Quality Adjustment for Health Care Spending on Chronic
advertisement

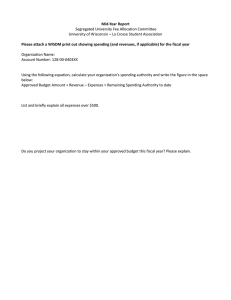
Quality Adjustment for Health Care Spending on Chronic Disease: Evidence from Diabetes Treatment, 1999–2009 The MIT Faculty has made this article openly available. Please share how this access benefits you. Your story matters. Citation Eggleston, Karen N, Nilay D Shah, Steven A Smith, Ernst R Berndt, and Joseph P Newhouse. “Quality Adjustment for Health Care Spending on Chronic Disease: Evidence from Diabetes Treatment, 1999–2009.” American Economic Review 101, no. 3 (May 2011): 206–211. As Published http://dx.doi.org/10.1257/aer.101.3.206 Publisher American Economic Association Version Final published version Accessed Thu May 26 12:32:16 EDT 2016 Citable Link http://hdl.handle.net/1721.1/87608 Terms of Use Article is made available in accordance with the publisher's policy and may be subject to US copyright law. Please refer to the publisher's site for terms of use. Detailed Terms American Economic Review: Papers & Proceedings 2011, 101:3, 206–211 http://www.aeaweb.org/articles.php?doi=10.1257/aer.101.3.206 Quality Adjustment for Health Care Spending on Chronic Disease: Evidence from Diabetes Treatment, 1999–2009 By Karen N. Eggleston, Nilay D. Shah, Steven A. Smith, Ernst R. Berndt, and Joseph P. Newhouse* $700 to more than $6,000 (David M. Cutler, Allison B. Rosen, and Sandeep Vijan 2006). Decomposing medical spending increases into changes in quantity, quality, and medical care– specific prices is difficult. Price indices based on measuring bundles of inputs, such as a day in the hospital or a physician visit, often yield misleading results, since they cannot fully account for changes in the technology of treatment (such as more intensive treatment for shorter lengths of stay) or improved quality of care. Traditional hedonic methods are ill-suited for measuring quality changes in health care: the insured patient does not face the full marginal cost of care, and the patient is not the sole (or even the primary) decision maker for many facets of treatment spending, such as hospital services. One cannot assume that the marginal value of care equals its social cost. Researchers using varying methods to evaluate quality change in health care have differed in their conclusions (Alan M. Garber and Jonathan Skinner 2008). As Rosen and Cutler (2007) note, “while some studies have suggested that [health care] productivity growth is reasonable in aggregate (Cutler and [Mark] McClellan 2001; Cutler, Rosen, and Vijan 2006), others argue that there is substantial waste at the margin ([Elliott S.] Fisher et al., 2003)”. Research dating back to the pioneering work of Anne A. Scitovsky (1967) suggests a promising approach: measuring the changes in quality associated with treatment of a specific medical condition, compared to changes in spending on that condition. Although several researchers have developed methods for allocating spending across diseases to supplement aggregate health expenditure accounts (Rosen and Cutler 2007; Charles Roehrig et al. 2009), much work remains to be done to link spending changes to changes in health outcomes (Susan T. Stewart et al. 2005; National Research Council 2010). This study follows the line of research on price adjustment in medical care started by US health care expenditures reached $2.5 trillion in 2009, representing 17.6 percent of gross domestic product (GDP) and $8,086 per person (US Department of Health and Human Services Centers for Medicare and Medicaid Services 2011). Since health care represents a large and growing share of the economy, and factors such as population aging imply that chronic disease treatment will continue to expand as a share of health expenditures, developing methods for assessing the value of quality improvement for chronic disease spending is of increasing importance for accurately measuring real economic activity. This paper develops a method for assessing the value of quality changes associated with health care for patients living with one important chronic disease, diabetes mellitus, using 11 years of detailed data on spending and quality of care for over 800 patients. We first provide an overview of measurement issues for health care quality, and then present our data, methods, results, and a brief discussion. I. Measuring the Value of Quality Improvements in Health Care Since 1960, real annual medical spending per person in the United States has risen from about * Eggleston: Stanford University Shorenstein AsiaPacific Research Center, 616 Serra Street, Encina Hall E301, Stanford, CA 94305-6055 (e-mail: karene@stanford. edu); Shah: Division of Health Care Policy and Research, College of Medicine, Mayo Clinic, 200 First Street SW, Rochester, MN 55905 (e-mail: Shah.Nilay@mayo.edu); Smith: Division of Endocrinology, Mayo Clinic College of Medicine, 200 First Street SW, Rochester, MN 55905 (e-mail: smith.steven@mayo.edu); Berndt: Massachusetts Institute of Technology Sloan School of Management and NBER, 50 Memorial Drive, Cambridge, MA 02142 (e-mail: eberndt@mit.edu); Newhouse: Harvard Kennedy School; Harvard Medical School; Harvard School of Public Health; and NBER, 180 Longwood Avenue, Boston, MA 02115-5899 (e-mail: joseph_newhouse@harvard.edu). We are grateful for comments from Marshall B. Reinsdorf as well as other discussants and seminar participants at the American Society of Health Economists 2010, AEA 2011, and Stanford University. 206 Quality Adjustment for Health care Spending VOL. 101 NO. 3 Cutler et al. (1998), who analyzed spending and outcomes for patients with heart attacks. Contrary to the perception that health care spending growth far exceeds associated benefits, Cutler and coauthors estimated that a qualityadjusted price index for heart attack treatments declined about 1 percent annually between 1983 and 1994. Jonathan S. Skinner, Douglas O. Staiger, and Elliott S. Fisher (2006) find that overall gains in heart attack survival more than justified the increases in costs during the 1986–2002 period, but since 1996 survival gains stagnated while spending continued to increase. Ernst R. Berndt et al. (2002) found that the incremental cost of treating an episode of acute phase major depression fell between 1991 and 1996. Focusing on cataract surgery between 1969 and 1993, Irving Shapiro, Matthew D. Shapiro, and David W. Wilcox (2001) found that spending has not increased faster than the general price level. Only three studies of which we are aware apply this approach to quality adjustment for expenditures on chronic disease. Alexandra Constant et al. (2006) use data from the Canadian Cancer Registry and the Ontario Case Costing Initiative to calculate that a quality-adjusted price index for cancer treatment declined 5.4 percent annually between 1995 and 2003. Examining colorectal cancer drugs, Claudio Lucarelli and Sean Nicholson (2009) estimate that two quality-adjusted price indices were roughly constant between 1993 and 2005. Eggleston et al. (2009) study diabetes, a chronic condition of growing importance and with an expanding literature on the economics of its management (CDC Diabetes Cost-effectiveness Group 2002; Nancy Beaulieu et al. 2006; Elbert S. Huang et al. 2007; Thomas J. Hoerger 2009). We extend the Eggleston et al. (2009) research, which found that between 1997 and 2005 the benefits of the additional or newer care for diabetes outweighed the greater costs for the average patient. II. Data and Methods A. Data Adjusting spending for quality improvement requires detailed data on changes in spending and quality over time. We use a sample of 821 employees and dependents diagnosed with diabetes enrolled in the Mayo Clinic’s self-funded 207 health plan between 1999 and 2009.1 The data include total direct medical spending for those patients, including all payments made for service use. Prices are actual transaction prices, not list charges. Our estimates are therefore based on “supply” prices, and if these results were used to compare to extant prices indices, they would be akin to the producer price index (PPI) published by the Bureau of Labor Statistics (BLS).2 Spending data are converted to constant 2009 dollars using the GDP deflator.3 B. Methods The net value of total spending is defined as the difference between the monetary value of improved quality (better health status and avoided treatment spending, ΔV ) and the increase in annual inflation-adjusted treatment spending over the 11-year period (ΔC) (i.e., ΔV − ΔC). To measure quality (ΔV ), we use a clinically relevant metric: “modifiable cardiovascular risk” based on the equation for predicting cardiovascular complications from the United Kingdom Prospective Diabetes Study (UKPDS; Richard J. Stevens et al. 2001). We define “modifiable” risk by holding constant the patient’s age and duration of diabetes at their values at cohort entry. Changes in modifiable risk reflect changes in risk factors amenable to control through medical care. A reduction in modifiable risk indicates a quality improvement. We estimate the value of improved probability of survival from reduction in ten-year risk of fatal coronary heart disease (CHD) or fatal stroke using $200,000 as the value of a life year. Since nominal GDP has roughly doubled since the early 1990s when analysts often used 1 We chose to begin in 1999 because earlier administrative records do not provide as comprehensive and consistent data on quality, spending, and absenteeism. 2 See the discussion in Berndt et al. (2000, p. 465). Focusing only on patient out-of-pocket expenditures would be similar to the CPI concept, but changes in out-of-pocket spending reflect not only supply price changes but also insurance benefit design. 3 To reflect opportunity cost in the overall economy, we also tried using the gross domestic purchases price index (which measures the prices of goods and services purchased by US residents, regardless of where the goods and services are produced); the results are very similar to those reported here. 208 $100,000 for the value of a life year, and since W. Kip Viscusi and Joseph E. Aldy (2003) estimate $7 million for the value of a statistical life for a prime age worker in 2000 with an income elasticity of 0.5–0.6, we posit that $200,000 is an appropriate value to use currently. We add the present discounted value of avoided CHD treatment spending, using the Rosen et al. (2007) estimate and assuming a 3 percent real discount rate. Calculating ΔV requires taking the difference between the present discounted value of remaining life at two points in time that correspond to the two technologies being compared: treatment prevailing in the baseline (1999–2001) and final (2007–2009) observation periods, respectively. To do so, we approximate the UKPDS predicted probability of a cardiovascular event in the next ten years, conditional on risk factors in that observation period, by giving a tenth of the predicted probability to each of the first ten years, and assuming that all patients surviving beyond year 10 die at the end of year 20.4 To smooth the variation in annual spending, the increase in spending or costs (ΔC) for each diagnosis cohort is defined by the difference between three-year spending averages for the baseline and final observation periods. For individuals diagnosed within a given three-year interval, we include only spending since diagnosis. For the 33 deaths (Table 1, second row), we include total spending in the year of death. To isolate the impact of technological change while allowing for differences across cohorts diagnosed in earlier or later years, we estimate net value three ways: (i) separately based on the average values for five different diagnosis cohorts, (ii) using the weighted average across diagnosis cohorts; and (iii) at the individual patient level by simulating quality-adjusted life years (QALYs) in the UKPDS Outcomes Model based on patient-specific trajectories of diabetes risk factors and complications. Although we attribute all the change in modifiable risk to medical care, we believe our estimates of net value are conservative for several reasons. First, the spending figures include all medical spending for these individuals, without attempting to isolate what fraction of spending is directly attributable to diabetes. We also assume 4 MAY 2011 AEA PAPERS AND PROCEEDINGS Our results are not very sensitive to this assumption. it costs the same amount to treat CHD in 1999 and 2009 and up to ten years into the future, even though spending for CHD treatment has been rising. We assume a patient with fatal CHD dies before receiving any medical care, even though many patients receive treatment before death. Finally, our estimates do not include the value of reduced treatment spending for strokes or other complications that are avoided by better metabolic control. As greater attention has been given to treatment guidelines for people with diabetes, there is some evidence that the predictions of risk based on the UKPDS trial may underestimate the strength of the association between the level of metabolic control and cardiovascular risk (ADVANCE Collaborative Group 2008; Action to Control Cardiovascular Risk in Diabetes Study Group 2008). III. Results Total real annual health care spending of patients in our sample increased 48.5 percent between 1999 and 2009, for an average annual increase of 4.4 percent based on the weighted average across diagnosis cohorts. Quality generally improved. All diagnosis cohorts except the most recent (2002–2004) experienced a statistically and economically significant reduction in modifiable risk of developing CHD, ranging from −41 percent (1 − (16.7/28.3)) for the pre-1985 diagnosis cohort to −3 percent for the 2002–2004 diagnosis cohort (Table 1). Trends for the other clinical measures were more mixed, generally exhibiting declines in modifiable risk for earlier diagnosis cohorts and little change or an increase for the patients diagnosed most recently. We find that the value of reduced mortality and avoided treatment spending, net of the increase in annual spending, averaged over all cohorts, was $9,094 (although three of the five cohorts experienced a decline in net value; Table 1). Estimates based on the UKPDS Outcomes Model are similar, suggesting that the average patient gained 0.123 QALYs and a net value of US$23,627 ($27,095 when adding avoided CHD treatment spending).5 5 Assuming drugs and other treatment for diabetes must be maintained into the future to achieve the gains the Quality Adjustment for Health care Spending VOL. 101 NO. 3 209 Table 1—Net Value of Increased Medical Spending between 1999 and 2009, by Diabetes Diagnosis Cohort Before 1985 1985–1996 1997–1998 1999–2001 2002–2004 Weighted average 40 5 24.3 178 12 11.7 116 2 6.5 279 9 7.5 208 5 4.9 821 33 8.4 15.1 9.3 7.3 7.9 6.1 6.5 28.3 18.4 14 15.8 12.4 15.9 16.7 11.2 11.1 11.6 12 11.8 $9,206 $186,332 $195,538 $5,803 $48,608 $54,412 $42,106 $30,808 $30,958 $30,821 $195,675 $22,525 $28,003 $21,589 $26,533 $49,468 Year of diagnosis Number of patients Number of deaths 1999 modifiable 10-year risk of fatal CDH or fatal stroke 2009 modifiable 10-year risk of fatal CDH or fatal stroke 1999 modifiable 10-year risk of CHD 2009 modifiable 10-year risk of CHD Saved CHD treatment spending Value of improved survival Total value (improved survival + saved treatment costs) 1999 Mean spending* 2009 Mean spending* Mean spending 1999–2001* Mean spending 2007–2009* Net value of increased spending −$16,202 −$13,157 $3,045 −$8,101 −$4,172 −$24,304 −$22,760 $1,544 $3,863 $8,417 $12,281 $18,235 $18,013 $17,574 $18,898 $13,213 $20,302 $14,816 $19,379 n/a $14,840 n/a n/a n/a n/a $9,094 −$14,481 $3,929 −$8,735 n/a $45,564 −$24,277 Notes: CHD = coronary heart disease. For the 2002–2004 diagnosis cohort, the baseline modifiable risk is for 2002, not 1999. n/a = Not applicable. *In 2009 dollars. Source: Authors’ calculations. IV. Conclusion These results suggest that despite significant expenditure increases, the value of quality improvements for patients with diabetes has generally kept pace with expenditures between 1999 and 2009. In other words, the unit cost of treatment for diabetes, adjusting for the value of health outcomes, has been roughly constant. Since we believe that input prices for health care have not been declining, our results are consistent with productivity improvement in health care. UKPDS model predicts, our values should be (but are not) net of the cost of that continuing treatment for the additional years of life and QALYs. In our study, however, the net increase in life expectancy is a fraction of a year (0.12 years for the average patient based on the UKPDS Outcomes Model), and results about net value are far more sensitive to assumptions about the monetary value of a life-year than to adding “maintenance costs” during additional years of life. Medical care represents a large and growing component of the services sector in the United States and globally (Jack E. Triplett and Barry Bosworth 2004; National Research Council 2010); therefore, further efforts to measure the value of quality changes in health care are important for accurately assessing economic productivity. REFERENCES Action to Control Cardiovascular Risk in Diabetes Study Group. 2008. “Effects of Intensive Glu- cose Lowering in Type 2 Diabetes.” New England Journal of Medicine, 358(24): 2545–59. ADVANCE Collaborative Group. 2008. “Intensive Blood Glucose Control and Vascular Outcomes in Patients with Type 2 Diabetes.” New England Journal of Medicine, 358(24): 2560–72. Beaulieu, Nancy, David M. Cutler, Katherine Ho, George Isham, Tammie Lindquist, Andrew 210 AEA PAPERS AND PROCEEDINGS Nelson, and Patrick O’Connor. 2006. “The Business Case for Diabetes Disease Management for Managed Care Organizations.” Frontiers in Health Policy Research, 9(1): 1–36. Berndt, Ernst R., Anupa Bir, Susan H. Busch, Richard G. Frank, and Sharon-Lise T. Normand. 2002. “The Medical Treatment of Depression, 1991–1996: Productive Inefficiency, Expected Outcome Variations, and Price Indexes.” Journal of Health Economics, 21(3): 373–96. Berndt, Ernst R., David M. Cutler, Richard G. Frank, Zvi Griliches, Joseph P Newhouse, and Jack E. Triplett. 2000. “Medical Care Prices and Output.” In Handbook of Health Economics, Vol. 1A. Vol. 17, Handbooks in Economics, ed. Anthony J. Culyer and Joseph P. Newhouse, 119–80. New York: Elsevier Science. CDC Diabetes Cost-Effectiveness Group. 2002. “Cost-Effectiveness of Intensive Glycemic Control, Intensified Hypertension Control, and Serum Cholesterol Level Reduction for Type 2 Diabetes.” Journal of the American Medical Association, 287(19): 2542–51. Constant, Alexandra, Marie-Chantal Benda, Ruolz Ariste, and Charles D. Mallory. 2006. “Is the Price of Cancer Treatment Falling?” Unpublished. Cutler, David M., and Mark McClellan. 2001. “Is Technological Change in Medicine Worth It?” Health Affairs, 20(5): 11–29. Cutler, David M., Allison B. Rosen, and Sandeep Vijan. 2006. “The Value of Medical Spending in the United States, 1960–2000.” New England Journal of Medicine, 355(9): 920–27. Cutler, David M., Mark McClellan, Joseph P. Newhouse, and Dahlia Remler. 1998. “Are Medical Prices Declining? Evidence from Heart Attack Treatments.” Quarterly Journal of Economics, 113(4): 991–1024. Eggleston, Karen N., Nilay D. Shah, Steven A. Smith, Amy E. Wagie, Arthur R. Williams, Jerome H. Grossman, Ernst R. Berndt, Kirsten Hall Long, Ritesh Banerjee, and Joseph P. Newhouse. 2009. “The Net Value of Health Care for Patients with Type 2 Diabetes, 1997 to 2005.” Annals of Internal Medicine, 151(6): 386–93. Fisher, Elliott S., David E. Wennberg, Thérèse A. Stukel, Daniel J. Gottlieb, F. L. Lucas, and Étoile L. Pinder. 2003. “The Implications of Regional Variations in Medicare Spending. Part 2: Health Outcomes and Satisfaction with MAY 2011 Care.” Annals of Internal Medicine, 138(4): 288–98. Garber, Alan M., and Jonathan Skinner. 2008. “Symposium: Health Care: Is American Health Care Uniquely Inefficient?” Journal of Economic Perspectives, 22(4): 27–50. Hoerger, Thomas J. 2009. “Using Costs in Cost-Effectiveness Models for Chronic Diseases: Lessons from Diabetes.” Medical Care, 47(7S): S21–27. Huang, Elbert S., Qi Zhang, Sydney E. S. Brown, Melinda L. Drum, David O. Meltzer, and Marshall H. Chin. 2007. “The Cost-Effectiveness of Improving Diabetes Care in U.S. Federally Qualified Community Health Centers.” Health Services Research, 42(6, part 1): 2174–93. Lucarelli, Claudio, and Sean Nicholson. 2009. “A Quality-Adjusted Price Index for Colorectal Cancer Drugs.” National Bureau of Economic Research Working Papers 15174. National Research Council, and the Panel to Advance a Research Program on the Design of National Health Accounts, Committee on National Statistics, Division of Behavioral and Social Sciences and Education. 2010. Account- ing for Health and Health Care: Approaches to Measuring the Sources and Costs of Their Improvement. Washington, DC: National Academies Press. Roehrig, Charles, George Miller, Craig Lake, and Jenny Bryant. 2009. “National Health Spend- ing by Medical Condition, 1996–2005.” Health Affairs, 28(2): W358–67. Rosen, Allison B., and David M. Cutler. 2007. “Measuring Medical Care Productivity: A Proposal for U.S. National Health Accounts.” Survey of Current Business, 87(6): 54–58. Rosen, Allison B., David M. Cutler, Douglas M. Norton, Hsou Mei Hu, and Sandeep Vijan. 2007. “The Value of Coronary Heart Disease Care for the Elderly: 1987–2002.” Health Affairs, 26(1): 111–23. Scitovsky, Anne A. 1967. “Changes in the Costs of Treatment of Selected Illnesses, 1951–65.” American Economic Review, 57(5): 1182–95. Shapiro, Irving, Matthew D. Shapiro, and David W. Wilcox. 2001. “Measuring the Value of Cataract Surgery.” In Medical Care Output and Productivity. Vol. 62, Studies in Income and Wealth, ed. David M. Cutler and Ernst R. Berndt, 411–38. Chicago: University of Chicago Press. VOL. 101 NO. 3 Quality Adjustment for Health care Spending Skinner, Jonathan S., Douglas O. Staiger, and Elliott S. Fisher. 2006. “Is Technological Change in Medicine Always Worth It? The Case of Acute Myocardial Infarction.” Health Affairs, 25(2): W34–47. Stevens, Richard J., Viti Kothari, Amanda I. Adler, Irene M. Stratton, and Rury R. Holman. 2001. “The UKPDS Risk Engine: A Model for the Risk of Coronary Heart Disease in Type II Diabetes (UKPDS 56).” Clinical Science, 101(6): 671–79. Stewart, Susan T., Rebecca M. Woodward, Allison B. Rosen, and David M. Cutler. 2005. “A Pro- posed Method for Monitoring U.S. Population Health: Linking Symptoms, Impairments, Chronic Conditions, and Health Ratings.” National Bureau of Economic Research 211 Working Paper 11358. Triplett, Jack E., and Barry P. Bosworth. 2004. Productivity in the US Services Sector: New Sources of Economic Growth. Washington, DC: Brookings Institution Press. United States Department of Health and Human Services, Centers for Medicare and Medicaid Services. 2011. Historical National Health Expenditure Data. http://www.cms.gov/nationalhealthexpenddata/02_nationalhealthaccountshistorical.asp#TopOfPage. (accessed January 15, 2011). Viscusi, W. Kip, and Joseph E. Aldy. 2003. “The Value of a Statistical Life: A Critical Review of Market Estimates throughout the World.” Journal of Risk and Uncertainty, 27(1): 5–76.