Review of methods used for quantifying excess water in Mandy Fader
advertisement

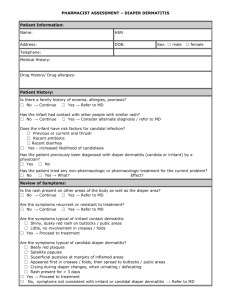
Skin Research and Technology 2010; 16: 1–8 Printed in Singapore All rights reserved doi: 10.1111/j.1600-0846.2009.00380.x r 2010 John Wiley & Sons A/S Skin Research and Technology Review of methods used for quantifying excess water in over-hydrated skin using evaporimetry Mandy Fader1, Sinead Clarke-O’Neill2, W. K. Rebecca Wong2, Bo Runeman3, Anne Farbrot3 and Alan Cottenden2 1 Continence Technology and Skin Health Group, School of Health Sciences, University of Southampton, Southampton, UK, 2Continence and Skin Technology Group, Department of Medical Physics and Bioengineering/Department of Medicine, University College London, London, UK, and 3SCA Hygiene Products AB, R&D, Göteborg, Sweden Background: Advances in diapers and skin barrier products are often aimed at reducing water penetration of the skin to prevent diaper dermatitis and evaporimetry has commonly been measured to quantify excess water in the skin. The aim of this study was to critically review the methods used to measure water vapour flux density (WVFD) using evaporimetry in order to identify a standardised methodology. Methods: We used MEDLINE (1980–2008) and hand searching to identify published papers that used evaporimetry to measure WVFD when the skin has been exposed to water/saline/urine. We compared the papers with respect to subjects, sites, methods of hydrating the skin, the conditions of logging, timing and analysing the evaporimetry data. Results: We identified 10 papers. Methods and techniques for measuring WVFD and analysing data varied consider- ably between studies and it was not possible to identify a standardised method. The main sources of error and variation are discussed. Conclusion: Little work has been carried out to establish the optimum methods and techniques needed to minimise variation in measurements of WVFD using evaporimetery. There is a need to develop more robust, standardised methods and to demonstrate their reliability for further work. D penetration of the skin and evaporimetry (use of a device which measures water evaporation from the skin) has often been used to quantify excess water in the skin as an indicator of product efficacy. Although such evaporimetry measurements have commonly been referred to as transepidermal water loss (TEWL), this term does not accurately describe measurement of water loss from the skin which has entered the stratum corneum externally such as via a wet diaper, because this water does not pass through the epidermis. We have therefore limited the use of the term TEWL to situations where water has evaporated from the skin surface having entered the stratum corneum from the tissues below and have used the term ‘baseline TEWL’ to describe trans-epidermal water loss under equilibrium conditions. Measurement of baseline TEWL is usually made either before the skin has been exposed to occlusion or external water (or both) or after full recovery from such exposure. We have used the is a common problem which affects almost all infants at some time (1) and up to about 50% of adults wearing incontinence pads (2). Over-hydrated skin is more easily damaged by friction, and is more vulnerable to chemical irritation and bacterial colonisation than dry skin (3). Based on experimental work Berg (4) postulated a ‘wet’ skin model of diaper dermatitis, whereby increased water in the skin, combined with faecal enzymes and rising pH lead to the development of dermatitis. In adults, pressure ulcers are associated with incontinence (5) and the higher coefficient of friction of over-hydrated skin is believed to contribute to mechanical abrasion damage (6), particularly over bony prominences such as the sacrum and coccyx. Reduction in skin water loading has therefore been an important goal for manufacturers of diapers and topical barrier products. Advances in diaper technology and in skin barrier products are often aimed at reducing water IAPER DERMATITIS Key words: diapers – trans-epidermal water loss – skin hydration – review & 2009 John Wiley & Sons A/S Accepted for publication 30 June 2009 1 Fader et al. general term water vapour flux density (WVFD) to describe the evaporative loss of water from the skin surface, whatever its source. The measurement of interest in wet diaper studies is the excess water in the skin and this is obtained by determining the area under the desorption curve (WVFD against time), having subtracted baseline TEWL. We have referred to this as the skin surface water loss (SSWL) and it is measured in g/m2. Other methods for measurement of excess water in the skin exist, such as measurement of impedence or conductance but these are proxy measures of water loading and measurement of water evaporation has the advantage of providing a more fundamental method of quantifying water in skin. Although the reliability and validity of evaporimetry measurement has been well described for the purposes of assessing skin barrier function, and guidance for standardisation has been published (7, 8) much less work has been published on the method when used to measure ‘wet’ skin conditions. Aim The aim of this study was to critically review the methods used to measure WVFD using evaporimetry in order to identify a standardised methodology to use for further work. Methods We searched the literature using MEDLINE (1980–2008) to identify papers where evaporimetry had been used to quantify the excess water penetration of skin following the application of wet material, with the aim of reviewing the methodologies used, rather than the outcomes of the studies. We used hand searching to complete our search. Results Ten studies were identified (3, 9–19) and they are listed in Tables 1 and 2, which summarise their key features. All used a Servo Med Evaporimeter (in its various models) (Servo Med AB, Kinna, Sweden) to measure WVFD. Zimmerer et al. (3) published the first substantial study to characterise skin that had been over hydrated by occlusion with wet diaper materials, and described in some detail the extensive WVFD measurements they made. Adults and babies 2 were studied using different fluid loadings on diapers (Dyne solution for babies) and on patches cut from diapers (urine for adults). WVFD from their skin was measured on patch/diaper removal. Each measurement involved determining the maximum WVFD value during a 20-s logging period. For adults – and a limited number of the babies – a first WVFD reading was taken immediately after patch removal, followed by periodic readings until the WVFD returned to its baseline value (after 15–20 min). WVFD was then plotted against time – having first subtracted the baseline TEWL value – and the area under the graph up to 20 min (SSWL) was determined as an estimate of the excess water in the skin caused by contact with the wet diaper material. For most of the babies a single WVFD measurement was taken 2 min after patch removal (when the rate of fall in the WVFD reading had abated somewhat). Analysis of data from the entire WVFD decay curves recorded for the minority of babies revealed that a spot reading at 2 min after diaper removal correlated quite well with the SSWL up to 20 min, and was much easier to obtain. Subsequent researchers have based their methods on those used by Zimmerer but there has been considerable variation in components of the method. In addition none of these studies appears to have conducted repeat experiments on the same subjects under the same conditions. Accordingly, the repeatability of the methodologies used is unknown. We discuss the main sources of variation below with a particular focus on the methods of water loading the skin and the type of WVFD outcome measure used when measuring the dynamic status of over-hydrated skin. Subjects, Sites and Methods of Hydrating the Skin (Table 1) Table 1 shows the characteristics of the subjects included in the studies, the various skin sites used and the different methods adopted to hydrate the skin. A variety of test fluids was used at different loadings in patches/products. In most studies, fluid loading was insufficient to achieve full saturation in patches/products and, except in the studies by Hatch et al. (12, 18), Markee et al. (19) and Cameron et al. (13) there was no attempt to distribute sub-saturation fluid loading uniformly throughout a test piece. Accordingly, the environment experienced by skin will have var- 3 knitted fabrics (1 cotton; 2 polyester) 8 diaper brands; 1 washable; 7 disposable Volar forearm Volar forearm Suprapubic area and buttock (thigh for baseline TEWL) Volar forearm 33 adults Unknown gender 5 male adults 1601 infants Unknown gender 5 male adults Hatch et al. (1992) and Markee et al. (1993) Berg et al. (1994) Hatch et al. (1997) 2 different fabrics Patches cut from 20 brands of incontinence pads; 3 washable; 17 disposable (10 with superabsorbent polymer, 7 without) Patches cut from 16 brands of diapers; 7 washable; 9 disposable (5 with superabsorbent polymer, 4 without) Dallas and Wilson (1992) Volar forearm 80 adults Unknown gender 4 disposable diapers (2 with superabsorbent polymer; 2 without) Patches cut from 1 disposable and 1 cloth diaper Whole disposable or cloth diapers (one variant of each) Diaper/patch material Wilson and Dallas (1990) Buttock Suprapubic area Volar forearm Skin site for measurement 150 infants Mixed gender 32 male babies Unknown N adults Unknown gender Subjects Davis et al. (1989) Expt #2 Zimmerer (1986) Expt #1 Authors (year) TABLE 1. Subjects, sites and methods of hydrating the skin Occlusive Hilltop chamber Not applicable Occlusive Hilltop chamber Knitted wrap retainer Elastic mesh retainer Not applicable Not applicable Elastic mesh bandage Patch held in place by Distilled water Subjects’ own urine Distilled water 1% saline with 0.025% Triton 1% saline with 0.025% Triton Subjects’ own urine Dyne solution Subjects’ own urine Fluid 2h 7 mL in 6.3 6.3 cm patch ( 5 ‘moderate loading’) 3 3 cm patches immersed in water, put through ringer with chromatography paper either side to give uniform distributions of 35 (PET fabric), 44 or 75 (cotton fabric) % saturation 30 or 60 min Variable 1, 2, 5, 10, 20, 30, 45 or 60 min 2h 7 mL in 6.3 6.3 cm patch ( 5 ‘moderate loading’) 38.6% saturated (just cotton); or fully saturated (all 3 fabrics). For partial saturation, 3 3 cm patches immersed in water, put through ringer with chromatography paper either side to give uniform distributions Whatever infant had voided Variable 1h 2h Diaper/patch wear time Whatever infant had voided (measured on diaper removal) 0, 50, 100 or 150 mL 1–6 dry patch weight Fluid load Review of methods using evaporimetry in over-hydrated skin 3 4 1h 1, 3 or 6 h Fluid delivered into in situ diaper to simulate micturition. Fluid loading level unclear. 3 mL in product centre Normal saline Physiological saline (except for dry pads worn for 3 h as controls) Physiological saline Whole menstrual pad with standard or vapourpermeable backing Elastic mesh bandage Methods and Conditions of Logging, Timing and Analysing WVFD Data (Table 2) Expt #2 TEWL, trans-epidermal water loss. Volar forearm 10 female adults Suprapubic area Expt #2 Shafer et al. (2002) Expt #1 Tape and nylon netting. Not applicable 3 disposable diapers (all with superabsorbent polymer; one with a microporous backing, two without) Volar forearm Unknown N female adults Unknown N infants Mixed gender Grove et al. (1998) and Akin et al. (1997) Expt #1 ied with position beneath a given patch, and from patch-to-patch in different experiments under nominally identical conditions. Likewise, diapers which were loaded naturally by their infant wearer may have varied greatly in the environment they provided for occluded skin, depending on how much urine the infant voided and when. Although such methods have often proved capable of detecting gross differences between products (e.g. diapers with and without superabsorbent polymers) a more reliable way of hydrating the skin is needed to examine the repeatability of WVFD measurements. 3h 40 min 2.5 2.5 cm patches immersed in water, put through ringer with chromatography paper either side to give uniform distribution Occlusive Hilltop chamber 16 different fabrics 35 female adults Cameron et al. (1997) Volar forearm Subjects Authors (year) TABLE 1. Continued Skin site for measurement Diaper/patch material Patch held in place by Distilled water Fluid Fluid load Diaper/patch wear time Fader et al. Perhaps most importantly, the procedure for logging WVFD data and processing it to obtain some measure of skin wetness has varied greatly between studies (Table 2). This is most easily reviewed by considering an example WVFD drying curve for very wet skin (Fig. 1). Following the initial delay in machine response, evaporation of water from the surface of the skin dominates, resulting in the high value, low gradient portion of the curve. If the skin is not very wet or surface water has been blotted away before data logging, this element of the curve may be much shorter or completely absent. Once surface water has evaporated, water loss from within the stratum corneum dominates and, as the stratum corneum dries out, the WVFD value falls – initially very rapidly – until the baseline TEWL level recorded for the skin before over-hydration is reattained. WVFD measurement in the reviewed studies varied from recording the maximum value 2 min after patch removal (minus the baseline TEWL) (12) to measuring WVFD repeatedly over time, constructing the desorption curve and measuring the SSWL (the area under the curve above the baseline measurement) (3). The approach of Zimmerer et al. (3) – who recorded the whole desorption curve and measured the area beneath it having subtracted baseline TEWL – would seem to be the most robust and defensible on theoretical grounds, although their decision to log WVFD for only 20 s per reading is likely to have introduced substantial errors. Other approaches were probably developed primarily to reduce the time and difficulty of capturing whole desorption Review of methods using evaporimetry in over-hydrated skin B 90 WVFD (gm–2h–1) A 60 C 30 Baseline TEWL 0 0 500 1000 Time (s) 1500 2000 Fig. 1. Example desorption curve for very wet skin. (A) Initial rapid increase in trace due to response time of machine. (B) Surface water evaporating. (C) WVFD value falls as the stratum corneum dries out. WVFD, water vapour flux density; TEWL, trans-epidermal water loss. curves – especially for measurements on infants. Taking measurements immediately after patch removal is particularly problematic as the desorption curve is changing very rapidly then (Fig. 1) and so readings will depend critically on the quantity of surface water on the skin (if any), the length of any delay before starting to log data, the time for which data are logged, and the way the data are processed; for example, the mean and maximum values over a period when WVFD is falling rapidly will differ greatly. Another important factor is that the Servo Med Evaporimeter probe is known to take of the order of 30–45 s to achieve a stable reading in measuring WVFD under equilibrium conditions on the volar forearm and palm (20, 21). It seems unlikely that it will deliver reliable readings in less than this time under the non-equilibrium conditions associated with skin drying curves. Accordingly, the 2 min logging period chosen for most wet skin studies is likely to have been too short. For some work the logging period was 30 s or less (3, 12), a practice likely to have yielded particularly inaccurate data. Notably, Cameron et al. (13) logged for 2 min but discarded data from the first 30 s of logging. Other Sources of Variation None of the studies appears to differentiate between surface water on the stratum corneum and water held within the stratum corneum: in general, Evaporimeter readings taken soon after patch/product removal are likely to have included some water coming from each of these two sources (Fig. 1). In another study of the impact of initially dry fabrics on skin worn under hot humid conditions, Hatch (1990) (22) addressed this issue by blotting sweat from the skin surface before logging WVFD. Subject, Environmental and Instrument Variables Tables 1 and 2 give the variables that are known to be sources of variation according to published guidelines for measuring baseline TEWL to characterise skin barrier function (rather than to quantify excess water in the skin) (7, 8). Variables have been usefully classified as (i) person-linked, (ii) environmental and (iii) instrumental (8). Some of the studies predated these guidelines and in others some variables were unreported, but in general, more recent studies have followed them more closely. The guidelines indicate that the anatomical site for TEWL measurement should be specified precisely as TEWL varies considerably over the surface of the body. In particular, there is some evidence that baseline TEWL may vary between dominant and non-dominant arms (23, 24) although some have found no difference (25, 26). Similarly, there is evidence for TEWL varying with position on the volar forearm (24, 27), although some have found little variation, pro- 5 Fader et al. TABLE 2. Methods and conditions of logging, timing and analysing evaporimetry data Authors (year) Temp (RH) Acclimatisation time Timing of evaporimeter measurement(s) Outcome variable(s) calculated Zimmerer (1986) Expt #1 Unknown Unknown ‘Precise intervals’ until baseline reached ( 20 min). Maximum reading over 20 s taken as WVFD value Area under curve above baseline Expt #2 Unknown Unknown First at 2 min after patch removal, then periodically until baseline reached ( 15 min). Maximum reading over 20 s taken as WVFD value Value at 2 min after patch removal (primarily) Davis et al. (1989) Unknown Unknown Data logged at 1 Hz for 2 min straight after diaper removal Area under drying curve over first 2 min (apparently without subtracting baseline TEWL) Wilson and Dallas (1990) 751F (241C) 40% Unknown First reading over 2 min straight after patch removal. Six further 2 min readings, each separated by 2 min rest. Means over each 2 min taken as WVFD value Difference between 1st and 6th Evaporimeter reading 5 ESW Dallas and Wilson (1992) 741F (231C) 42% Unknown Data logged for 2 min, starting 2 min after patch removal; second 2 min WVFD after 2 min rest. Baseline TEWL (on adjacent skin) taken between two other readings. Means over each 2 min taken as WVFD value Difference between 2nd ‘wet’ Evaporimeter reading and baseline 5 ESW Hatch et al. (1992) and Markee et al. (1993) 211C 65% Dry skin: 30 min; 80% hydrated skin: 1h Data logged for 30 s, starting 2 min after patch removal. Highest value during 30 s noted Difference between maximum from 30 s log after ‘treatment’ minus (mean) baseline value Berg et al. (1994) Unknown Unknown Immediately after diaper removal and at 60 and 120 s Hatch et al. (1997) 211C 65% 30 min Cameron et al. (1997) 201C 65% 10 min Data logged for 30 s, starting 2 min after patch removal. Maximum reading during 30 s taken as WVFD value 1 reading of 2 min taken immediate after patch removal, but discarded first 30 s of data. Mean taken as WVFD value Mean of data at all times and both locations (pubis and buttock) minus baseline 5 skin wetness Maximum value minus background (on adjacent skin) 5 Change in EWL 221C 40% Unknown 22C Unknown 40% 15 min Unknown 251C 50% 201C, 30% 251C, 50% 301C, 75% 30 min Grove et al. (1998) and Akin et al. (1997) Expt #1 Expt #2 Shafer et al. (2002) Expt #1 Expt #2 Notes Mean minus baseline (taken on nearby skin) 4 h minimum between test and retest Baseline: mean over last 15 s of 30 s logging period. After diaper removed: mean of 2 min logging period or ? repeats over various intervals over 5 min period ignoring first 10 s Mean minus baseline TEWL Probe holder used Plexiglas dome used for baseline infant measurements to reduce effects of air currents Immediately after patch removal, data logged for 45 s where centre of pad (with fluid loading) was Maximum value between 15 and 45 s. Baseline TEWL not subtracted ESW, excess skin wetness; EWL, excess water loss; WVFD, water vapour flux density; TEWL, trans-epidermal water loss. vided the skin near the wrist and elbow creases is avoided (25, 28, 29). TEWL also varies with skin temperature and so the ambient temperature should be noted and subjects should be acclima- 6 tised to ambient conditions for at least 15–30 min before measurements are made (8). Furthermore, when an ambient temperature probe is placed on the skin, the TEWL reading increases as the probe Review of methods using evaporimetry in over-hydrated skin warms to skin temperature ( 30 1C). For a Tewameters probe (Courage and Khazaka, Köln, Germany) this has been shown (25, 30) to take 1015 mins (which is similiar to that of the Servo Med device) and to be accompanied by a TEWL reading change of about 0.6 g/m2/h/ 1C (30). Mathias et al. (31) have provided a formula for normalising TEWL to a skin temperature of 30 1C, which some have adopted for studies of over-hydrated skin (12, 13). The temperature of the investigator’s hand can also affect readings from the hand-held probe and some have suggested that (s)he should wear an insulating glove (32) or that the probe should be held by a clamp instead (33). Physical, thermal and emotional sweating should also be controlled and so subjects should be calm and the ambient temperature such as to avoid both shivering and excessive sweating (34): 20–22 1C is recommended (7, 8). Ambient humidity also affects TEWL and 40% RH (7) and up to 50% RH (8) have been recommended. It is also known that TEWL is affected by draughts, which should be minimised and some have advocated the use of shields around the probe (7, 8, 14, 16, 35). It is recommended that the probe is held horizontal for measurements (7, 8). Care should also be taken with the pressure of the probe against the skin: Barel and Clarys (30) found that increasing the load on the Servo Med Evaporimeter probes from 100g to 300 g force increased TEWL readings by about 10%. Conclusion It is evident from this review that techniques and methods have varied widely in studies on overhydrated skin and that a robust methodology needs to be established for further work. Furthermore work to date has been confined to experiments on adult volar forearms or babies’ bottoms although an important target patient group for the development of better products to reduce skin damage from over hydration is older people and the target anatomical site is the skin within an incontinence pad (i.e. buttocks, hips and groins). Acknowledgements The authors would like to thank SCA Hygiene Products AB (Sweden), the Smith and Nephew Foundation (UK) and the Engineering and Phy- sical Science Research Council for supporting this work. References 1. Ward DB, Fleischer AB, Feldman SR, Krowchuk DP. Characterization of diaper dermatitis in the United States. 2000; 154: 943–946. 2. Gray M, Bliss DZ, Doughty DB, Ermer-Seltun J, Kennedy-Evans KL, Palmer MH. Incontinence-associated dermatitis: a consensus. J Wound Ostomy Continence Nurs 2007; 34: 45–54. 3. Zimmerer RE, Lawson KD, Calvert CJ. The effects of wearing diapers on skin. Pediatr Dermatol 1986; 3: 95– 101. 4. Berg RW. Etiology and pathophysiology of diaper dermatitis. Adv Dermatol 1988; 3: 75–98. 5. Spector WD, Fortinsky RH. Pressure ulcer prevalence in Ohio nursing homes: clinical and facility correlates. J Aging Health 1998; 10: 62–80. 6. Sivamani RK, Goodman J, Gitis NV, Maibach HI. Friction coefficient of skin in real-time. Skin Res Technol 2003; 9: 235–239. 7. Pinnagoda J, Tupker RA, Agner T, Serup J. Guidelines for transepidermal water loss (TEWL) measurement. A report from the Standardization Group of the European Society of Contact Dermatitis. Contact Dermatitis 1990; 22: 164–178. 8. Rogiers V. EEMCO guidance for the assessment of transepidermal water loss in cosmetic sciences. Skin Pharmacol Appl Skin Physiol 2001; 14: 117–128. 9. Davis JA, Leyden JJ, Grove GL, Raynor WJ. Comparison of disposable diapers with fluff absorbent and fluff plus absorbent polymers: effects on skin hydration, skin pH, and diaper dermatitis. Pediatr Dermatol 1989; 6: 102– 108. 10. Dallas M J, Wilson PA. Adult incontinence products: performance evaluation on healthy skin. INDA J Nonwovens Res 1992; 4: 26–32. 11. Wilson PA, Dallas MJ. Diaper performance: maintenance of healthy skin. Pediatr Dermatol 1990; 7: 179–184. 12. Hatch KL, Prato HH, Zeronian SH, Maibach HI. In vivo cutaneous and preceived comfort response to fabric Part VI: the effect of moist fabrics on stratum corneum hydration. Textile Res J 1997; 67: 926–931. 13. Cameron B A, Brown A M, Dallas M J, Brandt B. Effect of natural and synthetic fibers and film and moisture content on stratum corneum hydration in an occlusive system. Textile Res J 1997; 67: 585–592. 14. Grove GL, Lemmen JT, Garafalo M, Akin FJ. Assessment of skin hydration caused by diapers and incontinence articles. Curr Probl Dermatol 1998; 26: 183–195. 15. Berg RW, Milligan MC, Sarbaugh FC. Association of skin wetness and pH with diaper dermatitis. Pediatr Dermatol 1994; 11: 18–20. 16. Akin FJ, Lemmen JT, Bozarth DL, Garafalo MJ, Grove GL. A refined method to valuate diapers for effectiveness in reducing skin hydration using the adult forearm. Skin Res Technol 1997; 3: 173–176. 17. Schafer P, Bewick-Sonntag C, Capri MG, Berardesca E. Physiological changes in skin barrier function in relation to occlusion level, exposure time and climatic conditions. Skin Pharmacol Appl Skin Physiol 2002; 15: 7–19. 18. Hatch KL, Markee NL, Prato HH et al. In vivo cutaneous and perceived comfort response to fabric. Part V: effect of fiber type and fabric moisture content on stratum corneum hydration. Textile Res J 1992; 62: 638–647. 7 Fader et al. 19. Markee NL, Hatch KL, Prato HH, Zeronian SH, Maibach HI. Effect of fiber type and fabric moisture content on the hydration state of human stratum corneum. J Therm Biol 1993; 18: 421–427. 20. Blichmann CW, Serup J. Reproducibility and variability of transepidermal water loss measurement. Studies on the Servo Med evaporimeter. Acta Derm Venereol 1987; 67: 206–210. 21. Hatch KL, Wilson DR, Maibach HI. Fabric-caused changes in human skin: in vivo stratum corneum water content and water evaporation. Textile Res J 1987; 57: 583–591. 22. Hatch KL, Markee NL, Maibach HI, Barker RL, Woo SS, Radhakrishnaiah P. In vivo cutaneous and perceived comfort response to fabric. Part III: water content and blood flow in human skin under garments worn by exercising subjects in a hot, humid environment. Textile Res J 1990; 60: 510–519. 23. Treffel P, Panisset F, Faivre B, Agache P. Hydration, transepidermal water loss, pH and skin surface parameters: correlations and variations between dominant and non-dominant forearms. Br J Dermatol 1994; 130: 325–328. 24. Rodrigues LM, Pereira L. Basal transepidermal water loss: right/left forearm difference and motoric dominance. Skin Res Technol 1998; 4: 135–137. 25. Rogiers V. Transepidermal water loss measurements in patch test assessment: the need for standardisation. Curr Probl Dermatol 1995; 23: 152–158. 26. Oestmann E, Lavrijsen AP, Hermans J, Ponec M. Skin barrier function in healthy volunteers as assessed by transepidermal water loss and vascular response to hexyl nicotinate: intra- and inter-individual variability. Br J Dermatol 1993; 128: 130–136. 27. Panisset F, Treffel P, Faivre B, Lecomte PB, Agache P. Transepidermal water loss related to volar forearm sites in humans. Acta Derm Venereol 1992; 72: 4–5. 28. Pinnagoda J, Tupker RA, Smit JA, Coenraads PJ, Nater JP. The intra-individual and inter-individual variability and reliability of trans-epidermal water-loss measurements. Contact Dermatitis 1989; 21: 255–259. 8 29. Pinnagoda J, Tupker RA, Coenraads PJ, Nater JP. Comparability and reproducibility of the results of water-loss measurements – a study of 4 evaporimeters. Contact Dermatitis 1989; 20: 241–246. 30. Barel AO, Clarys P. Study of the stratum corneum barrier function by transepidermal water loss measurements: comparison between two commercial instruments: Evaporimeter and Tewameter. Skin Pharmacol 1995; 8: 186–195. 31. Mathias CG, Wilson DM, Maibach HI. Transepidermal water loss as a function of skin surface temperature. J Invest Dermatol 1981; 77: 219–220. 32. Agner T, Serup J. Time course of occlusive effects on skin evaluated by measurement of transepidermal water loss (TEWL). Including patch tests with sodium lauryl sulphate and water. Contact Dermatitis 1993; 28: 6–9. 33. Pinnagoda J, Tupker RA, Coenraads PJ, Nater JP. Comparability and reproducibility of the results of water-loss measurements – a study of 4 evaporimeters. Contact Dermatitis 1989; 20: 241–246. 34. Pinnagoda J, Tupker RA, Coenraads PJ, Nater JP. Comparability and reproducibility of the results of water-loss measurements - a study of 4 evaporimeters. Contact Dermatitis 1989; 20: 241–246. 35. Pinnagoda J, Tupker RA. Measurement of the transepidermal water loss. In: Serup J, Jemec GBE, eds. Handbook of non-invasive methods and the skin. Florida: CRC Press, 1995: 173–178. Address: Mandy Fader RN, PhD Continence Technology and Skin Health Group School of Health Sciences University of Southampton Highfield, SO17 1BJ UK Tel: 144 23 8059 7979 Fax: 144 23 8059 8909 e-mail: mf@soton.ac.uk