Altered Brain Activity in Women Recovered from Challenge: A Pilot Study
advertisement

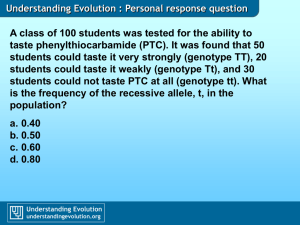
BRIEF REPORT Altered Brain Activity in Women Recovered from Bulimic-Type Eating Disorders after a Glucose Challenge: A Pilot Study Guido K. Frank, MD1,2 Angela Wagner, MD1 Sarah Achenbach, BSc1 Claire McConaha, BSN1 Kellie Skovira, BA1 Howard Aizenstein, MD1 Cameron S. Carter, MD3 Walter H. Kaye, MD1* ABSTRACT Objective: It is not known whether individuals with bulimic-type eating disorders have a dysregulation of brain pathways that modulate appetite. Taste plays a role in the regulation of appetite and the purpose of the current study was to determine whether bulimic women have alterations in the physiologic response to the blind administration of glucose. Method: To avoid the confounding effects of a current eating disorder, and to assess possibly trait-related disturbances, we studied 10 subjects recovered (1 year) from a bulimic-type eating disorder and 6 control women. Subjects were administered a solution of glucose or artificial saliva (control solution) in alternating blocks during a functional magnet resonance imaging scan. Results: Individuals who recovered from a bulimic-type eating disorder had significantly lower activation in the right Introduction Bulimic eating patterns are characterized by episodes of overeating and compensatory purging Accepted 17 April 2005 Presented at the Annual Meeting of the Society of Biological Psychiatry, New York, April 2004. Supported by a grant entitled ‘‘The Evaluation of Brain Neuronal Activity in Response to Taste Stimuli: A Pilot Study and Method for Taste Activation Assessed by fMRI’’ (to GKF) from the Obesity/Nutrition Research Center, Pittsburgh, PA, by the National Institute of Mental Health (NIMH) Training Grant T32MH18399 (to GKF), and by NIMH (WK PI) R01 MH42984 and MH46001 and K05 MH018940. *Correspondence to: Walter H. Kaye, MD, University of Pittsburgh Western Psychiatric Institute and Clinic, Iroquois Building, Suite 600, 3811 O’Hara Street, Pittsburgh, PA 15213. E-mail: kayewh@upmc.edu 1 Department of Psychiatry, School of Medicine, University of Pittsburgh, Western Psychiatric Institute and Clinic, Pittsburgh, Pennsylvania 2 Department of Psychiatry, University of California, San Diego, La Jolla, California 3 Department of Psychiatry and Behavioral Sciences, Imaging Center/UDCMC, University of California, Davis, Davis, California Published online 27 October 2005 in Wiley InterScience (www.interscience.wiley.com). DOI: 10.1002/eat.20210 ª 2005 Wiley Periodicals, Inc. 76 anterior cingulate cortex (ACC; Montreal Neurological Institute [MNI] coordinates x ¼ 8, y ¼ 22, z ¼ 28; cluster size ¼ 18 voxels, T ¼ 5.11, Z-score ¼ 3.78) and in the left cuneus (occipital cortex; MNI coordinates x ¼ 12, y ¼ 78, z ¼ 10; cluster size ¼ 21 voxels, T ¼ 4.27, Z-score ¼ 3.36), when glucose was compared with artificial saliva. Conclusion: The ACC plays a role in the anticipation of reward. Individuals with bulimic-type eating disorders may have a reduced reward response to nutrients, and thus may be vulnerable to overeating. However, this is a small sample and the current study will need replication in a larger sample size with investigation of additional regions of interest. ª 2005 by Wiley Periodicals, Inc. Keywords: brain pathways; appetite; bulimic-type eating disorder; overeating; (Int J Eat Disord 2006; 39:76–79) behavior, which may consist of self-induced vomiting and the use of laxatives or diuretics. Such eating behaviors occur in subjects with bulimia nervosa (BN) as well as in subjects with the binge/purge subtype of anorexia nervosa (AN-B/P). These eating disorders (EDs) are cross-transmitted in families1 and share similar behavioral symptoms,2 suggesting that they are related. It is not known whether individuals with BN have a primary disturbance of appetite regulation. The modulation of appetite is complex and involves smell, taste, conditioned learning behavior, various neurotransmitter systems, and peripheral as well as central neurotransmission.3,4 Altered taste perception has been found in women with BN, who preferred sweeter stimuli compared with women without an ED.5,6 Other studies found that altered hedonic response to sucrose may be related to conditioned thoughts about weight gain,7 and that taste response in BN may extend to other nutrient solutions such as fat preparations.8 Recent imaging studies suggest alterations of frontal, temporal, and cingulate brain regions in individuals with BN and AN-B/P.9–11 The orbital frontal cortex, anterior Int J Eat Disord 39:1 76–79 2006 ALTERED BRAIN ACTIVITY cingulate cortex (ACC), anteromedial temporal cortex, and insula contribute to the modulation of taste and other aspects of feeding, such as the hedonic or rewarding aspects of food consumption.12–14 Recently, we developed a method for the assessment of brain activity in response to taste stimuli using functional magnet resonance imaging (fMRI) scanning.15 In that methods study, we examined nonfasted control women (CW). The current study was conducted to test the possibility that BN subjects have a disturbance of appetitive modulation as reflected in altered processing of glucose (GLU) in regions that might play a role in the hedonic or rewarding aspects of feeding. Because all our other imaging studies in EDs have a standardized design with subjects fasted overnight, we changed the original fMRI design and studied fasted subjects. To avoid the confounding effects of the extremes of feeding behavior and malnutrition, our group has investigated women who had recovered for 1 year from an ED. Some, but not all studies, showed that a disturbance of serotonin activity persists after recovery from an ED.16 Moreover, anxiety, perfectionism, and obsessionality, as well as altered attitudes toward food and body image, have been found to occur premorbidly, and persist after recovery from an ED.16 Together, these data raise the possibility that vulnerabilities, such as altered appetite regulation, may be traits that contribute to the risk for developing an ED. Methods Subjects recovered from a bulimic-type ED (RBN; 7 BN without a history of AN and 3 BN with a history of AN [AN-B/P]) were compared with 6 CW. Criteria for the recovered state and CW have been described previously.9 Subjects were studied during the first 10 days of the follicular phase of the menstrual cycle. The study was approved by the local institutional review board, and written informed consent was obtained from all subjects. Subjects were fasted overnight before the study. The methods for taste activation using a customized design and fMRI have been described previously.15 In brief, a customized pump delivered taste stimuli during fMRI scanning. GLU was contrasted with artificial saliva (AS; control solution). 1 molar GLU solution was chosen to be able to compare results with studies from the Rolls group.17 fMRI scanning was performed on a 3T MR scanner. Each taste stimulus was followed by 6 T2* weighted functional scans (TE 7, TR 2000, flip angle 70 ; reverse spiral acquisition). Statistical parametric mapping (SPM2, London, UK; http:// www.fil.ion.ucl.ac.uk/spm/spm2.html) was used for image analysis. Images were realigned, coregistered (12-parameter Int J Eat Disord 39:1 76–79 2006 affine transformation) in Montreal Neurological Institute (MNI) space, and smoothed (8 mm isotropic Gaussian kernel). Data were analyzed in an event-related design. For each subject, contrast images were generated for GLU > AS, and then used for a second-level, random-effects regression analysis (independent sample t test). The statistical maps were thresholded at a significance level of p .001 (uncorrected for multiple comparisons), 7-voxel minimum cluster size to correct for multiple comparisons.18 The SPSS statistical software package19 was used for demographic statistical analyses. Due to the relatively small sample size, between-group comparisons were made with nonparametric Mann–Whitney U two-independent-samples tests calculating two-sided exact significance levels. This research was reviewed and approved by an institutional review board. Results The RBN subjects (27.5 ± 7 years) and CW (22 ± 2 years) were of similar ages (Mann–Whitney U ¼ 18.5; p ¼ .2). Current body mass index (BMI) was 22 ± 3 for RBN and 21 ± 2 for CW (Mann–Whitney U ¼ 19; p ¼ .6). The length of recovery was 12–180 months (45 ± 60 months). Within groups (data not shown), the CW had greater activation (GLU > AS) in the right ACC and posterior cingulate cortex, whereas RBN subjects had greater activation in the right lateral prefrontal cortex, subcallosal gyrus, and lingual gyrus. Between-group analysis (GLU > AS contrast images; Figure 1) showed that the CW had significantly higher activation compared with RBN in the right ACC (MNI coordinates x ¼ 8, y ¼ 22, z ¼ 28; cluster size ¼ 18 voxels, T ¼ 5.11, Z-score ¼ 3.78), as well as in the left cuneus (occipital cortex; MNI coordinates x ¼ 12, y ¼ 78, z ¼ 10; cluster size ¼ 21 voxels, T ¼ 4.27, Zscore ¼ 3.36). There was no area with higher activation in RBNs compared with CW. When contrasting subjects with BN without a history of AN (n ¼ 7) with the CW, the ACC with the similar MNI coordinates (x ¼ 8, y ¼ 22, z ¼ 28) was significant at p .01 (uncorrected for multiple comparisons). Conclusion To our knowledge, this is the first imaging study to investigate whether individuals with BN have an altered brain response to GLU. We found that women recovered from BN had reduced activity, compared with CW, in response to GLU, in the ACC and cuneus. Other imaging studies have 77 FRANK ET AL. FIGURE 1. Areas of significant greater activation in control women (CW) compared with recovered bulimic women (RBN) in the SPM format. (A) Glass brain with activation in the anterior cingulate cortex (ACC; Montreal Neurological Institute [MNI] coordinates x = 8, y = 22, z = 28; cluster size = 18 voxels, T = 5.11, Z-score = 3.78) and in the cuneus (MNI coordinates x = 12, y = 78, z = 10; cluster size = 21 voxels, T = 4.27, Z-score = 3.36), at p .001, uncorrected. (B) ACC activation overlaid on a reference image. found altered serotonergic activity in similar cingulate regions in BN subjects.11,20 Moreover, Uher et al.21 reported that pictures of food increased activity in the ACC and other regions in BN subjects compared with CW. The ACC plays an important role in initiation, motivation, and goal-directed behaviors,22 as well as in the anticipation of reward.23 It is possible that altered ACC activity could result in a disturbance of taste reward expectancy in individuals with BN. Thus, they may overeat or seek to eat sweeter foods. Consistently, a previous study found that BN subjects prefer sweeter stimuli compared with CW.5,6 All subjects reported the GLU solution as sweet and pleasant. This pilot study did not include a formal questionnaire for taste preference. Thus, it is not known whether the altered brain response in recovered BN subjects correlated with subjective pleasantness ratings. This question is currently being addressed in our ongoing studies. Little information exists on taste perception after recovery from an ED.24 It is not known whether alterations after recovery were present before the onset of BN, were a ‘‘scar’’ caused by the illness, or were an adaptive process related to recovery. Taste experience is strongly influenced not only by biologic processes, but also by conditioned processes.25 This is also the case for BN subjects.7 In addition, altered taste response has been related to altered perceptional physiology of the tongue in ill BN subjects.26 It is therefore possible that any of these factors could be implicated in the altered brain response in this group of RBN subjects. Those questions are targets for future research in our studies. Moreover, taste is only a part of appetite modulation3,4 and more complex studies that 78 discern biologic from cognitive factors will help to understand pathologic eating behavior in BN. To our knowledge, altered cuneus activation has not been reported in BN. This area may have functions that extend beyond visual activity including borderline personality,27 which shares behavioral traits with BN. We did not inquire about mood states in this pilot study. An exploratory analysis showed a relation between bulimia symptom scores, as assessed by the Eating Disorders Inventory,28 and the ventrolateral striatum (MNI coordinates 22, 16, 6, cluster size ¼ 15 voxels, p ¼ .005). Others have found binge eating to be associated with striatal activation.29 A previous study found regional cerebral blood flow normal in RBN compared with CW,30 suggesting this was not a contributing factor. In addition, data from our laboratory (data not shown), using positron emission tomography, suggested that there was similar resting blood flow between recovered pure BN and anorexic-bulimic subjects. There was an age difference between groups that was not significant. An exploratory analysis of an age relation with the outcome variable (contrast image) did not show any age relation for the studied groups. The cluster size in the current study was small compared with studies that stimulated emotional reactions.21 However, only a subset of neurons may respond to reward expectancy.23 In addition, expecting or receiving a food reward, or their combination, may have different activation patterns.31 We did not find differences in orbitofrontal activation within or between subject groups. Recent studies,32 as well as our preliminary data, suggest that orbitofrontal activation may be particularly related to sensory-specific satiety or to subjects’ Int J Eat Disord 39:1 76–79 2006 ALTERED BRAIN ACTIVITY fasting status. That is, we found orbitofrontal activation in nonfasted subjects in our previous study that described the methods for the current investigation,15 as well as in a second cohort of five nonfasted CW (unpublished data), but pronounced cingulate activation in fasted CW in the current study. Thus, the status of food ingestion before fMRI studies may have important influence on results.32 A limitation of this pilot study is its small sample size. A larger sample will be needed to replicate this finding as well as to investigate more regions of interest. This may help us to understand the pathways of central taste transmission in BN. In summary, the current study suggests lower activity in the ACC and cuneus in response to a GLU challenge in RBN compared with CW. This raises the possibility that women with BN may have alterations of mechanisms that model the taste reward aspect of food. The fact that this is found after recovery supports the speculation that this may be a trait-related disturbance. The authors thank Eva Gerardi for her editorial help with preparation of the article, and the staff at the University of Pittsburgh functional magnetic resonance imaging facility for their help with conducting the study. References 1. Kaye WH, Greeno CG, Moss H, et al. Alterations in serotonin activity and psychiatric symptoms after recovery from bulimia nervosa. Arch Gen Psychiatry 1998;55:927. 2. Garner DM, Garfinkel PE, O’Shaughnessy M. The validity of the distinction between bulimia with and without anorexia nervosa. Am J Psychiatry 1985;142:581. 3. Blundell J, Lawton C, Hill A. Mechanisms of appetite control and their abnormalities in obese patients. Horm Res 1993; 39:Suppl 3:72. 4. Rolls ET. Smell, taste, texture, and temperature multimodal representations in the brain, and their relevance to the control of appetite. Nutr Rev 2004;62:11 Pt 2:S193; discussion S224. 5. Drewnowski A, Halmi KA, Pierce B, et al. Taste and eating disorders. Am J Clin Nutr 1987;46:442. 6. Franko DL, Wolfe BE, Jimerson DC. Elevated sweet taste pleasantness ratings in bulimia nervosa. Physiol Behav 1994;56: 969. 7. Eiber R, Berlin I, de Brettes B, et al. Hedonic response to sucrose solutions and the fear of weight gain in patients with eating disorders. Psychiatry Res 2002;113:173. 8. Sunday SR, Halmi KA. Taste perceptions and hedonics in eating disorders. Physiol Behav 1990;48:587. 9. Frank G, Bailer U, Henry S, et al. Neuroimaging studies in eating disorders. CNS Spectr 2004;9:539. 10. Kaye WH, Frank GK, Meltzer CC, et al. Altered serotonin 2A receptor activity in women who have recovered from bulimia nervosa. Am J Psychiatry 2001;158:1152. Int J Eat Disord 39:1 76–79 2006 11. Tiihonen J, Keski-Rahkonen A, Lopponen M, et al. Brain serotonin 1A receptor binding in bulimia nervosa. Biol Psychiatry 2004;55:871. 12. O’Doherty J, Rolls E, Francis S, et al. Representation of pleasant and aversive taste in the human brain. J Neurophysiol 2001;85:1315. 13. Small DM, Zald DH, Jones-Gotman M, et al. Human cortical gustatory areas: a review of functional neuroimaging data. Neuroreport 1999;10:7. 14. Small DM, Voss J, Mak YE, et al. Experience-dependent neural integration of taste and smell in the human brain. J Neurophysiol 2004;92:1892. 15. Frank G, Kaye W, Carter C, et al. The evaluation of brain activity in response to taste stimuli-a pilot study and method for central taste activation as assessed by event-related fMRI. J Neurosci Methods 2003;131:99. 16. Kaye W, Strober M, Jimerson D. The neurobiology of eating disorders. In: Nestler DSCaEJ, editor. Neurobiology of mental illness. New York: Oxford Press; 2004, p 1112. 17. Francis S, Rolls E, Bowtell R, et al. The representation of pleasant touch in the brain and its relationship with taste and olfactory areas. Neuroreport 1999;10:453. 18. Forman S, Cohen J, Fitzgerald M, et al. Improved assessment of significant activation in functional magnetic resonance imaging (fMRI): use of a cluster-size threshold. Magn Reson Med 1995;33:636. 19. SPSS I. SPSS for windows. Release 11.0.1. Chicago: SPSS; 2001. 20. Bailer U, Price JC, Meltzer CC, et al. Altered 5-HT2A receptor activity after recovery from bulimia-type anorexia nervosa: relationships to harm avoidance and drive for thinness. Neuropsychopharmacology 2004;29:1143. 21. Uher R, Murphy T, Brammer M, et al. Medial prefrontal cortex activity associated with symptom provocation in eating disorders. Am J Psychiatry 2004;161:1238. 22. Devinsky O, Morrell M, Vogt B. Contributions of anterior cingulate cortex to behaviour. Brain 1995;118:279. 23. Richmond B, Liu Z, Shidara M. Neuroscience. Predicting future rewards. Science 2003;301:179. 24. Sunday S, Halmi K. Taste perceptions and hedonics in eating disorders. Physiol Behav 1990;48:587. 25. McClure S, Li J, Tomlin D, et al. Neural correlates of behavioral preference for culturally familiar drinks. Neuron 2004; 44:379. 26. Rodin J, Bartoshuk L, Peterson C, et al. Bulimia and taste: possible interactions. J Abnorm Psychol 1990;99:32. 27. Juengling F, Schmahl C, Hesslinger B, et al. Positron emission tomography in female patients with borderline personality disorder. J Psychiatr Res 2003;37:109. 28. Garner D. Eating Disorder Inventory-2 professional manual. Odessa, FL: Psychological Assessment Resources; 1991. 29. Inoue K, Kiriike N, Okuno M, et al. Prefrontal and striatal dopamine metabolism during enhanced rebound hyperphagia induced by space restriction—a rat model of binge eating. Biol Psychiatry 1998;44:1329. 30. Frank GK, Kaye WH, Greer P, et al. Regional cerebral blood flow after recovery from bulimia nervosa. Psychiatry Res 2000;100:31. 31. O’Doherty JP, Deichmann R, Critchley HD, et al. Neural responses during anticipation of a primary taste reward. Neuron 2002;33:815. 32. Kringelbach ML, O’Doherty J, Rolls ET, et al. Activation of the human orbitofrontal cortex to a liquid food stimulus is correlated with its subjective pleasantness. Cereb Cortex 2003;13:1064. 79