2009 Safety and Compliance Education/Test
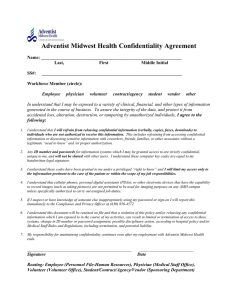
advertisement

2009 Safety and Compliance Education/Test The 2009 Safety and Compliance Education Test (Safety Fair) is now available. All AMH employees hired before January 1, 2009 must pass this quiz with a minimum score of 80% by December 31, 2009. If you were hired on January 1, 2009 or later, you are NOT required to take this quiz. 2009 Safety and Compliance Education/Test ....................................................... 1 Index .................................................................................................................. 1-2 Environment of Care ........................................................................................ 3-13 Emergency Management Codes ....................................................................... 3 Fire Prevention/Life Safety ................................................................................ 5 ∞ CODE RED............................................................................................. 5 ∞ R.A.C.E. Procedures .............................................................................. 5 ∞ Know How to Use a Fire Extinguisher .................................................... 4 ∞ Egress Safety & Compliance .................................................................. 6 ∞ Interim Life Safety: What is Interim Life Safety?.................................... 7 Utilities ............................................................................................................... 8 ∞ CODE GREEN........................................................................................ 8 ∞ These are Our Utilities ............................................................................ 8 ∞ Scope of Problem ................................................................................... 8 Secure Our Buildings! ....................................................................................... 9 Medical Equipment .......................................................................................... 10 ∞ User Error ............................................................................................. 10 ∞ Abuse.................................................................................................... 10 ∞ Safe Medical Device Act of 1990.......................................................... 10 Hazardous Materials & Waste ......................................................................... 11 ∞ CODE ORANGE................................................................................... 11 ∞ Material Safety Data Sheets ................................................................. 11 ∞ Do You Know If Your Department Has or Needs a Spill Kit? ............... 11 The Plan for Safety.......................................................................................... 12 ∞ Employee Injury Reporting ................................................................... 12 ∞ Oxygen Tank Safety ............................................................................. 12 ∞ MRI (Magnetic Resonance Imaging) Safety ......................................... 13 Risk Management .......................................................................................... 14-16 Patient Rights .................................................................................................. 14 1 It takes a Village when it comes to Victims ..................................................... 14 Patient Safety ................................................................................................. 15 National Patient Safety Goals from The Joint Commission ........................... 17-20 Patient Safety is our #1 Priority ....................................................................... 16 Infection Control .................................................................................................. 18 Precautions / Education .................................................................................. 18 Isolation Education .......................................................................................... 18 Patient Education ............................................................................................ 18 Family and Visitor Personal Protection ........................................................... 18 Personal Protective Equipment (PPE) ............................................................ 18 Influenza ......................................................................................................... 19 Tuberculosis & Bloodborne Pathogens............................................................... 21 Tuberculosis .................................................................................................... 21 Employee TB Skin Testing .............................................................................. 21 Annual N-95 Fit Testing................................................................................... 21 Bloodborne Pathogen Control ......................................................................... 21 Prevention of Exposure at Work...................................................................... 21 Engineering Practices ..................................................................................... 21 Work Practices ................................................................................................ 21 Warning Labels ............................................................................................... 22 Blood and Body Fluid Exposure Follow-Up ..................................................... 22 Hand Hygiene ..................................................................................................... 22 New Information: Hand Hygiene Alert!!! ......................................................... 23 Sharps Safety ..................................................................................................... 23 Fit For Duty? ...................................................................................................... 25 Ergonomics ......................................................................................................... 26 Safe Patient Handling...................................................................................... 27 Safe Lifting Basics ........................................................................................... 28 Corporate Compliance ........................................................................................ 30 Tips for Protecting Patient Privacy .................................................................. 30 Language Interpretation .................................................................................. 31 TIPS For Effective Use of An Interpreter ......................................................... 31 Celebrating Cultural Diversity ............................................................................. 32 S.H.A.R.E.......................................................................................................... 333 2 ENVIRONMENT OF CARE SAFETY Emergency Management CODES - When the Alarm Sounds . . . Know Your Emergency Codes Code Triage is the emergency code that tells us to expect an influx of patients. The command center opens and communication flows from the command center to the managers by pager, e-mail or courier. As part of the emergency preparedness and infection control plans, a broad range of options can be implemented to accommodate a large number of patients at one time and for weeks to come. Such options are to: ∞ Temporarily stop or limit services like outpatient tests or surgeries ∞ Increase patient discharge to home with home health support ∞ Transfer patients to other hospitals or nursing homes ∞ Limit visitors ∞ Allow only necessary staff and others to enter the hospital Communication with emergency responders, public health authorities and staff at the hospital are very important. Adventist Midwest Health Hospital Code Description Triage Disaster conditions exist; incoming patients Gray Security Assistance Yellow Trauma Team Green Utilities Failure Brown Bomb Threat Orange Hazardous material spill Blue Cardiac/Pulmonary Arrest Purple Patient Elopement Pink Infant or Child Abduction Red Fire, smoke or smell of something burning Black Severe Weather Some of our facilities use Code Silver to alert staff that Silver someone has displayed a deadly weapon Environment of Care Safety 3 Fire Prevention/Life Safety CODE RED It is each employee’s responsibility to know and participate in drills for their department’s fire and evacuation plan. Read it….review it often….practice…..be ready to put into action if it becomes necessary! If you discover a fire, smell or see smoke, you should LOUDLY call out CODE RED and with your departmental coworkers, immediately implement R-A-C-E procedures. R.A.C.E. Procedures R A = RESCUE anyone in immediate danger of being burned by the fire = ACTIVATE the ALARM by pulling the closest fire alarm pull station, AND report the fire by calling your facility’s emergency telephone extension below: Adventist Bolingbrook Hospital = x555 Adventist GlenOaks Hospital = x555 Adventist Hinsdale Hospital = x555 Adventist La Grange Memorial Hospital = x555 Non-Hospital Departments = 9-911 (If hospital based phone system is utilized) x911 (If NO hospital based phone system is utilized) C E = CONTAIN the smoke by closing all corridor/hall doors = EXTINGUISH the fire if possible, and be prepared to EVACUATE to a safe area as needed Know How to Use a Fire Extinguisher P A S S = = = = Pull the safety pin Aim the hose/horn at the base of the fire Squeeze the handle to discharge the extinguisher Sweep the hose/horn at the base of the fire Egress Safety & Compliance 4 Who do we need to comply with? Joint Commission EGRESS SAFETY & COMPLIANCE Life Safety Code 7.1.10 Means of Egress Reliability What about the 30 minute rule? There is no written rule by any of the Regulatory Agencies. Surveyors do understand that items may be in the hallway or in a doorway momentarily, but they monitor how long the object stays there. Some surveyors have been known to time on this time boundary 7.1.10.1 Means of egress shall be continuously maintained free of all obstructions or impediments to full instant use in the case of fire or other emergency. 7.1.10.2.1 No furnishings, decorations, or other objects shall obstruct exits, access thereto, egress therefrom, or visibility thereof. What about items in use? What does this mean for your department? • All egress of (pathway to any exit – you should see an exit sign) must be clear at all times. • Any time the FIRE ALARM sounds, all items in the means of egress shall be removed immediately. • See the 30 minute rule question. However, charging items in the corridor and then calling them “in use” is unacceptable and a violation of egress. Surveyors will watch to see if an item has moved, even the shortest distance. Can crash carts remain in the means of egress? Other unacceptable commonly found items in corridor: items charging, WOWs not in use, chairs at countertops located in the hallway, transportation items left unattended, any obstructions that expands beyond 7” from the wall, decorations, items stored in alcoves that go beyond the designated space of the alcove. Crash carts can remain in the means of egress, but a permanent location is preferred since items cannot be charged in the means of egress. Isolation carts and Latex Free carts for clinical need patients only can remain right outside the room. However, please remove out of the means of egress if FIRE ALARM sounds. For more information on egress safety & compliance or reporting of any safety hazards contact your hospital Safety Officer. Environment of Care 5 What is Interim Safety? Interim Life Safety ∞ Change in normal exit routes; ∞ Special direction or caution signage; ∞ Temporary construction partitions; ∞ More fire extinguishers; ∞ Special training for the staff in and around the area; ∞ Extra daily inspections to ensure the environment remains safe; ∞ Extra Fire Drills; ∞ Stay out of construction areas; ∞ Only those with hard hats may enter the area; ∞ Employees must participate in extra fire drills; ∞ Be aware of exit and evacuation route changes; ∞ Be aware of who is in the department – construction workers should display appropriate identification at all times; ∞ Follow the Interim Life Safety Plan developed for your area; ∞ Keep corridors and exits free from obstacles; ∞ Employ your best housekeeping practices at all times; ∞ Immediately report any concerns or problems to your Safety Officer. Environment of Care 6 Utilities CODE GREEN When a utility fails in the hospital, we call a Code Green. It is your responsibility to report utility failures to your supervisor, administrator on-call, or by checking any Quick Response Wall Cards or emergency manuals and following the directions. These are Our Utilities “Utilities” includes many things, some the same as you have in your home. In a hospital, utilities include: ∞ Oxygen ∞ Heat ∞ Vacuum ∞ Air conditioning ∞ Medical air ∞ Ventilation ∞ Nurse call ∞ Elevator ∞ Intercom system ∞ Electricity ∞ Telephone ∞ Water ∞ Computers ∞ Sewage Scope of Problem ∞ If a utility fails in one department, the problem will be resolved without calling a Code Green. There is a difference in resolving a sink drain back-up in one department from a sewer back-up that affects multiple departments. ∞ A Code Green will only be called when there is the potential for significant impact on the health and safety of our patients. Secure Our Buildings! 7 Since we work in a facility that is open 24-hours every day, you have a responsibility to ensure security measures are followed for the protection of patients and employees. To help create a more secure environment: ∞ Wear your photo identification badge at all times while in the building; ∞ Know and follow the Non-Employee Identification Policy – business visitors, repair persons, construction workers must all wear one of two types of identification IDs – a temporary badge if they are here for one day or less; a photo ID if they are here more than one day; ∞ Immediately report any suspicious people or activities to Security; ∞ Know your Security Department employees – use the appropriate method of contact based on the situation – call a “Code” for emergency situations – contact a security officer for routine business activities; ∞ Know and respect security-sensitive departments (areas with an elevated element of risk due to the nature of their business): the Birth Center, the Emergency Department, Pharmacy, Pediatrics, H.I.M.; ∞ Guide patients, visitors and other guests to appropriate entrances. Do not allow nonemployees through secured doors; ∞ Be aware of people trying to enter a secured entrance behind you. Do NOT open secured doors for anyone; ∞ Do NOT use your Employee I.D. Badge to provide secured area access to non-employees; ∞ Call Security if someone enters a secured area behind you. Be prepared to give a description of the individual(s). 8 Environment of Care Damaged or Malfunctioning? How is your equipment failing? Medical Equipment User Error User error is using a device against the recommendations of the original manufacturer, resulting in a failure or misdiagnosis in the clinical environment. If you are unclear about the proper use of any device - ask questions or request training from your supervisor. Abuse Physical abuse is damage caused by usage against the recommendations of the equipment manufacturer, or intentional destruction or damage of a device (e.g., sabotage). Physical abuse service events are reportable to the safety committees of the facilities of Adventist Midwest Health. Any device that has been involved in a physical abuse event requires a complete performance test of all operations and alarms prior to clinical use. If the error or abuse has compromised patient care or hospital operations, then it must be reported immediately to your supervisor or manager. A Risk Management Event Report Form is completed and submitted online. All user errors and physical abuse are reported to the Environment of Care Safety Committees on a monthly basis. The Joint Commission requires us to have a plan for equipment needs in an emergency situation. Talk with your supervisor or manager about procedures to follow in the event of an emergency equipment failure in your department! Safe Medical Device Act of 1990 You MUST report incidents that reasonably suggest a medical device has caused or contributed to a patient’s death, serious illness, or serious injury. Actions Required: Tag and Remove from service – the equipment and any disposable items used with the equipment involved in the incident (i.e. administration sets, syringes, etc.) NOTE: DO NOT clean, repair, change settings, test operation, or dispose of the item until specifically authorized by Risk Management. Report the incident to your supervisor or manager immediately; Report the incident to Risk Management immediately if a patient was injured; Identify the following: - Type of equipment / supplies - Manufacturer’s name with device. Include: - Model / Serial number - Settings of controls when incident was discovered - Alarms on / off - Sterility control number - Hospital inventory / prevention maintenance number - Last preventative maintenance check indicated on equipment - Power supply - List of disposable supplies used in conjunction with device (include lot number) - Condition of equipment / supplies - Location of equipment / supplies Complete the online Risk Management Event Report Form 9 Environment of Care Hazardous Materials & Waste CODE ORANGE Material Safety Data Sheets The Government Says You have a Right to Know! the chemicals in your department how to protect yourself when using those chemicals how to safely handle hazardous materials The healthcare setting is not the place to play loose and carefree with all of the chemicals and wastes that can be harmful to employees as well as patients. You have a responsibility to know ∞ Where do I find MSDS Information? What is MSDS? o Material Safety Data Sheet On the Adventist Midwest Health Intranet under "Online Applications" What information is on a MSDS? Not all MSDS look the same but they are required to contain the same data. Here are some of the items that are included: ∞ ∞ ∞ ∞ ∞ Full Chemical Name Manufacturer Name Manufacturer Contact Information First Aid Procedures Types of Personal Protective Equipment Needed Do you know if your department has or needs a spill kit? Any department that handles or stores hazardous materials should have an appropriate spill kit(s) for their area. Department Managers should train their employees annually on the location and use of these spill kits. 10 Environment of Care The Plan for Safety AMH hospitals follow a plan to reduce your risk of injury at work. 1. Safety Information ∞ In Orientation: fire, hazardous chemicals, body fluid exposure, infectious disease ∞ In Your Department: equipment, safety devices, safe practices. 2. Finding and reducing job-related hazards, including use of safety devices, respirators, and safety equipment 3. Following safe work practices 4. Investigating incidents that occur 5. Everyone is responsible for the plan. YOU, your SUPERVISOR, the SAFETY OFFICER, the SAFETY COMMITTEE Report unsafe conditions immediately to Plant Operations/Building Services or the appropriate person/department Use all safety and protective equipment appropriately EMPLOYEE INJURY REPORTING 1. NOTIFY your supervisor immediately 2. FILL OUT the Online Employee Incident Report completely including WHO you are, WHAT happened, WHEN it happened, and HOW you feel (where does it hurt). The employee Incident Report is found on the Adventist Midwest Health Intranet 3. BRING a printed copy of the Report to Employee Health if possible. (when closed, leave a voicemail & bring later) 4. DO NOT go to the Emergency Room UNLESS your injury requires emergency care (AFTER regular Employee Health hours) 5. CONTACT Employee Health within 24 hours and the nurses will help you to evaluate your need for follow-up. If the office is closed, leave a detailed message for us and we will be in touch. OXYGEN TANK SAFETY ∞ ∞ ∞ ∞ ∞ ∞ ∞ NEVER let patients hold O2 tanks in their arms NEVER lay an O2 tank on a patient’s bed or carrier ALWAYS store O2 tanks in the approved storeroom, at least 5 feet away from anything else in the room REMEMBER--Empty tanks are still a hazard—some O2 is still inside RETURN empty tanks to tank room, place in a holder, mark “EMPTY” NEVER carry an O2 tank in your arms ALWAYS place O2 tanks in approved carriers and holder 11 MRI (Magnetic Resonance Imaging) SAFETY The magnet is ALWAYS ON, even when not in use ∞ ∞ ∞ ∞ Things that contain metal may be pulled into the scanner, like: scissors, tools, IV poles, oxygen tanks, wheelchairs, floor buffers, even jewelry Patients are screened before they enter the scanner, especially for pacemakers, neurostimulators, aneurysm clips, cochlear implants, & some orthopedic hardware NEVER enter the scanner room until cleared by the MRI technician No “Codes” or resuscitative efforts are attempted in the scanner room. The MRI tech will immediately move the patient to the holding area, if necessary 12 Risk Management Patient Rights PATIENTS HAVE THE RIGHT TO: 1. Have their Advance Directives honored An ADVANCE DIRECTIVE is a document in which an individual either states choices for medical treatment or designates who should make treatment decisions when they no longer can. Examples of an advance directive are organ donation, Illinois Department of Public Health (IDPH) Uniform Do-NotResuscitate (DNR) Order Form, livings wills and/or durable power of attorney for health care. 2. Privacy Patient privacy is a right afforded to patients upon admission, during treatment and upon discharge from the hospital. It is everyone's duty to protect patient privacy. 3. Appropriate assessment and management of pain Our PAIN MANAGEMENT POLICY requires health care workers to assess pain and implement interventions according to patient’s needs and as ordered by the physician. 4. Receive information about the outcomes of their treatment This right is addressed in the Regional UNANTICIPATED OUTCOME policy and states that patients and families are entitled to information about the outcomes of diagnostic tests, medical treatments, and surgical interventions whether those outcomes are anticipated or not. 5. Have their ethical issues addressed The ETHICS COMMITTEE works to help support patients rights throughout the hospital and assist with any physician, staff, patient or family member who may have a disagreement or need concerning treatment that may be controversial or confusing. Every campus has its own ethics committee. You can contact pastoral care, risk management, or social services/discharge planning in order to access the ethics committee. 6. Have their rights and welfare protected if they decide to participate in research The IRB (Institutional Review Board) follows established protocol in accordance with current Department of Health and Human Services and Food and Drug Administration regulations. The IRB assures that risks to research subjects are minimized; that subjects are selected fairly and equitably, and participation is voluntary, and informed consent is obtained from each subject. It takes a Village when it comes to Victims We have a community responsibility to protect those who may be victims of abuse and neglect. Victims can be young or old and may be members of the same household. Abuse can be physical, sexual or psychological. Reporting abuse and neglect allows an investigation to be conducted. 13 Illinois law provides immunity for reporting suspected abuse and/or neglect which means there must only be a reasonable basis for suspicion. For some patient care providers reporting suspected abuse and neglect is not an option – it is mandatory. However, many times victims and their abusers go to great lengths to cover abuse when they know someone is watching. That is why housekeepers, mechanics, food service workers, and volunteers are equally and vitally important in protecting our patients from abuse and neglect. Refer to your hospital’s policy for phone numbers to report and resources for victims. What do you do if you observe something suspicious or a patient shares information with you that would indicate that the patient may have been abused or neglected prior to hospitalization but you are not sure if it is abuse or neglect? You should immediately contact your manager and/or social services. Patient Safety Patient safety initiatives provide information to help prevent and reduce potential future harm to patients from the delivery of medical services. This knowledge is gained by identifying, reporting, and analyzing problems. Adventist Midwest Health supports a non-punitive environment that encourages employees to report potential and actual events. This environment will help us improve all processes and services for the safety of our patients. The three processes used to promote patient safety in the Midwest Region are: ∞ ∞ ∞ Sentinel Event Management Unanticipated Outcomes Incident and Medication Variance Reporting Sentinel Event Management A Sentinel Event is an event resulting in an unanticipated death or “major permanent loss of function” not related to the natural course of a patient’s illness or underlying condition. Not every bad outcome is a sentinel event. The decision to call something a sentinel event is made after a thorough investigation. Examples of possible sentinel events: 1. Suicide of any patient receiving care, treatment, and services in a staffed around-the-clock setting or within 72 hours of discharge 2. Discharge of an infant to the wrong family 3. Rape (defined according to law/regulation) 4. Hemolytic transfusion reaction involving administration of blood or blood products having major blood group incompatibilities 5. Surgery on the wrong patient or wrong body part 6. Unanticipated death of a full term infant defined as any perinatal death unrelated to a congenital condition in an infant having a birth weight greater than 2500 grams 7. Abduction of any individual receiving care 8. Unintended retention of a foreign object in a patient after surgery or other procedure 9. Severe neonatal hyperbilirubinemia (bilirubin greater than 30 milligrams/deciliter) 10. Prolonged fluoroscopy with cumulative dose greater than 1500 rads to a single field, or any delivery of radiotherapy to the wrong body region or greater than 25 percent above the planned radiotherapy dose 11. All identified cases associated with a health care associated infection including the management of patient before and after the identification of infection 14 Procedure if you are involved with a Sentinel Event: 1. Ensure appropriate care of the patient 2. Secure and sequester any physical evidence/devices involved in the event 3. Notify Risk Management (RM) immediately. RM, with the “screening” team, will review the scope and impact of the event. Unanticipated Outcomes An Unanticipated Outcome requires disclosure to patients and/or families. An example of an unanticipated outcome - during abdominal surgery a bowel is perforated requiring further surgical repair. Procedure: 1. Notify Risk Management. Incident and Medication Variance Reports The online Risk Management Event Report Form is a mechanism for reporting quality issues, improper performance of patient care duties, injuries, property damage, accidents, medication variances, or other events not anticipated. In order to provide safe care, all of us need to report potential (what could have gone wrong) as well as actual (what did go wrong) events. Potential events/variances are recognized, corrected and reported before they reach the patient. Actual events/variances are reported because they reach or impact the patient. As an example, a medication variance is an event in which a medication is dispensed and/or administered in a manner that varies from what was prescribed. Medication variance could also include prescribing variances by the physician (potential variance), omission of dispensing (potential variance) and/or administration (actual variance) of a prescribed medication. Reports need to be completed by the end of the shift in which the incident/variance/concern was identified. Reports that have complete and accurate information filled out help us understand the variance and its potential or actual impact on safe patient care. Completed online reports are emailed to the Manager/Assistant Director/Director and Risk Management. 15 National Patient Safety Goals from The Joint Commission Patient Safety is our #1 Priority It’s everyone’s job to make it safer for patients in our hospitals The purpose of the NATIONAL PATIENT SAFETY GOALS is to prevent patient harm The goals are reviewed and revised every year based on recommendations from experts on how to prevent the problems reported by hospitals across the country Our Patient Safety Programs are evaluated during visits by Accrediting Agencies such as the Joint Commission. We are continuously evaluating & refining our Patient Safety Programs by doing EOC/Safety Rounds, Tracers and education at all of the AMH facilities. We look for: ∞ Safe practices in action ∞ Adherence to the patient safety goals GOAL: ACCURATE PATIENT IDENTIFICATION Always use at least two patient identifiers (FOUND ON THE WRISTBAND) when drawing blood, collecting specimens for clinical testing, providing other treatments or procedures or administering medications. Acceptable identifiers are: ∞ PATIENT NAME ∞ DATE OF BIRTH ∞ MEDICAL RECORD NUMBER Note: NEVER use the room number as an identifier! ∞ Be sure to compare the two patient identifiers from the wristband with the patient information on requisitions, medications, and patient stickers. And ∞ Always label specimens at the bedside point of collection in the presence of the patient. Doing these two things will help to prevent mislabeled specimens. GOAL: IMPROVE COMMUNICATION BETWEEN CAREGIVERS Certain Lab test results, Cardiology, Respiratory, and Radiology test findings are Critical Values. Critical values could have a significant impact for the patient. Critical Values must be communicated to a physician who can act on the results. 16 Reading back verbal & telephone orders and Critical Test Results means you are validating the information. Timeliness & documentation of critical test results are being tracked to evaluate need for improvement. Critical TESTS have also been identified in the same areas. Time of the order for a Critical TEST until the results are available for the physician will be monitored. Avoid the Use of Unapproved Abbreviations. Follow the Guidelines Printed On All Physician Order Forms Legibility and readability improve patient safety! Write and Print Clearly~ Poor communication is the #1 cause of medical errors. GOAL: IMPROVE RECOGNITION AND RESPONSE TO CHANGES IN A PATIENT’S CONDITION Adventist Midwest Health facilities have Rapid Response Teams which provide early response by specially trained individuals to changes in a patient’s condition. During 2008, Teams have: ∞ ∞ ∞ ∞ ∞ ∞ Identified ways in which the patient, family or others can call a Rapid Response Developed and tested models for use in some specialty areas (Obstetrics, Pediatrics) Educated doctors and clinical staff about new changes Developed patient/family education and appropriate signage for patient rooms Piloted the processes Prepared to be fully implemented with this program by January 1, 2009 17 Infection Control Precautions / Education Standard Precautions ∞ Applies to all patients, all the time ∞ Requires health care workers to wear gowns, gloves, masks & eye protection when contact with body fluids or blood is possible ∞ Are always in effect even when utilizing additional transmission precautions Transmission Precautions Contact Precautions ∞ Wear gown and gloves every time you enter the room ∞ Change gloves after contact with infective material ∞ Remove gown and gloves upon leaving room ∞ Perform hand hygiene after gloves and gown are removed. ∞ Use soap and water for patients with diarrhea Droplet Precautions ∞ Wear simple mask when entering the room Airborne Precautions ∞ N-95 mask required when entering room ∞ Visitors wear a simple mask Isolation Education Patient Education ∞ ∞ ∞ Family and Visitor Personal Protection ∞ ∞ Explain to patients/visitors/family the reason for isolation Review with patients the personal protective equipment that staff, family and visitors must wear to safely care for them Document in the medical record that this education took place on the interdisciplinary Education form; check off isolation type and write in the diagnostic results. ∞ ∞ Family and visitors of a patient requiring: Contact Precautions – must wear same personal protective equipment staff wear Airborne Precautions – must wear a simple mask Droplet Precautions – must wear a simple mask Personal Protective Equipment (PPE) 18 Gloves ∞ Worn as part of Standard Precautions when handling all body fluids and broken skin ∞ Worn upon entry to a patient’s room for Contact Precautions ∞ Hands must be washed before putting on gloves and immediately after removing gloves ∞ Always inspect gloves for holes before wearing them ∞ Replace worn out or torn gloves Gowns ∞ Worn as part of Standard Precautions if clothing may come in contact with body fluids or broken skin ∞ Required to be worn upon entering a patient’s room requiring Contact Precautions Masks with Eye Protection ∞ Worn when splashing is possible, as part of Standard Precautions ∞ Simple masks are required of staff caring for a patient requiring Droplet precaution N-95 Respirator ∞ Health care workers must be fittested to wear an N-95 Respirator ∞ Health care workers must fit-check the N-95 Respirator each time they enter the room of a patient on ∞ Airborne Precautions N-95 Respirators are required to care for patients suspected or known to have TB, SARS, Monkey pox, Chicken pox and Measles. Influenza The Joint Commission (JCAHO) requires all health care workers to receive influenza education. All health care workers are encouraged to receive an annual seasonal influenza vaccination because unvaccinated health care workers can transmit influenza to patients. Outbreaks of influenza have been documented in hospitals and long term care facilities. Getting an influenza vaccination reduces the transmission of influenza in health care setting as well as reducing staff illness and absenteeism. Influenza vaccine is free, available through Employee Health. Influenza is a viral disease that occurs in annual epidemics in the U. S. It is a serious disease - each year 200,000 people are hospitalized with influenza – about 36,000 die because of it. 19 The flu shot works to prevent influenza. You can get the flu shot at any time during the flu season – usually October through March. You can not get influenza from the flu shot. 20 Tuberculosis & Bloodborne Pathogens Tuberculosis ∞ ∞ ∞ TB is a communicable disease caused by the Mycobacterium Tuberculosis or the Tubercle Bacillus Infectious droplets are spread in air when an infectious person sings, coughs, sneezes, or speaks Common symptoms of TB include: 1. Cough lasting more than 3 weeks in duration 2. Chest pain and bloody sputum 3. Fever, chills and night sweats 4. Weight loss 5. Increasing fatigue Employee TB Skin Testing ∞ Employees must have annual skin testing which is required by IDPH (Illinois Department of Public Health) and EHS (Employee Health Services) of Adventist Health System Annual N-95 Fit Testing ∞ Annual fit testing is required for all staff who must wear the N-95 respirator when caring for a known or suspected TB patient Bloodborne Pathogen Control Route of Transmission Work Related: ∞ ∞ Accidental needle stick Unprotected splash to the face Bloodborne Pathogens ∞ ∞ Human Immune Deficiency Virus (HIV) Hepatitis B (HBV) ∞ Hepatitis C (HCV) Others: ∞ ∞ ∞ ∞ Unprotected sex with an infected person Tattoos Body piercing Sharing toothbrushes and razor Prevention of Exposure at Work Engineering Practices Work Practices 21 EQUIPMENT WHICH REMOVES INFECTIOUS AGENTS IN A SAFE MANNER ∞ ∞ ∞ ∞ ∞ o o o SHARPS CONTAINER – All sharps must be placed in a securely mounted, puncture proof container Discard when 3/4 full. SELF SHEATHING NEEDLES NEEDLELESS SYSTEM ISOLATION TRASH BINS – Red bins that prevent leaking BIOHAZARD LABELS – Should be placed on any blood or body fluid o o o o No eating, drinking and smoking in Patient Care Areas Hand Washing No Recapping of needles/use safety needles No mouth pipetting/use automatic pipettes Remove clothing contaminated with blood or body fluids immediately Use Personal Protective Equipment Use hospital approved disinfectants to clean. Pay attention to disinfectant contact time. Warning Labels Warnings labels are affixed to the following: ∞ ∞ ∞ Containers of regulated waste Refrigerators and freezers containing blood or other potentially infectious materials Other containers used to store, transport, or ship blood or other potentially infectious material. Blood and Body Fluid Exposure Follow-Up After treating the exposure site and receiving appropriate treatment, document the exposure using the Employee Injury Report which can be found on the INTRANET. ∞ Make sure to include the following information: 1. Route of exposure (Where were you splashed, stuck, etc…) 2. Describe the circumstances of exposure (Type of needle, etc…) ∞ Notify your supervisor and contact Employee Health. After hours go directly to Emergency Department. ∞ You can expect: 1. To have appropriate testing of yourself and the source individual (if identified) 2. To be provided with your test results and those of the source individual through Employee Health. 3. Post exposure counseling and medical evaluation as needed ∞ POST EXPOSURE PROPHYLAXIS WHEN MEDICALLY INDICATED Hand Hygiene 22 New Information: Hand Hygiene Alert!!! CDC Hand Hygiene Guidelines and The Adventist Midwest Health Hand Hygiene Policies state: ∞ No artificial nails or nail extenders on any clinical staff who directly or indirectly touch patients such as: nursing, dietary, central sterile processing, pharmacy, respiratory therapy, phlebotomy and neurophysiology ∞ Short natural nails are recommended for clinical staff ∞ Clear nail polish may be worn if it is not chipped ∞ Studies have shown that artificial nails have been associated with infection transmission in hospitals. Hand Hygiene Prevent the transmission of health care associated infections by proper hand washing and the use of gloves. Soap and Water Hand Wash ∞ ∞ When to wash your hands ∞ ∞ ∞ ∞ ∞ ∞ ∞ ∞ ∞ ∞ ∞ ∞ ∞ ∞ ∞ Wet hands Keeping hands lower than elbows, apply soap Wash for at least 15 seconds, working up a lather Cover all surfaces of hand, pay close attention to under and around fingernails and the webbing in between the fingers Rinse well under running water Pat dry hands with a paper towel. Don’t rub! Turn faucet off with paper towel Before starting work ∞ Before and after touching a patient Before and after handling a patient’s equipment ∞ Whenever hands are visibly soiled ∞ Between handling patients Before performing any invasive procedures ∞ Before giving medications Before and after wearing gloves Alcohol hand wash After personal use of the toilet After blowing or wiping nose ∞ Preferred method of hand hygiene. Before and after eating ∞ Apply alcohol based hand rinse Before preparing food ∞ Rub vigorously, covering all parts of hand Before going home – in and around the fingernails and the AND when in doubt webbing in between fingers ∞ Allow to air dry. Do not towel or dry off ∞ DO NOT USE WHEN HANDLING STOOL SPECIMENS OR CARING FOR PATIENTS WITH DIARRHEA, especially C. Difficile Hand Care ∞ ∞ Sharps Safety 23 Hand lotion provided by the hospital may be used. DO NOT USE HAND LOTION FROM HOME; IT IS NOT COMPATIBLE WITH GLOVES AND ANTIMICROBIAL SOAP. Did you know? AMH hospitals provide a wide variety of sharps safety devices to protect employees from accidental needle sticks and other sharps injuries Employees who use sharps are instructed about the safety features and are expected to use them properly Safety features must be activated after every use and before disposal Activated sharps safety devices must be disposed of by placing into rigid sharps containers Each facility has an Exposure Control Plan that explains how we plan and implement for prevention of exposure to blood and bloody body fluids. See the policy on the Intranet Sharps users are involved in evaluating and selecting safety engineered devices Sharps containers must be changed when ¾ full. Don’t wait! 24 Fit For Duty? Every hospital is a drug-free workplace. All employees must be free from the influence of drugs & alcohol at work. Employees who engage in the sale, use, possession, manufacturing, diversion, or transferring of illegal drugs or controlled substances will be subject to disciplinary action or termination. Employees who use alcohol during work hours, or who abuse prescription drugs, will also be subject to disciplinary action or termination, per our “Fitness for Duty” Policy. You must NOT drink alcohol or use drugs before coming to work. You must NOT be under the influence of drugs or alcohol while at work. TAKE CARE OF YOURSELF SO THAT YOU ARE FIT FOR DUTY AT ALL TIMES 1. 2. 3. 4. Get help with your personal problems Don’t drink alcohol frequently or in excess Don’t use illegal drugs Get enough food and sleep Call the Employee Assistance Program (EAP) for professional, confidential help 1-888-327-4827 25 Ergonomics Office Ergonomics Slouching, slumping or bending forward at the waist in a chair can lead to discomfort, fatigue and backache. Follow these guidelines to help prevent problems from occurring when sitting at your workstation. ∞ Monitor placed for eyes facing forward Top 1/3 of the screen at eye level with the Neck in neutral position. ∞ ∞ ∞ ∞ ∞ ∞ Wrists should be a natural extension of the forearm, not angled up or down Elbow relaxed, lower arm at approximately 90 degrees to upper arm Sit all the way back in the chair with your shoulders & back relaxed Hips, knees should be bent to 90 degrees Feet resting firmly on the floor Take mini-breaks every 30 to 60 minutes and frequently change position. Mini-breaks from 15 seconds to 3 minutes include alternating tasks such as a trip to the copier or standing and stretching or rolling head & shoulders. 26 Safe Patient Handling THINK IT THROUGH ∞ ∞ ∞ USE GOOD FORM Assess the patient’s ability to participate Clear away obstacles o Get help as needed: o slide boards o draw sheet o trapeze o CO-WORKER Use good form ∞ ∞ ∞ DON'T Push a carrier, cart or wheelchair. You can push twice as much without back strain as you can pull Stay close to the cart or wheelchair Use both arms and tighten your stomach muscles DO DON’T *********************** USE GOOD FORM ∞ ∞ ∞ ∞ ∞ ∞ Always lock wheelchairs, carriers and beds Position height of bed at elbow level of caregivers or same height as the carrier Ask the patient to assist if possible Use both arms and tighten your stomach muscles Keep your head up and back aligned. A forward bend to lift can put 1000 pounds of pressure on your lumbar (lower) spine Tighten your stomach muscles and pull on the draw sheet to move the patient to a carrier 27 DON'T STRAIN DO GET HELP Safe Lifting Basics USE GOOD FORM ∞ ∞ ∞ ∞ ∞ ∞ ∞ DO Keep back straight Bend your legs at hips & knees Tighten stomach muscles Keep object closer to body Use smooth, controlled movements Avoid twisting & jerking Avoid overhead lifting. Use approved stool or ladder DO DON’T 28 DON'T DO DON'T 29 DO Corporate Compliance Tips for Protecting Patient Privacy As healthcare workers we are stewards of PHI. PHI is “Protected Health Information”. PHI is any information that we receive or create about our patients that could (alone or in combination) identify who the patient is. You may access PHI only as you needed to do your job. You may disclose PHI only as needed to support the patient’s treatment or payment for services. 1. Know your Minimum Necessary Standard. This describes what PHI you may access, use and disclose as you do your job. If you don’t know your Minimum Necessary Standard, ask your manager or contact the Privacy Officer, Anne Herman at (630) 856.4572. 2. Monitor your Conversations. Patient information may only be discussed with those who have a need to know. If you are having a discussion about a patient with others who have a need to know, make sure it is in a private area, where it will not be overheard. 3. Manage Your Password: If you have access to PHI that is in computer systems, make sure you have your own unique password. Never, never, never share your password! 4. Manage Your Work Documents: PHI is everywhere; in medical records, on surgery schedules, on lab reports and “to do” lists. Take perfect care of any PHI in your possession; making sure it is secured and available only to those who have a need to know. 5. Manage Your Workstation: If you have a computer to do your job, make sure you complete: 1. Log off whenever you leave your workstation 2. Have operational screensavers that work. 3. Face monitors away from public traffic 6. Dispose of PHI in shredding bins: Located throughout your facility. Please make sure to use these bins to dispose of all confidential information. Respect your Coworkers’ Privacy: Employees have the same right to patient privacy as any patient who receives care. If you see a coworker receiving care, you can acknowledge that employee with a nod or a “hello”. Please remember that, unless you are supporting the care for that patient, you have no right to access or disclose ANY information about their visit. 30 Language Interpretation Language and Culture impact the health care experience. Our “duty to serve” crosses all cultures, religions, and languages. If you encounter a patient who does not reliably speak or understand English, you have a duty to offer the patient free interpreter services during critical communications. This includes individuals who are hearing impaired or who have a primary language other than English. Work with your manager to arrange for an interpreter, as needed. We have employees who are trained interpreters in addition to having contracted interpreter, and telephone interpretation via use of the Language Line. Below are tips for effective use of an interpreter for patients who do not speak or understand English reliably: TIPS For Effective Use of An Interpreter Brief the Interpreter: Identify who you are and the objective of the interpretation session. Speak Directly to the Patient: All communication should be directed to the patient, not the interpreter. Segments: Speak in one or two short sentences at a time. Pause to allow the interpreter to deliver the message. Ask Patient if they Understand: Inquire periodically to assure the patient has understood the message. Do Not Ask the Interpreter’s Opinion: The interpreter’s job is to relay meaning without a personal opinion. Reading Script: When reading prepared text or documents, slow down to give the interpreter time to keep up. Everything You Say will be Interpreted: The interpreter’s job is to relay your entire message to the patient. Do not relay information unless it is intended for interpretation. Avoid Jargon or Technical Terms: Clarify any potentially confusing technical terms as you speak. There is often not a 1:1 correlation between technical terms in English and in another language. Avoid Interrupting the Interpreter: The interpretation may be of greater length (more words) than your English message. Many concepts have no equivalent in another language. Give the interpreter time to provide the message to the patient. Culture: The interpreter may point out a cultural issue and ask you to rephrase if they believe a particular question is culturally inappropriate. 31 Celebrating Cultural Diversity DuPage and Cook County are home to a rapidly growing number of immigrants. There are many cultures represented in our workplace. The identity, values, and beliefs of both your coworkers and patients may differ from your own because of their cultural background. Culture shapes the way we think about illness and death, parenting, religion, pain, authority and work. We need to be more aware of our coworkers’ and patients’ cultural codes. We need to be more sensitive to our coworkers’ and patients’ cultural codes. Here are some best first steps: ∞ Establish and build relationships with your patients and coworkers ∞ Work to understand your own cultural code (what beliefs and values do you hold close)? ∞ Be respectful of cultural differences. ∞ Respect the appropriate level of formality in other cultures. ∞ Speak at a comfortable pace for your coworkers and patients who have a different primary language. Seek the assistance of an interpreter for those patients in need. ∞ Check yourself constantly for cultural assumptions. Reference books are available in many departments and in the library on various cultural differences and practices. Celebrate, respect, and integrate this knowledge into your interactions with them! 32 S.H.A.R.E. SHARE is an acronym representing the five points of our Adventist Health System customer service initiative. SHARE is deeply rooted in our organization's mission and vision. At the corporate level, our mission is "To extend the healing ministry of Christ." Within Adventist Midwest Health we have defined our Mission as: "Adventist Midwest Health is a Christian Healthcare leader committed to partnering with physicians and our community to provide whole person care and to promote wellness." Adventist Midwest Health's core values are: excellence, Christian service motivation, stewardship, integrity, and acceptance. SHARE is: SENSE people's needs before they ask HELP each other out ACKNOWLEDGE people's feelings RESPECT the dignity and privacy of others EXPLAIN what's happening SENSE: Sensing people's needs is about understanding the dynamics of where we work - in a hospital setting - and using what we already know about our patient's situation to take action to seek to meet their needs before they have to ask us. This SHARE behavior is about taking the initiative and about taking action. HELP: Helping each other out is about team. It is about being a team where anyone can feel free to stop any process at any time if they think something is unsafe or not in the patient's best interest. It is also about helping my co-workers. We all need a little help at times and it is always a boost to know there are people you can count on to help us when we need it. We (the staff) are many people (along with the patient and their loved ones) who make up the interdisciplinary team bringing our best to the table to help make our patients well, to bring about healing experiences. ACKNOWLEDGE: Acknowledging others is about empathy. Walk a mile in their shoes. We may not have experienced exactly what our patient is going through, but it will help us understand why they are having such a difficult time if we can empathize with them and where they are at in their journey. RESPECT: Respecting the dignity and privacy of others is about courtesy. It is about treating others the way we would want to be treated - regardless of how different they might be from us. It is about protecting their rights to privacy as they come to us in their time of greatest need. 33 EXPLAIN: Explaining what's happening is all about communication. This is the toughest job. We are all so different and it is so critical that we understand each other. So much of communication is non-verbal. Many times our actions speak louder than words. Do your part to make sure communications are appropriate and correct. 34