Anxiolytic and hypnotic drugs 1 ...
advertisement
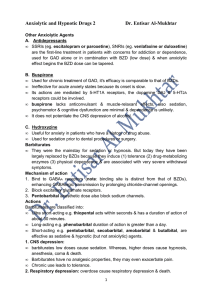
Anxiolytic and hypnotic drugs 1 Dr. Entisar Al-Mukhtar Anxiety is an unpleasant state of tension, apprehension, or uneasiness (a fear that seems to arise from a unknown source). • The physical symptoms of severe anxiety are tachycardia, sweating, trembling & palpitations) & involve sympathetic activation. • Episodes of mild anxiety are common life experiences & do not warrant treatment. Symptoms of severe, chronic, debilitating anxiety may be treated with anti-anxiety drugs (anxiolytic or minor tranquilizers) and/or some form of behavioral therapy or psychotherapy. . Benzodiazepines (BZDs) • Are the most widely used anxiolytic drugs. They have largely replaced barbiturates & meprobamate in the treatment of anxiety or insomnia, because BZDs are safer & more effective. • Certain antidepressants with anxiolytic action, such as the SSRIs, are preferred in many cases, and non BZD hypnotics and antihistamines may be preferable for insomnia. Mechanism of action BZDs modulate GABA effects by binding to a specific site on GABA receptors which are sometimes labeled “BZ receptors.” In the CNS the subtype receptors are designated as BZ1 and BZ2. • BZD increases the affinity of GABA to GABA receptors thus, increase the frequency of chloride channel openings resulting in a small hyperpolarization. Actions and therapeutic uses • BZDs show small differences in their relative anxiolytic, anticonvulsant & sedative properties. Also their duration of action are widely varies, and pharmacokinetic considerations are often important in choosing one BZD over another. • BZDs are used to treat the following: 1. Anxiety disorders: • At low doses, BZDs inhibit neuronal circuits in the limbic system of the brain. BZDs are effective for the treatment of anxiety symptoms secondary to panic disorder, generalized anxiety disorder (GAD), social anxiety disorder, performance anxiety, posttraumatic stress disorder, obsessive-compulsive disorder (OCD), and extreme anxiety due to specific phobias such as fear of flying. • BZDs are also useful in treating anxiety accompanying depression & schizophrenia. Notes: • Because of their addiction potential, BZDs should be reserved for continued severe anxiety, and should only be used for short periods of time. • The longer-acting (eg. clonazepam, diazepam) or intermediate-acting (eg. lorazepam) BZDs are preferred for treatment of anxiety for prolonged periods. • Cross-tolerance exists between BZDs & ethanol. • Tolerance is associated with a decrease in GABA-receptor density. 1 • Alprazolam is effective for panic disorders. 2. Sleep disorders: All BZDs have sedative or calming effects, some (not all) BZDs are useful as hypnotic at higher doses. • BZDs decrease sleep onset latency, increase Stage II of non rapid eye movement (NREM) sleep whereas, decrease both REM & slow-wave sleep. • In the treatment of insomnia, it is important to balance the bedtime sedative effect with the residual sedation (“hangover”) upon awakening. • Furazepam, temazepam & triazolam are the commonly prescribed hypnotic BZDs. a. Temazepam: • Intermediate-acting BZD, useful in patients who experience frequent wakening (insomnia due to inability to stay asleep). • Should be taken 1 - 2 hours before the desired bedtime. b. Triazolam: • Short-acting BZD used to induce sleep in patients with difficulty in going to sleep. • Because tolerance to triazolam develops rapidly (within few days) & its withdrawal results in rebound insomnia this drug is best used intermittently rather than daily. • In general, hypnotics should be given for only a limited time (less than 2 - 4 weeks). Notes: • Long-acting flurazepam is rarely used due to excessive daytime sedation. 3. Amnesia: • BZDs temporally impair memory, ability to learn & form new memories is also impaired. • Shorter-acting BZDs are employed as premedication for unpleasant procedures, e.g. endoscopy, bronchoscopy, certain dental procedures & angioplasty. • BZDs cause conscious sedation. • Midazolam is used for amnesia & sedation prior to & for induction of anesthesia. 4. Seizures: Several BZDs have anticonvulsant activity. • Clonazepam is occasionally used in the treatment of certain types of seizures, whereas diazepam & lorazepam are the drugs of choice for status epilepticus. • Due to cross-tolerance, chlordiazepoxide, clorazepate, diazepam, lorazepam & oxazepam are used to treat the alcohol withdrawal-related seizures. 5. Muscular disorders: • Diazepam is used to treat muscle strain & spasticity due to multiple sclerosis & cerebral palsy. Pharmacokinetics • BZDs are lipophilic. • BZDs half-lives & duration of action determine the clinical therapeutic usefulness. 2 • BZDs are divided into short (eg. Oxazepam, Triazolam), intermediate (eg. Alprazolam, Lorazepam, Temazepam) & long acting (eg. Chlordiazepoxide, Diazepam Clorazepate & Flurazepam) agents. • Chlordiazepoxide, Diazepam are metabolized into active metabolites. • Excretion and drug redistribution outside the CNS terminate BZDs effects. • All BZDs given before birth may depress newborn CNS. Also nursing infants may exposed to BZDs effects. Dependence • Prolong use of BZDs high doses can cause psychological & physical dependence & abrupt BZDs discontinuation results in withdrawal. • Withdrawal symptoms (confusion, anxiety, agitation, restlessness, insomnia, tension and rarely seizures) induced by short acting BZDs e.g., triazolam, are more rapid & severe than those induced by long acting BZDs e.g., flurazepam. Adverse Effects • Drowsiness & confusion. • High doses cause ataxia that precludes fine motor coordination activities, such as driving an automobile. • Cognitive impairment. • Triazolam, can cause rapid tolerance, early morning insomnia, daytime anxiety, amnesia & confusion. Precautions: BZDs • Should be used cautiously in patients with liver disease. • Should be avoided in patients with acute narrow-angle glaucoma. • Sedative-hypnotic effects are enhanced by alcohol & other CNS depressants. • Overdose is seldom lethal unless other central depressants are taken concurrently. Benzodiazepine antagonist • Flumazenil is a GABA-receptor antagonist that can rapidly reverse BZDs effects. It is available for IV administration only. • frequent administration is necessary to reverse a long-acting BZD. • Flumazenil may precipitate withdrawal in dependent patients or cause seizures if a BZD is used to control seizure. Seizures may also result if the patient ingests TCAs or antipsychotics. 3