Immunosuppression, induced upon intradermal infections, causes failures of
advertisement

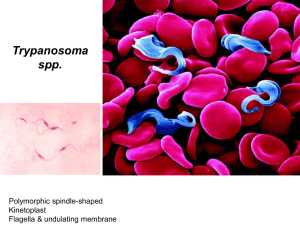
Immunosuppression, induced upon intradermal infections, causes failures of vaccines against African trypanosomiases. Henry Tabel1*, Guojian Wei1, Harold Bull2 1 Department of Veterinary Microbiology, University of Saskatchewan, Saskatoon, Saskatchewan, Canada, 2 Department of Microbiology and Immunology, University of Saskatchewan, Saskatoon, Saskatchewan, Canada Oct. 2, 2012 *e-mail address: henry.tabel@usask.ca Abstract African trypanosomes are hemoprotozoa that cause disease in humans and livestock. Each trypanosome is covered by a single layer of about 107 identical molecules of surface glycoprotein. It is generally believed that the almost unlimited capacity for antigenic variation of the surface glycoprotein is the major impediment for developing vaccines against African trypanosomiases. We have discovered contradictory evidence to this assumption. We found that, in contrast to infections of the blood, infections of the skin with low numbers of trypanosomes are controlled by innate resistance and the few killed trypanosomes induce enhanced susceptibility to reinfections. We argue that induction of immunosuppression by trypanosomes infecting the skin is the major impediment for developing effective vaccines. The role of suppressor macrophages and their L-arginine metabolism as well as the role of NKT cells in the immunosuppression are discussed. We propose a novel strategy for vaccine development to induce protective immunity to trypanosomal infections. The major thrust of this strategy is to use an intradermal vaccination procedure that counteracts the induction of immunosuppression and induces a Th1 imprint. We think this strategy may have relevance to the development of vaccines against other hemoprotozoal infections. Introduction African trypanosomes are pathogens of humans and livestock. Various members of the genus Trypanosoma are responsible for disease syndromes called African trypanosomiases [1]. Trypanosoma brucei gambiense and T. b. rhodesiense cause sleeping sickness in humans, also called human African trypanosomiasis (HAT), an emerging disease in East and Central Africa [2,3]. Infections in livestock with T. congolense, T. vivax, or T. b. brucei cause anemia, hypocomplementemia, cachexia, and susceptibility to secondary infections [1,4,5]. Various species of tsetse flies (Glossina spp.) can harbor African trypanosomes and act as their intermediate hosts. Humans and animals become infected with trypanosomes by bites of infected tsetse flies. A temporary local inflammation, the so-called chancre, develops in the skin at the site of the bite [6]. The trypanosomes move from the skin into the blood via the lymph system [7,8] (Fig. 1). African trypanosomes are single-cell, extracellular blood parasites. Shared characteristics of the different species of African trypanosomes include the ability to produce almost unlimited antigenic variation of their variant surface glycoprotein (VSG) [9,10,11] and to induce a predominantly T cell-independent antibody response to the VSG [12,13,14,15,16], profound immunosuppression [17], polyclonal B cell activation [18,19,20] and persistent hypocomplementemia [5,21,22] in infected mammalian hosts. Infections of mammalian hosts lead to cycles of parasitemia 1 associated with expression of new VSGs [9,11]. Each new VSG initially elicits a strong immunoglobulin M (IgM) anti-VSG response [9,16,19], which leads to phagocytosis of the trypanosomes, predominantly by macrophages of the liver [23,24,25,26]. Currently, there are no effective vaccines against African trypanosomiases, neither for humans nor for livestock. Figure 1. Mode of natural infections by African trypanosomes. Infected tsetse flies bite the host by inserting the proboscis into the skin, inject saliva into the site and puncture a small blood vessel, resulting into a small hemorrhage. The tsetse fly is sucking blood from the hemorrhage. During this process trypanosomes are deposited into the skin. Trypanosomes enter the lymph system and then reach the draining lymph node and the blood stream. Trypanosomes will circulate in the blood stream. Whole trypanosomes or fractions thereof end up by antibody- and/or complement-mediated phagocytosis in macrophages of liver and spleen. Resistance to infections by African trypanosomes In vitro, African trypanosomes can be killed by antibody/complement-mediated immune lysis [23,24], antibody-mediated phagocytosis by macrophages [25,26,27] and nitric oxide (NO) produced by macrophages [28,29]. Regarding infections in vivo, it is important to distinguish clearly between resistance to intradermal infections by low numbers of parasites and resistance to blood stage infections. Primary intradermal infections by low numbers of parasites in the skin are controlled by innate immunity mediated by induced nitric oxide [30]. At this stage, adaptive immune responses are not protective but are immunosuppressive [30] (discussed below). At the blood stage of infection, antibodies are absolutely required for the control of parasitemia [31,32,33,34]. Complement-mediated immune lysis of trypanosomes in vivo does not appear to be a major protection mechanism providing long-term survival. Complement C5-deficient mice (B10.D2/oSnJ) had survival times similar to those of control mice (B10.D2/nSnJ) when infected with either T. b. rhodesiense [35] or T. congolense (Tabel & Wei, unpubl.). Considering the marked hypocomplementemia in humans [21], livestock [5,22] and mice [36] infected with trypanosomes, the benefit of immune lysis is presumably cancelled out by detrimental pathological effects [24]. Because 2 of antigenic variation, each wave of parasitemia represents a new antigenic variant and is controlled by a variant-specific antibody response. This variant-specific immunity can be transferred by B cells but not by T cells [32]. The anti-VSG antibody response is both T cell-independent and T cell-dependent [12,16,37]. Although IgM antibodies to VSG are the major class of antibodies which do reduce parasitemia [38,39] and mediate phagocytosis of trypanosomes by the macrophage system [26,39], they do not enhance the survival time of infected mice [33,40]. There is evidence that IgG anti-parasite antibodies are required for survival of mice infected with T. b. rhodesiense [40] or T. congolense [33] and that anti-parasite-specific IgG2a and IgG3 antibodies, but not IgG1, are associated with protection [33,41]. The latter observation would indicate that responses by Th1 cells are associated with protection, which is confirmed by other findings [42,43]. Cumulative evidence suggests that for maximum resistance against trypanosomes, parasite-specific Th1 cells activate macrophages via IFN-γ to produce NO which is cytostatic for the trypanosomes [33,42,43,44]. The dilemma for the overall outcome of the infection is the fact that parasite-specific Th1 cells also mediate immunopathology [45,46,47,48,49] and NO is a major mediator of immunosuppression (see below). Protective anti-parasite immune responses wane with progression of chronic infections [50,51]. Mice that have developed parasitemia will eventually die. Their survival time depends on the virulence of the infecting parasite and the genetic resistance of the infected mice [52,53,54,55,56]. In some cases, however, self-cure does occur [15,57]. Why are there no effective vaccines? African trypanosomes have developed a highly sophisticated and complex system of antigenic variation [9,10,11]. In the mammalian host, the whole parasite is covered with a coat of about 107 identical molecules of a glycoprotein, the variant surface glycoprotein (VSG). The VSG is anchored into the cell membrane via a glycolipid, glycosylphosphatidylinositol (GPI) [58,59]. There is a widely held belief that the almost unlimited capacity for antigenic variation of the surface glycoproteins by the African trypanosomes is the major hurdle for producing a vaccine [17,60,61,62,63]. In view of our recent experimental results on intradermal infections with low numbers of trypanosomes [30,64], we do not share this belief. Several comprehensive reviews on the immunobiology of infections with African trypanosomes have been published [17,43,45,49,56,65,66,67,68]. Past research into the immunobiology has mostly been based on the immune responses of mice infected intraperitoneally, a route of infection that leads to development of parasitemia [17,33,43,56,65,69,70]. Although these studies have provided great insight into the host-parasite relationship, they have neglected to investigate the very early immunological events triggered by the infecting parasites. In nature, mammals become infected by skin bites from trypanosome-infected tsetse flies [1]. Thus, we have developed a model for intradermal infections of mice [30,64,71]. Intraperitoneal infections of mice with either T. brucei [16,17,31] or T. congolense [33,39] lead to infections of the blood and definitely require antibodies to VSG for the control of parasitemia. In contrast, we found that intradermal infections by low numbers (100-500) of African trypanosomes are controlled by innate resistance involving induced nitric oxide (iNO) and TNF-α, but require neither antibodies nor T cells for protection [30]. Relevant to these results, it was found that the average man required a minimal dose of 300-450 metacyclic T. b. rhodesiense to be infected by the bite of a tsetse fly [72]. We further provided evidence that primary intradermal infections were better controlled in CD1d-/- or MHC class II-/- mice, indicating that the innate resistance to low numbers of trypanosomes in primary intradermal infections is somewhat suppressed by CD1d-restricted natural killer T cells 3 (NKT cells) and MHC class II-restricted T cells [30]. Primary intradermal infections by 100-500 African trypanosomes which, in fact, are killed by innate resistance, not only failed to generate a longterm protective immunological state but resulted in enhanced susceptibility to intradermal challenges [30]. Even more surprisingly, intradermal injection of mice with a trypanosomal lysate, i.e., trypanosomes killed by sonication, does not provide protection but makes such mice more susceptible to an intradermal challenge [30]. The enhanced susceptibility to intradermal challenge is unrelated to antigenic variation. We suggest that intradermal infections with low numbers of trypanosomes or injections with mechanically killed trypanosomes prime the adaptive immune system to suppress protective immunity to an intradermal challenge. All previous attempts to produce vaccines against African trypanosomes were only partially successful or failed entirely, because they did not deal with the stated problem of induction of immunosuppression by infecting trypanosomes. A comprehensive review on previous vaccination attempts has been published recently [73]. We propose that in any attempt to produce an effective vaccine, it would be crucial to address the problem of induction of immunosuppression by the trypanosomes injected into the skin by infected tsetse flies. Immunosuppression in humans and animals infected by African trypanosomes Immunosuppression to heterologous antigens: Immunosuppression in mice infected by T. brucei was discovered as depressed immune responses to heterologous antigens, measured by plaqueforming assays (PFC), i.e. lower numbers of B cells specific for sheep red blood cells (SRBC) [14,19,55,74,75,76]. Humans [77], cattle [78,79,80,81] and mice [82] infected by African trypanosomes also showed lower immune responses to vaccines. Another characteristic of T. brucei or T. congolense infections of mice or cattle is the reduced proliferation of T cells in response to stimulation by T cell mitogens, such as ConA or PHA [75,83,84,85,86,87,88,89,90,91]. These observations would explain the enhanced susceptibility to secondary infections in T. b. gambiense infections in humans [77] and T. congolense and T. vivax infections in cattle [4]. Infections of mice with T. congolense or T. brucei lead to a disruption of the lymphoid architecture of the spleen, a gradual disorganization of the white pulp with eventual lymphoid depletion [82,92]. Immunosuppression to trypanosomal antigens: The suppression of immune responses to the infecting trypanosomes is not as well documented. Because intraperitoneal infections of mice always lead to infections of the bloodstream, there is a technical problem of demonstrating parasite-specific immunosuppression in such an experimental design. In a somewhat artificial experimental design, mice were infected with live T. brucei together with complete Freund’s adjuvant into the skin. Immunosuppression to trypanosomal antigens was demonstrated in these mice [50,93]. Lymph node cells taken 1-2 weeks after infection showed a proliferative response to T. brucei antigens [93]. In contrast, T cells taken from mice 3 weeks after infection no longer proliferated in response to T. brucei antigens [50]. Sacks and Askonas [51] showed trypanosome-induced immunosuppression of anti-parasite responses by infecting mice intraperitoneally with one clone of T. brucei and then immunizing these mice with irradiated trypanosomes of a noncross-reacting clone. The suppression of antibody response to the irradiated trypanosomes was virtually complete, resulting from acute infection by a highly virulent clone. The authors also tested the anti-VSG antibodies to homologous variants in a chronic infection after each of three waves of parasitemia. As the infections progressed, IgM and IgG anti-VSG 4 antibody responses declined. IgG antibodies declined more rapidly. After the third parasitemia, only low levels of IgM anti-VSG antibodies were detectable. Schleifer and Mansfield [94] infected mice with T. b. rhodesiense and prepared spleen cell cultures from these mice. They measured the proliferative response to VSG. They found that the proliferation index increased 3-fold, when they incorporated NG-monomethyl-L-arginine (NMMA), an inhibitor of nitric oxide synthase. These results indicated an NO-mediated suppression of response of VSG-specific T cells in the infected mice. Dagenais et al. [95] infected B10.BR mice intraperitoneally with T. b. rhodesiense and produced T cell hybridomas from spleen cells collected 1 week after infection. Of 11 hybridomas, which were specific for various VSG peptides, none of the hybridomas recognized epitopes of the relatively conserved invariant sequences of the VSG C-terminal domain. Although there is no proof, the results might indicate that T cells specific for the invariant VSG Cterminal domain become already suppressed or deleted within 1 week after the infection by T. b. rhodesiense. Of course, for a vaccine to be protective, the host has to produce memory T cells specific for common antigens of the parasite, such as the invariant domain of the VSG. Mechanisms of immunosuppression Historically, explanations for the mechanisms of immunosuppression had been conflicting, leaving unresolved whether immunosuppression is mediated by suppressor macrophages [76,96] or by suppressor T cells [97]. In 1984, Roelants and Pinder [17] carried out an extensive review and concluded both types of cells are involved. Askonas’ lab has convincingly shown that macrophages become immunosuppressive after antibody-mediated phagocytosis of T. brucei [65]. Suppressor macrophages play a predominant role in the immunosuppression at the blood stage of infection by African trypanosomes [76,83,87,88,89,91,98,99]. The induction of suppressor macrophages and their effector mechanisms appear to be complex and are by no means sufficiently elucidated. Phagocytosis of whole trypanosomes, membrane fractions or glycolipid fractions of the membrane made macrophages immunosuppressive [65,100,101]. The major component of trypanosomes that activates macrophages appears to be the GPI [102,103,104,105], the membrane anchor of the VSG, similar to the activation of macrophages by the GPI of Plasmodium falciparum [103,104,106,107]. Such macrophages are highly activated, producing prostaglandin E2, plasminogen activator, H2O2, O-2, IL-1, but have lower expression of mannose receptor, FcR and CR3 [65]. They also produce enhanced amounts of TNF-α, IL-6, IL-12, IL-10 and NO [28,108,109]. There appears to be a general dysregulation of homeostasis of these macrophages, eventually leading to their apoptosis [110]. The degree and pattern of activation depends on the genetics of the macrophage [28,108,109], the class of antibody opsonizing the trypanosomes [28], the number of engulfed trypanosomes and the virulence of the trypanosome [55,111]. Nitric oxide: In 1992, Sternberg et al. discovered that NO produced by macrophages is a mediator of immunosuppression in T. brucei infection of mice [89]. NO is a major mediator of immunosuppression in mice infected intraperitoneally [69,98,112,113,114], but only during the early phase of infection of the blood [69,112]. The phagocytosis of trypanosomal antigen does not result in the production of a great amount of NO in macrophages. It is the stimulation of such macrophages by IFN-γ that, in synergy with TNF-α, induces the synthesis of high amounts of NO [28,69,94,112,114]. In turn, the highly activated macrophages stimulate the interacting T cells to unusually high synthesis of IFN-γ [69,90,91,94,112,115,116]. Parasite-specific Th1 cells potentially induce protective immune responses by eliciting an IFN-γmediated NO synthesis in antigen-presenting macrophages, leading to killing of trypanosomes. Under 5 heavy trypanosome load, the macrophages can turn into “suppressor macrophages” preventing, by a NO-mediated mechanism, the proliferation of Th1 cells [94,113]. The production of cytokines by the incapacitated Th1 cells apparently continues [113]. In T. brucei-infected mice [86,87,117] and T. congolense-infected cattle [88] the IL-2 receptor of T cells is down-regulated. There is evidence that NO [84] as well as IFN-γ [118] mediate the down-regulation of the IL-2 receptor. NO is not the only mediator of immunosuppression. Prostaglandin E2 produced by the suppressor macrophages also contributes to the immunosuppression [65,87,94], possibly by reducing the production of IL-2 [87]. M1 versus M2 macrophages: The diverse biological activity of macrophages is mediated by phenotypically distinct subpopulations of cells that develop in response to inflammatory mediators in their microenvironment. Two major populations have been characterized: classically activated M1 macrophages and alternatively activated M2 macrophages [45,119]. The M1 type develops upon activation by IFN-α/β, IFN-γ and/or TNF-α. The M2 type develops after activation by IL-10, IL-4, and/or IL-13 [120]. Activation of the inducible nitric oxide synthase (iNOS or NOS2) has been regarded as one of the most specific marker for M1 macrophages and activation of arginase 1 (Arg1) the most specific marker of M2 macrophages121. Both types of macrophages have been associated with immunosuppression. The L-arginine metabolism in macrophages controls T-lymphocyte function [121,122]. Both the arginase pathway and the iNOS pathway use L-arginine as their substrate. Both pathways compete for the available L-arginine and cross-regulate each other [121]. In tumors, M1 macrophages produce high amounts of NO which has been found to interfere with IL-2R signaling in T cells [120,121]. The NO-producing suppressor macrophages observed in C57BL/6 mice infected intraperitoneally by T. brucei appear to be of M1 type. The suppressive effect of M2 macrophages in Leishmania major skin infections of BALB/c mice has been associated with local depletion of Larginine by arginase, impaired proliferation of T cells in the skin lesion and impaired production of IFN-γ [122]. In mammary carcinoma 4T1 of BALB/c mice, suppressor macrophages are polarized by interleukin 13 (IL-13) towards the M2 type with increased metabolism of L-arginine by enhanced activity of arginase [123]. Enhanced arginase activity can lead to exhaustion of L-arginine. T cells stimulated and cultured in the absence of L-arginine, present a sustained down-regulation of CD3zeta preventing the normal expression of the T cell receptor (TCR) [124]. Despite the distinct expression of iNOS and Arg1 in M1 and M2 macrophages, respectively, some macrophages have been shown to express both iNOS and Arg1 [120]. Thus, macrophages of mixed characteristic do exist. In tumor bearing mice, Foxp3+CD4+ Tregs can be induced by a pathway requiring IL-10 and IFN-γ [125]. This is reminiscent of macrophage-mediated immunosuppression in highly susceptible BALB/c mice intraperitoneally infected by T. congolense , which is mediated by IL10 and IFN-γ but not by NO [91]. BALB/c mice are highly susceptible to T. congolense [56] and also more susceptible to T. brucei [126] than relatively resistant C57BL/6 mice. In mice intraperitoneally infected with T. brucei, arginase mRNA is expressed higher in peritoneal macrophages of infected BALB/c than in those of infected C57BL/6 mice. In co-cultivation with macrophages, T. brucei directly induces increased arginase 1 and arginase 2 mRNA levels in macrophages as well as increases macrophage arginase activity, with higher levels in BALB/c than in C57BL/6 mice [127]. The mechanism is unknown. Under the same conditions, neither iNOS expression nor NO production is stimulated. Host arginase appears to be a marker of susceptibility/resistance to trypanosome infections [127]. From two days on after infection, arginase activity is increasingly up-regulated in peritoneal macrophages of Swiss mice subcutaneously infected with T. brucei. Under the same conditions, increasing iNOS activity is delayed by a couple of days [44]. 6 Immunity to infections is mediated by memory T cells and B cells, which are generated from naïve precursor cells after exposure to the microbial antigen. Upon interaction of naïve T cells with the antigen-presenting cell, naïve T cells rapidly proliferate and differentiate into effector T cells. This phase of proliferation lasts about 1 week and is followed by a contraction phase of about 14 days during which about 90 % of the effector T cells die whereas the remaining cells differentiate into memory T cells [128,129]. We conclude that, in African trypanosomiasis, there is a lack of expansion of trypanosome-specific Th1 cells and little or no development of Th1 memory cells specific for variant and common parasite antigens. We contend that, at the intradermal stage of infection, the immunosuppression is predominantly controlled by suppressor T cells [30] and possibly a mixed M1/M2 macrophages environment [44,120,127], whereas at the early parasitemic stage of infected C57BL/6 mice, this process is predominantly controlled by M1 suppressor macrophages [69,94,112]. Immunobiology of intradermal infections Knowledge of the immunological events in primary intradermal infections by African trypanosomes is very limited. Nevertheless our recent investigation [30] provides some unexpected findings and allows some fundamental conclusions. Resistance to low numbers of trypanosomes in primary intradermal infections: We have shown that, upon intradermal infection, low numbers (100-500) of trypanosomes are killed by innate immunity. Contrary to blood stage infections, intradermal infections do not require B cells or T cells to induce resistance. The innate resistance is mediated by induced NO and TNF-α [30]. What processes might lead to innate resistance to intradermal infections by low numbers of trypanosomes? T. brucei [130] and T. congolense [131] isolated from infected blood can have cleavage products of complement component C3 on their surface. T. brucei [132,133] as well as T. congolense [134] can form filopodia (slender membrane protrusions). Immune complexes of anti-VSG antibody and complement have been shown to be shed via filopodia [134], which, in turn, can be taken up by macrophages [27]. Thus, it is conceivable that trypanosomes with iC3b on their surface will temporarily attach to macrophages via CR3 (CD11b/CD18) [26]. It might be possible that, even in the absence of anti-VSG antibodies, a certain threshold number of iC3b-CR3 interactions might induce formation of filopodia. We speculate that these filopodia might separate from trypanosomes and then are engulfed by macrophages, without harming the trypanosomes involved. This process might activate these macrophages to synthesize TNF-α and induce them to synthesize and secrete NO. Macrophagederived TNF-α might, in an autocrine fashion, enhance synthesis of NO by the macrophages [135]. We suggest that all trypanosomes that subsequently attach to these activated macrophages are killed by NO-mediated products, such as nitrosylated proteins [136,137] (Fig. 2). Potential enhancement of the innate resistance by CD1d-restricted NKT cells [71] appears to be suppressed by other T cells [30,49,71]. 7 Figure 2. Proposed mechanism of resistance to low numbers of trypanosomes in primary intradermal infections. We anticipate that trypanosomes release a yet unknown substance that induces Arg 1 and Arg 2 in macrophages that are in close vicinity to these trypanosomes [129], skewing such macrophages towards M2 type. We contend that filopodia are engulfed by macrophages via iC3b-CR3 interaction and that the iNOS pathway gets stimulated by the GPI contained in the filopodia, skewing such macrophages predominantly to a M1 type (see text). The activated macrophages then kill surrounding trypanosomes via NO mediated process, predominantly via S-nitrosylated proteins [138]. Immunosuppression in primary intradermal infections: Highly susceptible BALB/c mice infected intradermally with 104 T. congolense develop parasitemia and die within 10 days. Treatment with an optimal dose of anti-CD25 antibodies of such infected BALB/c mice prevents the development of parasitemia and the mice remain entirely healthy [71]. There is evidence that induction of CD4+CD25highFoxp3+ T cells (Treg) down-regulate potential protective immune responses, since the spleens of the mice treated with anti-CD25 antibodies had a 100% reduction of CD4+CD25high T cells and a 75% reduction of CD4+CD25+Foxp3+ T Cells [71]. Intradermal infections of relatively resistant C57BL/6 mice with 104 T. congolense lead to development of parasitemia and disease [30]. CD1d-/- C57BL/6 mice infected with the same dose are completely protected and MHC class-II-/- C57BL/6 mice are mostly protected (8/10) [30]. These results indicate that in wild-type C57BL/6 mice intradermally infected with 104 T. congolense, the innate immunity is down-regulated by CD1d-restricted NKT cells139 and also by MHC class-II-restricted T cells. CD1d is an MHC class-I-like molecule that presents glycolipid antigens to a subset of T cells called natural killer T cells (NKT cells [138,139]. There are two subpopulations of NKT cells that vary in the programming of the T cell receptor (TCR): invariant NKT cells (iNKT), type I and variant NKT cells, type II. Both types of NKT cells recognize, with their TCR, lipids presented by CD1d expressed on the surface of antigen-presenting cells (APC) [140]. Type I NKT cells, upon interacting with APC, predominantly produce IFN-γ and activate the iNOS pathway in the APC, whereas type II NKT cells produce IL-13 and activate the Arg 1 pathway in APC [140,141]. There is evidence that there is crossregulation between the two types of NKT cells [140,141]. Since the innate resistant to intradermal infections by low numbers of trypanosomes is mediated by the iNOS pathway [30] whereas a subpopulation of NKT cells down-regulate this resistance [30], we speculate that the suppressive NKT cells might be type II NKT cells [140,141] which would predominantly produce IL-13 and activate the Arg 1 pathway in macrophages that have engulfed trypanosome GPI (Fig. 3). 8 Figure 3. Minimal model: immunosuppression at primary intradermal infections by low numbers of trypanosomes. Macrophages that have engulfed filopodia of trypanosomes [27] or whole killed trypanosomes will process trypanosome antigens and present them at their cell surface. GPI of the membrane VSG (mVSG) will be presented via CD1d to NKT cells [30,139]. We argue that the NKT cells are predominantly type II NKT cells that release IL-13 (see text) which, in turn, skew the macrophages toward M2 type. Thus the antigenpresenting macrophages will predominantly be a mixed M1/M2 type (see text). MHC class II will present peptides of variant and invariant domains of soluble VSG (sVSG) as well as other invariant peptides to MHC class II-restricted T cells. The microenvironment will skew the naïve MHC class II-restricted T cells towards Tregs [30,71], presumably via TGF-β produced by macrophages. The Tregs, in turn, activate the ARG 1 pathway of macrophages by production of IL-10. We propose that many of the naïve trypanosome-specific T cells that develop into Th1 effector cells are deleted by apoptosis, due to peroxynitrite (ONOO-) produced by macrophages under conditions of shortage of L-arginine supply [121] or functionally impaired, such as by downregulation of CD3zeta [124]. We have to keep in mind that our intradermal infections were performed by syringe and needle. In natural infections, the tsetse fly injects the trypanosomes together with fly saliva. The saliva of tsetse flies [142] as well of mosquitoes [143] induce Th2 responses. The tsetse fly saliva will likely alter the microenvironment of the infection site of the skin. Thus, IL-4 produced by Th2 cells will skew APCs towards activating the Arg 1 pathway and, like the suppressor T cells, interfere with the innate resistance. TNF-α- and iNOS-producing dendritic cells (Tip-DCs) are a major population of cells in the liver of C57BL/6 mice infected with T. b. brucei [144]. The most abundant APC in the skin are Langerhans cells [145]. Presently, we have no information to what degree Langerhans cells or other dendritic cells might be involved in the resistance or suppression of resistance to intradermal infections by trypanosomes. If our hypothesis is correct that the initial activation of macrophages occurs by phagocytosis of trypanosome filopodia via iC3b/CR3 interaction, there will be a predominant induction of the iNOS 9 pathway by trypanosome GPI. There are, however, reports that iC3b/CR3 interactions lead to the sequential production of TGF-β and IL-10 and down-regulation of IL-12 by the APC, exerting an immunosuppressive effect on Th1 cells [146,147,148]. Considering the profound complement activation in humans [21], cattle [5,149], sheep [22] and mice [36] infected with African trypanosomes, there might be another, yet to be identified, circuit of immunosuppression mediated by interactions with complement components C3b and/or iC3b [150]. Immunosuppression in secondary intradermal infections: Primary intradermal infections with low numbers of T. brucei or T. congolense, associated with innate resistance, fail to induce long-term immunity. Instead, primary intradermal infections with low numbers of trypanosomes result in enhanced susceptibility to intradermal challenges [30]. Even more surprisingly, intradermal injection with a single dose of killed T. brucei or T. congolense can induce a suppressive immune response as demonstrated by enhanced susceptibility to intradermal challenge by T. brucei or T. congolense [30]. Moreover, we found that intradermal injection with a lysate of T. congolense equivalent to 106 trypanosomes induces a significantly higher susceptibility to challenge than a lysate equivalent to 103 trypanosomes [30]. Thus, there is a dose-dependent effect. We presently have no information on the immune response that leads to enhanced susceptibility at the time of challenge. In this respect, it is worth commenting on an unexpected observation. We have characterized a protein of T. congolense as a homologue of the major surface protease, gp63 of Leishmania major [151], which we called Tco-MSP-D [64]. We have cloned and purified a protein encoding the amino-terminal domain of Tco-MSP-D. We detect Tco-MSP-D in the serum of T. congolense-infected mice. Mice immunized with the amino-terminal domain of Tco-MSP-D generate a persisting IgG1 antibody response. Surprisingly, such immunized mice show an enhanced susceptibility to an intradermal challenge with T. congolense, suggesting that antibodies to Tco-MSP-D might enhance a yet unknown virulence mechanism of Tco-MSP-D. We speculate that Tco-MSP-D might, like gp63 [151], be an enzyme that affects the complement cascade, cleaving C3b to iC3b and thus preventing the amplification of the terminal complement pathway that is required for complementmediated lysis of target cells. We presently have, however, not investigated whether antibodies to TcoMSP-D are a) induced at primary intradermal infections with low numbers of T. congolense or b) might be present at the time of challenge. What strategy should be pursued to produce an effective vaccine? As discussed above, we suggest a trypanosome-specific Th1 imprint is required for resistance against trypanosome infections (Fig. 4). We propose that inhibiting the arginase pathway [44] and adequately supplying L-arginine [121], combined with intradermal immunization with low numbers of trypanosomes, will ameliorate or abolish the immunosuppressive environment, lead to induction of a trypanosome-specific Th1 imprint and, in turn, enhance innate resistance. Intradermal injections of a lysate of T. congolense, clone TC13 equivalent to 1000 parasites or injections of a lysate of 100 T. brucei, strain Whatat 1.1 induced enhanced susceptibility to intradermal challenge with T. congolense, clone TC14 or T. brucei, strain 10-26, respectively [30]. These results clearly point to important conclusions: 1) Antigenic variation does not come into play in resistance to intradermal infections by low number of parasites. 2) For a vaccine to be successful, the induction of immunosuppression has to be prevented. Route of immunization: Since in natural infections, the host is first exposed to trypanosome antigens in the skin, immunizations should be carried out intradermally. 10 Interference with immunosuppressive environment. The strategy should be to suppress the arginase pathway and prevent a shortage of L-arginine, and to enhance the iNOS pathway in such a way that it does not inhibit, but enhances the induction of Th1 cells. a) Incorporation of anti-trypanosomal drugs: Difluoromethyl ornithine (DFMO), an inhibitor of the ornithine decarboxylase, a key enzyme in the arginase pathway, is now used in the treatment of human sleeping sickness [60]. It might be the drug of first choice to be incorporated at optimal concentration in the vaccine. Other potential candidates might be suramin, also being used for treatment of sleeping sickness [60] and berenil, effective for treating cattle infected with T. congolense [152]. b) Arginase inhibitors: Nω-hydroxy-nor-L-arginine (norNOHA) is an inhibitor of arginase [127]. When macrophages of BALB/c mice, which had been infected with T. b. brucei, were co-cultured with T. b. brucei, the incorporation of norNOHA increased NO synthesis of the macrophages and cytotoxicity for co-cultured trypanosomes [127]. Thus, incorporation of arginase inhibitors in the vaccine could prevent depletion of L-arginine by arginase and enhance the iNOS pathway [121,127]. c) L-Arginine. Addition of L-arginine is expected to enhance this effect [121,122,127]. Incorporation of appropriate concentrations of anti-trypanosomal drugs or arginase inhibitors and L-arginine should not pose a logistical problem. The next proposals are less practical. Nevertheless, we propose that incorporation of the following antibodies into a vaccine might be of benefit in counteracting the immunosuppressive effects on inducing a protective Th1 response. d) Anti-cytokine/cytokine receptor antibodies: The incorporation of anti-IL-13, anti-IL-10R, anti-IL4Rα and/or anti-TGF-β antibodies would, in different ways, skew the microenvironment towards a Th1 response. By blocking IL-13, IL-10R and/or IL4Rα, the induction of the arginase pathway in antigen-presenting cells would be inhibited [121,140]. Neutralizing TGF-β would inhibit the induction of Tregs. e) Anti-iC3b antibodies, immunoconglutinin: As discussed above, complement factor iC3b has been found to mediate inhibition of induction of Th1 cell responses [146,147,148]. Rabbits infected with T. b. brucei have been found to have high titers of immunoconglutinin [153]. Antibodies to iC3b (immunoconglutinin) [154], that block the function of iC3b, might reduce the inhibition of induction of Th1 cell responses. Such antibodies, however, are not readily available. Dose: The emphasis has to be on a low dose of antigen. One has to prevent hyperactivation of macrophages. Our quantitative data on injections of trypanosome lysates indicate that fewer trypanosomes induce less immunosuppression [30]. In experimental Leishmania major infections, susceptible BALB/c mice infected with a small number of parasites could be made resistant to a larger, normally pathogenic, challenge [155]. Bretscher et al. [156] convincingly argue that immunizations with low doses of non-pathogenic antigens or pathogens lead to a Th1 imprint, rather than a Th2 imprint. Since we aim at inducing a Th1 imprint to obtain a protective immune response against African trypanosomes, more antigen is not better, less is best. Choice of trypanosomal material: For mice to be immunized against T. brucei or T. congolense, an optimal dose might be a lysate equivalent to 100-500 organisms of the respective parasites. Final comment: Our proposal to use a vaccination procedure that enhances Th1 cell differentiation appears to run counter to the observation that Th1 cell/IFN-γ-induced NO mediates profound immunopathology and immunosuppression in African trypanosomiasis [49]. NO, however, is a doubleedged sword. Our reasoning is based on the observation that high concentrations of NO are immunosuppressive whereas low concentrations of NO enhance Th1 cell differentiation [157]. 11 Figure 4. Minimal model of envisioned protective immune response to vaccination. We propose that intradermal immunization with a low dose of antigens of the whole parasite is necessary but not sufficient. We suggest that the immunization has to be accompanied by a treatment that inhibits the arginase pathway of antigen-presenting cells. We anticipate that such vaccination procedure modestly enhances the iNOS pathway of antigen-presenting cells to induce a Th1 imprint, i.e., memory Th1 cells specific for relevant trypanosomal antigens Does the proposed strategy have relevance to development of vaccines against other infections? Malaria. Malaria is associated with immunosuppression [158,159]. Presently, there are still no effective vaccines against malaria, in spite of vast scientific efforts. Guilbride et al. [160,161] published an extensive investigation into immunization studies against malaria, covering a period from 1965 to 2010. The authors came to the conclusion that Plasmodium sporozoites induce a skin-stage–initiated immunosuppression inhibiting vaccine function. Intradermal vaccination against rabies has been shown to be as safe and immunogenic as intramuscular vaccination [162]. Thus, there does not appear to be an intrinsic property of the skin that necessarily leads to immunosuppression when a pathogen enters. We propose that pathogenic Plasmodia and Trypanosoma share parameters that initiate immunosuppression upon intradermal infections, but that these parameters are absent in rabies virus. Thus, as in African trypanosomiases, the challenge is to overcome the early induced immunosuppression to obtain an early Th1 imprint that leads to a protective immune memory. Leishmaniases. Visceral leishmaniasis caused by L. donovanni is associated with antigenspecific immunosuppression during acute disease [163]. Excessive increase of arginase is observed in macrophages of non-healing lesions of cutaneous leishmaniasis caused by L. major and has been found to be the cause for local suppression of Th1 cell responses. The local depletion of L-arginine impairs the T cells within the skin lesion to proliferate and to produce IFN-γ [122]. As in intradermal infections with African trypanosomes, intradermal injections of killed L. major enhance susceptibility to secondary infections [164]. Again, we see a great similarity between African trypanosomiases and leishmaniases as to the early induction of suppression of Th1 responses, preventing the development of 12 a sound Th1 memory. We contend that a vaccine strategy similar to the one we have proposed for African trypanosomiases might be effective. Summary There is the general belief that success in producing vaccines against African trypanosomiases is unlikely because of the almost unlimited capacity for antigenic variation of African trypanosomes. This conclusion, however, is based on the immunological knowledge of the blood stage of infection by African trypanosomes. We recently found that intradermal infections with low numbers of trypanosomes is controlled by innate immunity and that this innate immunity is, in fact, compromised by suppressive adaptive immune responses. On the basis of these findings, we propose a vaccine strategy that aims at a) preventing the early induction of suppression of Th1 responses by inhibiting the arginase pathway, but enhancing the iNOS pathway of antigen-presenting cells and b) using the optimally lowest dose of antigens of the whole parasite to induce a Th1 imprint (Fig. 4). We suggest that similar approaches might be successful in producing vaccines against other pathogenic protozoa that manipulate the immune system. Key Papers in the Field • Wei G, Bull H, Zhou X, Tabel H (2011) Intradermal infections of mice by low numbers of African trypanosomes are controlled by innate resistance but enhance susceptibility to reinfection. J Infect Dis 203: 418-429 • Roelants GE, Pinder M (1984) Immunobiology of African trypanosomiasis. Contemp Top Immunobiol 12: 225-274 • Duleu S, Vincendeau P, Courtois P, Semballa S, Lagroye I, et al. (2004) Mouse strain susceptibility to trypanosome infection: an arginase-dependent effect. J Immunol 172: 6298-6303 • Bronte V, Zanovello P (2005) Regulation of immune responses by L-arginine metabolism. Nat Rev Immunol 5: 641-654 • Guilbride DL, Gawlinski P, Guilbride PD (2010) Why functional pre-erythrocytic and bloodstage malaria vaccines fail: a meta-analysis of fully protective immunizations and novel immunological model. PLoS One 5: e10685 Acknowledgments The authors are grateful to Juliane Deubner who drew the diagrams of the presented figures. We thank John Allen and Vikram Misra for reading the first draft of the manuscript and for providing constructive criticism. 13 References 1. Mulligan HW, Potts WH, editors (1970) The African Trypanosomiases. New York: WileyINTERSCIENCES, a Division of John Wiley & Sons, Inc. 2. Venugopal R (2010) Sleeping sickness makes a deadly comeback. Medecins Sans Frontieres Canada Magazine -Dispatches 12: 12-14. 3. Welburn SC, Coleman PG, Maudlin I, Fevre EM, Odiit M, et al. (2006) Crisis, what crisis? Control of Rhodesian sleeping sickness. Trends Parasitol 22: 123-128. 4. Maxie MG, Losos GJ, Tabel H (1979) Experimental bovine trypanosomiasis (Trypanosoma vivax and T. congolense). I. Sumptomatology and clinical pathology. Tropenmed Parasitol 30: 274282. 5. Tabel H, Losos GJ, Maxie MG (1980) Experimental bovine trypanosomiasis (Trypanosoma vivax and T. congolense). II. Serum levels of total protein, albumin, hemolytic complement, and complement component C3. Tropenmed Parasitol 31: 99-104. 6. Emery DL, Moloo SK (1980) The sequential cellular changes in the local skin reaction produced in goats by Glossina morsitans morsitans infected with Trypanosoma (Trypanozoon) brucei. Acta Trop 37: 137-149. 7. Barry JD, Emergy DL (1984) Parasite development and host responses during the establishment of Trypanosoma brucei infection transmitted by tsetse fly. Parasitology 88 ( Pt 1): 67-84. 8. Gray AR, Luckins AG (1980) The initial stage of infection with cyclically-transmitted Trypanosoma congolense in rabbits, calves and sheep. J Comp Pathol 90: 499-512. 9. Barry JD, McCulloch R (2001) Antigenic variation in trypanosomes: enhanced phenotypic variation in a eukaryotic parasite. Adv Parasitol 49: 1-70. 10. Borst P, Rudenko G, Blundell PA, van Leeuwen F, Cross MA, et al. (1997) Mechanisms of antigenic variation in African trypanosomes. Behring Inst Mitt 18: 1-15. 11. Cross GA (1990) Cellular and genetic aspects of antigenic variation in trypanosomes. Annu Rev Immunol 8: 83-110. 12. Campbell GH, Esser KM, Phillips SM (1978) Trypanosoma rhodesiense infection in congenitally athymic (nude) mice. Infect Immun 20: 714-720. 13. Clarkson MJ, Cullingham,T.J. (1975) Immunoglobulin in mice infected with trypanosomes. Trans Roy Soc Trop Med Hyg 69. 14. Askonas BA, Corsini AC, Clayton CE, Ogilvie BM (1979) Functional depletion of T- and Bmemory cells and other lymphoid cell subpopulations-during trypanosomiasis. Immunology 36: 313-321. 15. Pinder M, Chassin P, Fumoux F (1986) Mechanisms of self-cure from Trypanosoma congolense infection in mice. J Immunol 136: 1427-1434. 16. Reinitz DM, Mansfield JM (1990) T-cell-independent and T-cell-dependent B-cell responses to exposed variant surface glycoprotein epitopes in trypanosome-infected mice. Infect Immun 58: 2337-2342. 17. Roelants GE, Pinder M (1984) Immunobiology of African trypanosomiasis. Contemp Top Immunobiol 12: 225-274. 18. Diffley P (1983) Trypanosomal surface coat variant antigen causes polyclonal lymphocyte activation. J Immunol 131: 1983-1986. 19. Hudson KM, Byner C, Freeman J, Terry RJ (1976) Immunodepression, high IgM levels and evasion of the immune response in murine trypanosomiasis. Nature 264: 256-258. 14 20. Oka M, Yabu Y, Ito Y, Takayanagi T (1988) Polyclonal B-cell stimulative and immunosuppressive activities at different developmental stages of Trypanosoma gambiense. Microbiol Immunol 32: 1175-1177. 21. Greenwood BM, Whittle HC (1976) Complement activation in patients with Gambian sleeping sickness. Clin Exp Immunol 24: 133-138. 22. Malu MN, Tabel H (1986) The alternative pathway of complement in sheep during the course of infection with Trypanosoma congolense and after Berenil treatment. Parasite Immunol 8: 217229. 23. Flemmings B, Diggs C (1978) Antibody-dependent cytotoxicity against Trypanosoma rhodesiense mediated through an alternative complement pathway. Infect Immun 19: 928-933. 24. Liu EW, Otesile EB, Tabel H (1993) Immune lysis of Trypanosoma congolense: generation of a soluble covalent complex of variant surface glycoprotein and bovine complement component C3b. Vet Immunol Immunopathol 38: 169-181. 25. Greenblatt HC, Diggs CL, Aikawa M (1983) Antibody-dependent phagocytosis of Trypanosoma rhodesiense by murine macrophages. Am J Trop Med Hyg 32: 34-45. 26. Pan W, Ogunremi O, Wei G, Shi M, Tabel H (2006) CR3 (CD11b/CD18) is the major macrophage receptor for IgM antibody-mediated phagocytosis of African trypanosomes: diverse effect on subsequent synthesis of tumor necrosis factor alpha and nitric oxide. Microbes Infect 8: 12091218. 27. Shakibaei M, Frevert U (1992) Cell surface interactions between Trypanosoma congolense and macrophages during phagocytosis in vitro. J Protozool 39: 224-235. 28. Kaushik RS, Uzonna JE, Gordon JR, Tabel H (1999) Innate resistance to Trypanosoma congolense infections: differential production of nitric oxide by macrophages from susceptible BALB/c and resistant C57Bl/6 mice. Exp Parasitol 92: 131-143. 29. Vincendeau P, Daulouede S, Veyret B, Darde ML, Bouteille B, et al. (1992) Nitric oxide-mediated cytostatic activity on Trypanosoma brucei gambiense and Trypanosoma brucei brucei. Exp Parasitol 75: 353-360. 30. Wei G, Bull H, Zhou X, Tabel H (2011) Intradermal infections of mice by low numbers of african trypanosomes are controlled by innate resistance but enhance susceptibility to reinfection. J Infect Dis 203: 418-429. 31. Campbell GH, Esser KM, Weinbaum FI (1977) Trypanosoma rhodesiense infection in B-celldeficient mice. Infect Immun 18: 434-438. 32. Campbell GH, Phillips SM (1976) Adoptive transfer of variant-specific resistance to Trypanosoma rhodesiense with B lymphocytes and serum. Infect Immun 14: 1144-1150. 33. Magez S, Radwanska M, Drennan M, Fick L, Baral TN, et al. (2006) Interferon-gamma and nitric oxide in combination with antibodies are key protective host immune factors during trypanosoma congolense Tc13 Infections. J Infect Dis 193: 1575-1583. 34. Magez S, Schwegmann A, Atkinson R, Claes F, Drennan M, et al. (2008) The role of B-cells and IgM antibodies in parasitemia, anemia, and VSG switching in Trypanosoma brucei-infected mice. PLoS Pathog 4: e1000122. 35. Jones JF, Hancock GE (1983) Trypanosomiasis in mice with naturally occurring immunodeficiencies. Infect Immun 42: 848-851. 36. Otesile EB, Lee M, Tabel H (1991) Plasma levels of proteins of the alternative complement pathway in inbred mice that differ in resistance to Trypanosoma congolense infections. J Parasitol 77: 958-964. 15 37. Mansfield JM, Levine RF, Dempsey WL, Wellhausen SR, Hansen CT (1981) Lymphocyte function in experimental African trypanosomiasis. IV. Immunosuppression and suppressor cells in the athymic nu/nu mouse. Cell Immunol 63: 210-215. 38. Seed JR (1977) The role of immunoglobulins in immunity to Trypanosoma brucei gambiense. Int J Parasitol 7: 55-60. 39. Shi M, Wei G, Pan W, Tabel H (2004) Trypanosoma congolense infections: antibody-mediated phagocytosis by Kupffer cells. J Leukoc Biol 76: 399-405. 40. DeGee AL, Mansfield JM (1984) Genetics of resistance to the African trypanosomes. IV. Resistance of radiation chimeras to Trypanosoma rhodesiense infection. Cell Immunol 87: 8591. 41. Uzonna JE, Kaushik RS, Gordon JR, Tabel H (1999) Cytokines and antibody responses during Trypanosoma congolense infections in two inbred mouse strains that differ in resistance. Parasite Immunol 21: 57-71. 42. Hertz CJ, Filutowicz H, Mansfield JM (1998) Resistance to the African trypanosomes is IFNgamma dependent. J Immunol 161: 6775-6783. 43. Mansfield JM, Paulnock DM (2005) Regulation of innate and acquired immunity in African trypanosomiasis. Parasite Immunol 27: 361-371. 44. Gobert AP, Daulouede S, Lepoivre M, Boucher JL, Bouteille B, et al. (2000) L-Arginine availability modulates local nitric oxide production and parasite killing in experimental trypanosomiasis. Infect Immun 68: 4653-4657. 45. Baetselier PD, Namangala B, Noel W, Brys L, Pays E, et al. (2001) Alternative versus classical macrophage activation during experimental African trypanosomosis. Int J Parasitol 31: 575587. 46. Drennan MB, Stijlemans B, Van den Abbeele J, Quesniaux VJ, Barkhuizen M, et al. (2005) The induction of a type 1 immune response following a Trypanosoma brucei infection is MyD88 dependent. J Immunol 175: 2501-2509. 47. Shi M, Pan W, Tabel H (2003) Experimental African trypanosomiasis: IFN-gamma mediates early mortality. Eur J Immunol 33: 108-118. 48. Shi M, Wei G, Pan W, Tabel H (2006) Experimental African trypanosomiasis: a subset of pathogenic, IFN-gamma-producing, MHC class II-restricted CD4+ T cells mediates early mortality in highly susceptible mice. J Immunol 176: 1724-1732. 49. Tabel H, Wei G, Shi M (2008) T cells and immunopathogenesis of experimental African trypanosomiasis. Immunol Rev 225: 128-139. 50. Gasbarre LC, Hug K, Louis J (1981) Murine T lymphocyte specificity for African trypanosomes. II. Suppression of the T lymphocyte proliferative response to Trypanosoma brucei by systemic trypanosome infection. Clin Exp Immunol 45: 165-172. 51. Sacks DL, Askonas BA (1980) Trypanosome-induced suppression of anti-parasite responses during experimental African trypanosomiasis. Eur J Immunol 10: 971-974. 52. Kemp SJ, Iraqi F, Darvasi A, Soller M, Teale AJ (1997) Localization of genes controlling resistance to trypanosomiasis in mice. Nat Genet 16: 194-196. 53. Levine RF, Mansfield JM (1981) Genetics of resistance to African trypanosomes: role of the H-2 locus in determining resistance to infection with Trypanosoma rhodesiense. Infect Immun 34: 513-518. 54. Levine RF, Mansfield JM (1984) Genetics of resistance to the African trypanosomes. III. Variantspecific antibody responses of H-2-compatible resistant and susceptible mice. J Immunol 133: 1564-1569. 16 55. Sacks DL, Selkirk M, Ogilvie BM, Askonas BA (1980) Intrinsic immunosuppressive activity of different trypanosome strains varies with parasite virulence. Nature 283: 476-478. 56. Tabel H, Kaushik RS, Uzonna JE (2000) Susceptibility and resistance to Trypanosoma congolense infections. Microbes Infect 2: 1619-1629. 57. Ogunremi O, Tabel H (1995) Genetics of resistance to Trypanosoma congolense in inbred mice: efficiency of apparent clearance of parasites correlates with long-term survival. J Parasitol 81: 876-881. 58. Ferguson MA (1999) The structure, biosynthesis and functions of glycosylphosphatidylinositol anchors, and the contributions of trypanosome research. J Cell Sci 112: 2799-2809. 59. Ferguson MA, Williams AF (1988) Cell-surface anchoring of proteins via glycosylphosphatidylinositol structures. Annu Rev Biochem 57: 285-320. 60. Brun R, Blum J, Chappuis F, Burri C (2010) Human African trypanosomiasis. Lancet 375: 148159. 61. Gray AR (1976) Immunological research and the problem of immunization against African trypanosomiasis. Trans R Soc Trop Med Hyg 70: 119-121. 62. Murray M, Barry JD, Morrison WI, Williams RO, Hirumi H, et al. (1979) A review of the prospects for vaccination in African trypanosomiasis- Part I. World Animal Review 32: 9-13. 63. Stuart K, Brun R, Croft S, Fairlamb A, Gurtler RE, et al. (2008) Kinetoplastids: related protozoan pathogens, different diseases. J Clin Invest 118: 1301-1310. 64. Marcoux V, Wei G, Tabel H, Bull HJ (2010) Characterization of Major Surface Protease Homologues of Trypanosoma congolense. J Biomed Biotechnol 2010: 418157. 65. Askonas BA (1985) Macrophages as mediators of immunosuppression in murine African trypanosomiasis. Curr Top Microbiol Immunol 117: 119-127. 66. Murray M, Morrison WI, Whitelaw DD (1982) Host susceptibility to African trypanosomiasis: trypanotolerance. Adv Parasitol 21: 1-68. 67. Paulnock DM, Freeman BE, Mansfield JM (2010) Modulation of innate immunity by African trypanosomes. Parasitology 137: 2051-2063. 68. Sileghem M, Flynn NJ, Darji A, De Baetselier P, Naessens J (1994) African trypanosomiasis. In: Kierszenbaum F, editor. Parasite Infections and the Immune System. New York: Academic Press. pp. 1-51. 69. Beschin A, Brys L, Magez S, Radwanska M, De Baetselier P (1998) Trypanosoma brucei infection elicits nitric oxide-dependent and nitric oxide-independent suppressive mechanisms. J Leukoc Biol 63: 429-439. 70. Dagenais TR, Freeman BE, Demick KP, Paulnock DM, Mansfield JM (2009) Processing and presentation of variant surface glycoprotein molecules to T cells in African trypanosomiasis. J Immunol 183: 3344-3355. 71. Wei G, Tabel H (2008) Regulatory T cells prevent control of experimental African trypanosomiasis. J Immunol 180: 2514-2521. 72. Fairbairn H, Burtt E (1946) The infectivity to man of a strain of Trypanosoma rhodesiense transmitted cyclically by Glossina morsitans through sheep and antelope: Evidence that man requires a minimum infective dose of metacyclic trypanosomes. Annals of Tropical and Medical Parasitology 40: 270-313. 73. Magez S, Caljon G, Tran T, Stijlemans B, Radwanska M (2010) Current status of vaccination against African trypanosomiasis. Parasitology 137: 2017-2027. 74. Goodwin LG, Green DG, Guy MW, Voller A (1972) Immunosuppression during trypanosomiasis. Br J Exp Pathol 53: 40-43. 17 75. Murray PK, Jennings FW, Murray M, Urquhart GM (1974) The nature of immunosuppression in Trypanosoma brucei infections in mice. II. The role of the T and B lymphocytes. Immunology 27: 825-840. 76. Wellhausen SR, Mansfield JM (1979) Lymphocyte function in experimental African trypanosomiasis. II. Splenic suppressor cell activity. J Immunol 122: 818-824. 77. Greenwood BM, Whittle HC, Molyneux DH (1973) Immunosuppression in Gambian trypanosomiasis. Trans R Soc Trop Med Hyg 67: 846-850. 78. Rurangirwa FR, Musoke AJ, Nantulya VM, Tabel H (1983) Immune depression in bovine trypanosomiasis: effects of acute and chronic Trypanosoma congolense and chronic Trypanosoma vivax infections on antibody response to Brucella abortus vaccine. Parasite Immunol 5: 267-276. 79. Rurangirwa FR, Tabel H, Losos G, Masiga WN, Mwambu P (1978) Immunosuppressive effect of Trypanosoma congolense and Trypanosoma vivax on the secondary immune response of cattle to Mycoplasma mycoides subsp mycoides. Res Vet Sci 25: 395-397. 80. Rurangirwa FR, Tabel H, Losos GJ, Tizard IR (1979) Suppression of antibody response to Leptospira biflexa and Brucella abortus and recovery from immunosuppression after Berenil treatment. Infect Immun 26: 822-826. 81. Whitelaw DD, Scott JM, Reid HW, Holmes PH, Jennings FW, et al. (1979) Immunosuppression in bovine trypanosomiasis: studies with louping-ill vaccine. Res Vet Sci 26: 102-107. 82. Radwanska M, Guirnalda P, De Trez C, Ryffel B, Black S, et al. (2008) Trypanosomiasis-induced B cell apoptosis results in loss of protective anti-parasite antibody responses and abolishment of vaccine-induced memory responses. PLoS Pathog 4: e1000078. 83. Borowy NK, Sternberg JM, Schreiber D, Nonnengasser C, Overath P (1990) Suppressive macrophages occurring in murine Trypanosoma brucei infection inhibit T-cell responses in vivo and in vitro. Parasite Immunol 12: 233-246. 84. Kierszenbaum F, Muthukkumar S, Beltz LA, Sztein MB (1991) Suppression by Trypanosoma brucei rhodesiense of the capacities of human T lymphocytes to express interleukin-2 receptors and proliferate after mitogenic stimulation. Infect Immun 59: 3518-3522. 85. Pearson TW, Roelants GE, Pinder M, Lundin LB, Mayor-Withey KS (1979) Immune depression in trypanosome-infected mice. III. suppressor cells. Eur J Immunol 9: 200-204. 86. Sileghem M, Darji A, Hamers R, Van de Winkel M, De Baetselier P (1989) Dual role of macrophages in the suppression of interleukin 2 production and interleukin 2 receptor expression in trypanosome-infected mice. Eur J Immunol 19: 829-835. 87. Sileghem M, Darji A, Remels L, Hamers R, De Baetselier P (1989) Different mechanisms account for the suppression of interleukin 2 production and the suppression of interleukin 2 receptor expression in Trypanosoma brucei-infected mice. Eur J Immunol 19: 119-124. 88. Sileghem M, Flynn JN (1992) Suppression of interleukin 2 secretion and interleukin 2 receptor expression during tsetse-transmitted trypanosomiasis in cattle. Eur J Immunol 22: 767-773. 89. Sternberg J, McGuigan F (1992) Nitric oxide mediates suppression of T cell responses in murine Trypanosoma brucei infection. Eur J Immunol 22: 2741-2744. 90. Uzonna JE, Kaushik RS, Gordon JR, Tabel H (1998) Experimental murine Trypanosoma congolense infections. I. Administration of anti-IFN-gamma antibodies alters trypanosomesusceptible mice to a resistant-like phenotype. J Immunol 161: 5507-5515. 91. Uzonna JE, Kaushik RS, Zhang Y, Gordon JR, Tabel H (1998) Experimental murine Trypanosoma congolense infections. II. Role of splenic adherent CD3+Thy1.2+ TCR-alpha beta- gamma delta- CD4+8- and CD3+Thy1.2+ TCR-alpha beta- gamma delta- CD4-8- cells in the 18 production of IL-4, IL-10, and IFN-gamma and in trypanosome-elicited immunosuppression. J Immunol 161: 6189-6197. 92. Morrison WI, Murray, M. and Bovell, D. L. (1981) The response of the murine lymphoid system to a chronic infection with Trypanosoma congolense. I. The spleen. Lab Invest 45: 547-557. 93. Gasbarre LC, Hug K, Louis JA (1980) Murine T lymphocyte specificity for African trypanosomes. I. Induction of a T lymphocyte-dependent proliferative response to Trypanosoma brucei. Clin Exp Immunol 41: 97-106. 94. Schleifer KW, Mansfield JM (1993) Suppressor macrophages in African trypanosomiasis inhibit T cell proliferative responses by nitric oxide and prostaglandins. J Immunol 151: 5492-5503. 95. Dagenais TR, Demick KP, Bangs JD, Forest KT, Paulnock DM, et al. (2009) T-cell responses to the trypanosome variant surface glycoprotein are not limited to hypervariable subregions. Infect Immun 77: 141-151. 96. Grosskinsky CM, Askonas BA (1981) Macrophages as primary target cells and mediators of immune dysfunction in African trypanosomiasis. Infect Immun 33: 149-155. 97. Jayawardena AN, Waksman BH (1977) Suppressor cells in experimentally trypanosomiasis. Nature 265: 539-541. 98. Mabbott NA, Sutherland IA, Sternberg JM (1995) Suppressor macrophages in Trypanosoma brucei infection: nitric oxide is related to both suppressive activity and lifespan in vivo. Parasite Immunol 17: 143-150. 99. Namangala B, Brys L, Magez S, De Baetselier P, Beschin A (2000) Trypanosoma brucei brucei infection impairs MHC class II antigen presentation capacity of macrophages. Parasite Immunol 22: 361-370. 100. Clayton CE, Sacks DL, Ogilvie BM, Askonas BA (1979) Membrane fractions of trypanosomes mimic the immunosuppressive and mitogenic effects of living parasites on the host. Parasite Immunol 1: 241-249. 101. Sacks DL, Bancroft G, Evans WH, Askonas BA (1982) Incubation of trypanosome-derived mitogenic and immunosuppressive products with peritoneal macrophages allows recovery of biological activities from soluble parasite fractions. Infect Immun 36: 160-168. 102. Magez S, Stijlemans B, Radwanska M, Pays E, Ferguson MA, et al. (1998) The glycosyl-inositolphosphate and dimyristoylglycerol moieties of the glycosylphosphatidylinositol anchor of the trypanosome variant-specific surface glycoprotein are distinct macrophage-activating factors. J Immunol 160: 1949-1956. 103. Tachado SD, Gerold P, Schwarz R, Novakovic S, McConville M, et al. (1997) Signal transduction in macrophages by glycosylphosphatidylinositols of Plasmodium, Trypanosoma, and Leishmania: activation of protein tyrosine kinases and protein kinase C by inositolglycan and diacylglycerol moieties. Proc Natl Acad Sci U S A 94: 4022-4027. 104. Tachado SD, Mazhari-Tabrizi R, Schofield L (1999) Specificity in signal transduction among glycosylphosphatidylinositols of Plasmodium falciparum, Trypanosoma brucei, Trypanosoma cruzi and Leishmania spp. Parasite Immunol 21: 609-617. 105. Tachado SD, Schofield L (1994) Glycosylphosphatidylinositol toxin of Trypanosoma brucei regulates IL-1 alpha and TNF-alpha expression in macrophages by protein tyrosine kinase mediated signal transduction. Biochem Biophys Res Commun 205: 984-991. 106. Schofield L, Hackett F (1993) Signal transduction in host cells by a glycosylphosphatidylinositol toxin of malaria parasites. J Exp Med 177: 145-153. 107. Tachado SD, Gerold P, McConville MJ, Baldwin T, Quilici D, et al. (1996) Glycosylphosphatidylinositol toxin of Plasmodium induces nitric oxide synthase expression in 19 macrophages and vascular endothelial cells by a protein tyrosine kinase-dependent and protein kinase C-dependent signaling pathway. J Immunol 156: 1897-1907. 108. Kaushik RS, Uzonna JE, Radzioch D, Gordon JR, Tabel H (1999) Innate resistance to experimental Trypanosoma congolense infection: differences in IL-10 synthesis by macrophage cell lines from resistant and susceptible inbred mice. Parasite Immunol 21: 119-131. 109. Kaushik RS, Uzonna JE, Zhang Y, Gordon JR, Tabel H (2000) Innate resistance to experimental African trypanosomiasis: differences in cytokine (TNF-alpha, IL-6, IL-10 and IL-12) production by bone marrow-derived macrophages from resistant and susceptible mice. Cytokine 12: 1024-1034. 110. Shi M, Wei G, Pan W, Tabel H (2005) Impaired Kupffer cells in highly susceptible mice infected with Trypanosoma congolense. Infect Immun 73: 8393-8396. 111. Namangala B, de Baetselier P, Brijs L, Stijlemans B, Noel W, et al. (2000) Attenuation of Trypanosoma brucei is associated with reduced immunosuppression and concomitant production of Th2 lymphokines. J Infect Dis 181: 1110-1120. 112. Mabbott NA, Coulson PS, Smythies LE, Wilson RA, Sternberg JM (1998) African trypanosome infections in mice that lack the interferon-gamma receptor gene: nitric oxide-dependent and independent suppression of T-cell proliferative responses and the development of anaemia. Immunology 94: 476-480. 113. Schleifer KW, Filutowicz H, Schopf LR, Mansfield JM (1993) Characterization of T helper cell responses to the trypanosome variant surface glycoprotein. J Immunol 150: 2910-2919. 114. Sternberg MJ, Mabbott NA (1996) Nitric oxide-mediated suppression of T cell responses during Trypanosoma brucei infection: soluble trypanosome products and interferon-gamma are synergistic inducers of nitric oxide synthase. Eur J Immunol 26: 539-543. 115. Bancroft GJ, Sutton CJ, Morris AG, Askonas BA (1983) Production of interferons during experimental African trypanosomiasis. Clin Exp Immunol 52: 135-143. 116. Darji A, Sileghem M, Heremans H, Brys L, De Baetselier P (1993) Inhibition of T-cell responsiveness during experimental infections with Trypanosoma brucei: active involvement of endogenous gamma interferon. Infect Immun 61: 3098-3102. 117. Sileghem M, Hamers R, De Baetselier P (1987) Experimental Trypanosoma brucei infections selectively suppress both interleukin 2 production and interleukin 2 receptor expression. Eur J Immunol 17: 1417-1421. 118. Darji A, Beschin A, Sileghem M, Heremans H, Brys L, et al. (1996) In vitro simulation of immunosuppression caused by Trypanosoma brucei: active involvement of gamma interferon and tumor necrosis factor in the pathway of suppression. Infect Immun 64: 1937-1943. 119. Laskin DL, Sunil VR, Gardner CR, Laskin JD (2011) Macrophages and tissue injury: agents of defense or destruction? Annu Rev Pharmacol Toxicol 51: 267-288. 120. Sica A, Bronte V (2007) Altered macrophage differentiation and immune dysfunction in tumor development. J Clin Invest 117: 1155-1166. 121. Bronte V, Zanovello P (2005) Regulation of immune responses by L-arginine metabolism. Nat Rev Immunol 5: 641-654. 122. Modolell M, Choi BS, Ryan RO, Hancock M, Titus RG, et al. (2009) Local suppression of T cell responses by arginase-induced L-arginine depletion in nonhealing leishmaniasis. PLoS Negl Trop Dis 3: e480. 123. Sinha P, Clements VK, Ostrand-Rosenberg S (2005) Interleukin-13-regulated M2 macrophages in combination with myeloid suppressor cells block immune surveillance against metastasis. Cancer Res 65: 11743-11751. 20 124. Zea AH, Rodriguez PC, Culotta KS, Hernandez CP, DeSalvo J, et al. (2004) L-Arginine modulates CD3zeta expression and T cell function in activated human T lymphocytes. Cell Immunol 232: 21-31. 125. Huang B, Pan PY, Li Q, Sato AI, Levy DE, et al. (2006) Gr-1+CD115+ immature myeloid suppressor cells mediate the development of tumor-induced T regulatory cells and T-cell anergy in tumor-bearing host. Cancer Res 66: 1123-1131. 126. Greenblatt HC, Diggs CL, Rosenstreich DL (1984) Trypanosoma rhodesiense: analysis of the genetic control of resistance among mice. Infect Immun 44: 107-111. 127. Duleu S, Vincendeau P, Courtois P, Semballa S, Lagroye I, et al. (2004) Mouse strain susceptibility to trypanosome infection: an arginase-dependent effect. J Immunol 172: 62986303. 128. Pepper M, Jenkins MK (2011) Origins of CD4(+) effector and central memory T cells. Nat Immunol 12: 467-471. 129. Pepper M, Linehan JL, Pagan AJ, Zell T, Dileepan T, et al. (2010) Different routes of bacterial infection induce long-lived TH1 memory cells and short-lived TH17 cells. Nat Immunol 11: 8389. 130. Devine DV, Falk RJ, Balber AE (1986) Restriction of the alternative pathway of human complement by intact Trypanosoma brucei subsp. gambiense. Infect Immun 52: 223-229. 131. Diffley P, Honigberg BM (1978) Immunologic analysis of host plasma proteins on bloodstream forms of African pathogenic trypanosomes. II. Identification and quantitation of surface-bound albumin, nonspecific IgG, and complement on Trypanosoma congolense. J Parasitol 64: 674681. 132. Macadam RF, Herbert WJ (1970) Fine structural demonstration of cytoplasmic protrusions (filopodia) in Trypanosomes. Exp Parasitol 27: 1-8. 133. Wright KA, Lumsden WH, Hales H (1970) The formation of filopodium-like processes by Trypanosoma (Trypanozoon) brucei. J Cell Sci 6: 285-297. 134. Frevert U, Reinwald E (1990) Trypanosoma congolense bloodstream forms evade complement lysis in vitro by shedding of immune complexes. Eur J Cell Biol 52: 264-269. 135. MacMicking J, Xie QW, Nathan C (1997) Nitric oxide and macrophage function. Annu Rev Immunol 15: 323-350. 136. Gobert AP, Semballa S, Daulouede S, Lesthelle S, Taxile M, et al. (1998) Murine macrophages use oxygen- and nitric oxide-dependent mechanisms to synthesize S-nitroso-albumin and to kill extracellular trypanosomes. Infect Immun 66: 4068-4072. 137. Mnaimneh S, Geffard M, Veyret B, Vincendeau P (1997) Albumin nitrosylated by activated macrophages possesses antiparasitic effects neutralized by anti-NO-acetylated-cysteine antibodies. J Immunol 158: 308-314. 138. Godfrey DI, Berzins SP (2007) Control points in NKT-cell development. Nat Rev Immunol 7: 505-518. 139. Schofield L, McConville MJ, Hansen D, Campbell AS, Fraser-Reid B, et al. (1999) CD1drestricted immunoglobulin G formation to GPI-anchored antigens mediated by NKT cells. Science 283: 225-229. 140. Berzofsky JA, Terabe M (2008) A novel immunoregulatory axis of NKT cell subsets regulating tumor immunity. Cancer Immunol Immunother 57: 1679-1683. 141. Ambrosino E, Terabe M, Halder RC, Peng J, Takaku S, et al. (2007) Cross-regulation between type I and type II NKT cells in regulating tumor immunity: a new immunoregulatory axis. J Immunol 179: 5126-5136. 21 142. Caljon G, Van Den Abbeele J, Sternberg JM, Coosemans M, De Baetselier P, et al. (2006) Tsetse fly saliva biases the immune response to Th2 and induces anti-vector antibodies that are a useful tool for exposure assessment. Int J Parasitol 36: 1025-1035. 143. Schneider BS, Soong L, Zeidner NS, Higgs S (2004) Aedes aegypti salivary gland extracts modulate anti-viral and TH1/TH2 cytokine responses to sindbis virus infection. Viral Immunol 17: 565-573. 144. Bosschaerts T, Guilliams M, Stijlemans B, Morias Y, Engel D, et al. (2010) Tip-DC development during parasitic infection is regulated by IL-10 and requires CCL2/CCR2, IFN-gamma and MyD88 signaling. PLoS Pathog 6: e1001045. 145. Merad M, Ginhoux F, Collin M (2008) Origin, homeostasis and function of Langerhans cells and other langerin-expressing dendritic cells. Nat Rev Immunol 8: 935-947. 146. Hammerberg C, Katiyar SK, Carroll MC, Cooper KD (1998) Activated complement component 3 (C3) is required for ultraviolet induction of immunosuppression and antigenic tolerance. J Exp Med 187: 1133-1138. 147. Sohn JH, Bora PS, Suk HJ, Molina H, Kaplan HJ, et al. (2003) Tolerance is dependent on complement C3 fragment iC3b binding to antigen-presenting cells. Nat Med 9: 206-212. 148. Yoshida Y, Kang K, Berger M, Chen G, Gilliam AC, et al. (1998) Monocyte induction of IL-10 and down-regulation of IL-12 by iC3b deposited in ultraviolet-exposed human skin. J Immunol 161: 5873-5879. 149. Tabel H (1982) Activation of the alternative pathway of bovine complement by Trypanosoma congolense. Parasite Immunol 4: 329-335. 150. Kemper C, Atkinson JP (2007) T-cell regulation: with complements from innate immunity. Nat Rev Immunol 7: 9-18. 151. Brittingham A, Morrison CJ, McMaster WR, McGwire BS, Chang KP, et al. (1995) Role of the Leishmania surface protease gp63 in complement fixation, cell adhesion, and resistance to complement-mediated lysis. J Immunol 155: 3102-3111. 152. Rurangirwa FR, Tabel H, Losos G, Tizard IR (1980) Hemolytic complement and serum C3 levels in Zebu cattle infected with Trypanosoma congolense and Trypanosoma vivax and the effect of trypanocidal treatment. Infect Immun 27: 832-836. 153. Coombs RRA, Coombs AM, Ingram DG (1961) The serology of conglutination and its relation to disease. Springfield, Illinois, U.S.A.: Charles C. Thomas. 154. Nilsson B, Ekdahl KN, Svarvare M, Bjelle A, Nilsson UR (1990) Purification and characterization of IgG immunoconglutinins from patients with systemic lupus erythematosus: implications for a regulatory function. Clin Exp Immunol 82: 262-267. 155. Bretscher PA, Wei G, Menon JN, Bielefeldt-Ohmann H (1992) Establishment of stable, cellmediated immunity that makes "susceptible" mice resistant to Leishmania major. Science 257: 539-542. 156. Bretscher PA, Ismail N, Menon JN, Power CA, Uzonna J, et al. (2001) Vaccination against and treatment of tuberculosis, the leishmaniases and AIDS: perspectives from basic immunology and immunity to chronic intracellular infections. Cellular and Molecular Life Sciences 58: 001018. 157. Niedbala W, Wei XQ, Campbell C, Thomson D, Komai-Koma M, et al. (2002) Nitric oxide preferentially induces type 1 T cell differentiation by selectively up-regulating IL-12 receptor beta 2 expression via cGMP. Proc Natl Acad Sci U S A 99: 16186-16191. 22 158. Butler NS, Moebius J, Pewe LL, Traore B, Doumbo OK, et al. (2012) Therapeutic blockade of PD-L1 and LAG-3 rapidly clears established blood-stage Plasmodium infection. Nat Immunol 13: 188-195. 159. Greenwood BM, Bradley-Moore AM, Bryceson AD, Palit A (1972) Immunosuppression in children with malaria. Lancet 1: 169-172. 160. Guilbride DL, Gawlinski P, Guilbride PD (2010) Why functional pre-erythrocytic and bloodstage malaria vaccines fail: a meta-analysis of fully protective immunizations and novel immunological model. PLoS One 5: e10685. 161. Guilbride DL, Guilbride PD, Gawlinski P (2012) Malaria's deadly secret: a skin stage. Trends Parasitol. 162. Anonymous (2010) Rabies. http://wwwwhoint/immunization/topics/rabies/en/indexhtml. 163. Carvalho EM, Bacellar O, Barral A, Badaro R, Johnson WD, Jr. (1989) Antigen-specific immunosuppression in visceral leishmaniasis is cell mediated. J Clin Invest 83: 860-864. 164. Okwor I, Liu D, Beverley SM, Uzonna JE (2009) Inoculation of killed Leishmania major into immune mice rapidly disrupts immunity to a secondary challenge via IL-10-mediated process. Proc Natl Acad Sci U S A 106: 13951-13956. 23