Injecting Healthcare
advertisement

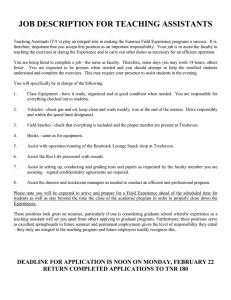
Injecting Healthcare with Human Factors CRISS investigators design and evaluate medical devices and health information technology. We have collaborated with the VA, other Vanderbilt centers and outside vendors to develop and improve the user experience. Teaching & Training Faculty and staff provide guidance in theories, methods and tools related to human factors through simulation-based training and assessment. Communication & Decision Making We investigate team communication, coordination, adaptive problem solving, culture and effectiveness, and individual and group performance-shaping factors, to generate improved clinical care processes and outcomes. Work Analysis & Improvement Using human factors engineering, cognitive psychology, biomedical engineering and implementation science, CRISS studies performance during patient care to understand how and why care deviates from optimal. Core Faculty & Staff Matt Weinger, MD CRISS Director HIT & Technology Usability, Event Analysis matt.weinger@vanderbilt.edu Current Application • Unstructured layout and data entry process • Difficult manual entry of labs • Out-of-workflow confirmation • No clear patient status indicators Sample pre-op workspace screen. (in development) Overview Displays for Hybrid Nuclear Power Plants We helped design a preincision, forced-function electronic time-out checklist that is displayed on a large monitor in the OR and mediated through existing intra-operative nursing electronic documentation. After use during 243,939 sequential operations at VUMC there were zero wrong surgeries, significantly fewer than would be expected from observed national rates, which would have been between 10 and 73. As part of a Department of Energy Nuclear Energy University Program (NEUP), we are assisting the Idaho National Laboratory in the design and evaluation of overview displays in nuclear power plant (NPP) control rooms as part of a modernization program for the nation’s NPP fleet. Current control rooms are largely analog requiring operators to assimilate myriad discrete data (Figure A); they do not support digital decision support and visualization. Unfortunately, proposed large screen overview displays (Figure B) are only economically feasible in new NPPs. Thus, we are studying alternative strategies for overview displays for existing largely analog control rooms. Simulation-Based Performance Assessment Example of complex neonatal intensive care unit setting. Video rating software. Research Assistant Professor (Anesthesiology) HIT UI Design & Evaluation Arna Banerjee, MD Methods This study evaluates the effects of the multidisciplinary participatory design and low-intensity implementation of a structured NICU-to-OR handover tool and process on the quality of handovers and the frequency of transition-of-care related events. To evaluate the intervention, trained observers, using a structured assessment tool, will observe and score actual NICU-to-OR handovers before, during and after interventions and collect data on non-routine events. Associate Professor of Anesthesiology, Assistant Professor of Surgery Education & Training arna.banerjee@vanderbilt.edu Research Associate Professor (Anesthesiology and Medicine) Healthcare System Modeling dan.france@vanderbilt.edu Effect of Decision Support Tools on Team Performance in Simulated Crises Amanda Lorinc, MD Assistant Professor (Pediatric Anesthesiology) Patient Safety, Quality Improvement amanda.lorinc@vanderbilt.edu Clinicians routinely deviate from CRISS collaborates closely with VanderThe goal of this project is to determine published guidelines and care teams if an electronic decision support tool bilt’s Center for Experiential Learning and often delay initiating resuscitative Assessment (CELA), a multipurpose, high(DST) can improve clinician performance measures during cardiac arrest fidelity simulation facility with 12 fully by improving the clinical team’s NTS. In despite the knowledge that equipped clinical exam rooms, a 4-bed this study, the effect on clinical teams of adherence to consensus guidelines ICU or ED, and an OR suite. It’s equipped different versions of an electronic DST improves patient survival and with two complete control rooms, man(a version that emphasizes only TS, a outcomes. It is increasingly evident nequin-based simulation, and the latest version that emphasizes only NTS and MatthewinB.virtual Weinger, MD*; Jason M. Slagle, PhD; Amanda Lorinc, MD; Gina Whitney, MD; Eric Porterfield, MS; that these failures are the result of reality simulators and partial a version that emphasizes both TS and Krys Dworski, Eva Cassidy, and thean PNRE Project Team by the Patient-Centered Institute)in both DEPARTMENT ANESTHESIOLOGY CELA(Funded control room’s view out to test bays. Outcomes Research deficiencies technicalOF skills task trainers. CELA aff ords optimal NTS) will be evaluated during simulated (TS) and non-technical skills (NTS). environment for research and teaching. emergencies. Introduction Figures & Tables Results • A Ò non-routine eventÓ (NRE) is defined as any event that is perceived by clinicians, patients and/or skilled observers to deviate from ideal care for that specific patient in that specific clinical situation (Figure 1).1 Barriers toIn Effprevious ective Handovers studies, we have shown that NREs: DST screen listing technical skills during pulseless arrest management. • In the 140 patients studied (age 58±14 yrs, 54% male), there were a total of 160 clinician-reported NREs and 87 patient-reported NREs. There were 214 unique NREs. Figure 1. NRE Schematic (41%) contained patient-reported NREs. (See examples, Figure 3) experimental paradigm has determined nearin the Intensive Care Unit (ICU) sound Findings With a positive predictive value of ~27%, false • Both the patient and at least Our one clinician reported an NRE in 39 cases (28%), • can be reliably collected prospectively Alarms from physicians 80 2,3 althoughclinicians they were rarely about the same event. and nurses in various care settings threshold auditory perception of alarms and the signalfrequently and 85-99% of cases do not require positive alarms are frequent, leading Preliminary 60 • CRNAÕ s were most likely to report an NREratio (69% which of cases),preserves OR nurses and surgeons performance. • are frequent (from 15% to 50%) to-noise clinician clinical intervention. As alarm frequency increases, to become desensitized to alarms. Yet, findings identify reported NREs in 53% and 55%, respectively, while anesthesia residents reported 40 • are often associated with patient impact or injury 4 Results show near-threshold auditory perception of clinicians develop ‘alarm fatigue’ resulting in failure to respond to the infrequent clinically NREs least often (34%). common barriers • provide data about the nature and severity of process deficiencies 20 • Morepatient than half (54%) of all NREs involved care tasks/processes, 23% involved alarms is around -27 decibels (dB) from background desensitization, missed alarms, and delayed significant alarm may lead to poor to effective that could cause future patient injury cliniciansÕ actions/inactions and 13% involved technology. 0 Figure for 2. P-CONES Probes for Ambulatory Surgery noise at 60 dB. Additionally, with visual offset of a patient responses. This is dangerous the patient when an outcomes. Fatigue from alarm amplitude and Distractions Lack of Many Inadequate Unclearabout how patients and their families/ handovers (see • SBAR ThusToo far, we know very little • The themes of the NREs are shown in Table 1. Structure Cooks Preparation Expectations • Did anything happen that you did • Did you understand • Did anything happen to you caregivers view Ô non-routineÕ events in perioperative care. monitor, there is preserved performance measured by an alarm-provoking event requires intervention nonspecifi c alarms not expect clinical or want to happen? what was supposed that was frustrating, from uniform uninformative graph) and items Reducing distractions is critical. inconvenient, or distracting? • DidSince you get the information you andto happen to you? Inverse Effi ciency Score (IES = Response Time/Accuracy) but is inadvertently missed. false alarm alarms is the post-monitor problem that missed during Conclusions needed to know at the right time? • Was everything you • Did the people taking care of Study Aims needed made can be addressed you know what youby needed? at -11 dB as compared withreported +4dBNREs with worsening at clinically insignificant alarm 80-99%, • Didrates anything reach happen that caused understanding the handovers. Through participatory design sessions, we have • In this preliminary study, 40% of ambulatory surgery patients available to you? you stress, worry, or concern? • Were you worse off afterwards • Determine what aspects of their clinical encounters do patients and and these included clinicalmore care deviations, communication failures, and performance is mainnegative SNRs. Thus, clinician practitioners distrust alarms, lose confi dence in their psychoacoustic properties of alarms and the than you expected to be? developed a tool that we hope will improve handover families view as Ò non-routineÓ and that reflect low care quality or service deficiencies. tained with alarms that are softer than background noise. signifi cance, and manifest alarm fatigue. aural perception of clinicians. safety issues. quality and decrease significant non-routine events. Figure 3. Sample Patient NREs • NRE collection from perioperative patients is feasible and appears a 100% • Elucidate the factors that influence the reporting of perioperative NREs and affect the nature of the NREs that are reported. • I got lost in the hospital trying to findÉ • Determine whether NREs obtained from patients/families add to evidence about clinical system failure modes beyond that obtained from clinicians caring for the same patients. • The lights and/or noise disrupted my sleep. Patient-Reported Non-Routine Events (NREs) In a series of studies, we have shown that perioperative clinician-reported NREs: v1) are frequent (≥1 NRE in up to 40% of all care periods studied); 2) capture a wide cross-section of system failures; and 3) are associated with increased clinician How everyday practice can deviate from best practice. workload and with significant patient physiological disturbances. NREs provide a window on system safety and can be used as a dependent variable in safety interventions. Dan France, PhD Figure B: Digital control room. Utilizing Multisensory Integration to Improve Psychoacoustic Alarm Design in the ICU • Eighty-two surgical cases (59%) contained clinician-reported NREs while 57 cases The Epidemiology of Perioperative Non-Routine Events Clinical practice frequently varies from optimal care, yet medical errors that do not cause patient harm are often not reported. We introduced to health care the concept of the Non-Routine Event (NRE), modeled after safety processes in the nuclear power industry where every deviation from standard operating procedures (SOPs) is reported and investigated. In health care, an NRE is defined as “any aspect of clinical care perceived by clinicians or trained observers as deviating from optimal care for that patient in that clinical situation.” Based on detailed observations of operator performance and interviews, overview display design guidelines are being developed. We will also be doing studies of putative overview displays in NPP control room simulators. Numerous problems remain to be solved, including optimal interface design to support dynamic conditions, how best to support both routine work and rare emergency events, integration with procedures and with alarm systems, and practical issues like hardware display size, number, location and control. Patient-Reported Perioperative Non-Routine Events Handover Tool Development, Implementation and Evaluation Background • Patient care transitions (i.e. patient handovers), while vital to patient safety, are variable and error prone. • Neonatal Intensive Care Unit (NICU) patients are especially vulnerable to medical errors yet, to our knowledge, there are no published studies on ICU-to-OR transitions of care. Figure A: Analog control room. Center for Experiential Learning & Assessment Participants successfully completed 75±13% of critical performance elements. Both technical (5.0±2.1) and nontechnical (5.4±2.0) ratings were distributed across the full 1-9 scale. 32% of BCAs were rated as not performing at the level of a consultant. Higher rated performances were associated with academic (vs. community practice) and participant age < 50 years. If these findings reflect performance during actual care, it calls into question the efficacy of existing systems of continuing education and training. Greater use of simulation-based assessment and training as part of physicians’ life-long learning may be warranted. It is important for physicians to maintain their competence throughout their career. We used standardized high-fidelity simulation scenarios to assess the performance of practicing board-certified anesthesiologists (BCAs) during medical emergencies. Consenting BCAs, who already participated in simulation-based courses at one of 8 sites, performed as the primary physician in standardized medical emergency scenarios. Video recorded performances were rated by trained, independent, blinded, and experienced BCAs. 268 participants managed 294 simulated events. Intra-rater and inter-rater reliability were 0.93 and 0.86, respectively. Shilo Anders, PhD shilo.anders@vanderbilt.edu Redesigned UI • Progressive disclosure of modular queries • Personalized access with ability to audit prior entries • Clear, easy confirmation process • Improved ability to scan for pertinent positives and alerts Electronic Time-Out Reduces Wrong Surgeries www.mc.vanderbilt.edu/criss Percent of Handovers Design & Usability Pre-op UI Redesign Highly interdisciplinary and collaborative, CRISS conducts basic and applied research in healthcare informatics, patient safety and clinical quality, and designs and evaluates health information technology, care processes and medical devices. Laurie Lovett Novak, PhD, MHSA Assistant Professor (Biomedical Informatics) Impact of HIT on Work Patterns laurie.l.novak@vanderbilt.edu In a study funded Methods by the Patient Centered Outcomes Research Institute (PCORI),• CRISS hasourcollected NREs from patients, familyOpenWe refined previous NRE collection tool, the Comprehensive ended Non-routine Event Survey (CONES),2 for use with patients based members and patients’ clinicians in four medical settings: on a thematic analysis of patient/caregiver focus groups, input from our ambulatory surgery, interventional cardiology, pediatric teamÕ s patient representatives, and pilot testing. (Figureoncology, 2) • Preoperatively, obtained written consent and demographicNREs data from and pediatric cardiac surgery.wePatientand clinician-reported patients having elective ambulatory surgery (discharged within 23 hours). were common. • Postoperatively, trained investigators collected NREs from the patients and also from their anesthesia providers, surgeons and perioperative In interventional cardiology cases, 69% contained patient-reported nurses. NREs (the highest of our four settings) while 46% contained clinician• Patients were surveyed with the Patient-specific CONES tool prior to reported NREs. Patient NREs overlapped with clinician discharge and rarely then again by phone approximately one-week NREs. later. Across all settings, most patient NREs reflected deficient care delivery processes – i.e., the care was not patient-centered. Joseph Schlesinger, MD Assistant Professor HIT, Alarm Development, Multisensory Integration joseph.j.schlessinger@vanderbilt.edu Matt Shotwell, PhD Assistant Professor (Biostatistics) Statistical Computing and Inference matt.shotwell@vanderbilt.edu • [Clinician] was condescending/ rude/didnÕ t listen. • I was Ò dumped on the sidewalkÓ before I was ready to go home. • An allergy band was never placed on me. • I couldnÕ t breathe when I woke up from surgery. valuable source of quality and safety data. • Patient NREs rarely overlapped with clinician NREs. • My inpatient diabetes management was Ò not very good.Ó Patient Chronic Illness Routines • Most patient NREs represented deficient care delivery processes Ð The care provided was not patient-centered! • These methods show promise for understanding and evaluating patientcentered perioperative care processes. Table 1. Key Themes from Focus Groups and their Occurrence in Cases and NREs* % of Cases % of NREs (n = 140) (n = 214) Key Non-Routine Event Theme Diagnostic and Therapeutic Issues (unfamiliarity with the patientÕ s condition, 47.1 46.3 44.3 43.9 32.1 31.3 Environment of Care (available food choices, incorrect diet, cleanliness, etc.) 17.9 14.0 Staffing Issues (too few nurses, adequately trained providers unavailable, etc.) 18.6 13.1 15.0 10.7 5.6 8.4 mistakes and errors, diagnostic delays or misdiagnoses, etc.) Health Care Process Deficiencies (unexpected care, failure to get access, delays in treatment, care disruptions or variability, etc.) Communication of Health Information (getting the wrong amount of information, or wrong content, or mistimed delivery, etc.) Patient-Provider Relationship (dismissal of patient concerns, not talking with or listening to patients, being rude or inflexible, etc.) No Relevant Focus Group Theme * Both patient- and clinician-reported NREs included. Key themes for patient-reported NREs in surgical setting. Jason Slagle, PhD Research Assistant Professor (Anesthesiology) Task, Workload & Event Analysis jason.slagle@vanderbilt.edu Scott Watkins, MD Assistant Professor (Pediatric Cardiac Anesthesiology) Cognitive Aids & Decison Support scott.watkins@vanderbilt.edu Clinician performance at varying signal-to-noise ratio In four separate studies, we are examining routines used by patients and their families to manage chronic illness in everyday life. In a References study & ofAcknowledgements cardiac patients, we explored the activities involved in self1. Weinger MB, Slagle J: Human factors research in anesthesia patient safety: Techniques to elucidate care routines and role of JAMIA physical artifacts and other actors. In factors affecting clinical task performance andthe decision-making. 2002; 9(6): S58-63 2. Oken A, Rasmussen MD, Slagle JM, Jain S, Kuykendall T, Ordonez N,who Weingerlost MB: A their facilitatedhomes in a major a study of people with diabetes survey instrument captures significantly more anesthesia events than does traditional voluntary event reporting. Anesthesiology 2007; 107(6), 909-22 flood event, we examined how routines are disrupted and the 3. Rayo M, Smith P, Weinger MB, Slagle JS: Assessing medication safety technology in the intensive people to re-establish routines. We examined asthma care unit. Procstrategies Hum Factors Ergon Soc 2007;use 51:692-96 4. Slagle JM, Anders S, Porterfield E, Arnold A, Calderwood C, Weinger with MB: Significant physiological management routines in teens asthma and their parent disturbances associated with non-routine event containing and routine anesthesia cases. J Patient Safety (in press) caregivers, raising questions about the role of teens’ emerging This study was also supported by Academic Program Support funds from VUMC to CRISS (Center for autonomy on the stability of chronic illness routines. Currently, we Research and Innovation in Systems Safety). are conducting a study of patients with diabetes to understand how routines contribute to diabetes outcomes. Russ Beebe Interaction Designer Jayson Ingram Application Developer Andrew Kline Program Coordinator Carrie Reale, MSN, RN Informatics Nurse Specialist Christopher Simpson Research Manager Jie Xu Research Fellow Obtaining Organizing/ Storing Administration Monitoring Preventive/ Predictive Shared elements among the many medication managing routines produce structure, which may increase resilience of the routines. Sources of Research Support Patient-Centered Outcomes Research Institute (PCORI) Agency for Healthcare Research and Quality (AHRQ) Technology (NIST) National Institutes of Health (NIH) National Institutes of Standards and Anesthesia Patient Safety Foundation (APSF) Veterans Affairs Health Services Research & Development & Research (FAER) Department of Energy (DOE) Foundation for Anesthesia Education