the 5 year core programme: Society and the Individual Mechanisms of drug action and the use of medicines (which begins in Year 2) Pathological sciences Cancer medicine (introduced in 2009-10) The Professional Development Spine (PDS) runs through the 5 year programme of study in a vertical format. It includes: Clinical and Communication Skills; Ethics and Law; Evaluation of Evidence; Health Promotion; and Community Medicine. It was introduced with the new Curriculum in 2000. Learning is mainly in small group work and reflective activities both in protected time and embedded in other clinical activities. It is therefore integrated with the rest of the curriculum, and students undergo integrated (and stand-alone) assessment of professional skills. Student choice In order to allow students to pursue personal interests or direct their learning to areas where they may wish to gain additional experience, the programme incorporates two optional elements. In 2003, the GMC stipulated that at least 20% of the programme should be “student selected”, but the proportion has been reduced to 10% in the 2009 recommendations. SES IQR MBBS 2010 16 of 29 Student Selected Components (SSCs) There is a wide range of Student Selected Components in each phase of the programme. Options include placements in clinical and voluntary organisations, joining a research team or undertaking a library project. SSCs are assessed through the submission of a written report and receive very positive feedback. Electives The 8 week final year elective is one of the most popular parts of the programme. The majority of students go abroad – about 50% to USA, Australia or New Zealand, and the rest to developing countries throughout the world. Many are supported by charitable bursaries. Occasionally students who have failed a module in Year 4 forfeit their electives in order to have directed remedial study. Preparation and guidance for electives is described above (see Preparation and progress of students away from College). Assessment is through a supervisors report from the host institution and the grading of a project submitted by each student. Student feedback is gathered, collated and made available to future students to facilitate their choices. The organisation of the medical electives conforms to, and in some ways exceeds, the expectations outlined in the Gold Book. Intercalated BSc All students (except graduate entrants) undertake a one year programme for which they are awarded an iBSc degree. The delivery, quality assurance, annual monitoring and IQR of these programmes rest with their host departments or divisions. The final assessment of the iBSc award incorporates marks from earlier years of the programme. The Academic Committee has recently agreed that the proportion of marks from Years 1, 2 and 3 should be 1:1:6, bringing UCL in line with other medical schools. UCL offers the widest range of iBScs in the UK and approximately 60 students join UCL iBScs from other schools each year, and 10 UCL students undertake BScs outside the institution. From 2010-11, students entering the programme will be advised that they will only be able to intercalate between Years 2 and 3 to limit fluctuations of numbers entering clinical placements. MB PhD Programme The MB PhD Programme, which began in 1994, enables up to 10 students per year studying for Medicine to be awarded the degrees of MB BS, BSc and PhD in just eight years, instead of the normal nine if the PhD is undertaken separately. The aim of the scheme is to foster academically-minded medical students who wish in the future to combine research with clinical medicine. Students undertake a modified MBBS programme from rd their 3 year. Securing funding for students and ensuring they are able to complete both their medical studies and stay focused on a thesis is a challenge. A UCL MBPhD graduate has just gained a professorial chair at the age of 33. Programme operation The UCL and Royal Free curriculum prior to the merger, conformed to what is known as a traditional Flexnerian model – two years of basic science, organised in disciplines taught in lectures and laboratories, followed by three years of clinical placements in the major specialties. The 2000 curriculum introduced a modularised programme which ensured horizontal integration (in body systems in Phase 1, and in clusters of related clinical areas in Phase 2). Phase 3 aimed at providing more direct clinical contact in district general hospital and GP practices. Vertical integration was built in through the longitudinal modules listed above. Phase 1 (Years 1&2) In addition to the Professional Development Spine and the vertical modules, Phase 1 is arranged as a series of systems-based, consecutive modules, each of which builds on knowledge, understanding and skills acquired in previous modules, and which provides for the acquisition of further knowledge and skills in subsequent modules. Each module is based on a physiological system and provides integrated teaching across all disciplines. The modules are: Year 1: Foundations of Health and Disease; Infection and Defence; Circulation and Breathing; Fluids, Nutrition and Metabolism. Year 2: Movement and Musculoskeletal Biology; Neuroscience; Endocrine Systems and Regulation; Reproduction, Genetics and Development; Cancer Biology. SES IQR MBBS 2010 17 of 29 Phase 2 Year 3 begins with a 3 week, Introductory Course in Clinical Methods, followed by four modules of clinical attachments and related pathological sciences. The clinical attachments are spent at the 3 main university hospitals and in the community, and each student will experience attachments at two of the three central hospital trusts. The clinical attachments for all students cover:General Medical Specialties (GMS); General Surgery (including vascular and urology); General Medicine and Medicine in the Community (GM (MiC)); Care of the Elderly, with Orthopaedics and Rheumatology (COOP / O&R). Year 4 is organised as three modules: Child and Family Health with Dermatology (CFHD); Clinical Neuroscience (Psychiatry and Neurology with Ophthalmology) (CN); Women’s Health and Communicable Diseases (WHCD). Related material from the vertical modules and the Professional Development Spine is incorporated. Phase 3 While professional development is a theme running through the entire programme, it assumes paramount importance in the final year. The year provides choices to fulfil personal interests and to allow exploration of career possibilities through elective and selective attachments. Parallel to this is preparation for the Foundation Year 1 training that follows immediately on qualification. This preparation involves attachments in Medicine and Surgery in DGHs, in general practices and in an accident and emergency department. A new curriculum and structure for Phase 3 will be introduced in 2010-11. Teaching and learning methods The methods of teaching and learning incorporate formal lectures, laboratory practicals, workshops and computer-aided learning (CAL) in Years 1 and 2. Small group learning is mainly in weekly PDS sessions, complemented by some patient contact and community visits. There are recent innovations in integrated casebased workshops taught jointly by scientists and clinicians in some modules. During Year 3 students rotate through clinical placements at two of the three central hospital sites with approximately 8 days in general practice. Patient-based learning is supported by three lecture programmes: Pathological Sciences, Taught Course in Medicine and Use of Medicines. In Year 4 they are placed in the central hospitals, DGH sites and general practice and have a series of study days with lectures and small group activities. Phase 3 is entirely placement-based in general practices and DGHs, incorporating a mock OSCE exam and clinical revision sessions. This is supported by an innovative Moodle programme, Case of the Month, integrating core elements of the final year syllabus with professional development tasks oriented towards foundation year requirements. The new final year aims to emphasise in-depth, practical experience, incorporating longer placements and student assistantships. In addition, students in all years receive highly rated teaching and support from clinical skills staff. Learning and Teaching strategy for the programme is summarised in the 2008 FBS Teaching & Learning Strategy. This will be updated in light of the curriculum review described in Section 3 of this document. Programme review After the introduction of the new curriculum a rolling process to review each phase was introduced. In 2007 a number of drivers led to the commencement of a full review of the entire programme. A description of the curriculum review process and current recommendations forms the basis of Section 3 of this document (the Self Analysis). 2.7 Assessment of Student Performance The structure of the MBBS assessments is largely determined by requirements of the GMC. The assessment team at UCL have an international reputation for best practice and innovation in the assessment of professional SES IQR MBBS 2010 18 of 29 competency. DoME holds contracts with the GMC on a number of professional assessment projects. The MBBS assessment leads also participate in a national exam item-sharing project. In-course assessment In-course assessment in Phase 1 consists of two written reports at the end of each SSC, some practical reports and four essays for PDS (two in each year). In addition, students must complete the following items in their portfolio via Moodle: reflective passages based on key events such as first patient contacts; a checklist of achievement against UCL key skills (Year 1); a checklist of achievement of key skills against the GMC guidance o Good Medical Practice (Year 2); and a 360 appraisal. Written work is passed through Turnitin software and must reach a required standard for the student to progress. Marks are also sent to academic advisors. o In Year 3 students complete a range of tasks for their portfolio including a further 360 appraisal. Students receive written feedback on all work submitted, and oral feedback and an itemised mark sheet for their 20 workbased assessments (WBAs). At the end of each module they have one-to-one meeting with a tutor and receive a Report Form. It is a progression requirement that the portfolio is completed satisfactorily and students must achieve a minimum score in the WBAs. In Year 4, students complete a range of tasks depending on the module, receive an end of module Report form and keep a log book of clinical activities . In Year 5 students also undertake written work as part of their GP and SSC attachments on which they receive structured feedback. They must undertake a minimum of 8 WBAs and receive an overall Grade (A-E) for each attachment. In each year students whose in-course assessment indicates an academic or pastoral problem will need to see a Welfare or Faculty tutor and are offered remedial sessions as appropriate. Formative and Summative assessment through examinations Phase 1,Years 1 & 2: There is a formative assessment at the end of each module, and a summative assessment at the end of each year which determine progression. Year 3: Formative assessments, in the form of written papers, take place at week 15, and summative assessments, in the form of one written paper, workplace based assessment marks, and an Objective Structured Clinical Examination (OSCE) take place at the year end. The aggregate scores obtained in these assessments and in module assessments determine progression to Year 4. Year 3 assessments are moderated by external examiners. Year 4: Related material from the vertical modules and PDS is incorporated. Summative assessments comprising a written paper and an OSCE are held at the end of each module and progression depends on the results obtained in these three assessments. These are moderated by external examiners Final year: The final MBBS examination is an integrated, written and clinical assessment in Medicine, Surgery, Pathology, Use of Medicines and Public Health. It includes assessment of general professional skills including practical and clinical skills, communication skills and ethics. It does not include Paediatrics, Obstetrics and Gynaecology or Psychiatry (because these have been assessed in Year 4) except where these occur in the context of common medical or surgical emergencies. The written assessments consist of case-based written tests in papers designed to integrate separate materials under broad headings, and including exercises in data interpretation. The clinical examination is divided into two parts: A Long Station OSCE that tests for consultation skills, clinical reasoning, and physical examination skills of all body systems, with additional assessment of communication skills, ethical problem solving and critical appraisal of evidence. This exam involves real patients and some simulated patients. A Short Station OSCE consisting of “short” cases based on clinical scenarios and focused on examination, communication and diagnostic skills in any relevant clinical area (including Ophthalmology and Dermatology) and testing ability in practical procedures. The exam relies on simulated patients and manikins. Full information provided for students is available on the assessment webpage Students also receive a briefing immediately before each clinical exam. See LSO briefing and SSO briefing. The operation of exam boards are described in the document: Medical School Examination Boards (3) SES IQR MBBS 2010 19 of 29 External examiners The MBBS assessments rely on a large number of external examiners who are recruited in accordance with College policy. The list is submitted to College and available on request. In addition to a briefing on the day, examiners at finals receive a detailed Guide for Examiners outlining our procedures and expectations. Careers advice to students Over the past three years, there has been a new development within the MBBS programme - a comprehensive and structured approach to career advice led by the Sub Dean for Careers and supported by the Medical Careers Adviser, UCL Careers and Medical Student Administration. Factsheets and podcasts can be seen on the website. The advice and material are highly valued by students. All students receive: Individualised career support from Year 4 with trained careers advisers; A series of workshops to assist with preparing for Foundation Programme applications; An extensive range of factsheets located in a dedicated careers webpage; Access to an exceptionally wide range of iBSc and SSC options, with a strong academic focus. First destinations of graduating students The proportion of the final year cohort who graduated at first attempt are as follows: 2008/09 2007/08 2006/07 2005/06 93% 98% 94% 97.6% Proportion of graduates which has achieved full registration with the GMC or deferred or failed to complete a Foundation Programme Year Full Reg Did not apply for Full Reg Deferred entry to F1 Withdrew from F1 Did not enter/Left medicine 2008/9 93.2% 1.9% 1.6% 2.7% 2007/8 97.5% 1.9% 0.3% 2006/7 98.8% 0.6% 0.3% 2005/6 95.5% 1.8% 0.9% 0.3% F1 = Foundation year 1 or preregistration year (first year post-graduation) Repeating F1 Unknown 0.3% 0.3% 0.3% 0.3% 0.6% 0.9% SES IQR MBBS 2010 20 of 29 3. SELF-ANALYSIS 3.1 Approach to Self-Analysis The purposes of this self analysis are to summarise strengths and weaknesses of the MBBS programme, to draw the attention of the review team to innovations and good practice, and to highlight challenges that the programme faces. This section also includes actions that are planned to address the issues identified. As the programme is concurrently in the process of a PSRB review from the GMC and a detailed, internal Curriculum Review, this section is based on the self analyses, recommendations and aspirations arising from these parallel review activities. The evolution of these processes can be seen in our Annual Monitoring reports for College QMEC and our Annual Returns to the GMC. 3.2 Historical Note 1 UCL Medical School has emerged from the amalgamation of a number of institutions: University College Hospital Medical School merged with the Middlesex Hospital Medical School in 1987, and the Royal Free Hospital Medical School in 1998. These organisations combine a rich past in the history of science and medicine with advanced clinical practice. The current curriculum, which fully merged the University College and the Royal Free Hospital medical schools, commenced in a double process in 2000 with a new first and third year simultaneously. The first cohort to graduate with new final examinations did so in June 2004. In 2005 the programme underwent a full review under the GMC Quality Assurance of Basic Medical Education (QABME) procedures and was tasked with addressing a number of requirements (must-do) and recommendations (should do). See Box 1 below. (The full report and the School’s annual returns to the GMC are posted on the QAU webpage.) The Faculty of Biomedical Sciences was established in 2005, incorporating several world-famous medical institutions into its divisions. Staff from these divisions design and deliver the MBBS programme together with colleagues from UCL Faculty of Life Sciences. The formation of a Division of Medical Education (DoME) (incorporating the Academic Centre for Medical Education, ACME) was approved by the Senior Management Group of the newly established Faculty of Biomedical Sciences in 2006. One of the principal aims of this initiative was to enhance integration of administrative and academic responsibilities throughout all phases of the MBBS programme, with oversight of management of the curriculum, assessments, student load and educational quality, under the directorship of Professor Jane Dacre. 2 Box 1: Summary of requirements for UCL Medical School from GMC QABME 2005 Integration 1. Changes towards integration of the management 2. Changes towards integration of content of all Phases of the curriculum 3. Review teaching styles in Phase 1 to facilitate transition of students between Phases Quality Assurance 4. Further development of quality assurance Resources 5. Ensure adequacy of teaching space following the completion of the move to the new UCH Student Selected Components 6. Review the School’s arrangements for SSCs to ensure that all graduates undertake sufficient learning within SSCs (including those who do not intercalate). 7. The School is required to ensure that students undertake a sufficient breadth of SSCs 8. Curricular time devoted to SSCs is not used for remedial learning 9. Improve mechanisms for feeding back to students on SSCs Self assessment Completed Ongoing Ongoing Completed Completed Completed Completed Completed Completed 1 The MBBS programme in its current form has never undergone IQR. The last IQR with reference to medicine reviewed the clinical course at UCL, (i.e. years 3-5) in 1998, prior to the merger with the Royal Free, the introduction of the 2000 curriculum and the establishment of FBS. 2 Formerly known as known as Royal Free & University College Medical School (RFUCMS). Since 2009 UCL has been included in the GMC list of institutions awarding primary medical qualifications. SES IQR MBBS 2010 21 of 29 Curriculum Review – the process & background information The MBBS Review was commissioned by Professor Ed Byrne following the reorganisation of the two faculties into the SLMS. The overall aim of the review was to reflect on the strengths and weaknesses of the current MBBS programme and to make recommendations for change. Stage 1 involved the formation of a Steering Group which met over the summer of 2007, with the support of Working Parties (WPs) looking at six, specific areas. This resulted in the publication of recommendations in November 2007, which are set out in the MBBS Review Report 2007 Stage 2 started with a consultation on those recommendations, and a report on that consultation exercise was produced in April 2008, Consultation Report. This resulted in a number of significant structural changes (see below). The final stage is a more detailed consultation focussing on the curriculum content and delivery, which will culminate in the publication of an implementation plan. The current part of the Review was launched in July 2009 by a scoping exercise which initially focused on Years 3 and 4 of the course (Phase 2). It has now incorporated all three Phases and the vertical components, because of the need to ensure that our course is fully integrated. The steering group, with four working parties, has now reported. WP1 – Achieving Integration WP2 – Learning Objectives and the Curriculum Map WP3 – Creative Teaching and Learning Strategies WP4 – Implementation Across HEI & Healthcare Delivery Settings A Draft Summary Report MBBS review 2009 has been prepared for discussion. These recommendations, and the principles that will underpin the curriculum, will be considered in a meeting with Professor Sir John Tooke at the end of March, prior to the publication of a final implementation plan. Curriculum Review – drivers for change The factors driving the Curriculum Review can be summarised as: 1. Formation of FBS and the Academic Health Science Centre 2. Alignment with UCL administrative structures 3. Student feedback 4. Need to make further progress on outstanding requirements from GMC QABME report 2005 regarding integration (see Box 1 above) 5. Publication of Tomorrow’s Doctors 2009, with which we need to be fully compliant by 2011-12 6. Rapid change within the NHS provider landscape as a whole, and impact of Skills for Health and the Darzi Report for London 7. Change in the framework of delivery of medical education at both undergraduate and postgraduate level (in particular the Foundation Programme) 8. Implementation of the MPET funding review which will significantly affect SIFT monies for undergraduate education (particularly London teaching hospitals), expected 2011-12. 9. Increasing need to provide evidence of financial transparency as the economic downturn progresses and influences university and health service funding streams. 10. A number of reports, reviews and research papers highlighting priorities for medical education (notably the Tooke Report, the Patel Review, research commissioned by the GMC from the Skills for Health and Illing’s Group) 3.3 What the Students Say Tracking student feedback over a number of years, the following major themes have emerged regarding their perceptions of the strengths and weakness of the programme. SES IQR MBBS 2010 22 of 29 Strengths • • Overall satisfaction is higher than sector as whole. Areas for improvement Lack of clarity re: overall goals More active learning & clinical orientation needed in Phase 1 Lack of learning culture and student-centeredness in some clinical settings (a major symptom being cancellations of teaching) Areas rated very highly: Formal teaching Organisation and management Learning resources High levels of student representation & feedback on curriculum Better formative feedback (both quantity and consistency) Inadequacy of resources – quality of the estate Sources include: UCLMS SEQs & Exit Questionnaires, NSS Major achievements following Curriculum Review Stage 1 (2007-9) Committee structures have been changed to comply with College expectations. All students are now registered on a single Portico programme code for the 5 years of the MBBS course. Similarly the MBBS Faculty Tutors and all academics with leadership roles are now in a single Faculty, FBS, with clear role descriptions and management through the Division of Medical Education. We have also agreed that students will only intercalate at one point to reduce fluctuations in numbers Findings of Curriculum Review Stage 2 (2009- ongoing) Our starting point has been to view the curriculum as a dynamic phenomenon that needs constant attention and refocusing in order to remain fit for purpose in training the doctors of tomorrow. In reviewing the curriculum and exploring opportunities to improve the curriculum we are mindful that our responsibility for the curriculum includes everything a school does to achieve its goals rather than the more narrow conception of a curriculum as what is prescribed to be taught. Below is an analysis of the strengths, areas under development and vision for improvement divided into curriculum content, structure and assessment, followed by an analysis of support areas such as admissions, welfare, diversity, quality assurance and resources. The section ends by highlighting two additional areas of good practice and a summary. 3.4 Planning, Structure, Content and Assessment Strengths The programme content is robust in terms of factual, professional and technical knowledge, and it is underpinned by best practice in assessment. It produces well-informed graduates, (UCL graduates have won the University of London Gold Medal for the last five years) the vast majority of whom graduate and pursue careers in the NHS. Areas of good practice and innovation include examples of vertical integration running through the whole curriculum such as the Cancer Vertical Module introduced in 2008-9 and the Professional Development Spine (PDS), which we seek to emulate in other areas as we complete the requirement to integrate the whole programme. Strengths of the PDS are its longitudinal presence, use of small group work and reflection, as well the popular on-line Case of the Month, recently added to support final year students. PDS incorporates clinical skills teaching from a dedicated and collaborative team with a strong emphasis on professional relationships with students, and pastoral care. The team uses their facilities to maximise training in low-tech simulation, as well as in clinical settings, to enable students to achieve all Tomorrow’s Doctors’ practical competencies. PDS assessments have pioneered the use of the portfolio. In core modules, progress has been made in integration between Phase 1 and 2, with more emphasis on the clinical relevance of science, by using educational approaches that develop and foster integrative learning with scientists and clinicians working together in tutorials, problem based workshops, simulations and practicals. There are some examples of spiral learning which we plan to build on, such as developments in the Circulation & Breathing module in Year 1, and the Critically Ill Patient in Year 3. SES IQR MBBS 2010 23 of 29 Evidence of increased integration between Phases 2 and 3, and Foundation Year 1 include more skills training, in-situ simulation and the introduction of the revised Year 5 syllabus document and a new Year 5 timetable including Assistantships in 2010-11. Strengths in assessment accrue from the expertise of the team and the use of the most up to date formats throughout the course to test the application of knowledge in written tests rather than its acquisition, and preparation for practice in Objective Structured Clinical Examinations (OSCEs). Blueprinting and standard setting ensures tests are comprehensive, and have a robust pass mark defined by the Anghoff procedure. The tests are statistically robust and reliable. The use of common Workplace Based Assessments (WBAs) provides in vivo assessments, with observation of practice and feedback in a format that enhances integration from Year 3 through to the foundation years. The curriculum and assessments are supported by effective administration responsible for maintaining all documents and web pages, managing timetables and examinations for nearly 2,300 students and tracking progress using the MSSR. Areas for development The curriculum is now in its tenth year and has benefited from the quality of its original design. It has been possible to make some improvements during that time, but further change is hampered by the restrictive timetabling, and the need to keep students in blocks. Despite its many strengths however, a number of ongoing concerns from students, growing professional expectations and other drivers for change, offer us a unique and timely opportunity for thorough review. Students, and to some extent staff, want clearer aims and objectives, and these need to be mapped onto Tomorrow’s Doctors 2009. We are aware that our graduates need to be more capable of integrating knowledge and skills across a range of domains and, most importantly, demonstrate better patient-orientated, problemsolving and decision-making abilities. We also wish to develop students’ learning skills further to ensure they graduate as reflective and independent learners with greater hands-on experience, despite the increasingly risk-averse, clinical environment. In assessment we will expand the use of the portfolio to harmonise with the role of portfolios in postgraduate professional development, and ensure all Phase 2 and 3 tests are blueprinted and test preparedness for practise. We need to continue to improve feedback to students for formative assessments. The wider use of eassessment would greatly reduce the administrative burden, but this depends on availability of resources. Current processes for curriculum planning, articulation, mapping, funding and module management tend to lead to stasis and disintegration, rather than promoting regular improvement and rewarding quality. We are reviewing structures and the timetable “matrix” to facilitate change rather than manage a status quo. Key areas for improvement are therefore: • • • • • • • • • Redefining and clarifying overall aims and learning outcomes for the MBBS course Further improvement in integration, to ensure a balance of basic science and clinical practice across the whole course Ensuring the programme takes a patient-centred approach, beginning with sustained, early patient contact Ensuring preparation for practice is a key feature of the course Investment in e-learning, e-assessment and further development of the portfolio and formative assessment Ensuring delivery is mindful of educational objectives, changes in the provider landscape, expectations of patients and of the GMC More investment in positive role modelling and the intellectual and social benefit offered by small group work and membership of clinical teams Developing structures that allow programme review and curriculum development to be continuous and adaptable to reflect the dynamic environment Enhancing the unique selling point of UCL, by effectively integrating scientific principles into the course at all stages Actions planned to achieve improvements The first steps in achieving improvements are to identify key principles for:- SES IQR MBBS 2010 24 of 29 (1) selecting content; (2) ensuring a coherent, pedagogical approach to educational activities. Our next priorities are to ensure that documentation clearly articulates the curriculum and its learning outcomes. This will follow mapping against Tomorrow’s Doctors’ key recommendations and updating our checklist of key skills acquisition. We are considering a single, agreed list of core conditions addressed in the MBBS curriculum. We are already working on more generic and flexible attachments in Phases 2 and 3, shifting emphasis progressively from range to depth of clinical experience. This approach will allow us to move students readily between rapidly changing healthcare providers (where key teaching hospitals are likely to close or downsize) and prepare our students to work within new healthcare environments (such as poly-systems). In assessment we have expanded the use of the portfolio through the Moodle platform in the current year, and this has allowed for more prompt, personalised feedback. Work on standard setting and blueprinting is nearly complete for all Phases. Focus group studies will look at ways of improving confidence in WBAs and informing staff development. The effectiveness of the module management structure will be reviewed. Increasingly close relationships with academic divisions (including the identification of a teaching lead and annual educational goals), and with NHS Trusts mean that HEFCE(t) and SIFT monies, intended to fund the MBBS programme, are beginning to be more clearly accounted for. Managing the student load and fluctuations in numbers remains a challenge and unfortunately data gleaned from College via the Portico system is often flawed. For example only 230 out of 380 finalists were invited to participate in the NSS in 2009, and College estimates our attrition rate over the 6 year programme as 16%, whereas our own data suggests the figure is less than 10%. Academic Services have been actively seeking ways to identify the source of these discrepancies. 3.5 Areas Supporting the MBBS Programme Admissions, widening participation, welfare and career advice The use of the BMAT in the selection of medical students facilitates an admissions process which is fair, transparent, defensible and able to identify potential irrespective of background, resulting in diversity in the medical student population (age, nationality, educational, religious, social and ethnic background, disability). The high academic offer aims to minimise the attrition rate. Best practice is demonstrated in the provision of timely advice to prospective applicants, acknowledgement of application and structured feedback to unsuccessful interviewees. We use trained interviewers from diverse backgrounds including ‘lay’ people with disabilities. ‘Customer’ satisfaction is high in solicited and unsolicited feedback on aspects of the process notably Medical School open days, helpfulness of the medical admissions staff and constructive feedback following interview. On arrival students participate in an induction week and special induction arrangements are made to welcome and orientate Oxbridge transfers and MBPhD students. Overall we believe that our recruitment and reception procedures exceed requirements. There is enthusiastic participation by students in WP activities which raise awareness, create aspiration, dispel myths and help prepare applicants. The Medical School has formed a Fair Access to Medicine Executive (FAME). There are daily Welfare Clinics, and the access to tutors across all Phases is a model of good practice. Mechanisms have been developed to identify and support students in difficulty. Innovative, special provision accommodates student needs such as support cards, the close supervision register, special adjustments, support tutors, and peer support. Welfare works closely with the College counselling service, occupational heath and the chaplain. The work of the welfare tutors is assisted by the electronic Medical Schools Student Record system (MSSR). We have in place comprehensive procedures for medical student fitness to practise, which we endeavour to integrate with College disciplinary processes. Our comprehensive careers services are valued by students, and function well in terms of applicants succeeding in their first choice of Foundation Programme. Areas for development in admissions, widening participation, welfare and careers advice. We are concerned about the maintenance of the quality and diversity of applicants, given the proposed changes to the UCL Admissions process and the financial challenges for graduates, overseas applicants and lower socio-economic groups, and for EU and Home students unable to take out loans. Retaining interviews is SES IQR MBBS 2010 25 of 29 important in this process. We need to reconsider involvement in the UCL Open Day given the negative impact on applicants (see feedback to CRAS). We foresee particular challenges to fair access. These include lack of finance to existing schemes which are run on good will with limited staff involvement. New ISA restrictions will present a number of challenges to the medical school and may compromise involvement of staff and students in WP activities. Changes to the national curriculum may disadvantage applicants from State schools and make them ill-equipped to deal with the demands of the medical programme. Lifting the cap on tuition fees may also provide a disincentive for some students from families on low incomes. The focus of existing WP projects has very much been on financially and educationally disadvantaged groups, so we are examining ways of working with applicants with disabilities and addressing the national policy focussing WP on underrepresented, demographic groups such as students from the former eastern European countries. (Target Medicine is looking to recruit a further school in West London to remedy this.) Welfare services would benefit from ring-fenced funding, increased engagement and training of welfare tutors and greater communication with the student body. We would like to embed careers planning further into the programme and indeed alert potential applicants to the Medical School of the career prospects in medicine. We are mindful of the impact of academic quartiles in selection and of Situational Judgment Test (SJTs) in the foundation years, and hope to take this as an opportunity to pilot SJTs for undergraduates. Quality assurance and student feedback processes The QA Unit has, to date, been able to handle increasing regulatory demands while maintaining its primary function of monitoring the student experience and feeding into curriculum and teacher development. The QA unit has close links with student representatives who participate in site review panels and has pioneered the use of on-line feedback. Through close liaison with the SIFT Office, joint NHS Trust undergraduate education committees have increased service coordination, quality enhancement and allowed some understanding of value for money. The EMEAs and Top Teacher awards, coordinated by the QAU, are much appreciated by teaching and administrative staff. We are actively seeking ways to help students feel they really do have a voice. We would like to be able to close the loop more effectively – enhancing not just monitoring – but this depends on focussing data collection and a more effective module management structure. We aspire to making monitoring and regulation forces for good by using funding to influence and reward quality. In addition to our awards system we are piloting a Targeted Educational Development and Innovation Fund that we hope will be adopted by the Faculty as a whole through recurrent funding. In addition to annual reports to the GMC and college QMEC, we now also provide an annual report to NHS London. Tomorrow’s Doctors 2009 requires us to start gathering feedback from patients and NHS employers. Currently the greatest challenges to quality assurance are the increased regulatory demands which are in need rationalising, and the lack of alignment between the College, the GMC and the NHS (the major funder). (See written response to the Council for Healthcare Regulatory Excellence.) 3.6 Resources Human resources & staff development The programme depends on its academic and clinical faculty, which is generally of the highest quality and is supported by committed Medical School and local leadership, and excellent administrators. The TIPS programme has been very popular but current funding arrangements (through SIFT) are coming to an end and we see this as an opportunity to refocus on enhancing the student experience and intellectual development. ACME, Medical Student Administration and the QA Unit actively promote peer observation of academics in accordance with College QMEC but this remains the responsibility of the academic’s host Division. We are examining ways of retaining and recognising academics and clinicians with an interest in medical education, especially in programme design and leadership. This is a particular challenge in the life sciences. Aspects to address include resolving issues with UCL HR related to the appointment of honorary senior lecturers and developing new appointment and promotion criteria. The performance enhancement process being developed within FBS will enable us to value and recognise educational contributions better. This a good time to review our staff development provision to ensure that teacher training directly sustains our vision for the curriculum, engages with clinical teachers and complements other initiatives such as postgraduate, supervisor development in the NHS. The administrative support required for a stable programme is somewhat different to SES IQR MBBS 2010 26 of 29 that which we will now need in order to sustain a dynamic curriculum that will have to adapt continually to complex external requirements. We are concerned that such an approach to administration is not the norm in higher education institutions and is especially challenging in the current financial climate. We are aware that there are perceived difficulties amongst the academic teaching staff in gaining recognition and achieving academic promotion. Learning resources & funding SLMS and MBBS have established a Facilities and Resources Committees (FRC) to ensure current and future needs are met, based on a Facilities Management Plan which will provide regular review of the fitness for purpose of the facilities. Students report good levels of satisfaction with resources and access to IT in College and NHS sites. The clinical skills centres are highly valued, but the continuity of SIFT funding remains unclear until the MPET review is implemented. Progress on best practice in teaching methods will depend on identifying suitable space, particularly for small group and computer-assisted learning. Annual Monitoring reports have repeatedly identified quality and quantity of teaching space as a major challenge, which is exacerbated by issues related to room booking systems. We await the outcome of the Space Utilisation Study for the core campus commissioned by the Provost. The instability of the NHS settings (with undecided service changes) poses opportunities and risk to clinical attachments, and a probable increase in community-based learning opportunities. For clinical attachments to remain viable, students need accommodation and NHS Smartcards (which allow access to patient records). If there is a loss of residential accommodation at the DGHs, students will be faced with hefty travel expenses or accommodation costs and it is unclear how we will be able to address this. UCL have asked the London medical deans to look at the issue of smartcards. Challenges to resources at NHS sites are compounded by the fact that most NHS Trusts in London have not signed the new Learning Development Agreement (that itemises their obligations to the Medical School) due to concerns about the redistribution of funds that will follow the MPET review. (UCLH currently receives approx £90,000 per FTE, where many DGHs and GP teachers receive less than £10,000; the proposed universal tariff will be around £40,000 per FTE). We understand previous SLAs (Service Level Agreements) are extant and legally valid, and will be applied in good faith. 3.7 Additional Areas of Good Practice Internationalisation Students are exposed to an internationalised curriculum and global health primarily through their medical electives (described in Section 1). All aspects of the preparation and support for these exceed Gold Book requirements. In addition to electives, all students participate in a global health seminar during the pubic health teaching in the Child and Family Health module. The Institute of Child Health offers a popular SSC in global health, linked to specific electives in developing or intermediate countries, as well as an oversubscribed iBSc. After a 5 year moratorium (due overcrowding) the Medical School has begun to welcome up to 40 students annually from aboard to undertake elective periods at UCL and associated sites, and who study alongside our students. Peer tutoring The Medical School is proud of the range of peer-to-peer and near-peer tutoring opportunities that is based around the PALs (Peer Assisted Learning SSC). In addition to participating in the Introductory Course for Clinical Medicine, peer tutors support science modules in Phase 1, and UCL graduates frequently teach students at the DGHs at which they are undertaking their foundation programme. 3.8. Summary – Change and Opportunity In summary, the MBBS programme at UCL remains a popular choice amongst applicants, and its graduates are a credit to the Institution. Students are satisfied with their experience overall, but tell us there are clear areas for development. While there is evidence of outstanding practice, there are other aspects that are in need of refreshment to satisfy our informed and diverse students. In addition, the dynamic nature of medical practice and health care provision compel us to adapt the programme and adopt a flexible, change-oriented approach to curriculum design, pedagogy and management. Many of the necessary developments are ours to make in FBS, however some depend on factors within the College such as facilities, human resources and support services. Others are determined by external forces SES IQR MBBS 2010 27 of 29 such as the requirement to retain our GMC licence and therefore comply fully with its recommendations. The NHS, especially in London, is in a state of flux presenting us with potential opportunities while stretching our foresight, decision making and risk tolerance. This means the leaders of the MBBS programme are tasked with reconciling a range of disparate priorities and negotiating with many bodies with diverse agendas and modi operandi in order to offer our students the highest quality education. Those who teach and learn medicine are living in interesting times - we hope we will be able to ensure UCL is in a position to seize fully the opportunities now before us. SES IQR MBBS 2010 28 of 29 MBBS IQR Document Register (http://www.ucl.ac.uk/medicalschool/quality/priv) 0910 MBBS Leadership PAs and Medical Student Admin for IQR 2008 FBS Teaching & Learning Strategy Clinical Providers for UCL medical students Community Based Teaching Standards Medical School & Community Based Teacher 2009-10 Draft Summary Report MBBS Review 2009 Feedback to CRAS Guide for Examiners Guide to Medical School MBBS Administration Guidelines for PDS Tutors Learning and Developmental Agreement between NHS London & Health Service Bodies Letter of Agreement between Medical School and Community Based Undergraduate Teaching 09-10 Letter of Agreement between Medical School and Small Providers of Undergraduate Teaching 09-10 Library Questionnaire LSO Briefing MBBS Student input and feedback (IQR) Medical School Examination Boards Programme specification Service Level Agreement between NHS London and UCLMS SSO Briefing Standard Tripartite Service Level Agreement- NHS London Medical School-NHS body 08-09 Targeted_Education_Development_and_Intervention_Fund_Final Widening participation in the MBBS programme Written response to the Council for Healthcare Regulatory Excellence UCLMS Glossary IQR 2010 SES IQR MBBS 2010 29 of 29