COMPARE 6

COMPARE
THE ARTS
CHILD POLICY
CIVIL JUSTICE
EDUCATION
ENERGY AND ENVIRONMENT
HEALTH AND HEALTH CARE
INTERNATIONAL AFFAIRS
NATIONAL SECURITY
POPULATION AND AGING
PUBLIC SAFETY
SCIENCE AND TECHNOLOGY
SUBSTANCE ABUSE
TERRORISM AND
HOMELAND SECURITY
TRANSPORTATION AND
INFRASTRUCTURE
WORKFORCE AND WORKPLACE
This PDF document was made available from www.rand.org
as a public service of the RAND Corporation.
Jump down to document
The RAND Corporation is a nonprofit institution that helps improve policy and decisionmaking through research and analysis.
Support RAND
Browse Books & Publications
Make a charitable contribution
For More Information
Visit RAND at www.rand.org
Explore RAND COMPARE
View document details
Limited Electronic Distribution Rights
This document and trademark(s) contained herein are protected by law as indicated in a notice appearing later in this work. This electronic representation of RAND intellectual property is provided for non-commercial use only.
Unauthorized posting of RAND PDFs to a non-RAND Web site is prohibited. RAND PDFs are protected under copyright law. Permission is required from RAND to reproduce, or reuse in another form, any of our research documents for commercial use. For information on reprint and linking permissions, please see RAND Permissions .
This product is part of the RAND Corporation occasional paper series. RAND occasional papers may include an informed perspective on a timely policy issue, a discussion of new research methodologies, essays, a paper presented at a conference, a conference summary, or a summary of work in progress. All RAND occasional papers undergo rigorous peer review to ensure that they meet high standards for research quality and objectivity.
COMPARE
P O L I C Y
I N S I G H TS
RAND ReseARch AReAs
Children and Families eduCation and the arts energy and environment health and health Care inFrastruCture and transportation international aFFairs law and Business national seCurity population and aging puBliC saFety sCienCe and teChnology terrorism and homeland seCurity this product is part of the rand Corporation occasional paper series. rand occasional papers may include an informed perspective on a timely policy issue, a discussion of new research methodologies, essays, a paper presented at a conference, a conference summary, or a summary of work in progress. all rand occasional papers undergo rigorous peer review to ensure that they meet high standards for research quality and objectivity.
© RAND 2010 www.rand.org
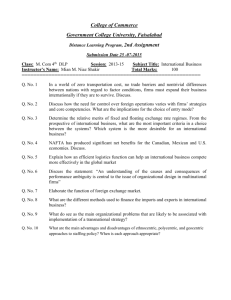
Grandfathering in the Small Group Market Under the
Patient Protection and Affordable Care Act
Effects on Offer Rates, Premiums, and Coverage
Christine Eibner, Federico Girosi, Carter C. Price, Elizabeth A. McGlynn
T he Patient Protection and Affordable Care Act
(P.L. 111-148, or PPACA), signed into law by
President Obama on March 23, 2010, will introduce new health insurance options for many Americans by creating state health insurance exchanges, incentivizing employers to offer coverage, requiring individuals to obtain health insurance, and providing subsidies for low-income Americans without qualifying employer offers. While these changes will alter the menu of health insurance options available to many people, one of the goals of the law is to enable Americans to keep the coverage they currently have if they choose to do so. In an effort to ensure that current coverage options do not change, PPACA exempts existing health insurance plans from certain regulations, a policy known as “grandfathering.” 1
Specifically, grandfathered plans are exempted from rate regulations limiting price variation across enrollees and from risk equalization policies designed to equalize the risk burden across insurers. Newly offered plans, including plans available through state health insurance exchanges, are not eligible for grandfathering and must abide by PPACA’s rating regulations and risk equalization policies. Low-risk plans currently in the market may have a strong incentive to maintain grandfathered status, since grandfathered plans have the ability to offer lower rates than permitted with
We are grateful to John Bertko and Jeanne Ringel for reviewing this manuscript and providing valuable suggestions. This work was funded by a contract from the U.S. Department of Labor (DOLJ089327414), as part of a master contract awarded in June 2008. This analysis builds on earlier work developed through RAND’s Comprehensive Assessment of Reform
Efforts (COMPARE) project, which receives funding from a consortium of sources, including RAND’s corporate endowment and contributions from individual donors, corporations, foundations, and other organizations. The views, opinions, and/or findings contained in this report are those of the authors and should not be construed as an official government position, policy, or decision, unless so designated by other documentation.
1 See Section 1251 of PPACA, 2010, for a complete definition of grandfathered plans.
rate limits and no health status underwriting under
PPACA. This effect is compounded by the fact that grandfathered plans avoid risk equalization, which tends to increase premiums for low-risk policyholders.
The rating regulations and risk equalization policies specified in PPACA limit variation in insurance premiums by effectively requiring lower-cost enrollees to cross-subsidize premiums for higher-cost enrollees.
In general, such policies have the effect of raising prices for individuals and firms with lower health insurance expenditure, and reducing prices for individuals and firms with higher health insurance expenditure. One potential consequence of grandfathering is that healthier individuals and businesses will maintain coverage in grandfathered plans, while sicker individuals and businesses with less-healthy employees will shift into the exchanges. This type of risk segmentation could cause plans offered in the exchanges to have relatively high premiums, which could reduce the total number of people insured.
In this analysis, we used the COMPARE microsimulation model to analyze the effects of grandfathering in the small group market on outcomes including the percentage of small firms (with 100 or fewer workers) offering coverage, premium prices in the grandfathered market and in the exchanges, the total number of people enrolled in health insurance coverage, and the number of people enrolled in exchange-based health insurance plans. We modeled a single, national health insurance exchange designed to represent an exchange for a large state with a typical distribution of firms and workers. Because each state currently has different regulations regarding rating rules in the small group market, we ran several versions of the analysis with different assumptions about premium prices in grandfathered plans. We also considered alternative assumptions about the degree of inertia (bias toward remaining with a status quo
– 2 –
It is likely that the first-year effects of the PPACA law will be different from the long-term or equilibrium effects.
choice) in firm decisionmaking and about risk pooling in the exchanges.
Scenarios Considered
We modeled the effects of PPACA on key outcomes, accounting for the individual mandate, employer penalties associated with not offering coverage, subsidies for low-income individuals, and a Medicaid expansion. We then considered how grandfathering in the traditional employer-sponsored insurance (ESI) market would affect coverage decisions among firms with 100 or fewer workers after health insurance exchanges are opened to these businesses. We also considered how the impact of grandfathering would vary depending on the degree of community rating in the current nongroup market. With full community rating, premiums cannot vary based on worker characteristics or past expenditure patterns among firms. Under modified community rating, premiums can vary with worker characteristics, but only within certain limits. With full experience rating, premiums are based entirely on the past claims experience of a firm. Since PPACA requires that all nongrandfathered plans be subject to risk equalization and adhere to
3:1 rate bands on age, it moves the nongrandfathered market to a situation similar to modified community rating. As a result, we expect that the effects of grandfathering will be stronger in states where there are less-restrictive rating regulations. That is, when there are less-restrictive rating regulations in the current market, firms with lower-cost enrollees have a greater incentive to stay in grandfathered plans.
We considered three scenarios regarding the degree of community rating in the pre-reform market: full community rating, full experience rating, and credibility rating. With credibility rating, premiums are a weighted average of the full communityrated and full experience-rated premiums. Full experience rating rarely occurs in the small to midsized group markets, since the year-to-year variance in expenditure within a firm is too high for insurers to rely on past experience as an accurate predictor of future claims. Nevertheless, we estimated a scenario that allows for full experience rating so that we could see the maximum potential effect of grandfathering on outcomes such as premium prices in the exchange.
We did not consider a scenario with modified community rating in the pre-reform period, however; in practice, the effects of modified community rating will be similar to the effects of credibility rating.
It is likely that the first-year effects of the PPACA law will be different from the long-term or equilibrium effects. If firms are fully or partially experiencerated in the status quo, then firms that have unusually low expenditure in the period leading up to the reform might be offered unusually low premium rates in the grandfathered market. These firms would be unlikely to switch to the exchange in the short run.
Over time, as expenditures revert to a more typical level, these firms may experience premium growth in the grandfathered market and eventually switch to the exchange. As a result, we modeled both first-year and equilibrium effects of the reform and reported results from the equilibrium.
PPACA allows states the option of combining the nongrandfathered small group and individual markets for the purposes of risk pooling. Since people who would be eligible to enroll in the individual exchange market may tend to have higher expenditures than people who would be eligible to enroll in the small group market, the decision to combine or split risk pools may affect premiums faced by firms who choose to offer coverage in the exchange. In our main scenario, we considered a situation in which the individual and small group markets were split for the purposes of risk pooling. However, in scenario testing, we also reported results in which risk pools were combined.
An important area of uncertainty in modeling firms’ decisions to take coverage in the exchanges is the degree of status quo bias, or inertia, in firm decisionmaking. Prior studies have documented inertia in individual decisionmaking, such that people remain loyal to a status quo decision (e.g., a stock portfolio allocation, a health insurance plan) even if standard models of economic behavior suggest that switching would be optimal. Because most studies of inertia in decisionmaking focus on individual rather than firm choices, and because PPACA introduces new health insurance options that have not been previously studied, it is unclear how much inertia we should expect following the reform. As a result, the main results considered in this analysis do not account for inertia in firm decisionmaking. However, because the Congressional Budget Office (CBO) builds substantial inertia into their model, we report results from scenarios with inertia in the appendix.
2 We do not consider inertia in premium prices, as would be the case if grandfathered premiums did not fall to actuarially fair values even after higher-risk enrollees moved into the exchanges.
3
2 Inertia has the effect of increasing the number of individuals who remain on grandfathered plans in scenarios that allow for grandfathering. Inertia has no effect in scenarios without grandfathering, since firms in this case do not have the option to retain their status quo insurance choice.
3 Economic theory and evidence suggest that—in general—prices may be sticky, especially in the short run (see, for example, Rotemberg, 1982). To the extent that traditional ESI premiums remain at high levels after the exchanges are opened, we would expect an increase in the number of firms offering coverage through the exchanges.
– 3 –
Overview of Methodology
The COMPARE microsimulation model uses data, economic theory, and computer programming to predict how individuals and firms will respond to policy changes, given the responses of others. Researchers at RAND developed COMPARE to help understand the effects of health care reform policies. The model relies on data from the Survey of Income and
Program Participation (SIPP), the Kaiser Family
Foundation/Health Research and Educational Trust
(Kaiser/HRET), the Statistics of U.S. Businesses
(SUSB), and the Medical Expenditure Panel Survey,
Household Component (MEPS-HC) to create a synthetic population of individuals, families, and firms with realistic behaviors. Individuals and families in the model make decisions about health insurance enrollment using utility maximization. More specifically, individuals weigh the benefits of an option
(e.g., reduced out-of-pocket expenditure, lower risk) against the costs (e.g., higher premiums). In making health insurance decisions, individuals in the model consider an array of factors, including eligibility for
Medicaid, eligibility for subsidies in the health insurance exchange, the generosity of employer benefits
(if available), and their expected health insurance expenditure. Firms in our model decide whether and what type of plan to offer based on a “group choice” model, where they consider the aggregate utility of their workers. Health insurance options available to small firms (with 100 or fewer workers) in our model include offering traditional ESI; offering a bronze, silver, gold, or platinum plan in the health insurance exchanges; or not offering coverage.
Premiums in the COMPARE model are determined endogenously, using the predicted expenditure of enrollees in each health insurance plan. The model calculates premiums and then allows individuals and firms to change their health insurance decisions using an iterative process, until results converge to an equilibrium. To model the effects of grandfathering, we made some modifications to the COMPARE model to more flexibly capture the effects of state-level rating regulations on prices for grandfathered plans.
For each small business, we calculated a communityrated premium (CP i
) that reflects the average medical expenditure for all firms in a given size category
(fewer than 25 workers, 25–99 workers, 100 or more workers) and Census region (insurers refer to community rating in this context as “manual” rating). In addition, for each firm, we estimated an experiencerated premium (EP i
) based on the observed medical expenditures of the firm’s workers and dependents.
In order to capture how year-to-year variance in small firms’ health care expenditures may influence short-term versus long-term decisions to remain in the grandfathered market, we used this information to estimate deterministic and stochastic components of the premium. The deterministic component is estimated using the following regression:
(1) EP i
= β
0 +
β
1 × (age i
) + β
(health_status i
(2) premium i
= α × EP i
2 × (wage i
) + β
)
3 ×
Above, i is a firm-level indicator variable, and age, wage, and health_status represent the mean age, wage, and health status at the firm.
4 The stochastic component of the premium is added from a draw from an error term, ε . Since we want to estimate the equilibrium effect, we iterate this stochastic procedure by assigning firms a different draw from the distribution of ε each time, so that firms with an unusually low draw of ε in the first period may eventually switch to the exchanges. We found that the model converges quite quickly, reaching a stable equilibrium after three iterations.
We assume that the actual premium faced by a small firm is a function of both the community-rated and the experience-rated premiums, using a credibility rating function. Specifically,
+ (1 – α ) × CP i
, where α is a term that ranges from 0 to 1 and reflects the relative weight insurers place on the firms’ claims experience compared to the expected expenditure among all similarly sized firms.
5 In states with pure community rating, α would be equal to 0. In states with modified community rating, α would be greater than 0, although the magnitude of α could vary depending on state-specific regulations. To get a sense of the impact of grandfathering and how this effect varies depending on the degree of regulation in the small group market, we consider a range of values for α , including 0, 0.25, and 1. States with pure community rating (e.g., New York) would be similar to the α equals 0 case, and states with fewer rating regulations (e.g., Pennsylvania) would be more similar to the α equals 0.25 case. With α equal to 0.25, our model predicts that 90 percent of premiums in the small group market are within plus or minus
35 percent of the mean premium. In this respect,
4 Mean age is the average age of all workers and dependents at the firm, and mean wage is the average worker wage at the firm. Mean health status is the average health status of workers and dependents, where health status is measured on a 5-point scale ranging from 1 (poor health) to 5 (excellent health). We include mean health status in the regression as if it were a continuous variable.
5 The Urban Institute uses a similar strategy to estimate premiums. See equation 9.1.2 on p. 128 of Blumberg et al., 2003.
We found that the model converges quite quickly, reaching a stable equilibrium after three iterations.
– 4 –
We predict a decline in small firm offer rates and a decline in the share of workers employed by offering small firms when grandfathering is eliminated.
the α equals 0.25 scenario approximates a modified community rating situation where premiums are constrained to vary within plus or minus 35 percent of a baseline value.
6 As discussed above, α is likely less than 1 in reality, so models with α equal to 1 represent an upper-bound estimate of the effects of grandfathering.
It is possible that plans could be disqualified from grandfathering if they experience changes, but—to date—the type of changes that would be substantial enough to end grandfathering have not been specified.
7 We did not attempt to model the erosion of the grandfathered market due to gradual disqualification. In calculating grandfathered ESI premiums, we assumed that plans offered by businesses with fewer than 25 workers had an actuarial value of 0.75, that plans offered by businesses with 25–99 workers had an actuarial value of 0.80, and that plans offered by businesses with 100 or more workers had an actuarial value of 0.85. Actuarial values for employer health insurance coverage in the COMPARE model correspond with actuarial values reported in the literature.
8 Exchange plans have actuarial values of
0.60 (bronze), 0.70 (silver), 0.80 (gold), and 0.90
(platinum). We assume that administrative costs are lower in the exchanges than in the grandfathered ESI market (12 percent of premiums in the exchanges versus 20 percent of premiums for firms with fewer than 25 workers in grandfathered ESI plans, and 13 percent of premiums for firms with 25–99 workers in grandfathered ESI plans). Administrative costs for traditional ESI plans correspond to values used by the Urban Institute in its health insurance simulation model (Blumberg et al., 2003). Administrative costs for exchange plans are uncertain; we set the administrative load for these plans at 12 percent, based on expert judgment, but have explored alternative assumptions in a forthcoming report (Eibner et al., forthcoming). A full description of the model methodology, including descriptions of how premiums are calculated, how individuals and firms make decisions, and how we model inertia, can be found in
Eibner et al., forthcoming.
To estimate the effects of grandfathering, we compared results from model runs that included the grandfathered market to results from model runs that eliminated the grandfathered market after health care reform goes into effect. When the grandfathered
6 During the 1990s, many states—including Alaska, Delaware, Indiana,
Ohio, and Tennessee—adopted small group rating rules that restricted premium prices to vary within 35 percent of an index rate. See GAO,
1995.
7 See Fernandez, 2010.
8 See, for example, Buntin et al., 2003, and Gabel et al., 2006.
market was eliminated, we assumed that there was no distinction between exchange-based and traditional
ESI plans. According to PPACA, these plans are subject to the same rating regulations and risk adjustment policies. Additionally, the law states that insurers must consider all enrollees in the small group market to be part of a single risk pool, regardless of whether they are enrolled in the exchanges or not
(Sec. 1312). As a result, it is unclear how nongrandfathered, nonexchange small group plans would be different from small group exchange plans. Potentially, nonexchange small group plans could have different actuarial values than exchange plans or different administrative costs. However, since we do not want our results to be driven by assumptions about actuarial value or administrative load, we assumed that these factors would be equivalent inside and outside the exchanges.
Results
Split Risk Pools, No Inertia
Tables 1, 2, and 3 (beginning on p. 8) show the effects of grandfathering using various assumptions about the degree of experience rating in the grandfathered market, assuming that risk pools are split for the purposes of determining small group and individual exchange premiums and that there is no inertia in firm decisionmaking. We assume that the grandfathered market is fully experience-rated ( α = 1) in Table 1, partially experience-rated ( α = 0.25) in Table 2, and fully community-rated ( α = 0) in Table 3. Regardless of the assumptions about community rating, we predict a decline in small firm offer rates and a decline in the share of workers employed by offering small firms when grandfathering is eliminated (Panel A).
For example, in all scenarios, the share of smallbusiness workers employed by offering firms falls from approximately 90 percent with grandfathering to approximately 86 percent without grandfathering. As with all simulation modeling, there is uncertainty in these results stemming from many sources, including inherent uncertainty in individual decisionmaking and the fact that the data used to populate the model are drawn from a sample. We focus on the share of workers at offering businesses rather than the share of businesses that offer coverage because, in prior analyses, we have found that results reported at the worker level are subject to less uncertainty than firm-level results.
This difference is due to the skewed nature of the distribution of firms. Specifically, there are many small firms that employ relatively few workers, so a change in offering behavior among small firms can have a big impact on firm-level results while affecting relatively few workers. This issue is compounded by the fact that
– 5 – the Kaiser/HRET data used to populate the model undersamples small firms, so a few small firms in the data can have a large influence on results.
The decline in the number of workers at offering firms reflects the fact that, without grandfathering, firms have fewer options, and the price for options of comparable actuarial value tends to be higher. This can be seen most clearly in Table 1, where the average premium in the grandfathered market is lower than the average exchange premiums for the silver, gold, and platinum plans. Although average grandfathered
ESI premiums ($3,604) are higher than average bronze premiums ($3,518), the actuarial value of the bronze plan (0.60) is lower than the actuarial value of plans in the grandfathered market (0.75 for firms with fewer than 25 workers and 0.80 for firms with
25–99 workers). When α equals 1, total enrollment in small group ESI-based coverage declines by 6.3 percent when the grandfathered market is eliminated.
Despite the relatively large decline in small group
ESI enrollment, the total decline in coverage is only about 900,000, or 0.3 percent of the nonelderly insured population. However, sources of coverage vary depending on whether grandfathering is allowed.
Without grandfathering, more people are enrolled in
Medicaid, and more people are enrolled in the nongroup exchanges. These increases are primarily driven by three factors. First, fewer workers are offered coverage through an employer when grandfathered plans are eliminated, so more enroll in coverage in the individual market or through Medicaid. Second, the price of some insurance policies for a given level of generosity is higher when grandfathering is eliminated, which drives some eligible individuals into publicly sponsored insurance programs. Finally, some employers may offer plans with lower actuarial values in the exchanges when grandfathering is eliminated, which may cause Medicaid-eligible workers to move into the
Medicaid program.
The increase in Medicaid and nongroup exchange enrollment without grandfathering increases costs to the federal government. Annual new government spending increases by $5.2 billion when grandfathering is eliminated in the α equals 1 scenario (Table 1), an increase of 4.3 percent relative to the scenario that allows grandfathering. Simultaneously, the decline in ESI enrollment and firm offering when grandfathering is eliminated reduces employer spending on health insurance. When α equals 1, employer spending among firms with 100 or fewer workers falls from
$190.5 billion with grandfathering to $179.1 billion without grandfathering. This decline occurs not only because fewer firms offer coverage when the option to grandfather is unavailable, but also because some firms offer less-generous plans. As modeled, both the bronze and platinum plans have lower actuarial values than grandfathered ESI plans for small firms.
Post-reform, we find that approximately 38 percent of individuals enrolled in small group policies in the exchanges are offered bronze or silver plans, suggesting a large shift into lower actuarial value coverage.
It is possible that firms that discontinue coverage or switch to less-generous plans will pass some of the savings back to workers in the form of increased wages. Since these wages would be taxable, government revenues could increase as a result. A limitation of this analysis is that, when calculating changes in government spending, we do not account for this potential cost offset.
When small group premiums in the traditional
ESI market are fully or partially experience-rated
( α = 1 or α = 0.25), premiums in the exchanges tend to fall when grandfathering is eliminated. For example, the small group bronze premium falls from
$3,518 to $3,379 in the fully experience-rated scenario ( α = 1) when grandfathering is eliminated, a difference of 4 percent. This decline occurs because the lower-risk population that would have chosen grandfathered ESI plans is forced into the exchanges when grandfathered plans are eliminated. The decline in premiums is less pronounced when grandfathered premiums are partially experience-rated ( α = 0.25), since premiums in the grandfathered market approximate a modified community rating scenario, similar to the exchange market.
When premiums in the small group market are fully community-rated (Table 3), small group premiums in the exchanges increase when the grandfathered market is eliminated. This occurs because a higher-risk group prefers the full community rating offered on grandfathered plans relative to the 3:1 rate banding offered in the exchanges.
9 When the option to grandfather is eliminated, these firms are forced into the exchanges, and exchange premiums increase.
This result suggests that risk segmentation caused by grandfathering keeps people enrolled in the ESI market, regardless of whether the grandfathered market is the lower-risk pool ( α = 1 or α = 0.25) or the higher-risk pool ( α = 0).
9 In Table 3, the gold plan premium is lower than the traditional ESI premium, and—since these plans have comparable actuarial values—it may seem as if there is no reason for a firm to stay grandfathered. However, because of the 3:1 rate bands on age, the exchange premium offered to any given firm will vary depending on the age composition of its workers. As a result, exchange premiums are higher than grandfathered premiums for some firms. We also note that some firms will opt to stay in the grandfathered plans even if the exchanges would represent a cost savings for a subset of workers, as long as aggregate worker utility is higher in the grandfathered market. This effect helps to sustain the grandfathered market in the community-rated case.
Without grandfathering, more people are enrolled in
Medicaid, and more people are enrolled in the nongroup exchanges.
– 6 –
Inertia causes some firms to remain in the grandfathered market even though this decision is suboptimal for them.
Split Risk Pools, Inertia
The main results described above are similar in scenarios that allow for inertia in firm decisionmaking
(Tables 4, 5, and 6, beginning on p. 11). Specifically, fewer firms offer coverage when the grandfathered market is eliminated. As a result, employer spending falls, Medicaid enrollment increases, and government spending goes up. The increase in government spending may be partially offset by a potential increase in taxable compensation when health benefits are eliminated or reduced. However, this effect is not captured in our model.
By definition, inertia causes some firms to remain in the grandfathered market even though this decision is suboptimal for them (e.g., they have high-risk workers and face higher premiums in the grandfathered market). When the grandfathered market is eliminated, firms no longer have the option to make a suboptimal choice, so results in Tables 4, 5, and
6 reflect both the elimination of the grandfathered market and, for some firms, the movement from a suboptimal to an optimal choice. This leads to some seemingly anomalous findings. For example, small-employer spending falls by 22 percent when we eliminate grandfathering in the fully experiencerated scenario with inertia (Table 4), compared with only 6 percent in the comparable scenario without inertia (Table 1). The large decline in spending is due to the fact that some firms remain in high-cost grandfathered plans in the initial scenario and— when the option to grandfather is eliminated—these firms move into less-costly plans in the exchanges.
We did not see such a large change in Tables 1, 2, and 3 because, without inertia, firms do not maintain grandfathered plans if they can get a better value in the exchanges. Similarly, exchange premiums go up when grandfathering is eliminated in the no inertia case with α equal to 0.25 (partial experience rating).
This increase stems from the fact that some highrisk firms remain in the grandfathered market in the initial scenario, even though they could have saved money by moving to the exchanges.
Comparing the inertia cases with the no inertia cases, it appears that a higher share of firms with 100 or fewer workers offer coverage when we allow for inertia (Panel A, line 1). However, we recommend caution in interpreting this result, since there tends to be a lot of variance in the firm-level results. Firmlevel results are imprecise because the Kaiser/HRET data used to populate the model undersample small firms (this issue is described more thoroughly in
Appendix C of Eibner et al., forthcoming). When we consider the share of workers at offering firms (Panel
A, line 2), results are stable with and without inertia.
Combined Risk Pools, No Inertia
The general pattern described in the Split Pools,
No Inertia section is also similar when the small group and nongroup markets are combined in the exchanges (Tables 7, 8, and 9, beginning on p. 14).
Again, when grandfathering is eliminated, employer offer rates fall, Medicaid and nongroup exchange enrollment increases, government spending increases, and employer spending falls. We also find a slight decrease in the number of people with insurance, ranging from 200,000 to 400,000 (see Tables 7, 8, and 9, Panel C).
When exchange risk pools are combined, premiums faced by small group enrollees in the exchanges reflect the experience of those insured through both the nongroup and small group markets. As a result, small group exchange enrollees are influenced not only by their employer’s ability to offer a grandfathered plan, but also by the dynamics of the individual market. Relative to the split risk pools scenarios
(Tables 1, 2, and 3), exchange premiums for the small group market are higher with the combined risk pool. Conversely, exchange premiums for the nongroup market are lower with the combined risk pool.
This result can be seen by comparing the combined exchange premiums reported in Table 7 with the individual and small group premiums reported in Table 1.
The higher premiums for small group enrollees in the combined scenarios cause fewer people to be enrolled in the small group exchange market when risk pools are combined, relative to the split risk pools scenarios. Conversely, when risk pools are combined, more people are enrolled in the nongroup exchange market. For example, in comparing the grandfathered scenarios in Table 7 with those reported in Table 1, we find that 3 million additional people are enrolled in the small group exchange when risk pools are split, and 4 million fewer people are enrolled in the individual exchanges.
Compared with the split risk pools scenarios, the change in government spending when grandfathering is eliminated is less pronounced in the combined risk pool scenarios. One reason for this effect is that, when the less-risky grandfathered enrollees enter the exchange market, exchange premiums fall for both small group and individual enrollees (at least in the
α = 1 and α = 0.25 scenarios). Since many individual exchange enrollees receive government subsidies, government cost per subsidized enrollee falls. In some cases, the decline in spending per enrollee is enough to outweigh small increases in individual exchange enrollment when grandfathering is eliminated. For example, government spending on premium subsidies falls by 1 percent when grandfathering is eliminated
– 7 – in the combined scenario with α equal to 1 (Table 7).
In the comparable scenario with split risk pools, government spending on premium subsidies increases by
2.8 percent when the option to grandfather is eliminated (Table 1). There are also compositional effects that influence results in the combined versus split risk pools scenarios. For example, when risk pools in the individual exchanges are combined, the population enrolled in Medicaid in the grandfathered scenario is slightly more expensive than the population enrolled when risk pools are split (this can be seen by comparing Medicaid spending per beneficiary in Table 1 with Medicaid spending per beneficiary in Table 7).
Summary and Discussion
As with any modeling results, these findings are subject to a large degree of uncertainty stemming from factors such as the level of administrative costs in health insurance exchanges, inertia in decisionmaking, and the government’s ability to effectively enforce the individual mandate. Because of these factors, we are more confident about the directionality and the general magnitude of the results than we are about the specific point estimates. With these caveats, we find that the elimination of grandfathering in the small group market is associated with a reduction in employer offer rates and a reduction in the number of people enrolled in ESI. The decline in employer offer rates leads to a decline in the number of people with insurance, with reductions ranging from 200,000 to 1,400,000, depending on assumptions about risk pooling and inertia.
Because some employers drop coverage and others reduce the generosity of benefits offered when grandfathering is eliminated, employer spending for small businesses is lower if there is no option to offer a grandfathered plan. As the number of people enrolled in employer-sponsored coverage falls, the number of people enrolled in Medicaid and subsidized exchange policies increases. These factors lead to an increase in government spending. When α equals 0.25 (potentially the most realistic representation of the current status quo), the increase in government spending following the reform would be 3.4 percent higher if grandfathering were eliminated. However, this result should be interpreted cautiously because we do not account for potential increases in tax revenue that might occur if employers who eliminate or reduce the generosity of health benefits pass some of these savings back to workers in the form of taxable wages.
To partially address this issue, we did a rough calculation where we assumed that 100 percent of prior health insurance spending would be passed back to workers as wages if an employer dropped coverage due to the elimination of grandfathering. By applying the average marginal tax rate at each firm to the estimated wage pass-back, we calculate that the government would receive $2.2 billion dollars in additional tax revenue if grandfathering were to be eliminated.
10
However, this result rests on the assumption that
100 percent of savings among firms that drop coverage would be passed back to workers. Simultaneously, it assumes that no savings would be passed back to workers if firms decreased the actuarial value of plans in response to the elimination of the grandfathered market.
We analyzed the effects of grandfathering under a variety of assumptions about the degree of community rating in the traditional ESI market, the degree of inertia in firm decisionmaking, and whether individual and small group risk pools are combined or segregated in the health insurance exchanges. The main results are very stable to all of these alternative assumptions. In all of the scenarios considered, when the grandfathered market is eliminated, ESI enrollment falls, Medicaid enrollment increases, government spending increases, and employer spending falls. Overall, these results suggest that, while grandfathering may lead to slightly higher exchange premiums (1.3 percent higher when fathering is also associated with higher ESI enrollment and lower government spending. As a result, grandfathering may be an effective policy if the goal is to maximize the number of people enrolled in employment-based coverage.
■
α = 0.25), grand-
10 This calculation includes federal income taxes, Social Security (Federal
Insurance Contribution Act [FICA]) taxes, and state income taxes. We do not incorporate multiplier effects (i.e., any additional economic stimulus caused by the wage change that could increase the tax base even further).
The calculation applies to the α equals 0.25, no inertia scenario.
While grandfathering may lead to slightly higher exchange premiums, grandfathering is also associated with higher employersponsored insurance enrollment and lower government spending.
– 8 –
Table 1
Split Risk Pools, No Inertia, α = 1
A. Offer rates
Offer rates, firms with ≤100 workers
Share of workers at offering firms (among firms with ≤100 workers)
B. Premiums (in 2010 dollars)
ESI premium (firms with 101+ workers)
ESI premium (firms with ≤100 workers)
Small group exchange, bronze
Small group exchange, silver
Small group exchange, gold
Small group exchange, platinum
Nongroup exchange, bronze
Nongroup exchange, silver
Nongroup exchange, gold
Nongroup exchange, platinum
Medicaid spending per beneficiary
C. Coverage among nonelderly (in millions)
Total insured
Medicaid
Large group ESI
Small group ESI
Traditional
Exchange
Individual exchange
Nongroup or other
Total uninsured
D. Health expenditure (in billions of 2010 dollars)
Total national health expenditure
New government spending
New Medicaid spending
Exchange premium subsidies
Exchange cost share subsidies
Revenue from penalties
Total employer spending (≤100 workers)
Total employer spending (101+ workers)
With
Grandfathering
(Equilibrium)
Without
Grandfathering
(Equilibrium)
80.7%
90.3%
$5,732
$3,604
$3,518
$4,186
$4,880
$5,599
$4,357
$5,185
$6,044
$6,935
$6,576
258.7
49.5
110.1
55.6
12.7
42.8
27.5
15.9
18.2
$2,369
$122.2
$71.2
$60.3
$5.0
–$14.4
$190.5
$496.9
75.3%
86.4%
$5,745
N/A
$3,379
$4,021
$4,688
$5,379
$4,301
$5,118
$5,966
$6,846
$6,464
257.8
51.2
110.2
52.1
0
52.1
28.5
15.9
19.0
$2,368
$127.4
$76.2
$62.0
$5.1
–$16.0
$179.1
$497.2
Difference
–5.4 ppts.
–3.9 ppts.
$13
N/A
–$139
–$165
–$192
–$220
–$56
–$67
–$78
–$89
–$112
–$1.0
$5.2
$5.0
$1.7
$0.1
–$1.6
–$11.4
$0.3
–0.9
1.7
0.1
–3.5
–12.7
9.3
1.0
0.0
0.8
% Change
–6.7%
–4.3%
0.2%
N/A
–4.0%
–3.9%
–3.9%
–3.9%
–1.3%
–1.3%
–1.3%
–1.3%
–1.7%
0.0%
4.3%
7.0%
2.8%
2.0%
11.1%
–6.0%
0.1%
–0.3%
3.4%
0.1%
–6.3%
–100.0%
21.7%
3.6%
0.0%
4.4%
– 9 –
Table 2
Split Risk Pools, No Inertia, α = 0.25
A. Offer rates
Offer rates, firms with ≤100 workers
Share of workers at offering firms (among firms with ≤100 workers)
B. Premiums (in 2010 dollars)
ESI premium (firms with 101+ workers)
ESI premium (firms with ≤100 workers)
Small group exchange, bronze
Small group exchange, silver
Small group exchange, gold
Small group exchange, platinum
Nongroup exchange, bronze
Nongroup exchange, silver
Nongroup exchange, gold
Nongroup exchange, platinum
Medicaid spending per beneficiary
C. Coverage among nonelderly (in millions)
Total insured
Medicaid
Large group ESI
Small group ESI
Traditional
Exchange
Individual exchange
Nongroup or other
Total uninsured
D. Health expenditure (in billions of 2010 dollars)
Total national health expenditure
New government spending
New Medicaid spending
Exchange premium subsidies
Exchange cost share subsidies
Revenue from penalties
Total employer spending (≤100 workers)
Total employer spending (101+ workers)
With
Grandfathering
(Equilibrium)
Without
Grandfathering
(Equilibrium)
80.9%
89.1%
$5,733
$4,759
$3,422
$4,072
$4,747
$5,447
$4,308
$5,127
$5,976
$6,858
$6,552
258.4
49.9
110.0
54.6
13.4
41.2
28.1
15.9
18.4
$2,368
$124.1
$73.5
$60.5
$5.0
–$15.0
$194.4
$498.2
75.3%
86.4%
$5,746
N/A
$3,377
$4,019
$4,685
$5,376
$4,306
$5,124
$5,973
$6,854
$6,464
257.8
51.2
110.2
52.2
0
52.2
28.4
15.9
19.0
$2,368
$128.3
$77.1
$62.0
$5.1
–$16.0
$179.2
$497.3
Difference
–5.6 ppts.
–2.7 ppts.
$13
N/A
–$45
–$53
–$62
–$71
–$2
–$3
–$3
–$4
–$88
–0.6
1.3
0.2
–2.4
–13.4
11.0
0.3
0.0
0.6
$0.0
$4.2
$3.6
$1.5
$0.1
–$1.0
–$15.2
–$0.9
% Change
–6.9%
–3.0%
0.2%
N/A
–1.3%
–1.3%
–1.3%
–1.3%
0.0%
–0.1%
–0.1%
–0.1%
–1.3%
–0.2%
2.6%
0.2%
–4.4%
–100.0%
26.7%
1.1%
0.0%
3.3%
0.0%
3.4%
4.9%
2.5%
2.0%
6.7%
–7.8%
–0.2%
– 10 –
Table 3
Split Risk Pools, No Inertia, α = 0
A. Offer rates
Offer rates, firms with ≤100 workers
Share of workers at offering firms (among firms with ≤100 workers)
B. Premiums (in 2010 dollars)
ESI premium (firms with 101+ workers)
ESI premium (firms with ≤100 workers)
Small group exchange, bronze
Small group exchange, silver
Small group exchange, gold
Small group exchange, platinum
Nongroup exchange, bronze
Nongroup exchange, silver
Nongroup exchange, gold
Nongroup exchange, platinum
Medicaid spending per beneficiary
C. Coverage among nonelderly (in millions)
Total insured
Medicaid
Large group ESI
Small group ESI
Traditional
Exchange
Individual exchange
Nongroup or other
Total uninsured
D. Health expenditure (in billions of 2010 dollars)
Total national health expenditure
New government spending
New Medicaid spending
Exchange premium subsidies
Exchange cost share subsidies
Revenue from penalties
Total employer spending (≤100 workers)
Total employer spending (101+ workers)
With
Grandfathering
(Equilibrium)
Without
Grandfathering
(Equilibrium)
80.6%
89.5%
$5,728
$4,993
$3,210
$3,820
$4,452
$5,109
$4,304
$5,122
$5,971
$6,852
$6,540
258.5
49.9
110.0
54.9
12.6
42.2
27.8
15.9
18.3
$2,371
$128.1
$78.7
$59.2
$5.0
–$14.8
$187.2
$497.4
75.1%
86.3%
$5,738
N/A
$3,376
$4,017
$4,683
$5,374
$4,313
$5,133
$5,984
$6,866
$6,466
257.8
51.2
110.1
52.1
0
52.2
28.5
15.9
19.0
$2,368
$134.1
$82.7
$62.0
$5.1
–$15.7
$178.9
$498.1
Difference
–5.5 ppts.
–3.2 ppts.
$10
N/A
$166
$197
$231
$265
$9
$11
$13
$14
–$74
–0.7
1.3
0.1
–2.8
–12.6
10.0
0.7
0.0
0.7
–$3.0
$6.0
$4.0
$2.8
$0.1
–$0.9
–$8.3
$0.7
% Change
–6.8%
–3.6%
0.2%
N/A
5.2%
5.2%
5.2%
5.2%
0.2%
0.2%
0.2%
0.2%
–1.1%
–0.3%
2.6%
0.1%
–5.1%
–100.0%
23.7%
2.5%
0.0%
3.8%
-0.1%
4.7%
5.1%
4.7%
2.0%
6.1%
–4.4%
0.1%
– 11 –
Table 4
Split Risk Pools, Inertia, α = 1
A. Offer rates
Offer rates, firms with ≤100 workers
Share of workers at offering firms (among firms with ≤100 workers)
B. Premiums (in 2010 dollars)
ESI premium (firms with 101+ workers)
ESI premium (firms with ≤100 workers)
Small group exchange, bronze
Small group exchange, silver
Small group exchange, gold
Small group exchange, platinum
Nongroup exchange, bronze
Nongroup exchange, silver
Nongroup exchange, gold
Nongroup exchange, platinum
Medicaid spending per beneficiary
C. Coverage among nonelderly (in millions)
Total insured
Medicaid
Large group ESI
Small group ESI
Traditional
Exchange
Individual exchange
Nongroup or other
Total uninsured
D. Health expenditure (in billions of 2010 dollars)
Total national health expenditure
New government spending
New Medicaid spending
Exchange premium subsidies
Exchange cost share subsidies
Revenue from penalties
Total employer spending (≤100 workers)
Total employer spending (101+ workers)
With
Grandfathering
(Equilibrium)
Without
Grandfathering
(Equilibrium)
84.3%
90.9%
$5,745
$5,307
$3,549
$4,224
$4,923
$5,650
$4,351
$5,178
$6,036
$6,926
$6,874
259.2
47.3
111.2
55.8
49.8
6.0
28.9
15.9
17.7
$2,367
$124.2
$71.8
$61.9
$5.0
–$14.5
$229.4
$498.1
75.3%
86.4%
$5,745
N/A
$3,379
$4,021
$4,688
$5,379
$4,301
$5,118
$5,966
$6,846
$6,464
257.8
51.2
110.2
52.1
0
51.1
28.5
15.9
19.0
$2,368
$127.4
$76.2
$62.0
$5.1
–$16.0
$179.1
$497.2
Difference
–9.0 ppts.
–4.5 ppts.
$0
N/A
–$170
–$203
–$235
–$271
–$50
–$60
–$70
–$80
–$410
–1.4
3.9
–1.0
–3.7
–49.8
45.1
–0.4
0.0
1.3
$1.0
$3.2
$4.4
$0.1
$0.1
–$1.5
–$50.3
–$0.9
% Change
–10.7%
–5.0%
0.0%
N/A
–4.8%
–4.8%
–4.8%
–4.8%
–1.1%
–1.2%
–1.2%
–1.2%
–6.0%
–0.5%
8.2%
–0.9%
–6.6%
–100.0%
751.7%
–1.4%
0.0%
7.3%
0.0%
2.6%
6.1%
0.2%
2.0%
10.3%
–21.9%
–0.2%
– 12 –
Table 5
Split Risk Pools, Inertia, α = 0.25
A. Offer rates
Offer rates, firms with ≤100 workers
Share of workers at offering firms (among firms with ≤100 workers)
B. Premiums (in 2010 dollars)
ESI premium (firms with 101+ workers)
ESI premium (firms with ≤100 workers)
Small group exchange, bronze
Small group exchange, silver
Small group exchange, gold
Small group exchange, platinum
Nongroup exchange, bronze
Nongroup exchange, silver
Nongroup exchange, gold
Nongroup exchange, platinum
Medicaid spending per beneficiary
C. Coverage among nonelderly (in millions)
Total insured
Medicaid
Large group ESI
Small group ESI
Traditional
Exchange
Individual exchange
Nongroup or other
Total uninsured
D. Health expenditure (in billions of 2010 dollars)
Total national health expenditure
New government spending
New Medicaid spending
Exchange premium subsidies
Exchange cost share subsidies
Revenue from penalties
Total employer spending (≤100 workers)
Total employer spending (101+ workers)
With
Grandfathering
(Equilibrium)
Without
Grandfathering
(Equilibrium)
85.7%
90.8%
$5,770
$5,551
$3,235
$3,849
$4,487
$5,149
$4,337
$5,162
$6,017
$6,904
$6,793
259.2
47.7
111.2
54.9
48.7
6.3
29.5
15.9
17.6
$2,369
$125.8
$71.2
$63.8
$5.1
–$14.3
$242.4
$500.3
75.3%
86.4%
$5,746
N/A
$3,377
$4,019
$4,685
$5,376
$4,306
$5,124
$5,973
$6,854
$6,464
257.8
51.2
110.2
52.2
0
51.2
28.4
15.9
19.0
$2,368
$128.3
$77.1
$62.0
$5.1
–$16.0
$179.2
$497.3
Difference
–10.4 ppts.
–4.4 ppts.
–$24
N/A
$142
$170
$198
$227
–$31
–$38
–$44
–$50
–$329
–$1.0
$2.5
$5.9
–$1.8
$0.0
–$1.7
–$63.2
–$3.0
–1.4
3.5
–1.0
–2.7
–48.7
44.9
–1.1
0.0
1.4
% Change
–12.1%
–4.8%
–0.4%
N/A
4.4%
4.4%
4.4%
4.4%
–0.7%
–0.7%
–0.7%
–0.7%
–4.8%
–0.5%
7.3%
–0.9%
–4.9%
–100.0%
712.7%
–3.7%
0.0%
8.0%
0.0%
2.0%
8.3%
–2.8%
0.0%
11.9%
–26.1%
–0.6%
– 13 –
Table 6
Split Risk Pools, Inertia, α = 0
A. Offer rates
Offer rates, firms with ≤100 workers
Share of workers at offering firms (among firms with ≤100 workers)
B. Premiums (in 2010 dollars)
ESI premium (firms with 101+ workers)
ESI premium (firms with ≤100 workers)
Small group exchange, bronze
Small group exchange, silver
Small group exchange, gold
Small group exchange, platinum
Nongroup exchange, bronze
Nongroup exchange, silver
Nongroup exchange, gold
Nongroup exchange, platinum
Medicaid spending per beneficiary
C. Coverage among nonelderly (in millions)
Total insured
Medicaid
Large group ESI
Small group ESI
Traditional
Exchange
Individual exchange
Nongroup or other
Total uninsured
D. Health expenditure (in billions of 2010 dollars)
Total national health expenditure
New government spending
New Medicaid spending
Exchange premium subsidies
Exchange cost share subsidies
Revenue from penalties
Total employer spending (≤100 workers)
Total employer spending (101+ workers)
With
Grandfathering
(Equilibrium)
Without
Grandfathering
(Equilibrium)
85.5%
90.2%
$5,775
$5,547
$3,020
$3,594
$4,190
$4,808
$4,355
$5,182
$6,041
$6,932
$6,669
259.0
47.8
111.2
54.9
48.8
6.1
29.3
15.9
17.8
$2,371
$126.0
$71.2
$64.3
$5.1
–$14.6
$243.4
$500.6
75.1%
86.3%
$5,738
N/A
$3,376
$4,017
$4,683
$5,374
$4,313
$5,133
$5,984
$6,866
$6,466
257.8
51.2
110.1
52.1
0
51.2
28.5
15.9
19.0
$2,368
$134.1
$82.7
$62.0
$5.1
–$15.7
$178.9
$498.1
Difference
–10.4 ppts.
–3.9 ppts.
–$37
N/A
$356
$423
$493
$566
–$42
–$49
–$57
–$66
–$203
–$3.0
$8.1
$11.5
–$2.3
$0.0
–$1.1
–$64.5
–$2.5
–1.2
3.4
–1.1
–2.8
–48.8
45.1
–0.8
0.0
1.2
% Change
–12.2%
–4.3%
–0.5%
7.1%
–1.0%
–5.1%
–100.0%
739.3%
–2.7%
0.0%
6.7%
–0.1%
6.4%
16.2%
–3.6%
0.0%
7.5%
–26.5%
–0.5%
–0.6%
N/A
11.8%
11.8%
11.8%
11.8%
–1.0%
–0.9%
–0.9%
–1.0%
–3.0%
– 14 –
Table 7
Combined Risk Pools, No Inertia, α = 1
A. Offer rates
Offer rates, firms with ≤100 workers
Share of workers at offering firms (among firms with ≤100 workers)
B. Premiums (in 2010 dollars)
ESI premium (firms with 101+ workers)
ESI premium (firms with ≤100 workers)
Exchange, bronze
Exchange, silver
Exchange, gold
Exchange, platinum
Medicaid spending per beneficiary
C. Coverage among nonelderly (in millions)
Total insured
Medicaid
Large group ESI
Small group ESI
Traditional
Exchange
Individual exchange
Nongroup or other
Total uninsured
D. Health expenditure (in billions of 2010 dollars)
Total national health expenditure
New government spending
New Medicaid spending
Exchange premium subsidies
Exchange cost share subsidies
Revenue from penalties
Total employer spending (≤100 workers)
Total employer spending (101+ workers)
With
Grandfathering
(Equilibrium)
Without
Grandfathering
(Equilibrium)
79.7%
89.0%
$5,736
$3,759
$3,854
$4,586
$5,346
$6,135
$6,675
259.5
48.7
109.6
53.4
13.5
39.9
31.9
15.9
17.3
$2,372
$113.6
$71.1
$51.6
$5.2
–$14.4
$200.6
$495.9
73.6%
85.2%
$5,716
N/A
$3,767
$4,482
$5,225
$5,996
$6,583
259.3
49.9
109.6
49.8
0
49.8
34.2
15.9
17.6
$2,374
$115.3
$74.0
$51.1
$5.3
–$15.1
$194.4
$495.2
Difference
–6.1 ppts.
–3.8 ppts.
–0.2
1.2
0.0
–3.6
–13.5
9.9
2.3
0.0
0.3
–$20
N/A
–$87
–$104
–$121
–$139
–$92
$2.0
$1.7
$2.9
–$0.5
$0.1
–$0.7
–$6.2
–$0.7
% Change
–7.7%
–4.3%
–0.1%
2.5%
0.0%
–6.7%
–100.0%
24.8%
7.2%
0.0%
1.7%
–0.3%
N/A
–2.3%
–2.3%
–2.3%
–2.3%
–1.4%
0.1%
1.5%
4.1%
–1.0%
1.9%
4.9%
–3.1%
–0.1%
– 15 –
Table 8
Combined Risk Pools, No Inertia, α = 0.25
A. Offer rates
Offer rates, firms with ≤100 workers
Share of workers at offering firms (among firms with ≤100 workers)
B. Premiums (in 2010 dollars)
ESI premium (firms with 101+ workers)
ESI premium (firms with ≤100 workers)
Exchange, bronze
Exchange, silver
Exchange, gold
Exchange, platinum
Medicaid spending per beneficiary
C. Coverage among nonelderly (in millions)
Total insured
Medicaid
Large group ESI
Small group ESI
Traditional
Exchange
Individual exchange
Nongroup or other
Total uninsured
D. Health expenditure (in billions of 2010 dollars)
Total national health expenditure
New government spending
New Medicaid spending
Exchange premium subsidies
Exchange cost share subsidies
Revenue from penalties
Total employer spending (≤100 workers)
Total employer spending (101+ workers)
With
Grandfathering
(Equilibrium)
Without
Grandfathering
(Equilibrium)
76.8%
88.2%
$5,729
$5,070
$3,819
$4,545
$5,298
$6,079
$6,631
259.3
49.1
109.6
52.3
15.2
37.1
32.4
15.9
17.5
$2,372
$114.6
$72.5
$51.4
$5.2
–$14.6
$210.9
$495.7
73.6%
85.2%
$5,717
N/A
$3,746
$4,457
$5,196
$5,963
$6,571
259.1
50.0
109.6
49.8
0.0
49.8
33.9
15.9
17.7
$2,373
$117.0
$75.1
$51.7
$5.3
–$15.1
$195.8
$495.3
Difference
–3.2 ppts.
–3.0 ppts.
–0.2
0.9
0.0
–2.5
–15.2
12.7
1.5
0.0
0.2
–$12
N/A
–$73
–$88
–$102
–$116
–$60
$1.0
$2.4
$2.6
$0.3
$0.1
–$0.5
–$15.1
–$0.4
% Change
–4.2%
–3.4%
–0.1%
1.8%
0.0%
–4.8%
–100.0%
34.2%
4.6%
0.0%
1.1%
–0.2%
N/A
–1.9%
–1.9%
–1.9%
–1.9%
–0.9%
0.0%
2.1%
3.6%
0.6%
1.9%
3.4%
–7.2%
–0.1%
– 16 –
Table 9
Combined Risk Pools, No Inertia, α = 0
A. Offer rates
Offer rates, firms with ≤100 workers
Share of workers at offering firms (among firms with ≤100 workers)
B. Premiums (in 2010 dollars)
ESI premium (firms with 101+ workers)
ESI premium (firms with ≤100 workers)
Exchange, bronze
Exchange, silver
Exchange, gold
Exchange, platinum
Medicaid spending per beneficiary
C. Coverage among nonelderly (in millions)
Total insured
Medicaid
Large group ESI
Small group ESI
Traditional
Exchange
Individual exchange
Nongroup or other
Total uninsured
D. Health expenditure (in billions of 2010 dollars)
Total national health expenditure
New government spending
New Medicaid spending
Exchange premium subsidies
Exchange cost share subsidies
Revenue from penalties
Total employer spending (≤100 workers)
Total employer spending (101+ workers)
With
Grandfathering
(Equilibrium)
Without
Grandfathering
(Equilibrium)
78.9%
88.4%
$5,728
$5,073
$3,720
$4,427
$5,161
$5,922
$6,696
259.7
48.6
109.4
52.2
15.5
36.7
33.6
15.9
17.2
$2,376
$117.9
$78.3
$48.9
$5.2
–$14.5
$206.2
$495.3
73.6%
85.3%
$5,716
N/A
$3,767
$4,483
$5,226
$5,997
$6,583
259.3
49.8
109.6
49.8
0.0
49.8
34.2
15.9
17.5
$2,374
$121.8
$80.4
$51.1
$5.3
–$15.1
$194.6
$495.2
Difference
–5.3 ppts.
–3.1 ppts.
–0.4
1.2
0.2
–2.4
–15.5
13.1
0.6
0.0
0.3
–$12
N/A
$47
$56
$65
$75
–$113
–$2.0
$3.9
$2.1
$2.2
$0.1
–$0.6
–$11.6
–$0.1
% Change
–6.7%
–3.5%
–0.2%
2.5%
0.2%
–4.6%
–100.0%
35.7%
1.8%
0.0%
1.7%
–0.2%
N/A
1.3%
1.3%
1.3%
1.3%
–1.7%
–0.1%
3.3%
2.7%
4.5%
1.9%
4.1%
–5.6%
0.0%
– 17 –
References
Blumberg LJ, Shen YC, Nichols LM, Buettgens M,
Dubay LC, and McMorrow S, The Health Insurance
Reform Simulation Model (HIRSM): Methodological
Detail and Prototypical Simulation Results ,
Washington, D.C.: The Urban Institute, July 2003.
As of May 27, 2010: http://www.urban.org/UploadedPDF/410867_
HIRSM_Report.pdf
Buntin MB, Escarce JJ, Kapur K, Yegian JM, and
Marquis MS, “Trends and Variability in Individual
Insurance Products in California,” Health Affairs ,
Vol. 22, July–December 2003, Suppl. Web
Exclusives: W3-449–459.
Eibner CE, Girosi F, Price CP, Cordova A, Hussey
PS, Beckman A, and McGlynn EA, “Establishing
State Health Insurance Exchange: Implications for Health Insurance Enrollment, Spending, and
Small Businesses,” Santa Monica, Calif.: RAND
Corporation, forthcoming.
Fernandez B, “Grandfathered Health Plans Under
PPACA (P.L. 111-148),” Congressional Research
Service, 7-5700, April 7, 2010.
Gabel J, McDevitt R, Gandolfo L, Pickreign J,
Hawkins S, and Fahlman C, “Generosity and
Adjusted Premiums in Job-Based Insurance: Hawaii
Is Up, Wyoming Is Down,” Health Affairs , Vol. 25,
No. 3, 2006, pp. 832–843.
GAO— see U.S. General Accounting Office.
PPACA— see Patient Protection and Affordable Care
Act.
Patient Protection and Affordable Care Act , Public
Law 111-148, 111th Cong., 1st Sess., March 23, 2010.
As of May 27, 2010: http://www.govtrack.us/congress/bill.xpd?bill= h111-3590
Rotemberg JJ, “Sticky Prices in the United States,”
Journal of Political Economy , Vol. 90, No. 6,
December 1982, pp. 1187–1211.
U.S. General Accounting Office, Health Insurance
Regulation: Variation in Recent State Small Employer
Health Insurance Reforms , GAO/HEHS-95-161FS,
Washington, D.C., June 12, 1995.
RAND publications are available at www.rand.org
The RAND Corporation is a nonprofit institution that helps improve policy and decisionmaking through research and analysis.
RAND’s publications do not necessarily reflect the opinions of its research clients and sponsors. R ® is a registered trademark.
OP-313-DOL (2010)
R
Headquarters Campus
1776 main street p.o. Box 2138 santa monica, Ca
90407-2138 tel 310.393.0411
Fax 310.393.4818
Washington Office
1200 south hayes street arlington, va 22202-5050 tel 703.413.1100
Fax 703.413.8111
Pittsburgh Office
4570 Fifth avenue, suite 600 pittsburgh, pa 15213-2665 tel 412.683.2300
Fax 412.683.2800
New Orleans Office rand gulf states policy institute
650 poydras street, suite 1400 new orleans, la 70130 tel 504.558.1975
Fax 504.299.3471
Jackson Office rand gulf states policy institute p.o. Box 3788
Jackson, ms 39207-3788 tel 601.979.2449
Fax 601.354.3444
Boston Office
20 park plaza, suite 720
Boston, ma 02116 tel 617.338.2059
Fax 617.357.7470
Doha Office
RAND-Qatar Policy Institute
P.O. Box 23644
Doha, Qatar tel +974.492.7400
Fax +974.492.7410
RAND Europe westbrook Centre milton road
Cambridge CB4 1yg united Kingdom tel +44.1223.353.329
Fax +44.1223.358.845
37, square de meeus
B-1000 Brussels
Belgium tel +32.2.791.7500
Fax +32.2.791.7900 www.rand.org