UCL Eastman Biobank Management Protocol Version Number: 05
advertisement

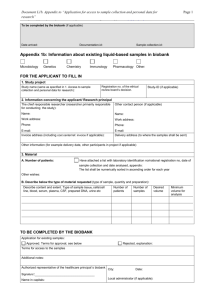
UCL Eastman Biobank Management Protocol Version Number: 05 Superseded Version Number & Date: 04 30/5/12 Prepared by: Dr Paul Ashley Authorised by: NRES Committee Yorkshire and the Humber – Leeds East 12/YH/0111 3/4/12 Date for Renewal 3/4/17 HTA Licence Number: 12277 Designated Individual, UCL Eastman Biobank Vehid Salih Signature: Date: UCL Eastman Dental Institute 256 Grays Inn Rd London WC1X 8LD Telephone: +44 (0) 20 3456 **** Fax: +44 (0) 20 3456 **** Email: Management Protocol (Version 5, 30/5/12) 1of17 Contents 1. INTRODUCTION ....................................................................................................... 3 2. PROTOCOL SCOPE................................................................................................. 3 3. ROLE AND GOVERNANCE OF THE BIOBANK ...................................................... 3 3.1 Biobank Ethical Review Committee Purpose ..................................................... 4 3.2 Membership of the Ethical Review Committee: ................................................. 4 3.3 Responsibilities of the Ethical Review Committee/its members ........................ 4 3.4 Reporting Structure of Ethical Review Committee ............................................. 6 3.5. Ethical Review Committee Modus Operandi ..................................................... 6 4. BIOBANK RESEARCH PROGRAMME .................................................................... 6 4.1 Principle Research Interests............................................................................... 6 5. TESTS OF POTENTIAL ETHICAL OR CLINICAL SENSITIVITY: APPROVED AND EXCLUDED USE .................................................................................................. 7 5.1 Potential Clinical Significance to Donors ............................................................ 7 5.2 Analysis and Use of Genetic Material ................................................................ 8 5.3 Cellular Cloning .................................................................................................. 8 5.4 Therapeutic cloning and derivation of stem cells for use in treatment ............... 8 5.5 Reproductive research including reproductive cloning ...................................... 8 6. INCLUSION AND EXCLUSION CRITERIA .............................................................. 8 6.1 Inclusion Criteria ................................................................................................. 8 6.2 Exclusion Criteria ................................................................................................ 8 7. CONTENT OF THE BIOBANK.................................................................................. 8 7.1 Transfer of samples and data from Tissue Collection Centre to the Biobank.... 9 8. CONSENT AND RECRUITMENT OF PARTICIPANTS ........................................... 9 8.1 Existing Biobank holdings.............................................................................. 10 8.2 Acceptance of samples from other sources ..................................................... 11 8.3 Withdrawal of consent ...................................................................................... 11 8.4 Ownership of samples ...................................................................................... 11 9. COLLECTION OF RESEARCH SAMPLES ............................................................ 12 10. BIOBANK STAFF: REQUIRED TRAINING AND EXPERIENCE ......................... 12 10.1 Obtaining consent ........................................................................................... 12 10.2 Tissue collection and administration .............................................................. 12 10.3 Safe Handling of Human Biological samples ................................................. 12 11. SECURITY AND CONFIDENTIALITY .................................................................. 13 11.1 Linked-anonymised/pseudoanonymised samples ......................................... 13 11.2 Physical security of samples and data ........................................................... 13 12. ACCESS POLICY AND NEW COLLECTIONS .................................................... 13 12.1 Process for requesting samples and new collections .................................... 13 12.2 Conditions for sample and data release to researchers ................................ 14 13. BIOBANK ADMINISTRATION .............................................................................. 14 13.1 Protocol amendments..................................................................................... 15 13.2 Governance policy, operating procedures and quality systems..................... 15 13.3 Reporting serious protocol non-compliance or breach of policy .................... 16 13.4 Clinical adverse event reporting ..................................................................... 16 13.5 Record retention ............................................................................................. 16 13.6 Funding ........................................................................................................... 16 13.7 Financial implications for donors .................................................................... 16 13.8 Communication and publication policy ........................................................... 16 13.9 Progress reports and accountability ............................................................... 16 Management Protocol (Version 5, 30/5/12) 2of17 1. INTRODUCTION The UCL Eastman Biobank will act as a physical repository for collections of biological samples and data for research purposes from consented patients at the Eastman Dental Institute and Hospital, University College London and University College London Hospitals Foundation Trust (Eastman). This will incorporate prospective collections of stored samples and new collections. It provides a unique opportunity to advance dental and medical research by making access to tissue surplus to requirements easier, and more efficiently, and with a high level of governance compliant with HTA standards. The Biobank will support projects principally involved in the study of human disease and the normal functioning of the human body. The Biobank will store normal and pathological specimens from relevant tissues and bodily fluids. Tissue will be stored in a variety of formats. The establishment of a core programme will enable a centralised approach to the management and integration of all research groups working within these institutions, providing appropriate structure and support. The Biobank aims include: 1. Facilitate research 2. Enhance availability of UCL holdings to researchers. The aim is to support primarily research in the Eastman but it will also support UCLH partners, as well as researchers nationally and internationally 3. Assistance with regulatory compliance (principally the HTA) 4. Improve research governance 2. PROTOCOL SCOPE This protocol defines: A management, operational, and ethical framework for the UCL Eastman Biobank The scope and content of potential future research using the Biobank 3. ROLE AND GOVERNANCE OF THE BIOBANK The Biobank has policies and guidelines to guarantee compliance with HTA legislation and to ensure quality standards will be maintained (http://www.ucl.ac.uk/Biobank). The Biobank will be governed by the Ethical Review Committee which will represent a range of stakeholders who will work together to maximise the potential of the samples stored or registered with the Biobank. The Committee will ensure that there is good governance, appropriate links to the relevant communities, and that progress, output and the development of the Biobank is regularly monitored. It will consider the concerns of sample donors and the tissue depositors and make recommendations to ensure direct benefit of the Biobank to ongoing medical and dental research. The Committee will also review requests for new sample collections and applications for use of samples/data for research, including those which do not have ethical approval and ensure they satisfy conditions laid down by IRAS before giving approval for the release and use of tissue. Management Protocol (Version 5, 30/5/12) 3of17 3.1 Biobank Ethical Review Committee Purpose The following terms of reference have been produced for the Ethics Review Committee to ensure the Committee fulfils its role. 3.1.1 The Committee represents a range of stakeholders who will work together to maximise the potential of the samples stored or registered with the Biobank. 3.1.2 The Committee should ensure that there is good governance, appropriate links to the relevant communities, and that progress, output and the development of the Biobank is regularly monitored. 3.1.3 The Committee will consider the concerns of sample donors and the tissue depositors and make recommendations to ensure direct benefit of the Biobank to ongoing medical and dental research. 3.1.4 The Committee will review requests for new sample collections and also requests for use of samples/data for research, including those which do not already have ethical approval and ensure they satisfy conditions laid down by NRES for the release of tissues by the Research Tissue Bank. 3.2 Membership of the Ethical Review Committee: 3.2.1 The Biobank Ethical Review Committee will be chaired by an elected member of the Review Committee 3.2.2 Members Designated Individual for HTA/Biobank licence for the Eastman UCL Biobank Facilitator Representative from UCL EDI Director of Research Representative from Eastman Dental Hospital (UCLH) Representative from sample users Lay member External member (eg charity or other Biobank) 3.2.3 Individuals will be invited to be members of the Ethical Review Committee for a term of 3 years from the date of acceptance of the invitation. This can be extended for a further three years as required by agreement of the Management Committee. The Chair of the board will be reviewed every 2 years. 3.3 Responsibilities of the Ethical Review Committee/its members 3.3.1 To attend Ethical Review Committee meetings. 3.3.2 To ensure that at all times the Biobank follows regulatory (Human Tissue Act 2004) and ethical guidelines and fulfils the standards of best practice. Including: Maintenance of the Appropriate Human Tissue Authority Licences Controlled and monitored storage of all samples within the Biobank at the appropriate temperature Quality and safety of all technical and administrative procedures Policies on data protection Policies for withdrawal of tissue Policies for disposal of tissue Policies for transfer of tissue 3.3.3 Approving and ensuring that the Biobank has appropriate agreements in place with those depositing collections and requesting samples to guarantee that: Appropriate consent is documented for the banking of all samples/data along with written protocols to support the same Samples being transferred to the Biobank follow regulations governing the transport of biological samples Samples and data being transferred to the Biobank follow agreed protocols Receipt of samples is confirmed by Biobank Management Protocol (Version 5, 30/5/12) 4of17 Payment for services (where appropriate) is provided by Biobank Appropriate disposal of any samples released to users by the Biobank. This includes any material passed on to a third party for ethically approved research studies, which should be covered via a Material Transfer Agreement with the third party stating disposal or return options. Intellectual property and commercial rights are appropriately addressed in contracts, particularly in relation to tissue requests from commercial companies. Compliance with the Biobank's policies on storage, health & safety, security, quality management, data protection, access, training, consent and audit of compliance. These policies have been put in place to ensure HTA compliance. 3.3.4 To provide independent review and advice To review the services provided by the Biobank to ensure specified targets, agreed with the depositor for receipt, processing and dispatch of samples are maintained Ensuring systems and resources are such to enable widespread use by the relevant scientific community Ensuring respect of the dignity and rights of donors 3.3.5 The status of the Biobank as a Research Tissue Bank requires that the Ethical Review Committee reviews and approves requests from researchers for use of samples and data in research, for which they do not have project-specific ethical approval. This will be carried out under conditions laid down by IRAS in its ethical review of the Research Tissue Bank. Projects will only be reviewed if the sample/data collector agrees in principle to supply the relevant samples and data. 3.3.5.1 Researchers will make a formal application to the Biobank Ethical Review Committee via the Biobank administrator using the application form (See Request form for samples/data). The form will require the following information The Principal Investigator’s contact details The type and amount of material required The data required to accompany the material The title of the project A short summary of the proposed research The justification that the research presents no material ethical issues 3.3.5.2 The application will be considered by the Biobank Ethical Review Committee, to determine whether it is ethically valid. The process for reviewing applications for ethical approval by the Committee will be as follows: All Committee members will be sent an electronic copy of the application requesting samples or data from the Biobank Committee members will be asked to return their views in writing within a specified 2 week timeframe The views of individual members will be circulated to the entire Committee with the aim of reaching a consensus decision. Where appropriate, applications will be discussed at a scheduled Committee meetings Response and agreement of all members of the Committee will be required to reach an approved decision. Committee members who have not responded within the designated time will be given an additional 3 days to comment on the decision before it is ratified If there is disagreement a telephone, electronic conference or a meeting will be held and a note taken of the decision. Alternatively, if a Committee meeting is scheduled proposed applications will be discussed at the next appropriate meeting. Where ethical considerations are not straightforward, the Committee may require that the person to come to a meeting to explain the project. If a decision still cannot be made, the applicant will be required to seek full project-specific REC approval Management Protocol (Version 5, 30/5/12) 5of17 Where the Committee believe an application is of a particularly specialised nature, beyond the scope of the Committee, they may seek an expert opinion on the research and may require additional information to be submitted Once the request has been approved, if appropriate the applicant will be required to sign a material transfer agreement for receipt of the samples Sample recipients will be required to send reports and copies of publications to the collector of the samples, as agreed in the material transfer agreement 3.3.6 To provide assistance in any enquiry, audit or investigation related to the Biobank. 3.4 Reporting Structure of Ethical Review Committee 3.4.1 The Ethical Review Committee will report to the Research Governance Committee (UCL and UCLH) and to the UCL HTA Compliance Committee. In addition an annual report will be sent to the NRES Committee that approved this Biobank. 3.4.2 Reporting to these committees will ensure dissemination of information about the Biobank to the wider community and allow comment on operational aspects of the Biobank. 3.5. Ethical Review Committee Modus Operandi 3.5.1 If the Chair is not present, the Vice-Chair will preside 3.5.2 The Chair may invite an individual(s) to attend a specific meeting or meetings to provide specialist advice to the Committee. 3.5.3 Meet three times a year. 3.5.4 For each meeting a quorum of 4/5th of the committee membership must be present. 4. BIOBANK RESEARCH PROGRAMME The Biobank will support the Research Programme and scientific needs of UCL research groups, primarily in the UCL Eastman Dental Institute. Many of the tissue samples collected will be for specific projects, however the consent proposed will permit long term storage of samples to be used for future projects. The Research Programme will include: 4.1 Principle Research Interests Although we are not intending to have an exhaustive list of research interests, they all should contribute to advancements in the understanding and treatment of oral and general disease They will include the following: 1. Search for biomarkers, molecular targets and profiles related to prognostic and predictive markers of disease but also disease progression and disease outcome. 2. Investigating the causes of disease, damage and degeneration in hard and soft tissues. 3. Establishing novel culture methodologies for generating distinct cell types from sources including dental pulp, periodontal ligament and alveolar bone. Cells obtained from these sources may have stem cell properties and therefore can be manipulated to produce a variety of tissues (e.g. bone, cartilage, tendon, muscle, brain cells) 4. Establishing methods to discriminate structure/function relationships based on mechanical testing and biochemical composition of tissues 5. Understanding disease related biology and testing drug response prior to clinical trials. 6. Developing and validating 3-dimensional models of tissue explanted intact or reconstructed on grafts and implants for studying novel therapies prior to clinical trials. Management Protocol (Version 5, 30/5/12) 6of17 7. Developing and validating models to predict responses to novel adjuvant treatments and agents. 8. Searching for evidence of age and disease relevant epigenetic modifications in tissue and investigating the mechanisms. 9. Developing non-invasive measuring tools to assess mechanical properties and early damage or repair markers to target more appropriately preventative strategies for rapid assessment of response to novel treatments and side effects on tissues. 10. Pharmacodynamic and pharmacokinetic evaluation and monitoring of drugs or therapeutic agents in target or surrogate tissue in early phase clinical trials. 11. Evaluate the association between molecular characteristics and profiles of tissue with therapeutic modulation. 12. Examine the influence of genetic variation on disease progression and response to therapeutic interventions to develop rational means to optimise diagnosis and treatment. 13. Develop and validate new materials for the repair of hard and soft tissues 5. TESTS OF POTENTIAL ETHICAL OR CLINICAL SENSITIVITY: APPROVED AND EXCLUDED USE In order to deliver the programme, many available tests/assays may be performed. At present these include, but are not limited to, the following: Immunohistochemical, molecular biology and biochemical studies Immunoassays and flow cytometry Genetic analysis including whole human deep genomic sequencing Genotyping and epigenetic typing, including genome wide searches Gene expression profiling Proteomics Metabonomics Imaging Quantification of RNA and other cellular molecules Genetic Modification: not reproductive cloning Cell/explant culture and biochemistry (including stem cells) Mechanical testing of specimens and of explants / scaffolds Microbiological assay Research samples will not be collected from donors who wish to impose conditions of use on their samples. Samples will only be released in a pseudoanonymised format for approved research projects. Material will not be used from fetuses and embryos Material will not be collected from the deceased Material will not be used for the purpose of cloning individuals 5.1 Potential Clinical Significance to Donors Patients will be informed that their samples will be used in research intended to develop advances in disease management in the future. During the consent process, it will be brought to the attention of the patient that their samples may be stored for many years and used in future research that may not be predicted at this time. There would be no feedback of results to the donor, their families or their health care providers, as much of the research will be performed in laboratories that are not accredited for diagnostic work. Management Protocol (Version 5, 30/5/12) 7of17 5.2 Analysis and Use of Genetic Material The research programme will examine genetic factors in order to develop improved tools for establishing prognostic and predictive factors for disease, including factors influencing response to treatment. Specific analyses may produce information that includes genetic sequence data, single nucleotide polymorphism data, genetic "fingerprint" data, ploidy data or cytogenetic data including the detection of mutations or genetic variants. Research may generate information on genetically transmissible disease (e.g. identifying genes that may be passed on within families). The research does not qualify as genetic testing as defined by insurance companies. The Biobank will not feedback results to the donor, their families or their doctor. Information generated from the research will be published in peer-reviewed journals, and presented at national and international scientific meetings. 5.3 Cellular Cloning The Biobank will support the collection of surplus fresh tissue taken during routine medical (therapeutic/diagnostic) procedures, which ensures prompt delivery to researchers who wish to grow cell lines. 5.4 Therapeutic cloning and derivation of stem cells for use in treatment These activities are excluded from the Research Programme portfolio and the Biobank will not supply material for this purpose. 5.5 Reproductive research including reproductive cloning These activities are excluded from the Research Programme portfolio and the Biobank will not supply material for this purpose. 6. INCLUSION AND EXCLUSION CRITERIA 6.1 Inclusion Criteria Potentially all patients referred to the Tissue Collection Centres (initially the Eastman) for diagnosis and/or treatment. Children under the age of 16 years will be included. In some instances the Biobank may seek patients’ permission to contact their family members in order to arrange for samples to be used for research. This contact will be via the family member, members of UCL staff must NOT contact family members independently. This will allow investigation of the effect that environmental and genetic factors may have on the development of a disease. Furthermore, healthy volunteers may be recruited from within the hospital to donate samples for research purposes. This will be done in line with relevant UCLH procedures and protocols. 6.2 Exclusion Criteria Approached donor (or qualified representative where necessary) is unwilling or incapable of giving informed consent to all the research conditions Patients known to be HIV, Hepatitis B or C positive. No formal testing will be undertaken by the bank Specimen samples damaged intra-operatively or specimen size is inadequate Other factors that in the opinion of the responsible clinician might jeopardise the safe and ethical conduct of patient care, Research Programme operations or dependent research projects Patients who wish to stipulate specific restrictions for use of their tissue for research 7. CONTENT OF THE BIOBANK Management Protocol (Version 5, 30/5/12) 8of17 The Biobank will act as a physical repository for biological samples and data collected from patients attending the Eastman and possibly other Tissue Collection Centres including UCLH. This will incorporate existing collections and new material collected prospectively. The Biobank will support projects principally involved in the study of human disease and functioning of the human body, in particular the research programmes of the UCL Eastman Dental Institute. To meet this need the Biobank will store normal and pathological specimens, surplus to diagnostic requirements, from relevant tissues and bodily fluids. Stored tissues will include; snap-frozen or cryopreserved tissue, formalin-fixed tissue, paraffin-embedded tissues, and slides prepared for histological examination. Tissues will include teeth or resection specimens obtained surgically or by needle core biopsy. Bodily fluids will include; whole blood and blood products, serum, plasma, urine, saliva and buccal smears and cytological specimens such as sputum. Where appropriate the Biobank will also store separated cells, protein, DNA and RNA isolated from collected tissues and bodily fluids described above. Some of the tissue and aspirated samples will be stored in the diagnostic archive. Snap frozen tissue will be stored in -80 degree C freezers or liquid nitrogen dewars, fixed tissue will be fixed in 10% formalin and processed and embedded in paraffin-wax where appropriate. Blood will be stored in -80 or -20 degree C freezers. All these samples can potentially be kept indefinitely if storage protocols are adhered to and optimal storage conditions maintained. 7.1 Transfer of samples and data from Tissue Collection Centre to the Biobank The samples and data collected for the Biobank will be from participants visiting the Tissue Collection Centres – initially the Eastman or UCLH. This data and samples will be transferred between the Tissue Collection Centre and the institution responsible for the Biobank (UCL) under a material transfer agreement between the Hospital Trust and the University. 8. CONSENT AND RECRUITMENT OF PARTICIPANTS The Biobank will operate under the guidance of the Biobank Research Ethics Committee to assure compliance with current best ethical practice. The underlying principle is that participants should give consent for access to their case notes, imaging, and to the use of their tissue surplus to diagnostic requirements for medical research to be used in any ethically approved research. The Biobank will not accept individuals’ participation in studies subject to conditions that exclude use in specific areas of research such as genetic testing, or add stipulations to the use of their tissue. The participant will retain no rights to the samples after acquisition other than the ability to withdraw consent for further storage and use. Patients may also withdraw to consent to giving access to their case notes and imaging for research purposes. Consent to use human tissue in research will be obtained via the generic Biobank consent forms and Patient Information Sheet. The consent form is separate to the NHS Trust "Consent to Investigation or Medical Procedure Form". Consent forms have been developed in line with National and Local guidelines on best practise. Targeted patient groups referred to the Eastman for a diagnostic/therapeutic procedure will be invited to consent to give access to their notes and imaging for research and to donate tissue for the Biobank. The majority of patients attending for treatment at the Eastman will have several appointments before the clinical diagnostic procedure. The relevant patient Management Protocol (Version 5, 30/5/12) 9of17 information sheets will be given to the patient at their initial appointment, so that patients will have at least 24 hours to consider the information given to them. At subsequent appointments they will meet an individual who has knowledge of the Biobank and related research programmes who will be able to answer any questions that the patient may have. This trained staff member will assess the patient's ability to understand and retain the information provided in the Patient Information Sheet and if they believe the patient is appropriately informed they will ask the patient to sign the consent form. If patients are unlikely to have several appointments before treatment, the patient information sheets will be sent out with the new patient appointments. The consent form is specific to the Biobank but is broad in scope and enduring. The patient is asked to consent to their clinical notes and imaging being accessible for approved research projects, and for tissue samples and data to be stored indefinitely and used in future projects that have not yet been planned. If the patient asks for any conditions to be placed on the use of their tissue, e.g. not to be used for genetic analysis, the patient will not be asked to sign the consent form. The consent form is signed and dated by both the patient and an individual who is appropriately trained in taking consent. A copy of the consent form is given to the patient, a copy is retained in the patient's medical notes and a third copy accompanies the sample to the Biobank. The patient will also be asked to consent specifically to allow access to his/hers clinical notes and imaging investigations, so that information can be linked to the tissue for future or current ethically approved research projects. Strict confidentiality will be observed in such studies. If information about a patient is documented, the patient’s identity will be coded and linked to the clinical information so that the researchers will then not have direct access to the patient’s identity but additional information can be later accrued from patients’ notes by a member of staff who has access and permission to unlocking and relocking the code. This will prevent patient data falling into the wrong hands, and will prevent patients being recognized when results are published. If a blood sample is required for research purposes, if at all possible, the sample will be taken at the same time as a blood sample is being collected as part of the patient’s management. However, if neither of the above is possible, an appropriately trained person will approach the patient and ask them if they are willing to have a blood sample taken. This will be done at the discretion of the trained individual; if for instance, a patient is very nervous, a decision may be made not to approach the individual. In the case of children, specific permission would be required for a particular project to take blood at a time when a sample was not being taken for treatment / diagnostic purposes. The consent procedure will take place in the normal course of healthcare provision and no extra appointments will be required. Blood samples from family members and other volunteers will be obtained by appointment at a time that is convenient to the participant. Participants under 11 who assent will be asked to re-consent once they reach the age of 16. If participants cannot be contacted samples will remain in the Biobank. 8.1 Existing Biobank holdings The existing research collections of tissue stored at the Eastman have informed consent for their use in research, or were collected prior to enforcement of the HTA in 2006. Management Protocol (Version 5, 30/5/12) 10of17 Tissue stored in the diagnostic archive will also be available for research provided that surplus material is available. In some cases, consent for use of this material for research will not have been requested, as the samples have been stored primarily for diagnostic purposes. However, as they represent a large valuable resource for research which is often unforeseen, access to these samples, where a surplus exists, is desirable. Obtaining retrospective consent in these circumstances is not feasible. In these circumstances such tissue would be available to researchers as long as they meet the following HTA-approved criteria; The tissue was collected from the living and is surplus to diagnostic requirements. The researchers obtain ethical approval (in this case from the Biobank Ethics Committee). Tissue and patient data will be released in a linked-anonymised form. It is not proposed to seek consent for material stored in the diagnostic archive if the patient has not been consented. 8.2 Acceptance of samples from other sources The consent forms that are being submitted with this application request patients to consent to giving access to tissue that is surplus to diagnostic requirements, case notes and imaging. Acceptance of such samples will be carefully considered in order to ensure that storage and use is covered by the terms of the original consent. 8.3 Withdrawal of consent A permanent link between the sample and the donor will always be maintained via the Biobank. The patient/participant information sheet provides information on what to do if the donor decides they no longer wish to participate in the Biobank Research Programme. The donor can either contact the clinician in charge of their care or they can contact the individual listed on the patient information sheet. The participant will be sent a "Withdrawal of Consent" form to sign. This step is in place to ensure the person withdrawing consent is the same as the person who originally gave consent, however it is not essential and if someone wishing to withdraw consent refuses to complete the form then they will still have their samples withdrawn from the study. The database manager, who is authorised to view the linked data of all samples held in the Biobank and can therefore establish where the donor’s samples are being held and/or by whom they are being used, then has 5 working days to contact researchers involved and request that the samples are removed from the Biobank and disposed of as per local regulations on tissue disposal. A confirmation of this action is signed by database manager and sent to the participant. A copy of the confirmation is retained in the participant's medical notes. The participant's research record is amended accordingly and although their data can no longer be seen by researchers, it is not entirely deleted as an audit trail must be maintained. This is fully explained to the donor. It will also explained to the donor that most data obtained from his/her samples may be used although if requested genetic data from closed access databases will be removed and destroyed. It will not be possible to remove the data from open access databases. 8.4 Ownership of samples Those samples collected from UCLH patients and stored as surplus diagnostic material would be expected to be 'owned' by the Biobank and to remain as part of the Biobank if the person responsible for a particular sample collection moved to another Institution or leave the employ of UCL/UCLH. For material that has been transferred in to the Biobank from other Institutions, ownership of the samples would be agreed with the collector of the samples before they were accepted by the Biobank. Management Protocol (Version 5, 30/5/12) 11of17 Where funding bodies support the collection of material to be banked, the collector of the samples would be expected to have agreed the conditions of ownership of the samples with the funding body and Institution, before the samples are accepted by the Biobank. In each case samples would only be released from the Biobank following the directions issued by the HTA for compliance with the HTAct 2004, i.e. to another HTA licensed premise or for ethically approved research. 9. COLLECTION OF RESEARCH SAMPLES Collection of samples for research is organized through collaboration and communication between research staff and clinical staff. Samples that are removed during surgical procedures for the purpose of diagnosis in the majority of cases will be first be assessed by a Consultant Histopathologist, although a case can be made if it is deemed that this is not a requirement. Researchers collecting research samples from the Biobank must register themselves prior to collecting their first sample. Registration involves providing evidence of REC approval. Only tissue that is surplus to diagnostic requirements will be released for research and patient diagnosis should never be compromised. The sample will be logged onto the research inventory system prior to release and all personal identifiers will be removed. The sample will be given a unique research code that will enable tracking and audit. Samples for research that do not require histological assessment and tissue to be discarded without pathology analysis (e.g. teeth, cartilage, bone) can be acquired directly from operating theatres. If this happens it is the responsibility of the clinician collaborating in the research project to ensure that the sample is logged on to the inventory database and that personal identifiers are removed. Consent forms must be delivered to the Biobank where they are stored centrally on a scanned electronic form, accessible to authorized staff. Some projects may require extra samples such as blood, and saliva to be collected from patients with certain conditions or healthy donors. Collection of blood, and saliva will normally take place in the pre-assessment clinic, in the outpatient department or in the wards for inpatients and only after appropriate consent has been obtained. Every effort will be made for blood samples to be taken from patients when a blood sample is being taken for diagnostic purpose or when a patient in under anaesthetic. However, exceptions to this can be made on a study by study basis. 10. BIOBANK STAFF: REQUIRED TRAINING AND EXPERIENCE 10.1 Obtaining consent All members of staff involved in the consent process will be trained appropriately. Specific training will be given on maintaining, and avoiding breaches of, patient confidentiality. Annual review of training status will be performed by the Designated Individual. Staff training records are maintained and regularly updated. 10.2 Tissue collection and administration All members of staff involved in the operation and running of the Biobank are appropriately trained. Areas of training include sample tracking, laboratory health and safety and risk management. 10.3 Safe Handling of Human Biological samples As part of their induction when they join the UCL, all clinical and research staff are made aware of the health and safety policies of UCL. All guidance that issued by the Biobank will be done so in accordance with these key documents. Risk assessments are conducted for Management Protocol (Version 5, 30/5/12) 12of17 all activities involving human tissue samples. Standard Operating Procedures (SOP) exist for all tasks involving human tissue samples. All sample handling, processing, transfer and disposal will be logged on the inventory database. 11. SECURITY AND CONFIDENTIALITY 11.1 Linked-anonymised/pseudoanonymised samples Data collected and stored for linkage with samples will include patient diagnosis, relevant clinical information including imaging, demographics and clinical outcome. Data will be derived from health records. All personal identifiers will be held securely within the facility. This information will be linkedanonymised, by numerical code to the sample, which will not include personal identifiers. The database holding information about the samples will be hosted on a secure UCL server, which will be regularly backed up. Only authorised personnel who have registered for access will be granted access to the database and ‘end use researchers’ will only receive coded samples and data. Authorised personnel will consist of Biobank staff and Research and Development staff members. The link to patients’ identifiable data is maintained in order to remove and dispose of the patients’ samples/data if they ever choose to withdraw their consent and to allow addition of outcome measures. In addition, if a researcher requires further clinical data (including imaging studies) they can apply to the Biobank for this data. The Biobank can disclose this information without disclosing any personal identifiers. 11.2 Physical security of samples and data The ‘banked’ tissue will be held in a secure, HTA-licensed research facility at the UCL Eastman. All electronic data are stored on computers that are housed in lockable rooms. All computers are password protected. Storage facilities are protected by lock, keypad and entry phone 12. ACCESS POLICY AND NEW COLLECTIONS The Biobank will support projects principally involved in study of human diseases and the normal functioning of the human body. The Biobank will be open to requests for samples/data from any research team investigating either within UCL, and UCLH, as well as from other researchers in the UK and abroad. The research projects must comply with the areas of research set out by the Biobank in this application. The open access policy will apply to academic, private or public sector researchers, whether they are, or work with not for profit or for profit organisations. 12.1 Process for requesting samples and new collections All researchers that wish to use the Biobank must apply via the Biobank administrator. Only projects that are covered by the scope of the Research Tissue Bank ethics application will be authorised. In addition to obtaining appropriate approval, if a researcher wishes to start their own sub collection or enter an existing collection under the cover of the Biobank, the researcher must provide evidence that they comply with the Biobank's policies on storage, health & safety, disposal, security, quality management, data protection, access, training and consent and audit of compliance. These policies have been put in place to ensure HTA compliance. Access to human biomaterials stored in the Biobank in the first instance will be, either via contact with the Biobank administrator who can direct enquiries to the collector of the samples, or directly to person who has collected the materials. The purpose of this is to ensure that appropriate samples are available for the proposed project. If a researcher Management Protocol (Version 5, 30/5/12) 13of17 wishes to gain access to the histopathological material held in the diagnostic archive, the researcher will be directed to the pathologist who has a specialist interest in the disease / tissue of interest. A list of pathologists with specialist interests will be held by the Biobank administrator. In the first instance the interested researcher obtains agreement of the collector or by an interested party, for instance, the histopathologist or clinician involved in the collection or diagnosis of that tissue. 1) If the person requesting access to the Biobanked samples already has a project –specific ethical approval for the proposed research project via NRES/IRAS, the samples will be released from the Biobank under the conditions stated below. 2) In the case where the person requesting the samples does not have ethical approval or local peer review for the project for which they are requesting samples, applications will be made using the Request Form to the Biobank Ethical Review Committee. The request form for use of samples (see attached information) requests information on the nature of the research project. The Biobank Ethical Review Committee, will where appropriate, seek additional expert guidance regarding a request. If the Biobank Ethical Review Committee do not feel they can review an application, the applicant will be advised to apply for ethical approval via NRES/IRAS. On receipt of requests for new collections or use of samples by the Biobank Administrator, the application will be assigned a reference number that will serve to identify all documentation which will also serve to track dissemination of material. The Biobank administrator will submit the application to the Ethical Review Committee for approval, where appropriate and will convey the decission of the Committee to the applicant. 12.2 Conditions for sample and data release to researchers The terms of reference for the Biobank Ethical Review Committee require electronic submission of requests so that the Board can review the applications within a 2-3 week time period. The Biobank committee will consider applications from all scientists wishing to perform research using the Biobank samples and information related to them. Researchers may include those in the UK and abroad, in the NHS and in commercial companies. Simple provision of tissues cannot constitute an intellectual event, as IP, by its very definition, requires intellectual input into an invention. Where tissues are provided as part of a wider research collaboration the provider may make an intellectual contribution to the discovery and would thus be a co-inventor under normal law, in this case UCL will enter into negotiations over IP and a suitable contract before tissue will be released. The researcher must satisfy the Committee that their research falls within the scope of the IRAS-approved Biobank and research programme, and is ethically sound and provide evidence that it is likely to make a contribution to scientific/medical knowledge. Applications to the Biobank Ethical Review Committee would be turned down if the applicants decline to provide sufficient information as to the nature of the research, the research is deemed not to advance research, applicants require unrealistic amounts of tissue, or they decline to accept the terms and conditions for tissue supply. Samples/data will only be released from the Biobank to external research groups when appropriate approval is in place and when a material transfer agreement has been signed. The material transfer agreement must ensure compliance with the UCL's policies on storage, data protection, health and safety, disposal, security, training, audit and HTA compliance. 13. BIOBANK ADMINISTRATION Management Protocol (Version 5, 30/5/12) 14of17 13.1 Protocol amendments Substantial amendments of this protocol or associate documents will be notified to the REC and approval sought before any amendments are implemented. The following should always be notified as substantial amendments: Any significant change to the policy for access and use of information in the clinical notes and imaging, and access to tissue in research, including changes to the types of research to be undertaken or supported by the Biobank Any significant change to the types of biological material to be collected and stored, or the circumstances of collection Any significant change to informed consent arrangements, including new/modified information sheets and consent forms A change to the conditions of generic approval Any other significant change to the governance of the RTB 13.2 Governance policy, operating procedures and quality systems The Biobank seeks to work to the following standards as defined by the human tissue authority. Consent Full consent to be taken by trained individuals. Governance & quality systems Policies, procedures and quality management systems to be in place and fully implemented for all licensed activities. All human-derived materials are to be traceable from collection to eventual use or disposal. Premises, facilities and equipment Materials should be kept in appropriate storage conditions that are regularly monitored and maintained. Contingency plans to be in place. Disposal Appropriate disposal procedures with consideration of the wishes of the donor (living person). A number of policies to which staff members are expected to adhere are in force. Areas covered by Biobank policies include: Linking patient consent to use in ethically approved studies Health and safety Staff training Security of data and samples Quality management Access to human material Governance, communication and feedback Disposal So that the Biobank Ethical Review Committee can be satisfied that its researchers are complying with Biobank policies it is a requirement that they register their collections on an annual basis and submit standard operating procedures which cover the areas noted below: Patient recruitment and consent: Process of obtaining consent for medical research that is both generic and enduring Management Protocol (Version 5, 30/5/12) 15of17 Sample and data collection: Process for collecting samples, acquiring and updating clinical data and ensuring data security Sample preparation and quality management: Methods for processing samples for different research and quality assurance procedures Sample tracking: System for linking consent to use in ethically approved projects Storage, inventory and disposal: Systems for inventory control, monitoring storage conditions and maintaining facilities and security. Procedures for disposal Request and allocation: Process for recording requests for samples and monitoring use Retrieval, packaging and distribution: System for removing samples, recording removal and transportation Use in ethically approved projects: Procedure for reviewing requests for samples and ensuring that use is ethically approved, appropriate and that potential users are legitimate. Agreements for material transfer, future use of research data and acknowledgment. Feedback: Systems for returning results (where appropriate) of experiments carried out on banked material. Reporting adverse events. Regular audits will be conducted to ensure quality is maintained. 13.3 Reporting serious protocol non-compliance or breach of policy The REC will be notified as soon as possible of any serious adverse event or reaction, any serious breach of security or confidentiality, or any other incident that could undermine public confidence in the ethical management of the tissue. The Human Tissue Authority will also be notified following standard procedure. 13.4 Clinical adverse event reporting The Tissue Collection Centres have clinical adverse event reporting system in place. This will be used if required. 13.5 Record retention Records of all samples are kept indefinitely and following appropriate regulation. An audit trail will be maintained for all samples including those that have been withdrawn. Certain records will only be accessible to the database manager for audit purposes. Record keeping will be done in a manner ensuring complete confidentiality of patients’ personal details. 13.6 Funding The cost of operating the Biobank will be met by either internal financial support or via grant monies from external sponsors. 13.7 Financial implications for donors There are no financial implications for donors. 13.8 Communication and publication policy Results obtained from research on these tissue samples will be presented at national and international meetings and published in peer reviewed journals. The Biobank expects to be acknowledged in all relevant publications. 13.9 Progress reports and accountability An annual report, including a financial breakdown, will be produced and submitted to the Biobank Ethical Review Committee, listing all projects for which tissue has been collected and/or released in the previous year. The list will provide the full title of each project, the name of the Chief Investigator, the sponsor, the location of the research and the date of Management Protocol (Version 5, 30/5/12) 16of17 approval by the Committee. This report will also be copied to the NRES Committee as described in 3.4.1. Management Protocol (Version 5, 30/5/12) 17of17