Laparoscopic Radical Prostatectomy Dr. J.L Hoepffner Clinique St Augustin,

Laparoscopic Radical
Prostatectomy
Dr. J.L Hoepffner
Clinique St Augustin,
Bordeaux
FRANCE
History
Schuessler ‘94
Raboy ‘97
Gaston ‘97
Guillonneau ‘98
2006: 50% prostatectomies laparoscopic
LAPAROSCOPIC APROACH
TRANSFORMATION of the
PROSTATECTOMY :
– Mini invasive Surgery
–
–
–
–
–
Easier exposition, Magnification of the vision
Définition anatomic plans
Précision of the gestual , Miniaturisation of the sutures
Bloodless
Post-operative more simple
LAPAROSCOPIC APROACH
IMPROVEMENT OPEN SURGERY
SAFETY ONCOLOGIC
REDUCTION OF FUNCTIONAL
SEQUELLA
LAPAROSCOPIC APROACH
LIMITS AND DISAVANTAGES :
– Quality of the vision
– Steadiness of the instrument
– Difficulty of the access ,
– Limit of the angular dissection
– Discomfort of the surgeon
LAPAROSCOPIC APROACH
NEW LIMITS FOR A DISSECTION
PRESERVATIVE AND ATRAUMATIC
OF THE PROSTATE
NEW LIMITS FOR PROGRESS IN
ERECTILE PRESERVATION
ROBOT ASSISTED:
ONE ANSWER ?
QUALITE OF OPERATIVE VISION +++
PRECISION OF THE ANATOMIC
DEFINITION
REDUCTION TRAUMATIC DISSECTION
DISAPPAERANCE OF THE LIMITS OF
THE DISSECTION
COMFORT AND LOGICAL ERGONOMY
FOR THE SURGEON
ROBOT ASSISTED :
A TECHNICAL ADVANTAGE?
DEMONSTRATION :
Bladder neck dissection
Bundle preservation
Suturing
Opératoring Indications
Curative
T1 – T2
T3 ?
Gleason score / age
Nerve Sparing ?
Alternative : EBRT – brachytherapy
Pre-operative Status
Cardiovasculary exam
Respiratory Fonction
Hemostasis blood test
No autologus transfusion
8-10 weeks after biopsies
Pré-opératorive State
Obesity not exclude
No bowel préparation
No specific contre-indications to the laparoscopic surgery
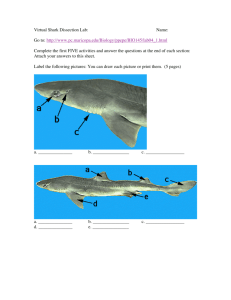
Technique
Patient in Trendelenburg position
One surgeon, one assistant
5 trocars: 1 x 10 mm , 4 x 5mm
Video column between the legs
Laparoscope 0°
Laparoscopic Instruments
•Needle driver
•Monopolaire
•Bipolaire
•Grasp
•Thin grasp
LAPAROSCOPIC APROACH
LAPAROSCOPIC APROACH
THE ROBOT
Trocards Placement
Optic Ports
Assistent Ports
Robot Ports
The ‘Da Vinci’ Sytem
THE ROBOT
THE ROBOT
THE ROBOT
Laparoscopic Bladder Neck
Dissection
Bladder Neck Robotic
Dissection
Seminales Vesicules
Laparoscopic Dissection
Right Bundle Laparoscopic
Dissection
Intrafasciale Robotic Dissection
Apex Laparoscopic Dissection
Apex Robotic Dissection (1)
Apex Robotic Dissection(2)
DVC Suture
(running suture)
Urétro-Vésicale Laparoscopic
Anastomosis
(running suture)
Anastomose Robotique urétro-vésicale
(running suture)
Laparoscopic Data
3000 patients
Study of 1574 files
Mean Psa 6,72
Mean Gleason score 6,27
Age 61,9 years old
Eur Urol. 2006 Feb;49(2):344-52
OUR DATA
OPERATIVE TIME 120 MN
HOSPITALISATION 5.7 JOURS
0 CONVERSION in 7 years
OUR DATA
COMPLICATIONS
HAEMORRHAGES 1.3%
ANASTOMOSIS FISTULA 0.3%
RECTAL INJURY 0.5%
URETERAL INJURY one case
ANASTOMOTIC STENOSIS <1%
EVENTRATION <1%
OUR DATA
PATHOLOGICAL RESULTS 1293
PT2A 10.2%
PT2B.C 57.8%
PT3A 28.2%
PT3B 3.8%
MARGINS
TOTAL 22%
T2 14%
T3 36%
FUNCTIONAL RESULTS
CONTINENCE
ERECTION : THE CHALLENGE
–
– better result ?
Better complete recovery?
– reduce the delay of recovery ?
– OBLIGATION of an EVALUATION
How can we improve functional result ?
?
!
Better knowledge of the prostate anatomy
Principles of preservation
High incision of pelvic fascia
From Eichelberg C,
European urology, 2006
During radical prostatectomy, innervation of the trigone, neobladder neck, and posterior urethra may become disrupted, because the surgical procedure involves anatomic dissection around the prostate, posterior aspects of the bladder base, and seminal vesicles.
afferent innervation of the trigone posterior urethra may lead to alterations in posterior urethral sensation indirectly contribute to outlet
UROLOGY 55: 820–824, 2000.
The percentage continence rates at a4 weeks and 12 months after surgery.
Level of Evidence 1b
96,3%
85,7%
62,7%
45%
From Peter Albers
BJU Int 1 0 0 , 10 5 0 – 10 5 4, 2007
Antegrade dissection
Traction on Seminal vesicles
Injury to the nerves
From Stolzemburg
European Urology 51 ( 2 0 0 7 ) 629–639
Detrusor apron
Detrusor apron (arrowheads) in Masson trichrome-stained sagittal section through adult cadaveric prostate. Detrusor apron ends in tuft (arrow) that is transected end of pubovesical (puboprostatic) ligament. Tuft contains fibrous tissue (blue) and smooth muscle fibers (red) that curve and course anteriorly to the large venous sinus. s, sphincter; u, urethra; P-pz, prostate-peripheral zone; Bu, bulb of penis; R, rectum.
Inset, magnified tuft. Note, smooth muscle fibers beneath leftmost arrowhead stained poorly.
From Robert P. Myers
UROLOGY 59: 472– 479, 2002
FUNCTIONAL RESULTS
QUESTIONNAIRE ICS CONTINENCE
NO PADS AT 6 MONTHS 87%
FUNCTIONAL RESULTS
AUTOQUESTIONNAIRE IEFF 5 FOR
THE SEXUALITY
57% AT ONE AYEAR
LAPAROSCOPY
REVOLUTION IN THE SURGICALTECHNIQUE
RESULTS THE SAME THAN OPEN
GREAT DEVELOPPEMENT
LAPAROSCOPY
DIFFICULTY OF THE FIRST CASES
LEARNING CURVE
PUBLICITY OF A NEW TECHNIQUE
LAPAROSCOPY
THE ROBOT ?
ROBOTIC DATA
230 PATIENTS 2005
2 CONVERSIONS IN CLASSICAL LAP
TRANSFUSION 2%
OPERATVE TIME 150MN
Positive Margins
Laparoscopy
30,75
69,25
81,50 %
18,49%
Sexuality
80 ,3%
58,5 %
41,5 %
19,7 %
Continence
Laparoscopy at 1 Year
95 %
Robotic at 4 months
92,40 %
7,60 %
5%
ROBOTIC DATA
HOSPITALISATION 4.6 DAYS
FOR 100CAS
CONTINENCE AT 3 MONTHS 72%
ERECTION +- viagra 66.9%
CONCLUSIONS
ROBOTIC ASSISTED :
………..MAKE EASIER THE RADICAL
PROSTATECTOMY
Quality of the vision
Miniaturization of the dissection
Preservation of the anatomical structures
…….IMPROVE FUNCTIONNALS RESULTS
CONCLUSIONS
ROBOTIC ASSISTED
………THE LIMITS :
– ECONOMIC COST
– TIME IN THE THEATER MORE LONGER
– LEARNING CURVE
CONCLUSIONS
ROBOTIC ASSISTED :
A HIGH LEVEL OF OPERATIVE
QUALITY
EXCELLENT FOR RADICAL
PROSTATECTOMY
LOGICAL AFTER OR AT THE SAME
TIME FOR A LAP CENTER
CONCLUSIONS
Radical prostatectomy: treatment of choice
Laparoscopic prostatectomy: excellent approach
Robotic prostatectomy: The future or the present??
But…
…we are still far away from the comprehension of the prostate’s anatomy, and we are confident that the robotic technique will give us a great help……