Use of joint teaching sessions with medical and pharmacy
advertisement
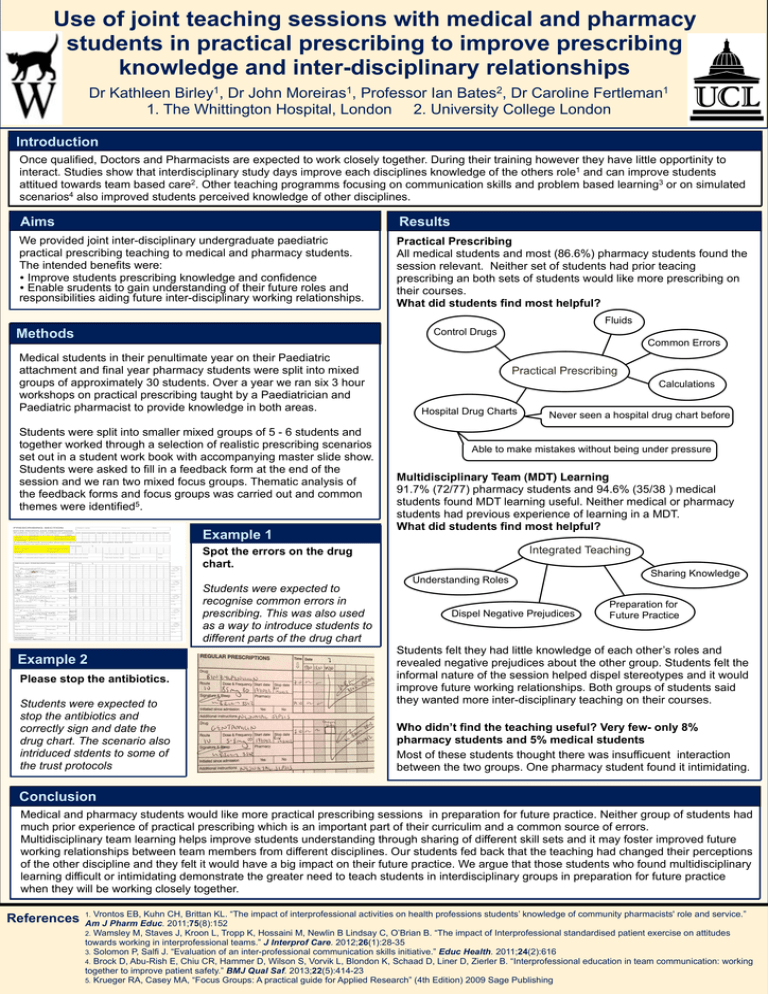
Use of joint teaching sessions with medical and pharmacy students in practical prescribing to improve prescribing knowledge and inter-disciplinary relationships Dr Kathleen Birley1, Dr John Moreiras1, Professor Ian Bates2, Dr Caroline Fertleman1 1. The Whittington Hospital, London 2. University College London Introduction Once qualified, Doctors and Pharmacists are expected to work closely together. During their training however they have little opportinity to interact. Studies show that interdisciplinary study days improve each disciplines knowledge of the others role1 and can improve students attitued towards team based care2. Other teaching programms focusing on communication skills and problem based learning3 or on simulated scenarios4 also improved students perceived knowledge of other disciplines. Aims Results We provided joint inter-disciplinary undergraduate paediatric practical prescribing teaching to medical and pharmacy students. The intended benefits were: • Improve students prescribing knowledge and confidence • Enable srudents to gain understanding of their future roles and responsibilities aiding future inter-disciplinary working relationships. Practical Prescribing All medical students and most (86.6%) pharmacy students found the session relevant. Neither set of students had prior teacing prescribing an both sets of students would like more prescribing on their courses. What did students find most helpful? Fluids Methods Control Drugs Common Errors Medical students in their penultimate year on their Paediatric attachment and final year pharmacy students were split into mixed groups of approximately 30 students. Over a year we ran six 3 hour workshops on practical prescribing taught by a Paediatrician and Paediatric pharmacist to provide knowledge in both areas. Students were split into smaller mixed groups of 5 - 6 students and together worked through a selection of realistic prescribing scenarios set out in a student work book with accompanying master slide show. Students were asked to fill in a feedback form at the end of the session and we ran two mixed focus groups. Thematic analysis of the feedback forms and focus groups was carried out and common themes were identified5. Example 1 Practical Prescribing Calculations Hospital Drug Charts Able to make mistakes without being under pressure Multidisciplinary Team (MDT) Learning 91.7% (72/77) pharmacy students and 94.6% (35/38 ) medical students found MDT learning useful. Neither medical or pharmacy students had previous experience of learning in a MDT. What did students find most helpful? Integrated Teaching Spot the errors on the drug chart. Students were expected to recognise common errors in prescribing. This was also used as a way to introduce students to different parts of the drug chart Example 2 Please stop the antibiotics. Students were expected to stop the antibiotics and correctly sign and date the drug chart. The scenario also intriduced stdents to some of the trust protocols Never seen a hospital drug chart before Understanding Roles Dispel Negative Prejudices Sharing Knowledge Preparation for Future Practice Students felt they had little knowledge of each other’s roles and revealed negative prejudices about the other group. Students felt the informal nature of the session helped dispel stereotypes and it would improve future working relationships. Both groups of students said they wanted more inter-disciplinary teaching on their courses. Who didn’t find the teaching useful? Very few- only 8% pharmacy students and 5% medical students Most of these students thought there was insufficuent interaction between the two groups. One pharmacy student found it intimidating. Conclusion Medical and pharmacy students would like more practical prescribing sessions in preparation for future practice. Neither group of students had much prior experience of practical prescribing which is an important part of their curriculim and a common source of errors. Multidisciplinary team learning helps improve students understanding through sharing of different skill sets and it may foster improved future working relationships between team members from different disciplines. Our students fed back that the teaching had changed their perceptions of the other discipline and they felt it would have a big impact on their future practice. We argue that those students who found multidisciplinary learning difficult or intimidating demonstrate the greater need to teach students in interdisciplinary groups in preparation for future practice when they will be working closely together. References Vrontos EB, Kuhn CH, Brittan KL. “The impact of interprofessional activities on health professions students’ knowledge of community pharmacists' role and service.” Am J Pharm Educ. 2011;75(8):152 2. Wamsley M, Staves J, Kroon L, Tropp K, Hossaini M, Newlin B Lindsay C, O’Brian B. “The impact of Interprofessional standardised patient exercise on attitudes towards working in interprofessional teams.” J Interprof Care. 2012;26(1):28-35 3. Solomon P, Salfi J. “Evaluation of an inter-professional communication skills initiative.” Educ Health. 2011;24(2):616 4. Brock D, Abu-Rish E, Chiu CR, Hammer D, Wilson S, Vorvik L, Blondon K, Schaad D, Liner D, Zierler B. “Interprofessional education in team communication: working together to improve patient safety.” BMJ Qual Saf. 2013;22(5):414-23 5. Krueger RA, Casey MA, “Focus Groups: A practical guide for Applied Research” (4th Edition) 2009 Sage Publishing 1.