Addressing structural uncertainty in health economic models Health economic evaluation
advertisement

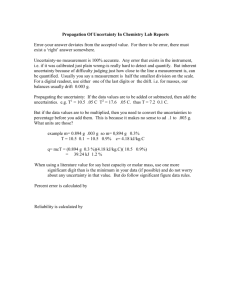
Addressing structural uncertainty in health economic models Simon Thompson University of Cambridge Chris Jackson, Linda Sharples MRC Biostatistics Unit, Cambridge Health economic evaluation Cost-effectiveness analysis • Necessary for health policy decisions and appropriate use of resources • Relevant for interventions which are more effective but also cost more • NICE threshold c. £20,000 per QALY Health economic models • Typically Markov models • Involve evidence synthesis • Usually involve extrapolation UCL, 15 Sept 2011 Cost-effectiveness plane: comparing two treatments Markov model for AAA surgical repair Incr. cost ∆C + Incr. effect ∆E Incremental cost-effectiveness ratio: ICER = ∆C / ∆E Incremental net benefit: INB = ∆E – ∆C Probability of cost-effectiveness: PCE() = Pr (INB > 0) n o s c re e n in v ite s c re e n in v ite AAA screening long-term model Health economic models No AAA U n d e te c te d D e te c te d S m a ll AAA S m a ll AAA D ro p p e d o u t f ro m fo llo w -u p M e d iu m AAA • Make many assumptions M e d iu m AAA In c id e n ta l d e te c tio n L a rg e AAA L a rg e AAA C o n tra in d ic a te d c o n s u lta tio n E le c o p p e n d in g ru p tu re E m e rg e n c y o p e ra tio n E le c tiv e o p e ra tio n AAA D e a th S u rv iv e d s u rg e ry • Are simplifications of clinical reality • Are subject to both: parameter uncertainty and structural uncertainty N o n -A A A D e a th 1 Uncertainty in health economic models Parameter uncertainty • Affects point estimates in (non-linear) costeffectiveness models i.e. Uncertainty about values of parameters in a given model • Important for confidence in decision making Usually handled by Monte Carlo simulation, drawing parameter values from distributions representing their uncertainty – probabilistic sensitivity analysis (PSA) • Relevant to whether more research should be undertaken “Health economic evaluation requires a full quantification of decision uncertainty.” e.g. independently for each parameter e.g. jointly from posterior distribution Generally well handled in practice Sculpher et al, Health Econ 2006 Structural uncertainty Abdominal aortic aneurysm (AAA) i.e. choice of structure to represent a complex process e.g. what clinical events / states should be included? e.g. what risk factors for each event should be included? e.g. how do parameters change over time? Handled by deterministic sensitivity analyses (if at all) Can lead to confusion in decision making Can we do better? Example of EVAR Markov model for AAA surgical repair Comparison: Endovascular aneurysm repair (EVAR) vs. open repair for elective AAA surgery EVAR has lower post-operative mortality higher rates of complications & re-interventions higher rates of late AAA mortality higher costs Health economic model based principally on 4-year follow-up data from UK EVAR1 randomised trial of 1082 patients Jackson et al, JRSS(A) 2009 2 Some structural uncertainties for EVAR model (a) CVD mortality in AAA patients vs. general population Hazard ratio 2.00 (95%CI 0.83 to 4.83) or 1 ? (b) Effect of EVAR vs. open repair on CVD mortality in 2nd year Hazard ratio 3.06 (95%CI 1.12 to 8.36) or 1 ? (c) Effect of EVAR vs. open repair on long-term AAA mortality Hazard ratio 5.84 (95%CI 0.70 to 48.5) or 1 ? Model averaging to address structural uncertainty More complex models with more parameters may – fit the observed data better – predict less well Measure of predictive ability Akaike Information Criterion (AIC) = –2 log likelihood + 2 number of parameters Give more weight to models with lower AIC Report a model-averaged result which incorporates – BOTH uncertainty over choice of model – AND uncertainty for each given model Model averaging techniques Some structural uncertainties for EVAR model AIC = –2 log likelihood + 2p Model weight = exp(–0.5 AIC) BIC = –2 log likelihood + 2p log(n) Model weight = exp(–0.5 BIC) (a) CVD mortality in AAA patients vs. general population Hazard ratio 2.00 (95%CI 0.83 to 4.83) or 1 ? (b) Effect of EVAR vs. open repair on CVD mortality in 2nd year BIC • larger penalty for complexity • converges to a single model choice as n increases • appropriate if one of the models is true AIC • aims to select model with best predictive ability • better predictions often come from larger models as n increases • appropriate if models are approximate representations of complex process Lifetime cost-effectiveness of EVAR vs. open repair ICER Hazard ratio 3.06 (95%CI 1.12 to 8.36) or 1 ? (c) Effect of EVAR vs. open repair on long-term AAA mortality Hazard ratio 5.84 (95%CI 0.70 to 48.5) or 1 ? Lifetime cost-effectiveness of EVAR vs. open repair ICER Probability cost-effective at: (£/QALY) £20K/QALY £40K/QALY Negative 353,000 0.01 0.02 0.08 0.15 Base case (a) (b) 44,800 0.08 0.46 (c) 51,400 0.07 0.38 Base case (a) … (a), (b) & (c) Probability cost-effective at: (£/QALY) £20K/QALY £40K/QALY Negative 353,000 0.01 0.02 0.08 0.15 (b) 44,800 0.08 0.46 (c) 51,400 0.07 0.38 (a), (b) & (c) 19,800 0.52 0.97 Model averaged 92,800 0.07 0.30 … 19,800 0.52 0.97 3 Incremental net benefit of EVAR vs. open repair at threshold of £20,000 per QALY Implantable cardioverter defibrillators (ICDs) Aim: Estimate cost-effectiveness of ICDs vs. anti-arrhythmic drug (AAD) amiodorone for patients at high risk of sudden cardiac death Data: (i) Prospective study of 535 patients with ICDs in UK (ii) RCT of 430 patients of ICD vs. AAD in Canada Previous evidence: Two published trials of ICD vs. AAD Bayesian framework: MCMC (WinBUGS / WBDev) Solid – with covariates Dashed – without (some) covariates Bold – model average Markov model for patients at risk of arrhythmia Transition parameters allowed to depend on: Treatment (ICD vs. AAD) Sex Cardiac ejection fraction Country (UK vs. Canada) Age (<60, 60-69, 70+) 59 parameters in base case model Log odds (95% CI) of death by age Jackson et al, JRSS(C) 2010 Structural uncertainties M1: base case (59 parameters) M2: age effects on length of stay (+12) M3: fewer effects on AAD toxicity (–4) M4: fewer sex effects (–5) M5: quadratic age (+0) M6: cubic age (+7) M7: quartic age (+14) M8: quadratic age x treatment (+14) M9: cubic age x treatment (+28) M10: quartic age x treatment (+42) Model averaging to address structural uncertainty Measure of predictive ability for Bayesian models Deviance Information Criterion (DIC) = Deviance at posterior mean + 2 x effective number of parameters = –2 log likelihood at posterior mean + 2pD For models with weak prior information and no random effects DIC AIC Model weight = exp(–0.5 DIC) Technical note: Weight for model k = probability that model k is selected by the predictive criterion; estimated by a bootstrap procedure, approximated by DIC-based weight 4 Lifetime cost-effectiveness of ICD vs. AAD M1 M2 … M7 … M10 Prob(Mk) ICER (£/QALY) PCE at £20K/QALY 0 0.24 17,000 17,000 0.67 0.68 0.47 38,000 0.06 0.24 71,000 0.17 30,000 0.25 Model averaged Incremental net benefit of ICD vs. AAD at threshold of £20,000 per QALY 10%, median, and 90% quantiles shown Blackness posterior density Extrapolation uncertainty Example: Oral cancer screening Alternative survival models following diagnosis 2-parameter Weibull model Other 2-, 3- and 4-parameter models Bayesian semi-parametric Cox model Comparison of model predictive ability Deviance Information Criterion (DIC) for Bayesian models Model averaging Represent uncertainty over model choice in addition to parameter uncertainty given the model Jackson et al, Int J Biostats 2010 Conclusions Structural uncertainty may be more important than parameter uncertainty Model averaging is an appealing approach for addressing some aspects of structural uncertainty Structural uncertainty may be especially important for age effects and extrapolation Model averaging without data To address structural uncertainty, can use formal averaging across different models with weights which • reflect model predictive ability (e.g. AIC or DIC) if data are available • can include prior weights as well • reflect elicited judgements (and associated uncertainty) if no data are available For extrapolation, model predictive ability based on shortterm data may be of limited usefulness, and elicited judgements are necessary Bojke et al, Value in Health 2010 Jackson et al, Med Decision Making 2011 References Jackson CH, Thompson SG, Sharples LD. Accounting for uncertainty in health economic decision models using model averaging. JRSS(A) 2009; 172: 383-404. Jackson CH, Sharples LD, Thompson SG. Structural and parameter uncertainty in Bayesian cost-effectiveness models. JRSS(C) 2010; 59: 233-253. There are many unresolved issues: e.g. Jackson CH, Sharples LD, Thompson SG. Survival models in health economic evaluations: balancing fit and parsimony to improve prediction. International Journal of Biostatistics 2010; 6: article 34. - Choice of models to average over - How to elicit judgements in real-life policy making - Handling other structural uncertainties (e.g. choice of states) - Better addressing uncertainty due to extrapolation Jackson CH, Bojke L, Thompson SG, Claxton K, Sharples LD. A framework for addressing structural uncertainty in decision models. Medical Decision Making 2011; 31: 662–674. 5