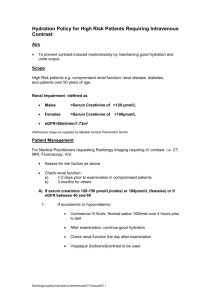
Introduction to the RxFiles Optimizing Medications for Older Adults
advertisement

Introduction to the RxFiles Optimizing Medications for Older Adults Julia Bareham & Dr Brian Martens September 17, 2015 RxFiles 2000: program expanded to provide service to physicians throughout Saskatchewan 2001: efforts to keep our drug selection tools up to date resulted in the publication of the RxFiles Drug Comparison Charts book 2011: program expanded to provide services to long‐term care Academic detailing program Not‐for‐profit Funded by a grant from Saskatchewan Health 1997: began as a service to Saskatoon family physicians This program exists to support health care professionals in making the best possible drug therapy choices for patients. Value is found in the balanced perspectives on drug effectiveness, safety, cost, clinical evidence & patient considerations. RxFiles Comparison Chart 1 RxFiles Resources RxFiles continues to serve health providers and educators through newsletter reviews, Q&As, Trial Summaries, and up‐to‐date drug comparison charts Tools for the front line practitioner wanting to provide the best possible drug therapy for their patients www.rxfiles.ca How much to access? Are you a health care provider in Saskatchewan? Yes? Then, it’s FREE! www.shirp.ca PIP (references) Health Region 2 Yes, there’s an app for that! But wait, there’s more!!!! Want to know more? Patient Case E‐mail me! julia@rxfiles.ca We will come to you!!! Anywhere in Saskatchewan In person, or via TeleHealth Variety of topics to discuss! 82 year old female Hypertension (longstanding) Depression (longstanding) Constipation (“last few years I’ve struggled”) Osteoarthritis (affects mostly her knees) Sleep complaints (“last few years I’ve struggled”) Complaints of worsening memory (“I’ve noticed it the past few months”) Urinary incontinence (diagnosed 8 years ago) Type II Diabetes (diagnosed 3 years ago) 3 There’s an app for that!!! Patient Case Serum creatinine: 112 umol/L Height: 152 cm Weight: 65 kg Estimated Renal Function (using CG equation): 35ml/min Cholesterol Levels: not available Blood Pressure: 127/72 Renal Function EGFR – Now reported on lab results Cr. Clearance – Not the same but close. Different formulas All are estimates! 4 What are your concerns related to your medications? Patient Case Metformin 500mg BID ASA 81mg daily Atorvastatin 20mg Sertraline 50mg daily Colace 100mg BID prn Oxybutynin 5mg BID Amitriptyline 25mg HS HCTZ 25mg daily Ramipril 10mg daily Zopiclone 7.5mg “Various other OTC products” Medication Assessment Tips Brown bag method Line up medication with an indication • Don’t assume an indication by the drug Watch out for prescribing cascades! I want to take fewer medications. I often wonder if I need all of them, and it’s costing me a lot of money each month. “Brown Bag Review” of Medications Encourages pts to bring all of their medications & supplements to medical appointments Provides clinical staff with an opportunity to review & discuss the medications that the pt is taking Reviewing medications with your pt may help you to: • Answer the pt’s questions • Verify what the pt is taking (what & how) • Identify &/or avoid medication errors & DIs • Assist pt to take medications correctly 5 “Brown Bag Review” Did they bring everything? Drugs from MEC’s Herbals from Whatever How often do they take this stuff? How often is it refilled? Intelligent non‐adherence Time‐To‐Benefit (T2B) Time‐To‐Benefit (T2B) & Risk vs Benefit Risks 82 year old female Type II Diabetes (diagnosed 3 years ago) Glycemic targets • A1c 6.5%? • A1c 7.0%? • A1c 8.5%? Benefits 6 T2B: Examples in Diabetes Outcomes of Desire?? ↓ cardiovascular events • ↓ all‐cause mortality ↓ hospitaliza ons ↓ new / worsening nephropathy ↓ re nopathy ↓ neuropathy ↓ foot care complications UKPDS‐34 (metformin vs standard tx in obese T2DM) • • • • (MI, stroke, CV death, HF) Risks Benefits ↓ all‐cause mortality NNT=14/10.7 years ↓ stroke NNT=48/10.7 years A1C achieved was 7.4% vs 8% ~10 years ADVANCE (mostly gliclazide ± metformin) • • • ↓ microvascular events NNT=67/5 years A1C: 6.5 vs7.3 ~5 years Guideline Targets 7 Glycemic Targets Glycemic Targets • • • • • • • *Priority = Hypoglycemia prevention Glycemic Targets Lack of evidence for tight control Maybe over time it improves When individualizing targets, consider: Limited life expectancy Functional dependency Extensive CAD at high‐risk of CV events Multiple co‐morbidities History of recurrent, severe hypoglycemia Hypoglycemia unawareness Available support & resources Risk vs Benefit How well do these drugs even work? Oxybutynin 5mg BID • Antimuscarinic (anticholinergic) • Urinary incontinence • diagnosed 8 years ago; at age 74 8 Risk vs Benefit Caution when using this class of medication in older adults! A retrospective cohort trial in older adult community living centres demonstrated that the benefit of treating with antimuscarinics is almost equal to the risk of causing a hip fracture • NNT for improved urinary incontinence at 90 days = 32 • 95 % CI 17‐125 • NNH for hip fracture at 90 days = 36 • 95% CI 12‐209 Moga DC, Carnahan RM, Lund BC, Pendergast JF, Wallace RB, Torner JC, Li Y, Chrischilles EA. Risks and benefits of bladder antimuscarinics among elderly residents of Veterans Affairs Community Living Centers. J Am Med Dir Assoc. 2013 Oct;14(10):74960. doi: 10.1016/j.jamda.2013.03.008. Risk vs Benefit Cochrane review: • MODEST effect • May result in 4 less leaks & 5 less voids per week • This effect may be useful for some, inadequate for others Nabi G, Cody JD, Ellis G, Herbison P, Hay-Smith J. Anticholinergic drugs versus placebo for overactive bladder syndrome in adults. Cochrane Database Syst Rev. 2006 Oct 18;(4):CD003781. Applying the Guidelines to Older Adults 9 Blood Pressure Targets Harms of sustained too‐high BP seen especially >160mmHg systolic Harms of too‐low BP seen especially: • <60mmHg diastolic for stroke & CVD risk • <70‐75mmHg for overall mortality Not too much, not too little, but just right! Blood Pressure Targets If the older person is dizzy, unsteady or falling, reassess BP meds and BP targets! Guideline targets >80yrs: • Blood Pressure Targets Do you get dizzy when you get up? Tired? <150mmHg over <90mmHg Individualize the target. • Risk vs Benefit Let the target serve the patient, not the patient the target! 10 Back to the case… HCTZ 25mg daily Ramipril 10mg daily Blood pressure 127/72 Type II Diabetes Urinary Incontinence Anticholinergics dry mouth blurred vision constipation drowsiness sedation hallucinations memory impairment difficulty urinating confusion delirium decreased sweating decreased saliva Back to the case… Metformin Low dose ASA Atorvastatin Sertraline Colace Oxybutynin Amitriptyline HCTZ Ramipril Zopiclone 11 Shared Decision‐Making Genetic & cancer screening tests? Respect for the pt’s values, preferences, & expressed needs Clear, high‐quality information & education for the patient and family Involves at minimum a clinician & the pt • • • Both parties share information Clinician: offers options & describes their risks & benefits Pt: expresses his/her preferences & values Statin everyday for primary prevention? “What matters to you?” as well as “What is the matter?” Barry MJ, Edgman-Levitan S. Shared decision making--pinnacle of patient-centered care. N Engl J Med. 2012 Mar 1;366(9):780-1. Shared Decision‐Making What is important to the patient? Patient values Risk / Benefit Present Both Sides • There is data on benefit available from different treatments Document! Decision Aids pt’s awareness & understanding of treatment options & possible outcomes Online, paper, videos Can efficiently help patients absorb relevant clinical evidence & aid them in developing & communicating informed preferences Result of using these tools (Cochrane review): • • • • • knowledge More accurate risk perceptions # of decisions consistent with pt’s values level of internal decisional conflict for pts Fewer pts remaining passive or undecided Barry MJ, Edgman-Levitan S. Shared decision making--pinnacle of patient-centered care. N Engl J Med. 2012 Mar 1;366(9):780-1. 12 Decision Aids http://shareddecisions.mayoclinic.org Succinct, easy to use tools that provide graphic displays of the benefits & harms of different options organised around concerns that are important to patients BREAK 13 Deprescribing polypharmacy • risk of adverse events • risk of drug interactions • pill burden • medication costs Deprescribing Considerations Medicines can be grouped as: 1. Those that keep the pt well and improve day‐to‐day QOL • • 2. Those that are used for the prevention of illness in the future • • In some circumstances, the only way to know whether or not to stop a medicine is to actually stop it & see what happens. Factors to consider when deciding if a medicine can be stopped include: • • • • • • The wishes of the pt Clinical indication & benefit Appropriateness Duration of use Adherence The prescribing cascade e.g. statins, aspirin, warfarin or bisphosphonates Consider the risks & benefits, T2B, life expectancy A practical guide to stopping medicines in older people. Best Practice Journal 2012;27 Alexander GC, Sayla MA, Holmes HM, Sachs GA. Prioritizing and stopping prescription medicines. CMAJ 2006;174(8):1083-4. Deprescribing Considerations e.g. analgesics, thyroxine or anti‐anginals In some cases, if these medicines are stopped, the pt may become ill or unable to function. However, some drugs may be able to be stepped down, stopped or used on an as required basis (prn) Deprescribing I am a hypocrite! Need a motivated patient and/or family Generally successful Go slow • Discussion • Time! Review results 14 Deprescribing Go for the low hanging fruit! Not Motivated • Won’t work (Patient values) • Hardest • • Metformin sleeping pills vitamins Docusate Docu‐Don’t Triple Whammy Docusate appears to be no more effective than placebo for stool frequency or softening stool consistency It does not appear to lessen symptoms associated with constipation (i.e. abdominal cramps) or affect the perceptions associated with completeness of or difficulties with stool evacuation http://www.cadth.ca/media/pdf/htis/nov‐ 2014/RC0561%20Stool%20Softeners%20Final.pdf Risk of acute kidney injury when an ACEI or ARB is combined with a diuretic and NSAID Who would take this combo? • hypertension, congestive heart failure, or renal disease who has arthritis or other mild to moderate pain PL Detail-Document, The “Triple Whammy.” Pharmacist’s Letter/Prescriber’s Letter. April 2013. 15 Zopiclone – New Warning! Recommended starting dose has been to 3.75 mg The lowest effective dose for each pt should be used The prescribed dose should not exceed 5 mg in elderly pts, in pts with hepatic or renal impairment or those currently treated with potent CYP3A4 inhibitors. Dose adjustment may be required with concomitant use with other CNS‐depressant drugs. SSRIs – SIADH & GI Bleeds SIADH & hyponatremia Risk factors: SSRIs, diuretics, age, volume depletion Sertraline + HCTZ http://healthycanadians.gc.ca/recall‐alert‐rappel‐avis/hc‐ sc/2014/42253a‐eng.php SSRIs – SIADH & GI Bleeds GI Bleeds Risk factors: SSRIs, NSAIDs, age SSRIs are associated with a modest in the risk of upper GI bleeding. This risk is significantly elevated when SSRI medications are used in combination with NSAIDs Setraline + ASA (+OTC Aleve) Metformin & Renal Function When to Discontinue, Decrease or Keep Going??? Anglin R, Yuan Y, Moayyedi P, Tse F, Armstrong D, Leontiadis GI. Risk of upper gastrointestinal bleeding with selective serotonin reuptake inhibitors with or without concurrent nonsteroidal anti-inflammatory use: a systematic review and meta-analysis. Am J Gastroenterol. 2014 Jun;109(6):811-9. 16 What do We Know? Almost always the first‐line drug of choice, except possibly for a lean, frail older adult No RCTs of metformin in the elderly, although clinical experience suggests it is an effective agent Minimal risk of hypoglycemia Must be initiated with a low dose & titrated up to minimize GI upset May be used in individuals with but STABLE renal function, at a dose Metformin & Renal Function Adjust dose for renal function! Current Canadian and American Guidelines suggest to avoid if CrCl <30ml/min due to risk of lactic acidosis; however, it is rational to have some flexibility with this suggested cut‐off. What do We Know? Metformin is a good, useful drug • insulin requirements Cheap! Does not cause weight gain Shown to reduce cardiovascular mortality rates in T2DM Metformin & Renal Function Given the outcome benefits seen with metformin, & the rare and controversial concern of its association with lactic acidosis, it is sometimes used cautiously in patients with even lower renal function. • • Alternative drugs carry their own risks (hypoglycemia with SUs; edema, weight gain, HF & fractures with TZDs) & often less evidence of benefit & safety in this population. It has been suggested that the risk of death as a result of sulphonylurea (or insulin) induced hypoglycemia in CKD ps is likely to be greater than the risk of death due to metformin‐associated lactic acidosis. 17 Suggested Maximum Dosing of Metformin Based on Renal Function Monitor renal function at regular intervals (via estimated CrCl) No renal impairment: ≤ 2550 mg/d Monitor with normal follow‐up CrCl 60‐90 ml/min: ≤ 1700 mg/d CrCl 60‐90 ml/min: Every 6 months CrCl 30‐60 ml/min: ≤ 850 mg/d CrCl 30‐60 ml/min: Every 3‐4 months CrCl < 30ml/min (&/or dialysis): Avoid N/A What About Lactic Acidosis? Metformin‐induced lactic acidosis • Rare! 1 to 9 cases/100,000 patient years • Link could be coincidental rather than causal Lactic acidosis risk factors: • Conditions that cause hypoxemia • Acute Cardiovascular Condition– heart failure • Acute Renal Condition – contrast media for diagnostic purposes • Acute Hepatic Condition – severe hepatic dysfunction • Respiratory failure • Sepsis • Hypovolemia RxFiles Q&A Metformin: Precautions with Renal Impairment, Hepatic Disease and Heart Failure Lactic Acidosis Life‐threatening event (40‐50% death rate) Onset is subtle, accompanied by non‐specific symptoms: • Malaise • Myalgias • Respiratory distress • somnolence • Abdominal distress Labs: • Low pH • anion gap • Elevated blood lactate Meds to Hold in Acute GI Illness Medications/Medication Classes to Hold in Acute GI Illness risk for a decline in renal function S Sulfonylureas (i.e. gliclazide Diamicron, glimepiride Amaryl, glyburide Diabeta) A ACE‐inhibitors (e.g. lisinopril Zestril, Prinivil, perindopril Coversyl, ramipril Altace) D Diuretics (e.g. hydrochlorothiazide, furosemide Lasix) Direct renin inhibitors (i.e. Aliskiren Rasilez) M Metformin clearance leading to risk of adverse events Glucophage, Glycon A Angiotensin receptor blockers (e.g. candesartan Atacand, valsartan Diovan) N NSAIDs (e.g. ibuprofen Advil, naproxen Aleve) & COXIBs (e.g. celecoxib Celebrex) 18 And now for a little musical interlude… https://www.youtube.com/watch?v=Lp3pFjKoZl8 CDA 2013 http://guidelines.diabetes.ca/CDACPG_resources/Appendices/Appendix_7.pdf Improving Communication Amongst the Interdisciplinary Team I am no expert Team Conferences (Long‐Term Care) Team Conferences Problems – Time, Time, Time, Time, Time, etc. Hard to do even one per year Ministry of Health mandates 4 per year Impossible • Best time for discussion between groups 19 Care By Design From Halifax Dr. assigned to a Unit / Floor (25 residents) Weekly scheduled review times Paramedic support Evidence‐based guidelines Sources of Information Best Science Medicine podcast RxFiles InfoPoems podcast Cochrane Review podcast “A Bitter Pill” by Dr. John Sloan Need to Change! Phone a friend. Or text. Or e‐mail. Or fax. druginfo@usask.ca (306) 966‐6340 [Saskatoon] 1‐800‐667‐DIAL (3425) Text: (306) 260‐3554 Fax: (306) 966‐2286 http://medsask.usask.ca/ 20 Questions?? julia@rxfiles.ca 21