Falls Prevention Awareness Week
advertisement

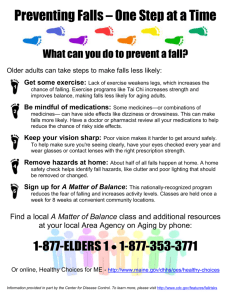
Volume 5, Issue 1 (FOR ADULTS ONLY) SPOTLIGHT ON EMS O F F I C E O F N J E M E R G E N C Y M E D I C A L S E R V I C E S D E P A R T M E N T O F H E A L T H P . O . B O X 3 6 0 T R E N T O N , N J 0 8 6 2 5 - 0 3 6 0 Fall 2013 Falls Prevention Awareness Week Did You Know. . .Every year in the U.S., one in three adults age 65+ falls; half of people 80 and older fall each year. People who fall are 2-3 times more likely to fall again. Did You Know. . .About half of falls result in injuries. Each fall increases the likelihood of more serious injury or death. Falls cause 90 percent of hip fractures and are the leading cause of head injuries. Did You Know. . .Taking four or more medications increases a person’s risk for a fall. Did You Know. . .In 2012, the total cost for treating fall injuries for older adults in NJ, including emergency department and inpatient stays was $1.6 billion. Falls changes lives. Bones are more fragile, and many older adults take blood thinners, which make head injuries especially dangerous. Falls lead to disability and a loss of independence. Many people who fall, even if not injured, develop a fear of falling. Falling, and the fear of falling, can lead to depression and hopelessness, loss of mobility, and loss of functional independence. Aging does not make people fall. Diabetes and heart disease affect balance. So do problems with circulation, the thyroid and nervous system. Some medications make people dizzy. Eye problems and alcohol can also contribute to this problem. Falls are NOT a normal part of aging. Preventing them is crucial. Through evidence-based interventions, practical lifestyle adjustments and community partnerships, we can substantially reduce the number of falls. The good news is falls are preventable. Most people know about keeping walkways clear and getting rid of throw rugs. There should be no clutter on stairways. Homes can also be made safer by adding grab bars inside and outside the shower and tub and next to the toilet, adding stair railings, and improving lighting. Even surfaces should be maintained on outside walkways, without cracks or obstacles. Dogs and cats are a tripping hazards. Shoes should have low heels, non -slip soles and fit well. Vision should be checked regularly and eyeglasses replaced as necessary. Be aware of the side effects of any medications. Exercise is especially helpful. It increases strength, flexibility and balance. New Jersey Falls Prevention Awareness Week is observed the first week of Fall to highlight fall hazards and promote and increase public awareness about how to prevent and reduce falls among older adults.. Governor Chris Christie has proclaimed September 22 through 29, 2013 Falls Prevention Awareness Week. The NJ OEMS has joined with the NJ Department of Human Services, Division of Aging Services Statewide Fall Prevention Workgroup to spread the fall prevention message. For additional resources please visit www.nj.gov/humanservices/doas/services/fallprev/index.html. Inside this issue: Special points of interest: Injuries from falls are largely a preventable community health problem. Fall Prevention Awareness Week 1 After the Fall 2 BEERS Criteria 3 Over 50 percent of falls happen in the home. Before the Storm 4 Understanding Geriatric Patients 6 To survive any natural or man-made disaster—plan ahead. Home Modifications for Elders 9 Post Test 8 Little courtesies will make patient encounters much smoother. After The Fall—Guidelines for the post-Fall Assessment By Marlene Tarshish,PT,NHA,CMC P ratfalls and banana peel slips in movies and television shows are laughable, but when an elder falls, the aftermath can end in a reduction in mobility, independence and worse. When treating and transporting an elder who might have fallen, try to obtain as much information as possible about the cause of the fall. Then communicate this data to the next care provider. Suffering a fall can hurt the psyche as well as the body. Many individuals will not readily admit to a fall, or they will blame the episode on the environment. Admitting to a fall might be interpreted as a loss of power, since walking and moving about independently are prized. On the other hand, the need for an assistive device, or help at home, is hard for many elders to accept. Questioning an elder about a fall should be done as soon as possible. Direct questions should include the following: How did you feel before you fell? Was there anything different about your home environment when you fell? (Note: if the individual is wearing shoes, was the floor wet or had there been an episode of incontinence.) Any change in how medication was taken that day? When was your last fall? The need for help may be taken more readily from a medical professional. If an elder will not readily discuss the details of a fall, communication of the findings by the transport team might assist in beginning that conversation. On many occasions, the ambulance call has been one of many to assist an elder up from the floor. Instead of assisting the client to a chair or bed and leaving, take the opportunity for educating the individual as well as others in the home of the severity of the situation. A homebound elder is eligible for many home-based services and recommendations for calling the physician and requesting services should be made. Alert elders to services such as lifecall buttons and lockboxes, to allow police and fire personnel to enter the home. Education of an elder immediately after a fall may prevent additional falls and fractures, loss of function, or even death. Opening the discussion about the high risks of further injury associated with falls is best made by those treating elders in the community – the opportunity is there and should be taken. ### As a Physical Therapist, Marlene is the Rehab Manager for Princeton Home Care, which is the Home Care Division of the University Medical Center of Princeton at Plainsboro. Myths of Aging A five-year-old thinks of himself as “grown-up” next to his baby sister and our children think forty is “old”. Many of us no longer think fifty or sixty is so old. How many misconceptions do you have about age and aging? MYTH: Elderly individuals are helpless and unable to care for themselves. REALITY: Contrary to popular belief, the overwhelming majority of older people are neither disabled nor institutionalized. Ninety-four percent of older people live independently and enjoy independence and many of the same activities as do younger people. Very few require specialized equipment and services. Only 4 to 6 percent of elderly persons are institutionalized at any given time. MYTH: Becoming forgetful and confused is a natural part of aging. REALITY: Any deterioration of mental function is not a normal process of aging. Growing old is not linked to forgetfulness, confusion and other changes in behavior and personality. Page 2 MYTH: Older persons cannot adapt to new ways or learn new things. REALITY: Aging does not affect one’s ability to learn. Older persons tend to solve problems by “thinking things out” as opposed to using the “trial and error” approach of many younger people. And although reaction time increases with age and complexity of the task involved, this increase can be measured in milliseconds. MYTH: As a person ages, he or she becomes less active and no longer productive. REALITY: Personal preferences and personality differences affect one’s level of activity. This results in some people staying active while others disengage, but this discrepancy is found through all ages of people. Although many people “retire” they don’t always stop working; choosing part-time employment or consultant work. ### S P O TL I G H T O N E M S ( F O R AD UL T S O N L Y ) Medications and the BEERS Criteria By: Xiao Zhang, Pharm.D. and Mary L. Wagner, Pharm.D., M.S. Medications are meant to improve health and quality of life, but sometimes they have a very opposite effect. They have the potential for overuse, misuse and life-threatening complications. Older adults consume more medications than any other age group. Approximately 1 in 3 who take at least 5 medications will experience an adverse drug event each year and two-thirds of those will require medical attention. Individuals who see multiple physicians for different complaints are also at higher risk for adverse drug events secondary to drug interactions. Those who have their prescriptions filled through multiple pharmacies face a similar risk. In 1991, Dr. Mark Beers and some of his colleagues published a listing of “potentially inappropriate medications” for people age 65 and older which became known as the Beers Criteria. The American Geriatric Society (AGS) has published subsequent updates, with the most recent release last year, identifying fifty-three medications or medication classes that should be avoided or closely monitored in any elderly patients who are using them. This most recent update created three separate listings of medications: Those to avoid; Those considered potentially inappropriate; and Those that should be used with caution. Health care providers who interact with older adults should familiarize themselves with the BEERS Criteria. A pocket-sized reference handout summarizing the Beers Criteria is available at www.americangeriatrics.org. A patient educational handout regarding medications that increase the risk of falling, developed by the New Jersey Department of Human Services Division of Aging Services, is available at http://www.nj.gov/humanservices/doas/healthy/ publicationsforms.html. It is also helpful to refer complicated patients to their pharmacist for a medication profile review. ### References 1. 2. 3. 4. AGS: The American Geriatrics Society <http:// www.americangeriatrics.org> American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc 2012;60(4):616-31. Chrischilles EA, VanGilder R, Wright K et al. Inappropriate medication use as a risk factor for self-reported adverse drug effects in older adults. J Am Geriatr Soc 2009;57:1000–1006. State of New Jersey Department of Health. http:// www.nj.gov/humanservices/doas/publicationsforms.html. 5. Stockl KM, Le L, Zhang S et al. Clinical and economic outcomes associated with potentially inappropriate prescribing in the elderly. Am J Manag Care 2010;16:e1–e10. 6. Healthcare Quality Strategies, Inc. Project in a Box: Medication and Falls. Accessed on March 5, 2013. http:// hqsi.org/index/providers/Adverse-Drug-Events/Medicationand-Falls.html.. -Xiao is a graduate of the Ernest Mario School of Pharmacy at Rutgers University. -Mary is Associate Professor, Department of Pharmacy Practice and Administration at the Ernest Mario School of Pharmacy at Rutgers University specializing in neurology. In New Jersey. . . In 2012, there are currently 1,749,077 residents of New Jersey aged 60+ years. 1,104 New Jersey residents fall every day (one every 78 seconds). At least one in three (402,833) adults age 65 and older in NJ will fall within the next 12 months. Of these, 75% (302,125) will fall a second time within six months of their initial fall. On average, 194 older adults are admitted to the hospital or treated in an Emergency Department for a fall every day. Falls are the leading cause of unintentional injury hospitalizations and death among older New Jerseyans. The average cost of an inpatient hospitalization to treat an older adult for a non-fatal fall in a New Jersey hospital was $71,420 in 2012. The majority of falls occur during routine activities. VOLUME 5, ISSUE 1 Page 3 Before the Storm - By Molly Berkowitz, RN, MSN, EMT-I — The best way to survive any natural or man-made Consider including additional items specifically for disaster is to be prepared. But what exactly does prepar- yourself: Medications – keep a week’s supply of necesedness mean to YOU? For many of us, it means running sary medications on hand. Include over the to the grocery store for “French toast supplies” (the milk, counter, as well as supplies for any regular bread, eggs…), as soon as we see a few snow flurries. For medical treatments. others, it means laying in a doomsday supply of canned Personal care items (toothbrush, toothpaste…). goods. And still others just hope to have a charge on the Glasses, hearing aids and batteries. phone so they can call 911 for assistance. Spare oxygen, if you use it daily. Well, the reality of preparedness falls somewhere A change of clothing, including shoes in between these extremes. The first thing to be done is A book or other diversion to have a plan. Having a plan begins with evaluating your Keep a flashlight with working batteries accessible in needs. What are the potential emergencies you can ex- every room (you never know when the lights might go pect in your area? Hurri- out). It’s also a good idea to have a small supply of canes, heavy snow, flood cash on hand, just in case you need supplies. If you conditions, and power routinely visit a clinic or medical facility for treatment outages are just a few (think dialysis or wound care, for example) be sure to examples of the weather ask the facility what their emergency plans are. related disasters we’ve Now it’s time to Make your Plan. What do experienced in the last you need on a daily basis? Who do you talk to, deyear. pend upon every day? Who depends upon you? Talk to those people, and The Internet offers a wealth of infortogether, form a plan of mation about personal and family emergency plans. You action. Collect imcan get started with Ready Together New Jersey at portant phone numbers www.nj.gov/health/er. and contact information, Once we’ve identified potential hazards, it’s time and keep it in an easily to put together an emergency kit. Specific items will vary accessible place. Have based upon your circumstances, but here are some esa transportation plan, as well as a back up, to get sentials: you to safety in an emer Water – one gallon per person for at least three gency. days (don’t forget your pets!). If you have a cell phone, keep it charged. Non-perishable food – enough for three days. If Designate an emergency contact outside of your aryou are including canned goods, make sure you ea, so that if local phone lines are down or busy, you have a manual can opener that you can easily opercan call someone to let them know you are OK. If ate. you can, learn how to text. Many times, when calls A battery powered or hand crank radio, so you can get news and weather updates. Include spare bat- won’t go through, a short text message will and you will be able to let your family know that you are OK, teries! or if you need help. If you have special needs, it is Flashlights and extra batteries. important that you register with the state, so that A stocked first aid kit. A whistle – to signal for help if necessary. Three local emergency responders will know to check on short blasts is a universally recognized distress call. you. The Special Needs Registry Moist wipes and garbage bags for personal sanitahttps://www13.state.nj.us/SpecialNeeds/ is a free, tion. confidential web-based registry designed for people A wrench or pliers to turn off utilities. Copies of important documents, like identification, who might find it difficult to get to safety in an emerinsurance, credit cards, medical and family history. gency. You can also call 2-1-1 (toll free) to register. Supplies for any pets. Continued on page 5 Page 4 S P O TL I G H T O N E M S ( F O R AD UL T S O N L Y ) Before the Storm ( . . . continued from page 4) When emergency officials advise you to evacuate, you should plan to do so. If necessary, tell them that you need assistance. If you are heading to a shelter, bring your personal items with you, so that you will have what you need. Not all shelters are pet friendly, so if you have a pet that also needs sheltering, find out their policy before you arrive. If you choose to “ride it out” at home, be aware that emergency responders may not be able to get to you right away. Your local responders are faced with the same challenges as you. Typically, it takes three days for emergency responders from other areas to get to any other disaster area. Now you know why experts recommend a three day supply of water and food! VOLUME 5, ISSUE 1 Finally, it is important that each of us adopts a policy to “Be Informed.” Listen to your local news stations for information. If your community has as emergency notification system or even a simple news feed, make sure you are a part of it.. Visit websites like www.ready.gov for more information about preparedness. You can also call 1-800-BEREADY with your questions and concerns. Most importantly, stay calm. Think before you act. Be patient. Remember, you’ve made a plan. You’ve got a kit. You are informed. You are ready. ### Page 5 Understanding Our Geriatric Patients -by Raphael M. Barishansky, MPH, EMT-B - I n order to better understand our geriatric EMS patients we first need to understand their numbers and what we are seeing as providers. In 1900, those 65 years of age and older made up only 4.1% of the US population. A rise in these numbers was seen in 1930, when America’s older population numbered less than 7 million – 5.4% of the population. The numbers increased to 8.1% in 1950 and 12.8% in 1995. These numbers are changing even more as some 77 million Baby Boomers, born between 1946 and 1964, move towards retirement age. According to the US Census Bureau, today 40.3 million Americans are age 65 and older, an estimated 13% of the population. This number is expected to increase significantly to 70 million by 2030 and 89 million by 2050. The elder population is now the fastest growing segment of the population. One out of every 9 Americans is “old.” Geriatric Use of EMS Services Clearly an increase in the overall number of elders translates to an increase in emergency calls involving older patients. Geriatric use of EMS services has been documented as being twice that of patients younger than 65 and three times greater for those over the age of 85. In 2011, NJ ALS calls recorded in the data warehouse totaled 360,765. Almost 1/3 of those calls – or 120,655 – were for individuals aged 65 years and older. Geriatric patients are at increased risks of morbidity and mortality when experiencing trauma of all varieties, and although they account for just 13% of the population, they account for one-third of all traumatic deaths. Unique Characteristics of Elders We are seeing people living longer due to improved living conditions, increased access to primary health care, improvements in acute health care and better pharmaceuticals. Health care and living standards have improved significantly since WWII. Although the birth rate is declining, life expectancy rates have risen – from 47.3 years in 1900 to 59.7 years in 1930, 73.7 years in 1980 and 78.7 years in 2010. Along with an increasingly older US population come the “joys of growing older.” The medical history is “longer.” Elders often suffer from more than one illness or disease at a time. The existence of multiple chronic diseases often leads to the use of multiple medicaPage 6 tions. (As EMS providers, we may experience this as a shoebox full of medications or an overstuffed bathroom cabinet.) The body becomes less efficient with age. Bones may lose some of their minerals and become less dense (a condition known as osteopenia, or at its later stage, osteoporosis). The spinal column becomes curved and compressed. Bone spurs may also form on the vertebrae. Tissue loss reduces the amount of water in the body. People typically lose about 1 cm (0.4 inches) every year after age 40. Height loss is even greater after age 70. The skin of elders is at higher risk for injury. Skin loses strength and elasticity and develops wrinkles. The number of pigment-containing cells (melanocytes) decreases. The outer layer of skin (the dermis) becomes thinner, more pale and clear. The ability to sense touch, pressure, heat and cold may be reduced. Aging skin repairs itself much more slowly. Wound healing may be up to 4 times slower. Loss of teeth can make the lips look sunken. The jawbone loses bone material, reducing the size of the lower face and making the forehead, nose and mouth look more pronounced. Wax glands decrease in number and ear wax becomes drier. This drier wax can block the ear canal and reduce a person’s ability to hear. The eye socket loses some of its fat pads, making the eyes look sunken and limiting eye movement. The colored portion of the eye (iris) loses pigment, making many very elderly people appear to have gray or light blue eyes. Although many age-related changes cannot be prevented, certain steps will help to slow or reduce them. Exercise, avoiding smoking and following a healthy diet often help to slow the progression of ageing changes. The picture of a hunched over, frail man or woman with a pot belly and skinny arms and legs does not happen to everyone. Communication Normal physiological changes may include impaired or loss of vision, decreased or loss of hearing, an altered sense of taste or smell and lower sensitivity to touch. Any of these conditions can affect your ability to communicate with the elder patient. There are some good general rules to follow – they can assist in the communication and assessment Continued on page 7 S P O TL I G H T O N E M S ( F O R AD UL T S O N L Y ) Understanding Our Geriatric Patients (. . .continued from page 6) process. If at all possible, face your patient when speaking and try to stay in the middle of their field of vision. Speak slowly and remember to avoid the medical jargon or terminology. You might be the only one who understands what you’re saying. Relatives and friends will sometimes speak up for your patient. They mean well, but then you might miss hearing what your patient has to say. Speak with your patient. They may feel that their complaint is trivial. He or she might not readily volunteer information or might even say “I don’t want to bother you.” You might have to probe for the significant complaints or symptoms. Always let your patient know everything you are doing - and I don’t mean just clinically. If you are going to step out of their line of sight, say that. Let them know you are still there. And tell them what you are doing. Talk your way through any procedures – remember, you know what you’re doing, but your patient most probably doesn’t. Manners Count Be formal and respectful in your approach. Do not use terms like “Pops”, “Honey”, “Dear” or “Sweetie”. Ask how they prefer to be addressed. Such a simple thing, but it helps to establish rapport and shows respect for your patient. They grew up in a different time. You are acknowledging this and it will be appreciated. Trauma The most common forms of elder trauma include falls resulting in fractures, open wounds, superficial injuries and sprains and strains, motor vehicle collisions and burns. In the US, one out of three adults age 65 and older falls each year. Among those age 65 and older, falls are the leading cause of accidental death. 81% of falls deaths were among people 65 and older in 2007. The chance of falling and of being seriously injured or dying in a fall increases with age. In the US in 2009, the rate of fall injuries for adults 85 and older was almost four times that for adults 65 to 74. People age 75 and older who fall are four to five times more likely than those age 65 to 74 to be admitted to a long-term care facility for a year or longer. In New Jersey, unintentional falls caused 338 deaths in 2012 among those 60 and older. Nearly twice as many older adults died as the result of a fall than because of a motor vehicle accident. VOLUME 5, ISSUE 1 Falls were the 16th leading cause of death overall among older adults, more than 2.5 times the number of occupants killed in motor vehicle crashes. You may need to encourage an elder to make their home safe. Older adults can take several steps to protect their independence and reduce their chances of falling. Tips to do so include the following. Exercise regularly. It’s important that the exercises focus on increasing leg strength and improving balance. Tai Chi programs are especially good. Ask a doctor or pharmacist to review medicines — both prescription and over-the-counter—to reduce side effects and interactions that may cause dizziness or drowsiness. Have eyes checked by an eye doctor at least once a year, and update eyeglasses to maximize vision. Make homes safer by reducing tripping hazards, adding grab bars and railings, and improving lighting. Elder Abuse The reasons for elder abuse are not always clear cut. They include increased life expectancy, increased dependence with that increased longevity, limited resources, decreased productivity and stress for any individual caught between being a parent to younger children and now caregiver to a parent(s) as well. As with child abuse, elder abuse can manifest itself in a variety of ways including physical abuse, sexual abuse, emotional or psychological abuse, neglect, abandonment and even economic/financial abuse. During your history-taking, note any explanations that just sound wrong. Conflicting histories from the patient versus the caregiver or a history that doesn’t match with the type or degree of injury should raise a red flag. Additional “red flags” should include any bizarre explanation for the injury, a delay between the time of injury and seeking your assistance or a history that someone is “accident-prone.” Always look for open or untreated wounds or multiple wounds in various stages of healing, bruises, welts, rope marks, black eyes or fractures. Listen whenever an individual tells you they are being abused. When you are doing the physical assessment, note the locations and patterns of all bruises and injuries. Take note of any bruising at the neck, circumferential bruising, injuries confined to just the torso or Continued on page 8 Page 7 Understanding Our Geriatric Patients (. . .continued from page 7) injuries that take the shape of an object. Advise the staff at the receiving facility of any suspicions. Don’t trust that they will notice the same things you did. Document both your findings and your actions. Legislatures in all fifty states have passed some form of elder abuse protection laws. In New Jersey Adult Protective Services (APS) programs have been established in each county to receive and investigate reports of suspected abuse, neglect and exploitation of any vulnerable adults living in the community. Call 1800-792-8820 or fax 609-943-3464. You can also call 221, 24 hours a day, 7 days a week. Suspected abuse, neglect or exploitation of the elderly in nursing facilities, assisted living residences and other licensed health care facilities should be reported to the Office of the Ombudsman for the Institutionalized Elderly at 1-877-582-6995. Elder abuse appears to be on the rise. According to APS, there were 2,249 reported cases of elder abuse, neglect or exploitation in New Jersey in 2007. In 2008, the number climbed to 2,492. And some studies indicate that for every reported case there are five unreported cases. Hospice Webster defines “hospice” as a program of medical and emotional care for the terminally ill. The concept of hospice is one of comprehensive care for the dying. The physical facilities may be very extensive or quite minimal, but the goal is to provide palliative or comfort care rather than curative care. More than 2,250 hospices across the United States provide support for those terminally ill and their families. During 2010, 58 hospice programs in New Jersey provided care to 30,884 persons for a total of 1,965,196 days of care. Most patients receive hospice care at home, but services might also be provided in nursing homes or hospice houses. EMS is geared to the “emergency” or acute care mode. Success is measured by how a patient’s outcome is improved. Hospice personnel work in a “non-emergency” or chronic care mode. Their patients will never get better and success is measured in how comfortable the patient is made. Sometimes a family member might “panic” and call for EMS services despite hospice involvement. It might be difficult for EMS personnel to know what to do when answering that call. Any transport decisions should be made in conjunction with the patient’s wishes, the primary caregiver and the hospice provider. Some Final Words of Wisdom When preparing to transport any patient (but especially the elder patient), remember to check not just for their medications which should be brought with them (or at least bring a listing of all medications), but ask if they need glasses, dentures, hearing aides, family contact information or anything else. Someone might want their purse, favorite sweater or house keys too. These little courtesies will ease their mind and make the encounter much smoother. ### References Elderly trauma inpatients in New York State: 1994-1998, Journal of Trauma. 2004. Jun: 56(6): 1297-1304. Emergency Medical Services utilization by the elder. Annals of Emergency Medicine. 1982; 11: 610-612. Geriatric use of Emergency Medical Services. Annals of Emergency Medicine 1996; 27: 199-203. Medical transport of the elder: A population-based study. American Journal of Emergency Medicine 1995; 13: 297-300. Raphael M. Barishansky is the Director of the Office of EMS for the Connecticut Department of Public Health. A frequent contributor to various publications, he can be reached at rbarishansky@gmail.com. POST TEST 1. A safe-return bracelet should be considered after an individual with Alzheimer's begins to wander. A. True B. False 2. When EMS personnel are called to the home of a hospice patient they should provide care according to the patient, caregiver and hospice provider’s wishes. A. True B. False 3. 75% of persons aged 65 and older who fall once will fall again within 9 months. A. True B. False Page 8 4. Experts recommend maintaining a 1 week supply of food and water for use during an emergency. A, True B. False 5. 4% to 6% of elderly persons are institutionalized at any given time. A. True B. False 6. Many individuals will exhibit a deterioration of mental function as a normal part of aging. A. True B. False 7. A person is more likely to fall while out shopping. A. True B. False S P O TL I G H T O N E M S ( F O R AD UL T S O N L Y ) Home Modifications for Elders - by Marlene Tarshish,PT,NHA,CMC— A ging in place is the preference of many seniors, but their safety needs and abilities should be considered, especially if there has been a recent change in mobility and cognition. A formerly safe environment can become a danger zone when an elder is confused, using a device for walking or has had multiple falls. To assess a safe walking environment, walk through the home while shuffling. Are there any uneven surfaces, especially at thresholds and change of surfaces from linoleum to carpet? Are wood floors smooth and vinyl tile secured? Are throw rugs in use? They greatly increase the risk of tripping. Ease of entering and exiting the home should be assessed, especially for those using an assistive device such as a cane or walker. Are handholds available beyond railings? Use of an accessory handle added to the doorframe can allow confident and independent access instead of depending upon another. The construction or rental of a ramp should be recommended as early as possible if a chronic concern may lead to use of a wheelchair. Many homes could be made more accessible for wheelchair-level residents by using offset hinges at bedroom and bathroom doors. Their use will offer greater width to safely pass through a doorway. Removing sliding doors on tubs will allow use of a transfer bench. Kitchen cabinets can be reconfigured with the use of pull-out drawers to place most frequently used items at a lower height. In the case of an elder who has been newly diagnosed with Alzheimer’s, it is best to introduce home modifications early, so that familiarity and use become second mature. Tub bars, seats, and handheld shower units as well as emergency call systems are recommended for installation before the need arises since the individual will probably not have the capacity to learn or understand the need for a new device once the condition has progressed. Use of safe-return b ra c e l et s o r o th e r e me r ge n c y-p e r s o nn e l notification systems should be started as early as possible – before the first wandering incident occurs. Baby monitors are useful as intercom systems for caregivers. An elder who will not call for help might be heard attempting to exit a bed. Flipdown rails and armchairs at bedside are helpful when transferring in and out of bed. Bed heights should be assessed for ease of transfer as well as safety. Risers are available to increase the height of beds and chairs. Many home modification aides can be purchased via the web, but a professional such as an occupational or physical therapist should be consulted for installation and training. Tub grab bars when properly placed can act as an assist, while those not located appropriately to serve as handholds might end up being used only as towel bars. Home modifications may be covered by VA benefits or insurance. Modifying a home needs to be considered as early as possible – it might make the difference between aging in place and moving an elder out of the home he or she has occupied for decades. ### As a Physical Therapist, Marlene is the Rehab Manager for Princeton Home Care, which is the Home Care Division of the University Medical Center of Princeton at Plainsboro. POST TEST (continued from page 8) 8. The iris loses color pigment as part of aging. A. True B. False 9. The BEERS Criteria identifies potentially inappropriate medications for those over age 65. A. True B. False 10. Age-related changes include all of the following EXCEPT: A. Ear wax becomes drier. B. Compression of the spinal vertebrae. C. Increased bone density. D. Thinning of the outer layer of skin. VOLUME 5, ISSUE 1 11. Homes can be made safer by: A. Addition of extra towel bars in the bathroom. B. Addition of a second floor with spare rooms C. Addition of throw rugs. D. Addition of a tub seat. 12. Identify the true statement. A. Life expectancy has decreased over the past 20 yrs. B. Americans age 65 and older make up 21% of the US population. C. Falls are the most common form of elder trauma. D. One NJ resident falls every 84 seconds. Page 9 Published by the STATE OF NEW JERSEY Chris Christie, Governor Kim Guadagno, Lt. Governor NJ Department of Health Mary E. O’Dowd, M.P.H. Commissioner OFFICE OF EMERGENCY MEDICAL SERVICES NJ DEPARTMENT OF HEALTH P.O. BOX 360 TRENTON, NJ 08625-0360 Office of Emergency Medical Services Karen Halupke, Director ANSWER SHEET (#130259162) Spotlight on EMS Newsletter, Fall 2013 EMT Name _______________________________ ID # __________ 1 (One) Elective CEU for NJ EMTs with a minimum score of 70% Address ____________________________________________ 1 (One) Professional Development Hour for NJ School Personnel with a minimum score of 70% Town _______________________________________________ State: _________ Zip Code: _____________________ E-MAIL ________________________________________________ Answer sheets must be submitted prior to March 31, 2014. Complete and return only the answer sheet via mail, fax or e-mail—do not fax & mail the same form. OEMS Attention NEWSLETTERS P.O. Box 360, Trenton NJ 08625-0360 Fax (609) 633-7954 E-mail ems@doh.state.nj.us □ Check this box if NJ EMT □ Check this box if NJ School Personnel Falls Awareness, Fall 2013 (circle correct answer only) 1. A B 7. A B 2. A B 8. A B 3. A B 9. A B 4. A B 10. 5. A B 11. A B C D 6. A B 12. A B C D A B C D NJ/PA Reciprocal Continuing Education Documentation Name* _____________________________________________Date of Birth*_______________________________ PA Certification Level* ______________PA Region*_______________ PA Provider # *_______________________ Course Title: NJOEMS Newsletter Volume 5, Issue 1 Falls Awareness # 130259162 Dates Available: September 20, 2013—March 31, 2014 Total Credits: 1 elective CEU/Medical Location: Trenton (Mercer County) NJ Coordinator/Instructor Signature: _____________________________________________________________ _ Name of Coordinator/Instructor: Kathleen S. Lutz Date:________________________ *If requesting proof of CEU for PA CEUs please complete the 5 items marked * and submit form with answer sheet. PA Providers—This document will be returned to you signed and dated. Then you must submit a copy directly to your Regional EMS Council for addition to your continuing education records. VOLUME 5, ISSUE 1 Page 10