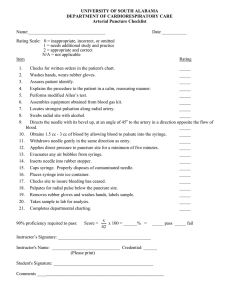
SKILLS REFERENCE and COMPETENCIES BOOK
advertisement

1 Medic to Practical Nursing SKILLS REFERENCE and COMPETENCIES BOOK 2015-2016 THIS BOOK BELONGS TO: _________________________________________________ 2 Medic to PN Certificate NURSING PROGRAM I have received my copy of the “Nursing Skills Reference and Competencies Book” and will become familiar with its contents. The requirements and guidelines as stated are acceptable to me and will provide information for completing skills demonstrations while in this program. I understand that failure to abide by the contents in this book may result in disciplinary action and/or my failing the Medic to PN Certificate Program. ____________________________________ Print Name ____________________________________ Signature ____________________________________ Student ID ____________________________________ Date 3 PRACTICAL NURSING SKILLS Head-to-Toe Physical Assessment Female Cath Administering a Nasogastric Tube Feeding Administering Meds via Nasogastric Tube Colostomy Care Non-sterile Dressing Change Open Sterile Pack/Add Sterile Items Hand Washing Administering Oral Meds Administering Intramuscular (IM) Injection Administering Meds from Ampule Administering Subcutaneous Injection Administering Meds from Vial Administer Medication by Suppository Female Cath Male Cath Tracheostomy Care Tracheostomy Suctioning NG Tube Insertion Sterile Dressing Suture and Skin Staple Removal Hand Washing IV Equipment Set-Up Care for and Monitor a Peripheral IV Site Discontinue an IV Z-Track Method of IM Injection Mixing and Administering Insulin Peripheral Venipuncture with Over the Needle Cath Insertion 4 TABLE OF CONTENTS Adult Head-to-Toe Physical Assessment .................................................................... 6-18 Blood Glucose Testing .............................................................................................. 19-20 Hand Washing ........................................................................................................... 21-28 Sterile Gloves ............................................................................................................ 29-30 Suture and Skin Staple Removal ............................................................................... 31-32 Opening Sterile Packages and Adding Sterile Items to the Sterile Field .................. 33-34 Non-Sterile Dressing Change .................................................................................... 35-36 Sterile Dressing Change ............................................................................................ 37-39 Pulse Oximeter ............................................................................................................... 40 Female Catheterization ............................................................................................ 41-44 Male Catheterization ................................................................................................. 45-48 Catheter Management................................................................................................ 49-51 Catheter Irrigation ..................................................................................................... 52-53 Catheter Removal ...................................................................................................... 54-57 Care for and Monitor a Peripheral IV Site ..................................................................... 58 IV Equipment Set-up ................................................................................................. 59-60 Discontinuing an IV ....................................................................................................... 61 Saline Lock Flush ...................................................................................................... 62-63 Administering IV Push Medication (Existing Line & Saline Lock) ......................... 64-66 Administering IV Meds by Secondary Set (IVPB) ................................................... 67-69 Giving Meds through a Central Venous Catheter ..................................................... 70-71 Central Line Site Care and Dressing Change ............................................................ 72-74 Peripheral Venipuncture with Over-the-Needle Catheter Insertion .......................... 75-80 Mixing and Administering Insulin ........................................................................ 81-82 Administering Subcutaneous Medications ................................................................ 82-86 Administering IM Injections to an Adult .................................................................. 87-91 Z-Track Method of IM Administration ..................................................................... 92-93 Administering Oral Medications ............................................................................... 94-96 Preparing an Injectable Medication from an Ampule ............................................... 97-98 Preparing an Injectable Medication from a Vial ..................................................... 99-100 Inserting a Nasogastric Tube ................................................................................. 101-103 Irrigating a Nasogastric Tube ................................................................................ 104-105 Removing a Nasogastric Tube .............................................................................. 106-107 Administering a Tube Feeding .............................................................................. 108-110 Administering Medications via a Nasogastric Tube ............................................. 111-112 Changing and Emptying an Ostomy Appliance .................................................... 113-115 Irrigating a Colostomy........................................................................................... 116-117 Administering Medication by Suppository……………………………………….118-119 Tracheostomy Care................................................................................................ 120-124 Tracheostomy Suctioning ...................................................................................... 125-127 5 GENERAL STEPS With almost every demonstration, there are eight initial general steps and five closing general steps. These are listed below. The student will be expected to include these when they are performing the skill demonstration and to explain any specific information related to them in a particular demonstration. INITIAL GENERAL STEPS 1. Check the physician’s order. When this is a new order. If it is not clearly stated on the worksheet. If you have any questions concerning a procedure for a particular client. 2. Wash hands. 3. Gather needed equipment. 4. Respect client’s privacy by knocking on door or requesting permission to enter. 5. Introduce self to client unless already done so. Address client in a respectful manner, using the name the client prefers. 6. Identify client, preferably using identification band: Have client state name and birth date. Ask family or regular staff to identify client. Utilize picture ID used by facility. 7. Explain procedure to client. Take into consideration the previous experience of the client with this procedure, the level of understanding and any communication deficits such as language barriers, hearing loss, or confused state. 8. Provide for privacy by drawing curtains or closing the door of the room. CLOSING GENERAL STEPS 1. Remove gloves, if used, and wash hands. 2. Make sure client is safe and comfortable by: Readjusting clothing and coverings to provide privacy and warmth. Positioning in chair or bed in a comfortable position. Returning bed to lowest position. Making sure side rails are up and wheels are locked. Placing call signal within reach of the client. 3. Straighten room and remove any soiled items to the appropriate place. 4. Record information regarding the specific procedure. 5. Demonstrate an ability to give appropriate rationale for any step in the demonstration when requested to do so by the instructor. 6 Adult Head-to-Toe Physical Assessment Performance Comments Satisfactory Unsatisfactory Time needed: 30 minutes Supplies needed: Stethoscope and blood pressure cuff Patient gown Alcohol wipes Penlight Other: Partner needed 1. Wash hands. 2. Bring equipment to room. Client in hospital gown. 3. Introduce self and identify client by asking them to state their name and checking their wrist band. 4. Explain procedures (going to be checking their pulse, lungs, etc.) now and throughout the assessment. 5. Provide for privacy. Keep the client covered during the procedure exposing only areas being examined. 6. Prior to the start of the return demonstration, the student will be sure the client is dressed in a patient gown and will collect the following vital sign information: 7. A. client’s lying, sitting, and standing B/P B. temperature, radial pulse and respiration Elevate bed to working height. COGNITIVE AND SENSORY ASSESSMENT 8. General Appearance and Behavior A. Are the client’s actions and responses to questions as you would expect (appropriate) or are they inappropriate? B. Identify the client’s predominant emotion or feeling (i.e., examples of “mood” could be 7 Performance Comments Satisfactory Unsatisfactory happy, sad, depressed, fearful, etc.). C. Assess typical dress and grooming. NOTE: Is clothing clean? Body odor? Grooming? COGNITIVE FUNCTION AND THOUGHT PROCESSES 9. Cognitive Function and Thought Processes A. Is client Awake and Alert? Understands questions and responds appropriately and reasonably quickly? B. State if client does not respond to question. Proceed with the following – noting both the stimulus required to elicit a response from the client and the specific type of response to the stimulus. (If client responds to 1, you would not need to proceed to 2, 3, 4, or 5). 1) Instruct client to do something (i.e., squeeze my hand or open your eyes.) 2) Does client respond to his name? 3) Does client respond to touching of an extremity? 4) Does client respond to shaking of shoulder? 5) Does client respond to nail bed pressure (pain)? C. 3 Spheres of Orientation: Ask: 1) Person: What is your name: 2) Place: Where are you? 3) Time: What is the date or day and what time is it? 8 Performance Comments Satisfactory Unsatisfactory D. Memory 1) Long-term memory: (distant past) Ex: Where did you go to school? Where born? 2) Short-term memory: (last 24 hours) Ex: What did you have for breakfast? 3) Immediate recall: Is client able to repeat a series of 4 or 5 numbers or words unrelated to each other? E. Cranial Nerves (Eyes and Ears) 1) Hearing A) Ask if he/she has hearing problems or hearing aid. B) Assess speech. Speaking loudly? C) Assess hearing by occluding one ear by pressing inward on the tragus and speak. Have client repeat it. Then, repeat with the other ear. 2) Vision A) Check if wears glasses. If so, do they correct vision? Have them read small print, covering one eye than the other. B) If cannot read print, have them cover one eye and hold up 2 fingers and ask how many fingers are held up. 3) Pupil Response Assess pupils by shining penlight into one eye and then the other. Check for: A) Size B) Shape C) Equality 9 Performance Comments Satisfactory Unsatisfactory D) Reaction to light E) Symmetry to reaction to light (check one eye and then other to see if same amount of reaction). 10. 11. Neck Assessment: Carotid Pulses A. Use the pads of the index and 2 middle fingers for palpation of pulses. B. Palpate the carotid arteries (one at a time). Slide index and middle fingers around the medial edge of the sternocleidomastoid muscle to locate artery (toward the trachea). Ask client to turn head toward side examined Never vigorously palpate or massage a carotid artery. Chest Assessment: (Cardiac and Respiratory) Ask client to sit on side of bed or raise bed to sitting. Face client to assess the anterior chest. Ask the client if he/she is having any difficulty breathing, any cough, or any sputum production. A. Inspection: (expose upper chest and observe) Inspect for shape: 1) Retraction/bulging of intercostals spaces 2) Presence of masses/deformities 3) Equal chest expansion B. Palpation Feel all of anterior upper chest with fingers flat against skin moving in circular motion. Feel for: 1) Masses/deformities 2) Equal chest expansion 3) Tenderness (ask if touching hurts) 10 Performance Comments Satisfactory Unsatisfactory C. Auscultation: (With stethoscope, listen for heart and lung sounds.) Expose only as needed. 1) Finding Anterior Land Marks A) Locate the angel of Louis and 2nd intercostals space to the left of the sternum. B) Count down the intercostals spaces to locate the 5th intercostal space. C) Slide finger along the 5th space to the mid-clavicular line. D) Identify that: the apex of the heart, where the APICAL PULSE is located, is at approximately the 5th rib at the mid-clavicular line. 2) Apical Pulse: Ask client to breathe normally and to refrain from speaking during listening period. A) Auscultate the apical pulse for one full minute. The instructor will check the radial pulse at the same time. Student’s reading must be within 4 beats of the instructor’s reading. B) State: The S1 is the first heart sound (lub) and the S2 is the second heart sound (dub). Assess the beat for strength and rhythm. 3) Auscultate Anterior Lung Sounds A) Auscultate and listen for one full inspiration and expiration at each lung location. B) Compare breath sound characteristics of both lungs. 11 Performance Comments Satisfactory Unsatisfactory C) During auscultation, direct client to: i. turn and face opposite nurse ii. breath normally with open mouth iii. if unable to hear breath sounds, ask client to take deeper breaths iv. refrain from talking during assessment v. instruct to tell you if they get dizzy or tired D) Do not auscultate over bone or clothing. Follow sequence as shown in picture: 1. Above clavicle 2. @ 2nd intercostal L-sternal boarder 3. @ 4th intercostal L-sternal boarder 4. @ 6th intercostal mid-clavicular line E). Cover client anteriorly and positions client facing away. (Or examiner can go to other side of bed). Expose the posterior chest. 4) Find Posterior Land Marks A) Locate 7th cervical spinous process (ask client to flex neck so this is easier to locate). B) Palpate each spinous process down to the 10th and 12th thoracic spinous process. 12 Performance Comments Satisfactory Unsatisfactory NOTE: The lower boarder of the lungs is at the level of the 10th spinous process on expiration and descends to the 12th spinous process on inspiration. 5) Auscultate Posterior Lung Sounds A) Auscultate and listen for one full inspiration and expiration at each lung location. B) Compare breath sound characteristics of both lungs. C) Follow sequence as shown in picture: 6) After auscultating lung bases, locate the Lateral Lung Boarder. Follow the 10th intercostals space around the side of the (mid-axillary line) and count up to 2 ribs to the 8th intercostals space. The inferior boarder of the lungs laterally is approximately at the level of the 8th rib at the mid-axillary line. 12. GU: Any hesitancy, frequency, burning, pain with urination or change in urinary pattern? 13. Abdominal Assessment: (GI Assessment) (Have client lie supine and expose the abdomen from the lower costal margin to the super-pubic region). 13 Performance Comments Satisfactory Unsatisfactory Ask the client when their last bowel movement was. Any changes in bowel habits? A. Landmark Abdomen: (4 quadrants) Visualize a vertical line and a horizontal line crossing the umbilicus. Name the 4 quadrants: ULQ – Upper Left Quadrants (on the client’s side) URQ – Upper Right Quadrant LLQ – Lower Left Quadrant LRQ – Lower Right Quadrant B. Inspection: Observe from both sides and foot of the bed at eye level for: i. shape (rounded, conclave, or flat) ii. masses/deformities iii. peristaltic movement C. Auscultation: (NOTE: Auscultation is done prior to palpation to prevent increased bowel sounds caused by palpation). Listen in all 4 quadrants until a bowel sound is heard in each quadrant. *Must listen for a full 5 minutes before stating, “No bowel sounds.” D. Palpation: Light palpation of all areas of the abdomen. Using pads of the fingers, palpate no more than 1 inch deep, feeling for lumps or masses. Ask if there is any tenderness. NOTE: No palpation is done on any client with undiagnosed abdominal pain. 14. Peripheral Pulses & Circulation Use the pads of the index and middle fingers for palpation of pulses (total of 3 fingers). A. Upper Extremities 14 Performance Comments Satisfactory Unsatisfactory 1) Radial Pulses: Locate radial artery on the radial (thumb side) of the wrist. Feel both right and left at the same time to compare for symmetry. NOTE: On actual client, if radial pulses are present, you would not need to check any more proximal pulses. For demonstration purposes, you will need to show location of all upper extremity pulses on one arm. B. 2) Ulnar Pulse: Locate ulnar artery on the opposite side of the wrist. 3) Brachial Pulse: Locate the brachial artery by finding the groove between the biceps and triceps muscle above the elbow at the anticubital fossa. 4) Inspects and palpates for circulation comparing for equality with the opposite extremity: a. nail bed and skin color b. temperature c. capillary refill d. presence of edema e. characteristics of the most distal pulse Lower Extremities 1) Dorsalis Pedis (PEDAL) Pulses: Locate pedal pulse by placing fingertips between the great and first toe and slowly inching up the foot until the pulse is palpable. Feel both right and left at the same time to compare for symmetry. NOTE: On actual client, if pedal pulses are present, you would not need to check any more proximal pulses. For demonstration purposes, you will need 15 Performance Comments Satisfactory Unsatisfactory to show location of all lower extremity pulses on one leg. 2) Posterior Tibial Pulse: Locate artery by placing fingers behind and below the medial malleolus on the inner aspect of the ankle. (Cup fingers over ankle bone pointing finger tips toward the heel.) 3) Popliteal Pulse: Locate artery behind the knee. Palpate with index and middle fingers of both hands deeply into the popliteal fossa just lateral to the mid area of the knee. Ask client to keep leg relaxed as you lift knee to slightly flex it. 4) Femoral Pulse: Expose inguinal area. Locate artery midway between the anterior superior iliac spine and the symphysis pubis. (Student can demonstrate the position to them self during return demo). 5) Inspect and palpate pulses and compare the following for equality with the opposite extremity for: A) nail bed and skin color B) temperature C) capillary refill D) presence of edema E) characteristics of the most distal pulse 15. Sensory Function Assessment To assess sensory function (feeling), do the following: Ask the client if they have numbness, tingling, or decreased ability to feel on any part of their body. If so, identify the area and its boundaries. 16 Performance Comments Satisfactory Unsatisfactory 16. Motor Function A. B. Assess ROJM as follows: 1) Ask the client to move each extremity through the normal range of joint motion. Model each movement for the client. First arms, then legs. 2) If client is unable to do this independently, assess ROJM passively. Assess Muscle Strength Test by asking client to move actively against your resistance or to resist your movement. Compare symmetrical areas. 1) Upper Extremities A) At the elbow, test flexion and extension by having the client pull and push against your hand. B) To test grip, ask the client to squeeze 2 of your fingers. (Do both hands simultaneously). Use the index and middle fingers with the middle fingers atop the index fingers. 2) Lower Extremities A) While client is in sitting position, test flexion and extension. Have client push both legs forward against examiner’s hands and pull lower legs back as the examiner tries to pull them forward. B) At the ankle, test dorsiflexion, and plantar flexion by asking the client to pull up and push down against your hand. 17 Performance Comments Satisfactory Unsatisfactory C. Posture 1) Check current activity orders and if the client is allowed out of bed, assist to the standing position. Open gown and visualize the client’s spine. A) From the side, inspect the spinal profile noting the cervical, thoracic, and lumbar curves. B) From behind, inspect for lateral curves. Check for any differences in the shoulder height, the iliac crests, and the skin creases below the buttocks. D. 17. Assess Gait 1) Determine the client has an activity order to ambulate. If so, determine if client needs assistance (1 or 2 persons) or any equipment (cane, crutches, or walker). If needed, provide the assistance/equipment needed. 2) Have client walk and assess the gait observing for balance, leg movement, and arm movement. Cover the client and assist them to a comfortable position. 18. Make sure the bed is in low position, the side rails are up, and the client has the call light. 19. Document the findings accurately on the appropriate section of the database tool which is copied on this form. (See the following page.) 20. Be able to explain the rationale for any step of the procedure as requested by the instructor. 18 Adult Head-to-Toe Physical Assessment Worksheet (This worksheet may be used during the Adult Head-to-Toe Physical Assessment Return Demo) Objective: Distinguish between normal and abnormal. Cognitive & Sensory Assessment Cardiac Assessment (Chest Assessment) Respiratory Assessment GU Abdominal Assessment Peripheral Pulses & Circulation Sensory Function Assessment Motor Function General Appearance ______________ Behavior _______________________ Awake & Alert __________________ Orientation _____________________ Memory_______________________ Hearing________________________ Vision ________________________ Pupil Response__________________ Carotid Pulse____________________ Inspection ______________________ Palpation _______________________ Apical Pulse ____________________ Inspection ______________________ (If not completed with the Cardiac) Palpation _______________________ Anterior Lung Sounds _____________ Posterior Lung Sounds _____________ Ask _____________________________ Ask ____________________________ Inspection ______________________ Auscultation ____________________ Palpation _______________________ Ask ____________________________ Radial __________________________ Nail bed_______________________ Ulnar __________________________ Temperature____________________ Pedal __________________________ Cap. Refill _____________________ Posterior Tibial __________________ Edema ________________________ Popliteal _______________________ Femoral _______________________ Characteristic of the most distal pulse ________________________________ Numbness/Tingling _______________ ROM _________________________ Posture ________________________ Gait ___________________________ (Revised 07/12) 19 Blood Glucose Testing Performance Comments Satisfactory Unsatisfactory Time needed: 30 minutes Supplies needed: Blood glucose monitor Lancet Test strips Cotton balls Alcohol wipe Clean disposable gloves Clean gauze (2x2) and Band-Aid (if needed) 1. Verify order, ID patient using two forms of identification and provide for privacy. 2. Turn on glucose monitor and press “continue.” 3. Enter your operator ID. 4. Select “Patient Test.” 5. Enter the patient’s ID number or scan the patient’s bar code on their identification bracelet. 6. Select the test strip lot number or code on the monitor screen to match the number/code on the test strip bottle. You may need to scan the test strips. 7 Apply disposable gloves. 8. Select a puncture site. For fingers, the lateral aspect at the level of the nail bed is optimal. Avoid areas of bruising, callouses, or multiple puncture sites. 9. Cleanse the site with an alcohol wipe. Allow area to dry or wipe with a cotton ball or 2x2 gauze. 10. Insert test strip into slot on glucose monitor. Read results after monitor counts down. 11. Use the lancet to puncture the chosen site. Apply a large drop of blood to the test strip pad. Do not add a second drop. Some meters may require for you to insert test strip into slot on glucose monitor first before using the lancet to puncture chosen site. (See Blood Application picture on following page.) 20 Performance Comments Satisfactory Unsatisfactory 12. Dispose lancet device in sharps container. Discard test strip and cotton ball or 2x2 gauze in trash container. 13. Assure puncture site is no longer bleeding. 14. Document reading in patient’s chart, along with any actions taken for abnormal readings. 21 Hand Washing Performance Comments Satisfactory Unsatisfactory Time needed: 5 minutes Supplies needed: Water Soap Paper towels Hand Washing (with non-antiseptic soap) and Antiseptic Hand Wash (soap contains antiseptic agent) 1. Use technique when hands visibly soiled, before eating, and after using the restroom. 2. Stand away from sink so as not to touch sink. 3. Turn on faucet to have warm (not hot) water. 4. Wet hands and wrists with water. 5. Keep fingers pointing down during hand washing to prevent contaminating arms. 6. Apply liquid soap. If you have to use bar soap, rinse before applying. 7. Rub hands together for at least 15 seconds covering all surfaces of hands, fingers, and wrists. May extend hand washing if indicated. 8. Clean under your fingernails. 9. Rinse hands and wrists under running water keeping fingers pointed downward (water should flow from wrists to hands). 10. Dry hands and wrists thoroughly by using single paper towels wiping in the direction from finger tips to wrists. Dispose of each paper towel after reaching the wrist. Do not return to the fingers with a used paper towel. (Will use multiple paper towels). 11. Use a new clean and dry paper towel to turn off faucets. 22 Performance Comments Satisfactory Unsatisfactory 12. Repeat procedure at step 4 if your hands touch the anytime between step 4 and 10. Hand rubs: Use of a waterless antiseptic agent containing alcohol to decontaminate hands. 1. Use technique before and after direct patient contact, after removing gloves, and after contact with bodily fluids or excretions, mucous membranes and would dressings, provided hands are not visibly soiled. 2. Apply agent to palm of one hand. (Use volume of agent recommended by the manufacturer.) 3. Rub hands together covering all surfaces including sides of hands and fingers. 4. Continue rubbing until all surfaces are DRY. 5. Do not use paper or cloth towels in conjunction with waterless antiseptic agents. 23 24 25 26 27 28 29 Sterile Gloves Performance Comments Satisfactory Unsatisfactory Time needed: 5 minutes Supplies needed: Sterile Gloves (in student nursing kit) 1. Application of sterile gloves A. Wash hands thoroughly. B. Follow principles of surgical asepsis during all movements. C. Place glove package on a clean, dry, firm surface at waist length. D. Remove outer package wrapper by peeling sides apart. E. Grasp inner package and lays it on a clean flat surface. F. Open the package. Keep gloves on the wrapper’s inside surface. G. Identify the right and left glove. H. Glove the dominant hand. I. With the thumb and first two fingers of the non-dominant hand, grasp the edge of the cuff of the glove for the dominant hand. Touch only the inside surface of the glove and keep finger pointed downward. J. Move back and away from the sterile field and keep sterile glove above the waist and in view at all times. K Pull the glove over the dominant hand. L. With gloved dominant hand, slip the finger underneath the second glove’s cuff. 30 Performance Comments Satisfactory Unsatisfactory 2. M. Pull the second glove over the nondominant hand. Do not let any part of the gloved hand touch the ungloved hand. Keep thumb of dominant hand abducted back. N. Keep both sterile gloves in front of you above waist level. Removal of contaminated gloves A. Grasp outside cuff of one gloved hand without touching any bare skin. B. Peel glove off, turning it inside out and discard glove in receptacle. C. Tuck 2 fingers of bare hand inside the remaining glove’s cuff without touching the contaminated portion of the glove. D. Peel glove off, turning it inside out and discard glove in receptacle. 3. Wash hands. 4. Explain rationale for any step of the procedure as requested by instructor. 31 Suture and Skin Staple Removal Performance Comments Satisfactory Unsatisfactory Time needed: 10 minutes Supplies needed: Suture removal kit Skin staple remover Clean gloves Biohazard bag Material to cleanse wound 4 x 4 with at least 5 interrupted sutures 4 x 4 with a least 5 staples 1. Check for doctor’s order to remove sutures or skin staples. 2. Gather equipment. 3. Implement Initial General Steps. 4. Put on gloves, remove and discard any dressing. Remove and discard gloves. 5. Wash hands. 6. Observe wound characteristics. 7. Suture Removal A. Open disposable suture removal kit. B. Put on clean gloves. C. Pick up suture scissors with dominant hand. D. Place curved tip of suture scissors under suture, next to the knot. E. Cut suture and with forceps pull suture through skin with one movement. (Refer to figure on next page.) 32 Performance Comments Satisfactory Unsatisfactory NOTE: Remove every other interrupted suture. Check incision line for gaping. If the edges remain approximated, remove the rest of the sutures. 8. Discard suture material in biohazard bag. Dispose of forceps and scissors in sharps container. 9. Skin Staple Removal A. Put on clean gloves. B. Obtain disposable staple remover. C. Place staple remover under the staple and pinch down to exert pressure on its center. (This motion raised the ends of the staple, allowing it to be easily removed.) NOTE: Remove every other staple. Check incision line for gaping. If the edges remain approximated, remove the rest of the sutures. 10. Discard staples and disposable staple remover in sharps container. 11. Observe the appearance of the wound; approximation of the edges, presence of inflammation and edema, and appearance of any drainage. 12. Clean wound, redress as ordered. Remove and discard gloves. 13. Document the procedure, observations of the wound, and patient tolerance. 33 Opening Sterile Packages and Adding Sterile Items to the Sterile Field Performance Comments Satisfactory Unsatisfactory Time needed: 5 minutes Supplies needed: Sterile package with four flaps for sterile field Sterile item enclosed in package with 1 flap Sterile item enclosed in package with 2 peel back (i.e., 2 x 2 dressing) 1. Gather equipment. 2. Demonstrate principles of surgical asepsis during all movements. 3. Establish sterile field. To open items packaged in linen and commercially packaged items with four flaps, the nurse: A. Removes any type or seal indicating sterilization date. B. Grasps the outer surface of the tip of the outermost flap. C. Opens the flap away from the body. D. Keeps the arm outstretched and away and away from the sterile field. E. Grasps the outside surface of the first side flap. F. Opens the side flap, allowing it to lie flat on the table surface. Keeps arm to side and not over sterile field. G. Repeats steps E and F for remaining flaps. 4. Sterile items are now added to the sterile field. 5. To open commercially packaged sterile items enclosed in a wrapper with one flap and add this item to the sterile field, the nurse: 34 Performance Comments Satisfactory Unsatisfactory A. grasps the flap by the unsealed corner and pulls flap away from self. B. positions the pack so the open end faces the sterile field. C. holds open pack to the side of the sterile field and about 6 inches above it. D. allows contents to drop within sterile field. 6. 7. To open commercially packaged sterile items enclosed in a wrapper with two peel back flaps and add this item to the sterile field, the nurse: A. Grasps both flaps and gently pulls them apart. B. Holds package so open end is facing sterile field. C. Folds flaps back so the outside of the flaps cover hands. D. Holds package to the side of the sterile field and about 6 inches above it. E. Allows contents to drop within the sterile field. Explain rationale for any step of the procedure as requested by instructor. 35 Non-Sterile Dressing Change Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Clean, non-sterile dressing Non-sterile gloves Biohazard bag Appropriate screening to provide for privacy Sterile saline Materials to cleanse site of wound 1. Assemble equipment, knock on client’s door, introduce self and identify the client by checking the arm bracelet or using facilityapproved and accepted method of identification. 2. Provide for privacy for the client. Explain procedure to client. 3. Wash hands. Put on non-sterile gloves. Grasp old dressing with covered hand and pull off dressing. Turn covering inside-out over the old dressing. 4. Ensure proper disposal of old dressing following agency protocol. Arrange supplies. 5. Cleanse the wound. Sterile saline is the cleansing agent of choice. Topical antiseptics (i.e., povidone-iodine, hexachlorophene, alcohol or boric acid) may be used on intact skin surrounding the wound but should never be used within the wound or if allergy is noted to any of these products. 6. Allow skin to dry; prepare clean dressing. 7. Apply clean dressing to wound. 8. Remove any materials used to apply the nonsterile dressing, cleansing any items prior to storage. Discard non-sterile gloves according to facility policy and procedure. 36 Performance Comments Satisfactory Unsatisfactory 9. Ensure that client is in a comfortable and safe position. Leave call light, telephone and fresh water close at hand; return bed to lowest position; remove any screening used for privacy, wash hands. 10. Report and record any significant observations (i.e., wound size, color, drainage). 37 Sterile Dressing Change Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Sterile materials for dressing change Tape Sterile gloves Disposable gloves Biohazard bag Appropriate screening Sterile saline to loosen the dressing Sterile cleansing materials for the wound 1. Assemble equipment, knock on client’s door, introduce self and identify the client by checking the arm bracelet or using facilityapproved and accepted method of identification. 2. Provide for privacy for the client. Explain procedure to client. 3. Wash hands. 4. Use sterile technique and observe universal precautions during dressing change. 5. Remove the old/soiled dressing: A. Put on disposable gloves. B. Loosen dressing by removing tape from skin. Use care not to disturb wound closures or any newly formed tissue. C. Remove old/soiled dressing. Use sterile water or sterile saline to loosen the dressing, if needed. Do not moisten “wet to dry” dressings. D. Place old/soiled dressings in waterproof bag for disposal. 38 Performance Comments Satisfactory Unsatisfactory 6. Assess condition/characteristics of the wound: color, skin characteristics, presence of drainage, characteristics or any drainage, and security of wound closure. 7. Remove gloves. Establish safe, clean site for sterile dressing supplies. 8. Open sterile supplies and cleansing materials. 9. Put on gloves using sterile technique. 10. Cleanse the wound using supplies provided and observing the following principles: A. Cleanse from top to bottom of wound. B. Cleanse from center of wound to periphery of wound. C. Use cleansing items for one pass over the wound. D. Discard used cleansing items. E. Place materials used for cleansing in a moisture-proof bag. 11. Redress wound; apply smaller non-adhering dressing to wound followed by primary dressing designed to collect drainage. 12. Cover entire wound with secondary, larger dressing. 13. Remove gloves. Secure dressing with tape. 14. Remove any materials used to change the sterile dressing. Dispose of soiled/old dressings and materials following facility guidelines. 15. Ensure that client is in a safe and comfortable position. Leave call light, telephone and fresh water close at hand. Return bed to lowest position. Remove any screening used for privacy. 39 Performance Comments Satisfactory Unsatisfactory 16. Wash hands. 17. Report and record characteristics of the wound, amount and type of drainage and characteristics of skin surrounding the wound. 40 Pulse Oximeter Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Pulse Oximeter 1. Evaluate for presence of any factors which could interfere with accuracy of reading of arterial oxygen saturation levels including degree of light, client movement, temperature, blood pressure level and vasoconstriction and nail polish. (Remove dark nail polish.) 2. Read the monitor recording of oxygen saturation levels. 3. Protect the transducer from strong light. Check the skin with monitor placement for abrasion and vascular insufficiency. Compare pulse reading and client’s actual pulse and report any discrepancies. 4. Assess for adequacy of placement. Rotate the transducer every four hours to discourage skin impairment. 5. Ensure that client is in a comfortable and safe position. Leave call light, telephone and fresh water close at hand; return bed to lowest position; remove any screening used for privacy; remove soiled linens; wash hands. 6. Invite visitors to return to bedside. 7. Report readings as required by agency protocol. 8. Chart the following: A. Initial assessment findings that warrant use of oximeter. B. Subsequent respiratory assessments. C. Actual pulse oximeter readings. 41 Female Cath Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Catheter tray and drainage bag Velcro catheter strap Disposable gloves Wash cloth Soap & water Bath towel Bath blanket Source of extra light Two plastic bags Waste receptacle 1. Check for iodine allergy. Ask client about iodine allergy prior to procedure. 2. Provide for privacy and explain purpose of procedure. Explain steps of procedure as you do them. 3. Don clean gloves and wash perineum with soap and water, if necessary. 4. Remove gloves and wash hands. 5. Raise bed to working height. Place over bed table with equipment on it perpendicular to bed on dominant side. 6. Position client in dorsal recumbent position. Drape bath blanket in diamond fashion over client. Wrap one corner of blanket around each foot. Leave perineum covered. 7. Open sterile catheterization tray according to directions on package. Open package with four flaps, making sure not to reach over the sterile field and do not allow wrapper to hang over the sides of the over bed table. 8. Follow principles of surgical asepsis during all movements. Instruct client to keep hands folded on chest during procedure and to refrain from moving, if possible. 42 Performance Comments Satisfactory Unsatisfactory 9. Expose perineal area. If a second person is available, he or she may expose the perineal area. 10. Don sterile gloves. 11. Prepare items in catheter kit on overbed table before transferring the tray to the bed. A. Move sterile container close to your side of the field to avoid reaching over the field when preparing the items. B. Open antiseptic solution & simulate pouring contents over sterile cotton balls. Discard antiseptic solution package. When discarding items allow them to drop into a receptacle; remembering to keep sterile hand above the waist. C. Connect syringe to port. D. Simulate lubricating catheter tip (2-3 inches) without plugging drainage port and discard this package. 12. Pick up solid sterile drape, allow it to unfold, and allow top edge of drape to form a cuff over both hands. Ask the client to raise hips off of the bed and slip the cuffed edge just under the client's buttocks. Avoid contaminating gloves. 13. Place sterile catheter tray and tray with cotton balls on sterile drape between client's thighs. NOTE: If client is unable to remain still, keep sterile trays on over bed table and position within reach. 14. With non-dominant hand, retract labia outward and upward to fully expose the meatus. Maintain this position during the procedure. 15. With dominant hand, pick up a cotton ball with forceps and cleanse perineal area. Wipe from front to back, clitoris towards anus, in over meatus. Use a new sterile cotton ball for each wipe. Do not cross over the sterile tray discarding them. 43 Performance Comments Satisfactory Unsatisfactory 16. With dominant hand, pick up catheter about 2 inches from the tip. Make sure the catheter end is over the collection basin or attached to drainage bag. 17. Ask the client to take a deep breath and slowly insert catheter until urine appears (about 3 inches). If the catheter is inserted into the vagina, leave it in the vagina and insert another sterile catheter into the urinary meatus. Then, remove the first catheter from the vagina. 18. When urine appears, advance catheter another 2 to 3 inches. Do not force catheter against resistance. 19. Release labia and holds catheter with non-dominant hand about 1" from meatus. 20. Inject total amount of solution into port. If the client experiences pain, aspirate back solution and advance catheter farther. (Actually insert water into catheter with demonstration manikin). Maintain pressure on plunger of syringe until syringe is disconnected. 21. Pull gently on catheter to feel resistance. Move non-dominant hand to syringe part and disconnect syringe from catheter. 22. Obtain sterile urine specimen if ordered. 23. Utilize Velcro foley catheter strap to secure the catheter tubing to the client’s upper leg. If the catheter is secured to the right thigh, hang the bag on the right side of the bed frame. 24. Place excess coil of tubing on bed and fasten it to the bottom sheet with a clip. 25. Discard equipment. Cover the client, lower bed height, put the side rails up, and give the call light to the client. 26. Moisten wash cloth with warm water. Return to bedside. Cleanse and dry the perineum, remove gloves properly, and cover the client. 44 Performance Comments Satisfactory Unsatisfactory 27. Assist the client to a comfortable position. 28. Teach client as appropriate: A. the importance of fluids B. to keep the bag off of the floor and below the level of the bladder C. how to hold the catheter when walking D. the importance of keeping the tubing taped to the thigh E. not to lie on the tubing F. not to pull on the catheter G. to cleanse around the catheter site with soap and water daily 29. Tie knot in plastic bag and remove it from the waste receptacle. Place clean plastic bag in the receptacle. 30. Wash hands. 31. Discard plastic bag in dirty utility room. 32. Wash hands. 33. Chart – Utilizing Nursing Notes at end of booklet: A. Catheter size and balloon volume B. Amount and characteristics of urine obtained C. Catheter secured to leg with tap D. Connected to closed drainage system E. Client teaching done F. Client's response to the procedure 45 Male Catherization Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Catheter tray and drainage bag Wash cloth, soap, water, bath towel Bath blanket Source of extra light (flashlight, gooseneck lamp) Velcro catheter-strap Disposable gloves Sterile gloves Two plastic bags Waste receptacle 1. Check for iodine allergy. Ask client about iodine allergy prior to procedure. 2. Provide for privacy and explain purpose of procedure. Explain steps of procedure as you do them. 3. Don clean gloves and wash perineum with soap and water, if necessary. 4. Remove gloves and wash hands. 5. Follow sterile asepsis during procedure. 6. Put on clean gloves and wash penis with soap and water if necessary. If uncircumcised, retract foreskin to cleanse the urethral meatus. 7. Remove gloves and wash hands. 8. Raise bed to working height. 9. Place overbed table perpendicular to bed on dominant side and place equipment on table. 10. Position client in supine position. 11. Cover client’s upper trunk with bath blanket and covers lower extremities with the bed sheets. Places clean towel over perineum. 46 Performance Comments Satisfactory Unsatisfactory 12. Open sterile catheterization tray according to directions on package. Open package with four flaps, making sure not to reach over the sterile field and do not allow wrapper to hang over the sides of the over bed table. 13. Instruct client to keep his hands away from sterile field and to refrain from moving during procedure. 14. Expose perineal area. 15. Put on sterile gloves. 16. Lift sterile drapes out of catheterization tray and lay on sterile field (wrapper of tray). 17. Open antiseptic solution and simulate pouring contents over sterile cotton balls. 18. Connect syringe to port, and leave syringe connected to port. 19. Simulate lubricating catheter liberally for about 3-5 inches. 20. Position sterile drapes. A. Pick up solid drape by corner and allow it to unfold. Place over client’s thighs just below perineal area. B. Pick up fenestrated drape and allow it to unfold. Place hole over penis. 21. With non-dominant hand, retract the foreskin of the uncircumcised male. Firmly grasp the penis shaft just below the glans. 22. With dominant hand, pick up cotton ball with forceps and clean the glans. Move in a circular motion from the meatus around the glans down to the base of the glans. Repeat cleaning motion three to four more times using a new cotton ball each time. 47 Performance Comments Satisfactory Unsatisfactory 23. With dominant hand, pick up catheter 3-5 inches from tip, and avoid getting lubricant on gloves. (Lubricant is very slippery and may cause nurse to lose grip.) 24. Lift penis to a position perpendicular to client’s body and apply light traction. Instruct client to bear down as if to void and slowly insert catheter into meatus. 25. Make sure catheter end is over collection basin or attached to drainage bag. 26. Advance the catheter up to the “Y” at the port or until urine returns (at least 7-8 inches for an adult or 2-3 inches for a young child). 27. Advance catheter (1-2 inches, if possible) to allow for balloon to expand in bladder. Hold the catheter about 1” away from the meatus, with the non-dominant hand. 28. Inject solution into balloon through port. If client complains of discomfort, deflate balloon, advance catheter and then reinflate balloon. 29. Gently pull on catheter to feel resistance. (This determines that balloon has inflated sufficiently.) Maintain pressure on the plunger of syringe until the syringe is disconnected. 30. If urine is being collected in basin or drainage bag, note amount that has been obtained. Obtain urine specimen if ordered. 31. Attach bag to the side of the bed frame. 32. Utilize Velcro leg strap to secure the catheter tubing to the client’s upper leg. 33. Coils excess tubing on bed and fastens to bottom sheet with clip. 34. Teach client the following as appropriate: A. Why increasing fluid intake is important. 48 Performance Comments Satisfactory Unsatisfactory B. Keeping bag off the floor and below bladder level. C. How to hold catheter when walking. D. Importance of keeping catheter secured to body. 35. E. Avoid tugging on catheter. F. How to cleanse around catheter with soap and water when bathing. Chart – Utilize Nursing Notes at end of booklet: A. Catheter size and balloon volume. B. Amount and characteristics of urine obtained. C. Closed drainage system connected. D. Catheter taped in place. E. Client teaching given. F. Client’s response to procedure and teaching. 49 Indwelling Catheter Management: From Habit-based to Evidence-based Practice Author(s): JoAnn Mercer Smith, BSN, RN, CWOCN Pretesting silicone balloons is not recommended; the silicone can form a cuff or crease at the balloon area that can cause trauma to the urethra during catheter insertion.10,13 Inflation Much confusion exists about the proper volume to be used for balloon inflation. The guiding principle is to follow the manufacturer’s instructions. Catheter manufacturers test their balloons to determine the amount of fluid required to obtain a symmetrical balloon. Under- or overinflation can result in an asymmetrical balloon, which can deflect the catheter tip to one side. This deflection can cause occlusion of the drainage eyes, irritate the bladder wall, and lead to bladder spasms (see Figure 1 and Figure 2). In general, a 5-cc balloon requires about 10 cc of fluid for symmetrical inflation. Manufacturers recommend that sterile water be used to fill catheter balloons; normal saline can lead to crystal formation in the inflation lumen (and difficulty deflating the balloon), and inflation with air will cause the balloon to float in the bladder.24 Silicone catheter balloons can lose fluid over time as fluid diffuses out into the urine; therefore, fluid levels should be checked at least every 2 weeks and fluid added as needed.25 Catheter Securement All urinary catheters should be secured, yet securement is not routinely performed in practice. Unsecured urinary catheters can lead to bleeding, trauma, pressure sores around the meatus, and bladder spasms from pressure and traction.26 It is recommended that the catheter be secured to the thigh for women and to the upper thigh or lower abdomen for men. The lower abdominal position in men decreases the potential for pressure necrosis and urethral erosion at the penile-scrotal junction.24 Ambulatory men may find abdominal securement difficult; these patients can be instructed to secure the catheter to the upper thigh in the daytime and to change the position to the lower abdomen for sleep. Many securement devices are available, including adhesive, non-adhesive straps and catheter-specific anchors. A new catheter specific anchor (StatLock Foley™, Venetec International®, Inc. San Deigo, Calif. ) offers advantages that include a reclosable locking mechanism that swivels as the patient moves and an adhesive comfort pad that can be left in place for up to 1 week without altering skin integrity.26 Whatever product is selected, nurses should instruct patients in the proper use and removal of the securement device. Urine Collection Drainage bags now come with a special “safe sampling” port designed to obtain urine specimens while maintaining a closed system. The CDC recommends that urine specimens be obtained directly through these ports using an aseptic technique.8 The drainage tubing is occluded below the port temporarily, allowing the urine to collect in the tubing. The port is swabbed with alcohol, and the urine is withdrawn following manufacturer’s instructions using a needle, blunt cannula, or luer lock syringe. 50 Urine for a culture and sensitivity should be obtained from a newly inserted catheter and drainage bag to avoid culturing the system (catheter and drainage bag) rather than the urine. References: 1. Dobson C, Naidu S, Johnson M. Nurses’ perceptions of urinary catheter selection and management. Urology Nursing. 1996;16:140–144. 2. Evans E. Indwelling catheter care: dispelling the misconceptions. Geriatric Nursing. 1999;20(2):85–89. 3. Maki DG, Tambyah PA. Engineering out the risk of infection with urinary catheters. Emerg Infect Dis. 2001;7(2)342–347. 4. Wilde M. Meanings and practical knowledge of people with long-term urinary catheters. Journal of Wound Ostomy Continence Nursing. 2003;30(1):33–39. 5. Saint S, Veenstra DL, Sullivan SD, et al. The potential clinical and economic benefits of silver alloy urinary catheters in preventing urinary tract infection. Arch Intern Med. 2000;160(17):2670–2675. 6. Cravens DD, Zweig S. Urinary catheter management. Am Fam Physician. 2000;61(2):369–376. 7. Fanti JA, Newman DK, Colling J, et al. Clinical Practice Guidelines, No. 2, 1996 Update: Urinary Incontinence in Adults. Acute and Chronic Management. Rockville, Md. US Department of Health and Human Services. Public Services Agency for Health Care Policy and Research; March 1996. AHCPR Publication No.96-0682. 8. Wong ES, Hooten TM. Guideline for prevention of catheter-associated urinary tract infection. Center for Disease Control and Prevention. 1981;Feb. [serial online]. Available at: http://www.cdc.gov/ncidod/hip/GUIDE/uritract.htmnece. Accessed September 8, 2003. 9. Addison R, Mould C. Risk assessment in suprapubic catheterization. Nursing Standard. 2002;14(36):43–46. 10. Robinson J. Deflation of a foley catheter balloon. Nursing Standard. 2003;17(27):33–38. 11. Mitsui T, Minami K, Furuno T, et al. Is suprapubic cystostomy an optimal urinary management in high quadriplegics? A comparative study of suprapubic cystostomy and clean intermittent catheterization. Eur Urol. 2000; 38(4):434–438. 12. Nomura S. Ishido T, Teranishi J, Makiyama K. Long-term analysis of supra-pubic cyctostomy drainage in patients with neurogenic bladders. Urologia Internationalis. 2000;65(4):185–189. 13. Parkin J, Scanlan J, Woolley M, et al. Urinary catheter “deflation cuff” formation: clinical audit and quantitative in vitro analysis. British Journal of Urology. 2002;90(7):666–671. 14. Liss GM, Sussman GL. Latex sensitization: occupational versus general prevalence rates. Am J Ind Med. 1999;35(2):196–200. 15. Vila L, Sanchez G, Ano M, et al. Risk factors for latex sensitization among health care workers. J Investig Allergol Clin Immunol. 1999;9(6):356–360. 16. Department of Health and Human Services. FDA. Federal Register: Natural Rubber-Containing Medical Devices; User Labeling, Federal Register 1997;62(189):51021–51030. 17. Tullock AGS. Ferguson AF. Catheter-induced urethritis: a comparison between latex and silicone catheters in a prospective clinical trial. British Journal of Urology. 1985;57(3):325–328. 18. Studder UE, Bishop MC, Zingg EJ. How to fill silicone catheter balloons. Urology. 1983;22(3):300–302. 19. Salgado CD, Karchmer TB, Farr BM. Prevention of catheter-associated urinary tract infections. In: Wenzel RP, ed. Prevention and Control of Nosocomial Infections, 4th ed. Philadelphia, Pa.: Lippincott Williams & Wilkins; 2003;297–311. 20. Robinson J. Urethral catheter selection. Nursing Standard. 2001;15(25):39–42. 21. Newman DK. Managing indwelling urethral catheters. Ostomy/Wound Management. 1998;44(12):26–35. 22. Chinnes L, Dillion A, Fauerbach L. Home Care Handbook of Infection Control 2002. Washington, DC: Association of Professionals in Infection Control and Epidemiology (APIC);2002. 23. Gerard L, Sueppel C. Lubrication technique for male catheterization. Urology Nursing. 1997;17(4):156–158. 24. Cancio LC, Sabanegh ES JR, Thompson IM. Managing the foley catheter. Am Fam Physician. 1993;48(5):829–836. 25. Wilde M. Long-term indwelling urinary catheter care:conceptualizing the research base. J Adv Nurs. 1997;25(6):1252–1261. 26. Hanchett M. Techniques for stabilizing urinary catheters. Am J Nurs. 2002;102(3):44–48. 27. Getliffe K. Managing recurrent urinary catheter blockage: problems, promises and practicalities. Wound Ostomy Continence. 2003;30(3):146–151. 51 28. Dille C, Kirchhoff K. Increasing the wearing time of vinyl urinary drainage bags with bleach. Rehabilitation Nursing. 1993;18(5):292–295. 29. Rutala WA, Barbee SL, Aquiar NC, et al. Antimicrobial activity of home disinfectants and natural products against potential human pathogens. Infect Control Hosp Epidemiol. 2000;21(1):33–38. 30. Daifuku R. Stann WE. Association of rectal urethral colonization with urinary tract infection in patients with indwelling catheters. JAMA. 1984;252(15)2028–20230. 31. Warren JW. Catheter-associated urinary tract infections. Int J Antimicrob Agents. 2001;17(4):299–303. 32. Maki DG, Knasinski V, Halvorson K, Tambyah PA. Risk factors for catheter-associated urinary tract infection: a prospective study showing the minimal effect of catheter care violations on the risk of CAUTI (abstract). Infect Control Hosp Epidemiol. 2000;21:165. 33. Stickler DJ. Bacterial biofilms and encrustations of urethral catheters. Biofouling. 1996;94:293–305. 34. Donlan RM. Biofilms and device-associated infections. Emerg Infect Dis CDC. 2001;(7)2:277–281. 35. Kunin CM, Chin QF, Chambers S. Formation of encrustations on indwelling urinary catheters in the elderly: a comparison of different types of catheter materials in “blocker” and “nonblocker”. J Urol. 1987;138(4):899–902. 36. Tambyah PA, Maki DG. Catheter-associated urinary tract infection is rarely symptomatic; a prospective study of 1,497 catheterized patients. Arch Intern Med. 2000;160(5):678–682. 37. Gammack JK. Use and management of chronic urinary catheters in long-term care: much controversy, little consensus. Journal of the American Medical Directors Association. 2002;3(3):162–168. 38. McGeer A, Campbell B, Emori TG, et al. Definitions of infection for surveillance in long-term care facilities. Am J Infect Control. 1991;19(1):1–7. 39. Switters DM. Assessing leakage from around the urethral catheter. Urological Nursing. 1989;9(3):8–10. 40. Bhatia NN, Bergman A. Cystometry: unstable bladder and urinary tract infection. Brit J Urol. 1986;58(2):134–137. 41. Ziemann LK, Lastauskas NM, Ambrosini G. Incidence of leakage from indwelling urinary catheters in homebound patient. Home Healthcare Nurse. 1984;2(5):22–26. 42. Stickler DJ. Hewitt P. Activity of antiseptics against biofilms of mixed bacterial species growing on silicone surfaces. Eur J Clin Microbiol Infect Dis. 1991;10:416–421. 43. Morris NS, Stickler DJ. Does drinking cranberry juice produce urine inhibitory to the development of crystalline, catheter-blocking Proteus mirabilis biofilms? BJU Int. 2001;88(3):192–197. 52 Catheter Irrigation Performance Comments Satisfactory Unsatisfactory Time needed: 10 minutes Supplies needed: Catheter irrigation set Sterile irrigating solution Disposable gloves Alcohol wipes Towel 1. Follow asepsis during procedure. 2. Put on clean gloves. 3. Pour solution into basin properly, then recap bottle. 4. Aspirate 30 ml of solution into syringe. 5. Expose catheter-drainage tubing junction and place a clean towel under this area. Place basin within reach of working area. 6. Open one edge of alcohol wipe packet. 7. Remove protective covering and separate tubing from catheter. Insert end of tubing into wrapper from the alcohol wipe. Hold end of catheter in non-dominant hand while tucking tubing under draw sheet or towel in a manner to prevent it sliding off of the bed. 8. Wipe end of catheter with alcohol wipe. Insert tip of irrigating syringe into distal end of catheter. Hold catheter and irrigating syringe perpendicular to the floor. Slowly inject the 30cc. of solution. 9. Pinch catheter with finger of non-dominant hand and remove syringe. 10. Hold end of catheter over basin and allow urine to drain until flow stops. 11. Repeat steps 9 through 11 as necessary until urine flows freely. 53 Performance Comments Satisfactory Unsatisfactory 12. Retrieve drainage tubing. Wipe across opening of drainage tubing and catheter with a new alcohol wipe. 13. Reconnect catheter to drainage tubing while maintaining sterility of system. 14. Implement Closing General steps. 15. Chart the following: A. Amount and type of sterile solution used B. Number of irrigations needed C. Color and character of return D. Amount of urine returned (subtract amount of solution used from total return) E. How client tolerated procedure 54 Catheter Removal Performance Comments Satisfactory Unsatisfactory Time needed: 10 minutes Supplies needed: Sterile syringe (no needle) larger than the balloon size of the catheter you are removing Disposable gloves Bath towels and washcloth Paper towels Plastic bags Waste receptacle Appropriate urine collection device 1. Check physician’s most current order. 2. Wash your hands. 3. Introduce self to the client, unless you already have done this. 4. Identify client by asking them to state their name and checking their wrist band. 5. Explain the procedure and provide for privacy. 6. Elevate bed to working height and assist the client to a supine position. Ask the female client to abduct her leg. 7. Remove Velcro strap anchoring catheter to client’s leg. 8. Don clean gloves. 9. Place bath towel between the female client’s thighs with one edge under the buttocks. If the client is a male, place a towel over his thighs and under his penis. 10. Keep client draped with top covers. 11. Assess the balloon size, as indicated on the balloon injection port of the catheter, to determine the approximate amount of fluid in the balloon. Insert the syringe into the balloon injection port. Turn the syringe clockwise so it fits well into the port & withdraw all fluid. 55 Performance Comments Satisfactory Unsatisfactory 12. Tell client they may feel a burning sensation as the catheter is withdrawn. 13. Hold a paper towel under the catheter tubing close to the insertion site. Pull the catheter out smoothly and slowly; collecting it in the paper towel. 14. Cover the client with the top sheets. 15. Tell the client they may experience some burning when urinating for the first time. Ask the client to urinate in a collection device so the amount can be measured and to call the nurse each time they urinate. 16. Disconnect catheter from tubing and discard paper towel and catheter in waste receptacle. 17. Cleanse perineal area with soap and water and dry. Remove towel beneath them. Cover client. 18. Assist client to a comfortable position. 19. Lower bed height. Make sure side rails are up and give the client the call light. 20. Empty catheter drainage bag into graduated container. Place spigot over container. Unclamp spigot and drain urine from the bag. Place container on a flat surface and assess the amount of urine present at eye level. 21. Discard drainage bag. 22. Remove gloves. 23. Tie knot in plastic bag and remove it from waste receptacle. Place clean plastic bag in the receptacle. 24. Wash hands. 25. Document amount of urine drained from bag on the client’s I & O sheet. 26. Discard plastic bag in dirty utility room. 56 Performance Comments Satisfactory Unsatisfactory 27. Wash hands. 28. Chart: 29. A. Time catheter removed. B. Characteristics of urine and amount of drainage bag. C. Client’s response to the procedure. Provide a collection device, as directed below, and write the client’s name and room number on it. The urine collection device may be taken to the room before or after the procedure. A. B. Ambulatory Client 1) Man - provide urinal 2) Woman - provide specimen hat 3) Explain procedure for use 4) Store device in the bathroom Bedridden Client 1) Man - provide urinal, explain procedure for use and place within reach. 2) Woman - provide bedpan and store in a drawer of the bedside nightstand. 3). Follow-up care includes: A ) Maintaining I & O. B) Encouraging 2-3L of fluid per day unless contraindicated. C) Assessing for signs of urinary retention and notifying the physician if these occur. 57 Performance Comments Satisfactory Unsatisfactory D) Notifying the physician if the client is unable to void within 8 hours of removal or if the client has signs of urinary retention or discomfort. After the catheter has been removed, this time frame may be less than 8 hours depending on the client’s condition, treatment regimen, or physician’s order. A bladder scan may also be utilized/ordered to assist with determining urinary retention. E) Reporting to the nurse working the next shift the time the catheter was removed and whether or not the client voided. 58 Care for and Monitor a Peripheral IV Site Performance Comments Satisfactory Unsatisfactory Time needed: 5 minutes Supplies needed: Clean Gloves 1. Wash hands and don clean gloves. 2. Identify the patient. 3. Introduce yourself. 4. Explain the procedure. 5. Provide for privacy. 6. Observe the IV site, noting any redness, swelling, or drainage. 7. Assess the dressing, reinforcing if necessary. 8. Remove gloves and wash hands. 9. Document date, time, any observations about the IV site, name and title. 59 IV Equipment Set-Up Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Correct solution IV tubing & label IV pole Disposable gloves Needleless adaptor Saline flush 1. Open sterile packages using aseptic technique. 2. Check solution, using 8 “Rights” of drug administration (drug, dose, client, route, time, allergies, expiration date, documentation), comparing with order, label bag with patient name, ID information, room number, date, time, solution, expiration date, and any additives. Initial the label. 3. Open tubing set, maintaining sterility of both ends. 4. Place roller clamp about 2-4 cm (1-2 in) below drip chamber, and move roller to off position. 5. Hang bag on IV pole. 6. Insert tubing set spike into IV fluid bag A. Remove protective cover from IV bag without touching opening & maintaining sterility. B. Remove protector cap form tubing insertion spike, not touching spike, and insert spike into opening of IV bag. 7. Prime tubing A. Compress drip chamber, release & fill to line. B. Remove protective cap at end of tubing and attach needleless adaptor. Release roller clamp, slowly allowing fluid to travel from 60 Performance Comments Satisfactory Unsatisfactory drip chamber through tubing. Be sure to invert filter & y-site & tap as fluid flows through. Return roller clamp to off position after tube is filled. C. Be certain tubing is clear of air bubbles. D. Replace cap protector. E. Attach label to tubing indicating date/time/initials. 8. Put on gloves and inspect site of IV infusion for complications (redness, swelling, tenderness, induration, etc.) If complications are present, discontinue the site. 9. Set up IV pump – set rate according to physicians order with ml per hour. 10. Remove gloves and dispose of equipment properly. 11. Record in nurses’ notes type of fluid, flow rate, and time infusion was begun as well as site condition, patient’s response and teaching performed. 12. Observe client at least every hour or as needed to determine response to fluid therapy: A. Correct amount of solution infused as prescribed B. Proper flow rate ml/hour C. Patency of IV catheter or needle D. Absence of infiltration, phlebitis, or inflammation 61 Discontinuing an IV Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Disposable gloves Bandaid Sterile gauze dressing (2x2) Tape Adhesive remover (if needed) 1. Identify the patient. 2. Wash hands and put on gloves. 3. Close the flow clamp and disconnect tubing from needleless adapter. 4. Inspect site for complications (redness, swelling, tenderness, induration, etc). 5. Remove all the tape except the last piece holding the cannula. 6. While holding the hub, remove the last piece of tape. 7. Remove the cannula by pulling it out in a direct line opposite to insertion. 8. Gently press a sterile 2 x 2 over the entry site as the cannula is being removed until bleeding stops. Check cannula for visual intactness. 9. Apply band-aid to site. 10. Dispose of equipment properly. Dispose of tubing, bag in soiled waste container. 11. Remove gloves and cleanse hands. 12. Chart the procedure: Time and date, reason for discontinuing, condition of the site, nursing interventions, amount of IV infused, visual intactness of cannula, and client response, and any teaching done. 62 Saline Lock Flush Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Clean gloves Alcohol swabs Syringes (needleless) 0.9 Sodium Chloride (normal saline) 1. Review agency policy regarding amount of saline & frequency of saline flush. 2. Peripheral venous access devices (VADs) shall be flushed with a minimum of 3 ml of normal saline (0.9 sodium chloride). 3. Routine flushing shall be performed every shift if not in use, or with the following: A. Administering of blood and blood components B. Blood sampling C. Administration of incompatible medications or solutions D. Administration of medication E. Intermittent therapy F. When converting between intermittent and continuous therapies 4. Prior to beginning procedure: A. Use aseptic technique and observe standard precautions throughout procedure. Saline Lock Flush With saline (0.9% sodium chloride, injection) only: Flush with saline to maintain patency of intermittent VADs. 63 Performance Comments Satisfactory Unsatisfactory B. Cleanse access port with antiseptic solution. C. Connect saline-filled syringe to catheter via insertion into prepared injection/access port. D. Slowly aspirate until positive blood flow is obtained to confirm catheter patency. E. Slowly inject flush, maintaining positive pressure. F. Disconnect syringe from injection/access port. 64 Administering IV Push Medication (Existing Line and Saline Lock) Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: IV push (existing line) or IV push (IV lock) Medication in vial or ampule Syringe (3 to 5 ml) Syringe (3 ml) Sterile needles (21 and 25 gauge) or needleless device Antiseptic swab Vial of heparin flush solution (1 ml + 100 units or 1 ml + 10 units) or vial of normal saline (depending on agency policy) Disposable gloves Watch with second hand or digital read out 1. Check physician’s order for type of medication to be administered, dosage and route. Assess 8 “Rights” (drug, dose, client, route, time, allergies, expiration date, documentation). Bring medication book. A drug will be selected for you to look up and explain. Be able to indicate over what period of time the medication is to be administered. 2. Prepare equipment and assemble three 3 cc syringes and label 2 as NS and 1 as the medication; alcohol wipes, gloves. Keep end of syringe sterile. Note: Facility policy will dictate how much saline to use. 3. Prepare ordered medication from vial or ampule. Read package directions carefully for proper IV dilution of medication, if needed. Determine if IV incompatibilities exist with IV fluid/IV medication concurrently administered and time period over which it is to be given. 4. Wash hands. 65 Performance Comments Satisfactory Unsatisfactory 5. Administer medication by IV push (existing line): A. Check client’s identification by looking at armband and asking name. Compare with patient’s MAR. B. Observe site. C. Select injection port of IV tubing closest to client and prior to the filter. D. Clean off injection port with antiseptic swab. Allow to dry. E. Connect tip of syringe to injection port. F. Inject medication slowly over time period indicated. (Read direction on drug package. Check for compatibility of drug and existing IV fluid/medication added.) Use watch to time administrations. G. After injecting medication, release tubing, withdraw syringe, and recheck fluid infusion rate. (Be sure to maintain positive pressure on syringe plunger whenever using a syringe.) 6. IV Push Medication (Saline lock) Using SAS (Saline-Administration-Saline) method. A. Cleanse access port with antiseptic solution. B. Connect first saline-filled syringe to injection/access port. C. Slowly aspirate until positive blood return to confirm catheter patency. D. Flush with saline. E. Cleanse port with appropriate antiseptic solution. 66 Performance Comments Satisfactory Unsatisfactory F. Connect medication to injection/access port. G. Administer medication as stated in drug book. H. Disconnect medication from injection/ access port. I. Cleanse injection/access port with appropriate antiseptic solution. J. Connect second saline-filled syringe to injection/access port. K. Flush with saline. L. Disinfect injection/access port with appropriate antiseptic solution. 7. Post-Flush A. Monitor patient’s response. B. Discard used supplies in appropriate receptacles. C. Remove gloves. D. Wash hands. E. Document in patient’s medical record: 1) Amount of saline used. 2) Condition of the site. 3) Any problems encountered in flushing and action taken. 4) Response of client and teaching done. 5) Any adverse reactions to medication 67 Administering IV Medication by Secondary Set (IVPB) Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Drug book Disposable gloves Alcohol swabs Correct medication Syringes (10 ml needeless) Metal hook (optional) For this demo, you need to go review pump operation instructions (printed on pump and enclosed in your IV Therapy objectives booklet). A pump problem will be provided for you to solve. Practice using the pump before your demo time. 1. Check physician’s order to determine type of medication and dosage and type of solution to be used. Assess 8 “Rights” (drug, dose, client, route, time, allergies, expiration date, documentation). A drug will be selected for you to look up and explain. Be able to calculate the rate which the medication is to be administered. Assess compatibility of drug and primary infusion components. 2. Assess patency of existing IV infusion line and note infusion rate of main IV line. 3. Assess IV site for signs of infiltration or phlebitis and other problems. 4. Prepare equipment & supplies: Secondary set A. Medication prepared in a labeled infusion bag with IV line, microdrip or macrodrip infusion tubing set with needleless connector. B. Alcohol swab C. Plastic hook (optional) D. Disposable gloves 68 Performance Comments Satisfactory Unsatisfactory 5. Check client’s identification by looking at identification bracelet and asking name. 6. Wash hands and apply gloves. 7. Administer medications by piggyback/ secondary set. A. Hang medication bag at or above level of main fluid bag. Hook may be used to lower main bag. B. Clean injection port of main line with antiseptic swab. C. Administer medication by pump via secondary set. To set secondary: 1) Press Secondary. 2) Press Drug List. 3) Select medication from drug list. 4) Press correct medication dosage listed on pump. 5) Press Next to confirm. 6) Press Start. D. After medication has infused, check flow of primary infusion. Primary infusion should automatically begin to flow after piggyback is empty. E. Leave secondary bag and tubing in place for future drug administration or discard in appropriate containers. (Based on facility policy.) 8. Remove and dispose of gloves. Wash hands. 9. During infusion, periodically check infusion rate, pump function and condition of IV site. Assess for side effects and therapeutic effects of medication. 69 Performance Comments Satisfactory Unsatisfactory 10. Record drug, dose, route and time administered on medication form. Record volume of syringe on intake and output form. Document any side effects and therapeutic effects of medication. 11. Demonstrate ability to give appropriate rationale for any step when requested to do so by instructor. 70 Giving Medication through a Central Venous Catheter Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Disposable gloves Alcohol swabs Syringes (10 ml needleless) Saline (0.9 sodium chloride) Correct medication Drug book 1. Check physician’s orders regarding the medication. Check 8 “Rights” (drug, dose, client, route, time, allergies, expiration date, documentation). A medication will be selected for you to look up and explain. Be sure to be able to indicate over what period of time the medication is to be administered and its compatibility with existing concurrent infusion.) 2. Wash your hands. 3. Draw up medication in a 10 ml syringe. Assemble and fill two 10 ml syringes with 10 ml normal saline. Label all syringes: Medication and normal saline (x2). 4. Identify patient, introduce self and explain procedure. 5. Put on gloves. 6. Check CVC catheter site for complications. (See Site Inspection from CVC Dressing procedure.) 7. Cleanse port of CVC catheter tubing with alcohol. 8. Using the needleless system at your facility, insert needleless syringe containing 10 ml of NS into end of CVC tubing port. 9. Open CVC tubing clamp and aspirate to check for blood return. If blood doesn’t return, 71 Performance Comments Satisfactory Unsatisfactory reposition patient. If it still doesn’t return, inject slowly. DO NOT USE FORCE. If saline doesn’t flush easily, stop and report situation. Flush tubing. Note any problems around CVC insertion site. 10. Clamp CVC catheter and remove syringe from port. 11. Insert syringe containing medication into end of CVC catheter after cleansing its port with alcohol. 12. Open clamp and give medication over correct period of time, watching for any adverse reactions. 13. Clamp CVC catheter and remove medication syringe. 14. Insert syringe containing normal saline into CVC tubing port after cleansing with alcohol. 15. Open clamp and flush catheter tubing with 10 ml normal saline. 16. Close clamp and remove the syringe. 17. Dispose of equipment. (Syringes into sharps container.) 18. Assist patient as necessary and answer questions. Do teaching as needed. 19. Remove gloves, wash hands. 20. Chart procedure, medication, condition of site, patient toleration, and teaching. 21. Assess patient for response to medication (therapeutic and side effects). 22. Demonstrates ability to give appropriate rationale for any step when requested to do so by instructor. 72 Central Line Site Care and Dressing Change Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Mask for you and patient Clean gloves Sterile gloves Central line dressing kit Alcohol sticks, if allergic to tincture of chlorhexidine 1. Put following equipment in “sterile” package (use your catheter package): Sterile gloves, 2% tincture of chlorhexidine (if allergic to chlorhexidine, use packages of alcohol sticks), transparent dressing. 2. Identify patient and introduce yourself. 3. Position patient. Turn his/her head away from the dressing to make the insertion site more accessible and to minimize risk of contamination (put make on patient). 4. Prior to Beginning Procedure A. Check for allergies. B. Wash hands. C. Don clean gloves. D. Open dressing change kit. E. Use aseptic technique and observe standard precautions throughout procedure. 5. Equipment Inspection Inspect and monitor the following vascular access equipment: A. Connections B. Fluids being infused C. Pump function including flow rate 73 Performance Comments Satisfactory Unsatisfactory 6. Site Selection A. Don mask. Don patient with mask. B. Remove dressing from CAD insertion/exit site with clean gloves. C. Inspect site for signs of infusion-related complications to include but not limited to: 1) Discoloration (i.e., blaching, erythema) 2) Disruption of sensation (i.e., pain, tenderness, numbness) 3) Edema (i.e., pitting, non-pitting) 4) Localized swelling – Exudate (i.e. drainage) 7. D. If there is indication of complication development, notify the physician. E. Discard gloves. Dressing Change A. Don sterile gloves. B. Disinfect catheter-skin junction using septic solution: 1) Using friction, apply 2% tincture of chlorhexidine in a sweeping motion. 2) If sensitivity to chlorhexidine exists, use friction to apply 70% alcohol three times in a sweeping motion and allowing air dry between applications. 3) Cover an area approximately the size of the dressing. 4) Allow solution to air dry. 74 Performance Comments Satisfactory Unsatisfactory 5) Repeat if necessary. C. 8. Apply transparent dressing over site, leaving the catheter hub and tubing exposed. Do not apply gauze. Post-Dressing Change A. Discard used supplies. B. Remove gloves. C. Wash hands. D. Label new dressing with date, time and nurse initials. E. Document in patient’s medical record assessment of site, what was used to cleanse area and new dressing applied. 75 Peripheral Venipuncture with Over-the-Needle Catheter Insertion Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Correct solution Catheter (18-24 gauge depending on vein size) IV tubing and IV pump 2% tincture of chlorhexidine Tourniquet Transparent dressing Tape Towel Disposable gloves Sharps container 1. Observe for signs and symptoms indicating fluid or electrolyte imbalances. A. Sunken eyes B. Edema C. Greater than 2% increase or decrease in body weight D. Dry mucous membranes E. Flattened or distended neck veins F. Hypotension, tachycardia G. IV Regular pulse H. Crackles in lungs I. Inelastic skin turgor J. Increased or decreased bowel sounds K. Decreased urine output L. Behavioral changes M. Confusion 76 Performance Comments Satisfactory Unsatisfactory 2. Review orders for solution to be administered, dose of medication, rate of administration, frequency of administration, and route of administration. 3. Assemble necessary equipment for initiating IV line. 4. Identify client and explain procedure. Change client’s gown to IV gown. 5. Wash hands (15-20 seconds). 6. Organize equipment on clutter-free over-bed table. 7. Assemble equipment/maintaining sterility of connecting parts, attach syringe of normal saline to needles connector and flush. 8. Site selection A. Assess patient’s upper extremities. NOTE: Do not use lower extremities in patients of walking age without a specific order from a physician. B. Assess veins on both the ventral and dorsal surfaces: 1) Metacarpal 2) Cephalic 3) Basilic 4) Median cubital C. Select the most distal site for peripheralshort catheter placement: 1) Select sites that are proximal to previous cannulation sites. 2) When possible, avoid areas of flexion; existing phlebitis; bruises; or previous areas of infiltration. 77 Performance Comments Satisfactory Unsatisfactory 3) Avoid arms with comprised circulation, post-mastectomy or postaxillary node dissection, and fistualated extremities. NOTE: If these areas must be used, obtain a specific order from the physician. 4) In pediatric/neonatal patients, a site in the scalp, hand or foot is preferred over sites in the leg, arm, or antecubital fossa. D. Assess availability of acceptable veins by applying tourniquet 4 to 8 inches proximal to intended vein puncture site: 1) Place patient in comfortable position. 2) Palpate extremity distal to tourniquet to assess vein condition and visually inspect skin integrity. 3) Palpate to differentiate arteries from veins. 4) If unable to palpate vein, instruct patient to open and close fist several times: apply warm heat to the extremity for approximately 15 minutes to promote vein relaxation and dilation if necessary. E. Select insertion site. F. Select the smallest gauge, shortest length device to achieve the required therapy. (See figure on the following page for suggested gauge application). 78 Performance Comments Satisfactory Unsatisfactory Gauge and Suggested Application Catheter Gauge Size Use this size gauge for: Trauma patients 14 to 18 Surgery patients Blood transfusions General infusions 20 Intermittent infusions Blood transfusions General infusions: Child and adult, elderly 22 Intermittent infusions Blood transfusions General infusions: 24 Children and elderly Intermittent infusions 9. Site preparation A. Don gloves. B. Wash intended cannulation site with antiseptic soap if visible dirt and contaminated insertion site. C. Remove excess hair from intended cannulation site with clippers or scissors if necessary. Do not shave area as this may cause micro abrasions. D. Cleanse site, using friction with 2% tincture of chlorhexidine in a sweeping motion for 30 seconds. Allow to air dry for 30 seconds. NOTE: For infants under 2 months or if there is a sensitivity to chlorhexidine, the site will be cleansed using friction with alcohol in a sweeping motion three times, allowing drying between applications. 10. Cannula insertion A. Insert cannula for product integrity. B. Stabilize vein below intended access site with non-dominant hand. C. Insert cannula bevel up through skin at a 15-30 degree angle and observe for blood return with flashback chamber. 79 Performance Comments Satisfactory Unsatisfactory D. Lower angle of cannula inserting to about 15 degrees and continue to advance cannula into vein. E. Holding stylet steady, push cannula off stylet and into the vein until cannula hub is situated against the skin. F. Occlude tip of cannula by pressing fingers on non-dominant hand over approximate vein pathway to prevent retrograde bleeding. G. Release tourniquet. Remove stylet. H. Optional: Blood may be drawn at this point using a tube-holder with a male leur adapter. I. Use a new device for each cannulation attempt. J. If unsuccessful at cannulation after two (2) attempts, have another person competent in peripheral cannulation assess the patient. K. Stabilize site with sterile transparent dressing. For neonates/pediatrics, place dressing so that it does not extend beyond the back edge of the catheter hub. L. Label site with date, time, and initials of the inserter. M. Flush site as per protocol and/or initiate prescribed therapy. N. If restarting a site, discontinue previous site at this time. O. Discard equipment in appropriate receptacles. P. Document procedure, site, catheter size and number of attempts made to cannulate in patient’s medical record. 80 Performance Comments Satisfactory Unsatisfactory Q. Remove gloves. R. Cleanse hands. 11. Teach client about the purpose of IV therapy, complications and to notify RN in event of complications. Indicate complications that might occur. 12. Observe client every hour or as needed to determine response to fluid therapy. A. Correct amount of solution is prescribed B. Proper flow rate C. Patency of IV D. Absence of infiltration, phlebitis, or inflammation 13. Record in nurses’ notes cleansing procedure, number of attempts, type of fluid, location of insertion site, solution flow rate, size and type of IV catheter or needle, time infusion was begun, teaching done, client’s response and any problems encountered in inserting the catheter. 14. Demonstrate ability to give appropriate rationale for any step when requested to do so by instructor. 81 Mixing and Administering Insulin Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Insulin syringe Vial of “regular” insulin Vial of “NPH” insulin Clean gloves Alcohol wipes 1. Check doctor’s orders for correct dosage. (If patient is to undergo surgery or diagnostic procedures, check with the physician regarding insulin amount adjustment.) 2. Check 8 “Rights” (drug, dose, client, route, time, allergies, expiration date, documentation) of giving medications. 3. Check compatibility of insulin and time period. Regular insulin needs to be given within 5 minutes of preparation. 4. Gather equipment. 5. Roll the cloudy insulin between palms to distribute solution. (Know that shaking vial will cause insulin to foam and form bubbles.) 6. Clean the top of each insulin vial with an alcohol wipe. 7. Pull back plunger on syringe and fill with the amount of air that corresponds to the correct number of units of NPH insulin. Inject air into NPH vial without withdrawing insulin. 8. Remove needle and syringe from NPH insulin vial. 9. Pull back plunger on syringe and fill with the amount of air that corresponds to the correct number of units of regular insulin. Inject air into regular insulin and withdraw correct number of units of insulin. 82 Performance Comments Satisfactory Unsatisfactory 10. Withdraw needle and syringe and check syringe for air bubbles before next step. If bubbles are present, push plunger to expel them. Recheck number of units in syringe. If more is needed, withdraw correct amount or expel excess. No airlock is needed. Have another nurse verify the order, the regular insulin vial, and the dose drawn up in the syringe. 11. Return to NPH insulin vial, insert needle and carefully withdraw correct number of units of NPH insulin into syringe so that the exact amount is in syringe. (Know that it cannot be pushed back into vial, as syringe now contains a mixture of regular and NPH insulin.) 12. Have another nurse verify the order, the NPH insulin vial, and the total dose drawn up in the syringe. 13. Administer insulin correctly using subcutaneous technique. 14. Put away/dispose of equipment correctly. 15. Correctly record medication administered. 16. Check client for side effects and therapeutic response. 17. Demonstrate an ability to give appropriate rationale for any step in the demonstration when requested to do so by the instructor. 83 Administering Subcutaneous Medications Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Ampule Clean gloves 2 alcohol swabs Needle and syringe Bandaid 1. Verify medication order with original doctor’s order in the chart if: A. You are the first nurse giving the client the medication. B. There is no nurse verification signature on MAR. C. There is any discrepancy or lack of clarity with the order or the transcription. 2. If the above criteria are met, do not need to verify the MAR transcription with the original chart order. 3. Wash hands. 4. Maintain medical or surgical asepsis as appropriate throughout the procedure. 5. Prepare the medication at the medication cart using the MAR as point of reference. 6. Read the medication order and check the 8 “Rights” (drug, dose, client, route, time, allergies, expiration date, documentation) for each medication. 7. Choose the correct equipment: - Needle length: 3/5 – 5/8 - Needle gauge: 8. 25 to 27 gauge Give only small doses (no more than 1 ml) of water soluble medication per subcutaneous route. 84 Performance Comments Satisfactory Unsatisfactory 9. Correctly draw up the medication from an ampule or vial (Follow steps outlined in these separate procedures). For this demonstration draw up the medication from an ampule. Follow written procedure. 10. Subcutaneous Medication Administration A. Provide for client privacy by closing curtains around bed and exposing only chosen injection site. B. Raise bed to working height. C. Don clean gloves. D. Select appropriate injection site on actual person by: 1) Assess for tenderness, hardness, bruising, infection, or edema and avoiding those areas. 2) Consult MAR for previous injection sites and rotating sites. a) outer aspects of upper arms b) anterior aspects of thigh c) abdomen from below costal margins to iliac crest and at least 2 inches away from umbilicus d) scapular areas of upper back e) upper gluteal areas site E. Position client comfortably in relation to site. F. Cleanse the site with alcohol swab starting at center of site and rotate outward in a circular direction for about 2 inches. G. Hold swab between fingers of nondominant hand. 85 Performance Comments Satisfactory Unsatisfactory H. Remove needle cap from syringe by pulling cap straight off. I. Hold syringe between thumb and forefinger of dominant hand as if grasping a dart or pencil. J. For an average sized or an obese client, inject at a 90 degree angle. For a child or very thin adult, inject at a 45 degree angle (with needle bevel up). K. With non-dominant hand, lift and pull up to separate subcutaneous tissue from muscle and form a cushion of subcutaneous tissue. L. With non-dominant hand, pinch the subcutaneous cushion with injection of needle (To minimize pain of needle penetration of skin). Inject needle through skin using a smooth darting motion. M. Release tight pinch before injections and maintain the lifted subcutaneous cushion during injection. N. Withdraw the needle quickly while placing the alcohol swab just above the injection site. Keep non-dominant hand away from needle when withdrawing from site. O. Activate needle safety device. P. Massage site lightly unless contraindicated. Q. Apply band-aid only if necessary 9. Assist client to comfortable position. 10. Lower bed height, put up side rails, and give client the call light. 86 Performance Comments Satisfactory Unsatisfactory 11. Dispose of syringe unit and cap in identified receptacle in client’s room. If no receptacle in room, recap needle without sticking self by placing needle cap on flat surface and sliding syringe unit into cap. Do not hold needle cap with hand. Keep hand away from dirty needle until needle in cap. Secure cap on needle. Dispose of paper/plastic cups in waste receptacle. 12. Wash hands. 13. Correctly chart medication according to agency policy. 14. Return medication cart to secure area. 15. Explain rationale for any step of procedure as requested by instructor. 87 Administering IM Injections to an Adult Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Clean gloves Alcohol swabs Vial Syringe & needle Injection pad Band-aid 1. Verify medication order with original doctor’s order in the chart if: A. You are the first nurse giving the client the medication. B. There is no nurse verification signature on MAR. C. Or, there is any discrepancy or lack of clarity with the order or the transcription. 2. If the above criteria are met, do not need to verify the MAR transcription with the original chart order. 3. Wash hands. 4. Maintain both medical & surgical asepsis throughout the procedure. 5. Prepare the medication at the medication cart using the medication record point of reference. 6. Correctly calculate volume of drug as necessary. 7. Choose the correct equipment: A. Needle length (weight influences needle length): 5/8 – 1½” B. Needle gauge (selection based on viscosity of medication): - 20-25 gauge for aqueous - 18-25 gauge for oral based or viscous 88 Performance Comments Satisfactory Unsatisfactory Children: Adult: Elderly: 5/8 – 1” 1 – 1½” May need 5/8” 8. Validate the medication order against the 8 “Rights” (drug, dose, client, route, time, allergies expiration date, documentation). 9. Correctly draw up the medication from an ampule or vial. (Follow steps outlined in these separate procedures.) 10. Change the needle if the medication is irritating to the tissues and/or for Z-track method. 11. Take the following to the client’s bedside: A. Prepared medication B. Medication record C. Alcohol swab D. Band-aid E. Clean gloves 12. Introduce self to client unless have already met client. Identify client by asking client to state name and verifying name on client’s wrist band. Use second client identification method according to agency policy. 13. Explain procedure to client. 14. Explain the purpose of the medication and its action to the client. 15. Again verify the 8 “Rights” (drug, dose, client route, time, allergies, expiration date, documentation). 16. Provide for client privacy by closing curtains around bed and exposing only chosen injection site. 17. Raise bed to working height. 89 Performance Comments Satisfactory Unsatisfactory 18. Don clean gloves. 19. Select appropriate injections site on actual person by: A. Volume of fluid to be given (No more than 1 ml. in deltoid or no more than 3 ml. in other sites). B. Assessing for tenderness, hardness, bruising infection, or edema and avoiding these areas. C. Consulting MAR for previous injection sites and rotating sites. 20. Describes rationale for choice of injection site to instructor (For purpose of return demo, instructor will select injection site to be used from the following: deltoid, vastus lateralis, or ventrogluteal). 21. Position client comfortably and correctly in relation to injection site. Deltoid – Sitting or lying flat with lower arm flexed and resting across abdomen or lap. Vastus Lateralis – Supine with knee slightly flexed. Ventrogluteal – Side or back with knee and hip flexed on the side to be injected. 22. Locate and palpate site on actual person (not lab simulators) using correct anatomical landmarks. State anatomical landmarks using correct terms. Deltoid Acromion process Mid-point of lateral aspect of upper arm 1 to 2 inches below acromion process Vastus Lateralis Handbreadth above knee Handbreadth below groin & greater trochanter Middle third of muscle which is lateral to top of thigh 90 Performance Comments Satisfactory Unsatisfactory Ventrogluteal Use opposite hand and opposite hip Heel of hand on greater trochanter Thumb toward groin Fingers toward head Index finger over anterior superior iliac spine Middle finger extended along iliac crest toward buttock Give in center of “V” formed by index and middle finger 23. Cleanse the site with alcohol swab starting at center of site and rotating outward in a circular direction for about 2 inches. 24. Hold alcohol swab between fingers of nondominant hand. 25. Remove needle cap from syringe by pulling cap straight off. 26. Hold the syringe between thumb and first 2 fingers (with a dart or pencil hold). (If irritating preparation, use Z-track method of administration described at end of procedure). 27. Spread skin over site with non-dominant hand (If client’s muscle mass is small, grasp the body of the muscle with non-dominant hand). 28. Tell client that he/she will feel a stick now. 29. Inject needle quickly and smoothly at a 90 degree angle. 30. Maintain pencil hold on syringe with dominant hand and avoid any syringe movement. 31. Once the needle enters the site, move nondominant hand to top of plunger. 32. With non-dominant hand, slowly pull back slightly on the syringe to aspirate. Should blood appear, withdraw the needle, dispose of the syringe and start medication preparation again. 33. If no blood appears, inject medication slowly. 91 Performance Comments Satisfactory Unsatisfactory 34. Withdraw the needle quickly while placing the alcohol swab just above the injection site. Engage the needle safety device (keep nondominant hand away from needle being pulled out of skin). 35. Massage site lightly unless contraindicated. 36. Apply bandaid only if necessary. 37. Assist client to comfortable position. 38. Lower bed height, put up side rails, and give client the call light. 39. Dispose of syringe unit and cap in identified receptacle in client’s room. If no receptacle in room, recap needle without sticking self by placing needle cap on flat surface and sliding syringe unit into cap. Secure cap on needle. 40. Wash hands. 41. Correctly chart medication and site according to agency policy. 42. Explain rationale for any step of procedure as requested by instructor. 92 Z-Track Method of IM Administration Performance Comments Satisfactory Unsatisfactory Time needed: To Be Completed with IM Injection Supplies needed: Clean gloves Alcohol swabs Vial Syringe & needle Injection pad Bandaid Med tray May use for any IM injection. Must use when medication to be given is irritating to tissue, may stain tissue, or if to be given deep IM. 1. Check 8 “Rights” (drug, dose, client, route, time, allergies, expiration date, documentation) of giving medications. 2. Use at least a 1½ inch needle. Add 0.2 - 0.3 ml of air after accurate dose measurement. Change needle after drawing up med. 3. Give injection only in ventrogluteal site. 4. Locate appropriate landmarks using previously describe guidelines. 5. Cleanse a 3-inch area with alcohol swab using previously described guidelines. 6. Pull overlying skin and subcutaneous tissue approximately 1 to 1 ½ inches to the side and hold it over with the little finger side of the non-dominant hand. Do not contaminate prepared area when displacing skin. Maintain this position until withdrawing needle. 7. Aspirate with thumb & first finger of dominant hand. 8. Inject medication into original site and subcutaneous tissue displaced. 9. Maintain position with both hands for 10 seconds after medication injected. 93 Performance Comments Satisfactory Unsatisfactory 10. Withdraw needle quickly while simultaneously releasing displaced skin. 11. Do not massage site. 12. Explain rationale for any step of procedure as requested by instructor. 94 Administering Oral Medications Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Medication (Pill or Liquid) Clean gloves Medicine cup 1. Verify medication order with original doctor’s order in the chart if: A. You are the first nurse giving the client the medication. B. There is no nurse verification signature on MAR. C. There is any discrepancy of lack of clarity with the order or the transcription. 2. If the above criteria are met, do not need to verify the MAR transcription with the original chart order. 3. Wash hands. 4. Maintain medical asepsis throughout the procedure. 5. Prepare the medication at the medication cart using the medication record as point of reference. 6. Read the medication order and check the 8 “Rights” (drug, dose, client, route, time, allergies, expiration date, documentation). 7. Pill Form A. Compare label on unit dose package with the order on the MAR for exact accuracy. B. Leave pill in original wrapper and place entire package in medicine cup. 95 Performance Comments Satisfactory Unsatisfactory C. Take the medicine cup and the medication record to the client’s bedside. 8. Liquid Form A. Compare drug label on bottle with the order on the medication record for exact accuracy. B. Remove bottle cap and place it upside down. Hold bottle with label against palm of hand while pouring. Pour liquid into plastic graduated medicine cup if exact amount is so marked on the cup. Verify correct amount with cup on a flat surface and read amount poured at eye level. Wipe lip of bottle with paper towel if necessary. C. If dosage amount is not marked on graduated cup, draw up dosage in a syringe and then squirt correct dosage amount into medicine cup. 9. Take prepared medication and medication record to client’s bedside. Leave medication cart in med room or take to door of client’s room within easy view. 10. Introduce self to client unless have already met client. 11. Identify client using 2 methods: A. Asking client to state name and by verifying name on client’s wrist band. B. Using second method according to agency, policy, i.e., birthday. 12. Again, check the 8 “Rights” (drug, dose, client, route, time, allergies, expiration date, documentation) against the order on the medex. 13. Explain the purpose of the medication and its action to the client. 96 Performance Comments Satisfactory Unsatisfactory 14. Assist client to a sitting position in chair or elevate head of bed unless contraindicated. If sitting contraindicated, assist to side-lying position. 15. Open pre-packaged pill form and drop medication into medication cup. 16. Do not touch pill with your hands. 17. Give client pill cup or liquid medication if he/she is able to hold it. Assist client if necessary. 18. Give client full glass of fresh water unless contraindicated. (Some meds need to be given with juice or other drinks. Consult drug resource for this information.) 19. Stay with client until he/she has completely swallowed each medication. If uncertain, ask client to open mouth. Never leave medications for client to take independently unless specifically ordered that way. 20. Assist client to comfortable position. 21. Discard used medication cup, wrappers, etc. 22. Lower bed height, put up side rails, and give client the call light. 23. Wash hands. 24. Correctly chart medication according to agency policy. 25. Return medication cart to secure area. 97 Preparing an Injectable Medication from an Ampule Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Clean gloves Alcohol swabs Ampule Syringe & needle Injection pad Band-aid 1. Wash hands 2. Read the medication order and check the 8 “Rights” (drug, dose, client, route, time, allergies, expiration date, documentation). 3. Sign out medication in narcotic/record book if appropriate. 4. Tap the top of the ampule lightly and quickly with a finger to dislodge any medication from the top into the ampule. 5. Place a small, dry gauze pad or alcohol wipe still in opened wrapper around the neck of the ampule. 6. Snap the neck of the ampule in a direction away from your hands and face. 7. Insert the needle (use a filter needle when available) into the center of the ampule taking care not to allow the tip or shaft of the needle to touch the outer rim of the ampule. 8. Invert (turn upside down) the ampule with needle inserted. Hold ampule & syringe with non-dominant hand. 9. Aspirate the medication into the syringe by pulling back on the plunger with the dominant hand. 10. Keep the needle tip below the surface of the liquid. Tilt ampule to bring all the fluid within reach of the needle if all the volume of medication is to be withdrawn. 98 Performance Comments Satisfactory Unsatisfactory 11. If air bubbles are aspirated, do not expel the air into the ampule. 12. To expel excess air bubbles, remove the needle from the ampule. Hold the syringe with the needle pointing up. Draw back slightly on the plunger, and then push the plunger upward to eject the air. Do not eject fluid. 13. Hold the syringe and needle upright and tap the syringe barrel to dislodge air bubbles. Eject the air as described in step 12. 14. Verify accurate and exact amount of drug and correct if necessary by adding or deleting fluid. 15. Cover the needle with its sheath or cap maintaining surgical asepsis. 16. Explain rationale for any step of the procedure as requested by instructor. 99 Preparing an Injectable Medication from a Vial Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Clean gloves Alcohol swabs Vial Syringe & needle Injection pad Band-aid 1. Wash hands. 2. Read the medication order and check the 8 “Rights” (drug, dose, client, route, time, allergies, expiration date, documentation). 3. Sign out medication in narcotic/record book if appropriate. 4. Remove the metal cap to expose the rubber seal. 5. With an alcohol swab wipe off the surface of the rubber seal. 6. Remove needle cap. Pull back on the plunger to draw air into the syringe equivalent to the volume of mediation to be aspirated from the vial into the syringe. 7. Insert the tip of the needle, with bevel pointing up, through the center of the rubber seal. Apply pressure to the needle point during insertion. 8. Inject the air into the vial and hold onto the plunger after injecting the air. 9. Invert the vial while keeping a firm hold on the syringe and plunger. 10. Hold the vial and the syringe with the nondominant hand. 11. Grasp the end of the barrel and plunger with thumb and forefinger of the dominant hand. 100 Performance Comments Satisfactory Unsatisfactory 12. Keep tip of the needle below fluid level. 13. Allow air pressure to gradually fill the syringe with medication. Pull back slightly on the plunger if necessary. 14. Tap the side of the barrel carefully to dislodge any air bubbles. 15. Eject any air remaining at the top of the syringe into the vial. 16. Once the correct volume is obtained, remove the needle from the vial by pulling back on the barrel. 17. Remove any remaining air from the syringe and again verify that there is correct amount of medication in the syringe. 18. Recover needle with cap maintaining surgical asepsis. 19. Explain rationale for any step of the procedure as requested by instructor. 101 Inserting a Nasogastric Tube Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: NG tube - appropriate size (8 to 18 French) Stethoscope Glass of H2O with straw Water soluble lubricant Flashlight/Penlight Disposable gloves Tape, 1” wide Tissues Bath towel Emesis basin Safety pin & rubber band 1. Check physician’s order for insertion of nasogastric tube. 2. Explain procedure to patient, discussing with patient the need for the nasogastric tube; answer any questions patient may have. 3. Gather equipment. A. Set up suction, intermittent – set to high (120 mmHg), continuous – set to low 0-80 mmHg, or to ordered suction. B. Cut a 4-inch piece of tape and split bottom 2 inches, or use packaged nose tape for nasogastric tubes. 4. Perform hand hygiene. Don disposable gloves. 5. Assist patient to high Fowler’s position, or to 45 degrees if unable to maintain upright position, and determine which nostril will be easier access by using a penlight to inspect for a deviated septum or other abnormality; or ask the patient to occlude one nostril and breathe normally through the other, selecting the nostril through which air passes more easily. 6. Drape chest with bath towel or disposable pad. and have emesis basin and tissues handy. 102 Performance Comments Satisfactory Unsatisfactory 7. Measure distance to insert the tube by placing tip of tube at patient’s nostril and extending to tip of earlobe and then to tip of xiphoid process. Mark tube with a piece of tape. 8. Lubricate tip of tube (at least 1 to 2 inches) with water-soluble lubricant. 9. After having the patient lift his or her head, insert tube into nostril while directing tube upward and backward. Patient may gag when tube reaches the pharynx. Provide tissues for tearing or watering eyes. 10. Instruct patient to touch his or her chin to chest. Encourage him or her to sip water through a straw, or to swallow if no fluids are permitted. Advance tube in a downwardand-backward direction when patient swallows. Stop when patient breathes. If gagging and coughing persist, check placement of tube with a tongue blade and flashlight. Keep advancing tube until tape marking is reached. Do not use force. Rotate tube if it meets resistance. 11. Discontinue the procedure and remove the tube if there are signs of distress, such as gasping, coughing, cyanosis, or the inability to speak or hum. 12. Cleanse nose with alcohol pad and allow to dry. Secure tube with tape to patient’s nose. Be careful not to pull tube too tightly against nose. A. Place unsplit end over bridge of patient’s nose. B. Wrap split ends under tubing and up and over onto nose. 13. While keeping one hand on tube, determine that the tube is in the patient’ stomach using one of the following methods: 103 Performance Comments Satisfactory Unsatisfactory A. Insert 10-20ml air. Place stethoscope over epigastric area inject air while listening for air rush. B. Attach syringe to end of tube, aspirate for stomach contents. C. Obtain radiograph of placement of tube (as ordered by physician. 14. Attach tube to suction or clamp tube and cap it according to physician’s orders. 15. Secure tube to patient’s gown by using a rubber band or tape and a safety pin. If double-lumen tube is used, secure vent above stomach level. Attach at shoulder level. 16. Assist or provide patient with oral hygiene at regular intervals. 17. Remove disposable gloves and perform hand hygiene. Remove all equipment and make patient comfortable. 18. Record the insertion procedure, type and size of tube. Also document description of gastric contents, which naris used, patient’s response, and method used to verify placement. 104 Irrigating a Nasogastric Tube Performance Comments Satisfactory Unsatisfactory Time needed: 10 minutes Supplies needed: Irrigation set, or 50 cc catheter tip syringe Clean basin Container of normal saline Towel or waterproof pad Clean gloves Stethoscope NOTE: It is suggested that you plan to carry out this procedure with the insertion of the nasogastric tube procedure. 1. Raise level of bed to working height. 2. Put on gloves. 3. Place towel or waterproof pad across client’s chest. 4. Turn off suction or feeding and disconnect tubing. 5. If possible, check for tube placement as described in tube insertion. (Know that this may not be possible if tube is occluded.) 6. Fill syringe with 30-50 cc of normal saline and insert tip into end of tubing. (Saline is preferred over water because it reduces electrolyte depletion.) 7. Gently instill fluid into tubing. If fluid will not enter, loosen tape and move tube slightly, then retape. (Know that tip of tubing may be against mucosa.) 8. Aspirate fluid and discard basin. (If not returned, instill another 30-50 cc. If still not returned, do not instill more as it may cause distention.) 105 Performance Comments Satisfactory Unsatisfactory 9. Repeat instillation and aspiration with normal saline until tubing is cleared of clotted material or thick mucus. 10. During procedure, keep track of amount of saline instilled. If all of this amount is not returned, make sure the amount remaining in the stomach is included in intake for client. 11. Reconnect tubing to suction or feeding. 12. Inject 10 cc of air into air vent lumen and insert anti-reflux valve. 13. Chart: A. Signs and symptoms that prompted irrigation. B. Position of tube if determined. C. Amount of normal saline used and amount of return. D. Characteristics of returned fluids. E. Any difficulties encountered. F. Outcome of procedure (i.e., was patency reestablished?) G. How client tolerated procedure. 106 Removing a Nasogastric Tube Performance Comments Satisfactory Unsatisfactory Time needed: 10 minutes Supplies needed: Disposable gloves Towel Adhesive remover Tissues Emesis basin 1. Check physician’s order for removal of nasogastric tube. 2. Explain procedure to patient and assist to semiFowler’s position. 3. Gather equipment. 4. Perform hand hygiene. Don clean disposable gloves. 5. Place towel or disposable pad across patient’s chest. Give tissues and emesis basin to patient. 6. Discontinue suction and separate tube from suction. Unpin tube from patient’s gown and carefully remove adhesive tape from patient’s nose. 7. Instruct patient to take a deep breath and hold it. 8. Clamp tube with fingers by doubling tube on itself. Quickly and carefully remove tube while patient holds breath. 9. Dispose of tube per agency policy. Remove gloves and place in bag. 10. Offer mouth care to patient and facial tissues to blow nose. 11. Measure nasogastric drainage in suction device. Remove all equipment and dispose according to agency policy. Perform hand hygiene. 107 Performance Comments Satisfactory Unsatisfactory 12. Record removal of tube, patient’s response, and measure of drainage. Continue to monitor patient for 2 to 4 hours after tube removal for gastric distention, nausea, or vomiting. 108 Administering a Tube Feeding Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Disposable gloves Tube feeding at room temperature Stethoscope Syringe (60 ml) Towel Tap water 1. Explain procedure to patient. Use a stethoscope to assess bowel sounds. 2. Assemble equipment. Check amount, concentration, type, and frequency of tube feeding on patient’s chart. Check expiration date of formula. 3. Perform hand hygiene. Don disposable gloves. 4. Position patient with head of bed elevated at least 45 degrees or as near normal position for eating possible. 5. Unpin tube from patient’s gown and check to see that nasogastric tube is properly located in stomach, as described in step 12 of the “Inserting a Nasogastric Tube” demo. 6. Check residual by using a syringe to aspirate all gastric contents and measure. Return immediately through tube. Proceed with feeding if amount of residual does not exceed policy of agency or physician’s guideline. Disconnect syringe from tubing. 7. When using a feeding bag (open system): A. Hang bag on intravenous pole and adjust to about 12 inches above stomach. Clamp tubing. B. Cleanse top of feeding container with alcohol before opening it. Pour formula into feeding bag and allow solution to run through tubing. Close clamp. 109 Performance Comments Satisfactory Unsatisfactory C. Attach feeding setup to feeding tube, open clamp, and regulate drip rate according to physician’s order or allow feeding to run in over 30 minutes. D. Add 30 to 60 ml (1 to 2 ounces) of water for irrigation to feeding bag when feeding is almost completed and allow it to run through tube. E. Clamp tubing immediately after water has been instilled. Disconnect from feeding tube. Clamp tube and cover end with sterile gauze secured with rubber band and apply cap. 8. When using a large syringe (open system): A. Remove plunger from 30 or 60 ml syringe and irrigate with 30 ml of water. B. Attach syringe to feeding tube, pour premeasured amount of tube feeding into syringe, open clamp, and allow feeding to enter tube. Regulate the rate by raising or lowering the height of the syringe. Do not push formula with syringe plunger. C. Add 30 to 60 ml of water for irrigation to syringe when feeding is almost completed and allow it to run through the tube. D. When syringe has emptied, disconnect from the tube. Clamp the tube. 9. When using prefilled tube feeding setup (closed system): A. Remove screw-on cap and attach administration setup with drip chamber and tubing. Hang set on intravenous pole and adjust to about 12 inches above the stomach. Clamp tubing and squeeze drip chamber to fill to one-third to one-half of capacity. Release clamp and run formula through tubing. Close clamp. 110 Performance Comments Satisfactory Unsatisfactory B. Follow Actions 7c, 7d, and 7e. Feeding pump may be used with tube feeding setup to regulate drip. For Continuous Feedings 10. When using a feeding pump (continuous feeding): A. Close flow regulator clamp on tubing and fill feeding bag with prescribed formula. Amount depends on agency policy. Place label on container. B. Hang feeding container on intravenous pole and allow solution to flow through tubing. C. Connect to feeding pump following manufacturer’s directions. Set rate. 11. Observe patient’s response during and after tube feeding. 12. Have patient remain in upright position for at least 30 to 60 minutes after feeding. 13. Wash and clean equipment or replace according to agency policy. Remove gloves and perform hand hygiene. 14. Record type and amount of feeding, residual amount, verification of placement, and patient’s response. Monitor blood glucose, if ordered by physician. 111 Administering Medications via a Nasogastric Tube Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Disposable gloves 60 ml syringe Medications (crushed or in liquid form) Water for flush 1. Check to see whether medications to be administered come in a liquid form. If pills or capsules are to be given, check with pharmacy about crushing or opening capsules. Ensure that the tube is patent and irrigate as necessary (see Skill 11-4). 2. Using medicine cups, prepare all medications to be given. Also prepare 15-20 ml of water for each medication that is to be given. 3. Perform hand hygiene and don gloves. If patient has continuous tube feedings, pause tube feeding pump. 4. Verify placement of tube with instillation of 10-20 ml air. While inserting air bolus, auscultate for air rush. 5. Fold tube over and clamp with fingers. Insert tip of 60 ml syringe into gastric tube. Release NG tube. Pull plunger back using a constant gentle pressure to check for residue. 6. After noting amount, replace residual feeding back into stomach. 7. Fold NG tube over and clamp with fingers. Remove 60 ml syringe. Remove plunger from syringe. Flush with 10 ml of water, administer each medication, flushing between each medication with 5-10 ml of water. 8. Flush with 30 ml of water after last medication is administered. 112 Performance Comments Satisfactory Unsatisfactory 9. Fold tubing back over and clamp with fingers. If more medications are to be given, repeat Actions 7 and 8. If no more medications are to be given, reconnect tube feeding or clamp NG tube. Do not return to suction for at least 45 minutes. 10. Remove gloves and perform hand hygiene. 11. Record amount of water uses to flush tube and document on the medication administration record. 113 Changing and Emptying an Ostomy Appliance Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Disposable gloves Basis with water, soap & towel Ostomy wafer and measuring device Skin protectant or barrier Ostomy bag (correct size) Graduated container Scissors Adhesive 1. Gather the necessary equipment. 2. Perform hand hygiene and apply non-sterile gloves. 3. Explain procedure to the patient. 4. Provide for patient’s privacy. Assist to a comfortable sitting or lying position in bed or a standing or sitting position in the bathroom. To empty a pouch, proceed to Action 11. To change a pouch, continue to Action 5. 5. Empty the partially filled appliance or pouch into a bedpan if it is drainable. 6. Slowly remove the appliance, beginning at the top while keeping the abdominal skin taut. If any resistance is felt, use warmth or the adhesive solvent to facilitate removal. Discard the disposable appliance or pouch in a plastic bag. 7. Use toilet tissue to remove any excess stool from the stoma. Cover stoma with a gauze pad. Gently wash and pat dry the peristomal skin. Mild soap may be used to cleanse the peristomal skin, taking care to ensure that all soap is rinses before reapplying pouch. Do not apply any lotion to the peristormal area. 114 Performance Comments Satisfactory Unsatisfactory 8. Assess the appearance of the peristomal skin and stoma. A moist reddish-pink stoma is considered normal. 9. Apply one-piece or two-piece system: A. Select size for stoma opening by using the measurement guide (template). B. Trace same size circle on the back and center the skin barrier. C. Use scissors to cut an opening 1/4 to 1/8 inch larger than stoma. D. Remove the backing of protective skin barrier. Apply additional skin protection necessary. E. Remove gauze pad covering stoma. F. Ease barrier appliance or pouch onto the abdomen and over the stoma, and gently press onto skin while smoothing out creases or wrinkles. Hold in place for 3 minutes. 10. Close the bottom of appliance or pouch by folding the end upward and using a clamp or clip that comes with product. Continue to Action 15. To Empty Appliance or Pouch 11. Plan to drain the appliance or pouch when it is one-third to one-half full. Remove clamp and fold the end of the pouch upward like a cuff. 12. Empty contents into bedpan, toilet, or measuring device. Rinse appliance or pouch with tepid water or water mixed with a drop of mouthwash administered with a squeeze bottle. 13. Wipe the lower 2 inches of the appliance or pouch with toilet tissue. 14. Uncuff the edge of the appliance or pouch and apply the clip or clamp. 115 Performance Comments Satisfactory Unsatisfactory 15. Dispose of used equipment according to agency policy. Remove non-sterile gloves from inside out and discard. 16. Perform hand hygiene. 17. Document the following: appearance of stoma, condition of peristomal skin, characteristics of drainage (amount, color, consistency, unusual odor), and patient’s reaction to procedure. 116 Irrigating a Colostomy Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Disposable gloves Irrigation container with cone tubing Water soluble lubricant Warm solution as ordered (tap water) 1. Assemble the necessary equipment. If tap water is used, adjust temperature as it flows from the faucet to a warm temperature. 2. Explain procedure to the patient and plan where he or she will receive irrigation. Assist patient onto bedside commode or into nearby bathroom. 3. Perform hand hygiene. 4. Add irrigation solution to container. Release the clamp and allow fluid to progress through the tube before reclamping to prime tubing. 5. Hang container so that the bottom of bag will be at the patient’s shoulder level when seated. 6. Put on disposable gloves. 7. Remove appliance and attach irrigation sleeve. Place the drainage end into the toilet blow or bedpan. 8. Lubricate the end of the cone with watersoluble lubricant. 9. Insert the cone into the stoma. Introduce the solution slowly over a period of 5 minutes. Hold tubing (or if patient is able allow patient to hold tubing) all the time that solution is being instilled. Control the rate of flow by closing or opening the clamp. 10. Hold the cone in place for an additional 10 seconds after the fluid is infused. 117 Performance Comments Satisfactory Unsatisfactory 11. Remove the cone. Assist patient to remain seated on toilet or bedside commode. 12. After most of the solution has returned, allow patient to clip (close) the bottom of the irrigating sleeve and continue with daily activities. 13. After solution has stopped flowing from stoma, remove irrigating sleeve and cleanse skin around stoma opening with mild soap and water. Gently pat peristomal skin dry. 14. Attach new appliance to stoma (see Changing and Emptying an Ostomy Appliance demo) if needed. 15. Document the procedure, including the amount of irrigating solution used; color, amount, and consistency of stool returned; condition of the patient’s stoma; degree of patient participation; and patient’s reaction to the irrigation. 118 Administering Medication by Suppository Performance Comments Satisfactory Unsatisfactory Time needed: 15 Minutes Supplies needed: Medication in suppository form Disposable gloves Lubricant Medication order Tissues Disposable bag 1. Assemble equipment (medication in suppository form, glove, lubricant), go to client’s room, knock, introduce self and identify the client by checking the arm bracelet or using facility approved and accepted method of identification. 2. Provide for privacy of the client. Arrange appropriate screening. Explain the procedure to the client, family member, or caregiver. 3. Wash hands. 4. Help the client assume a left sidelying/lateral position with the top knee in acute flexion. 5. Unwrap the suppository and place it on the work surface on the wrapper or a clean, protected surface. Put on the glove. Place a small amount of lubricant on the tip of the suppository. 6. Ask the client to breathe deeply to help relax the anal sphincter to ease insertion of the suppository. The suppository is inserted in a smooth motion up to 10 cm. (4”) into the rectal passage with the finger of the gloved hand directing the suppository into the anus. Attempt to place the suppository along the rectal wall. 7. Observe anal area for hemorrhoids. 119 Performance Comments Satisfactory Unsatisfactory 8. Remove finger (the glove is removed by drawing the inside over the outside). Wipe lubricant off anus. 9. Encourage the client to hold the buttocks together to prevent expulsion of the suppository in response to an urge to defecate. 10. Return after 15 minutes to ensure client is comfortable. 11. Chart medication and results obtained. 120 Tracheostomy Care Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Tracheostomy care kit Sterile normal saline Hydrogen peroxide Sterile gloves Disposable gloves Waste receptacle lined with plastic bag Bath towel Cleaned and cleared overbed table 1. Wash hands for 3 minutes and applies face shield or goggles if splashing is likely. 2. Introduce self to the client. 3. Identify the client. 4. Explain reason for procedure & tell client the steps of the procedure prior to doing them. Provide for privacy. 5. Raise bed to working height. 6. Place cleaned & cleared over-bed table perpendicular to the head of the client’s bed within reach of working area. 7. Suction the client through the tracheostomy prior to performing tracheostomy care. (Separate demo for students) Replace the client’s oxygen source. 8. Using same gloves previously donned for the suctioning, remove soiled dressing & discard in receptacle. Remove gloves & discard. 9. Open tracheostomy care kit and establish sterile field. 10. Fill one fluid receptacle of the tray (one on your left) with about 2 inches of peroxide. 121 Performance Comments Satisfactory Unsatisfactory 11. Uncap bottle of normal saline & fill the other receptacle with about 2 inches of normal saline. 12. Set up sterile field with all cleaning equipment and dressings. 13. Don sterile gloves. 14. Maintain surgical asepsis throughout procedure with dominant hand. 15. Remove oxygen source from tracheostomy with non-dominant hand. 16. While holding the outer cannula with the non dominant hand, unlock the inner cannula with the dominant hand (sterile hand) by turning it to the left 90 degrees. 17. Remove the inner cannula & place it in the tray of peroxide with dominant hand. (Or replace inner cannula with a new disposable inner cannula. If the patient has disposable inner cannula, do not clean the old inner cannula; simply discard it.) NOTE: If the client is on a ventilator, a spare sterile inner cannula should be inserted at this time so the client can be quickly reattached to the ventilator. 18. Replace oxygen source (non-dominant hand). 19. Cleanse the lumen & the outside surface of the inner cannula with the brush. Hold end of brush with non-dominant hand. 20. Rinse inner cannula with normal saline & shake off excess moisture. 21. Remove oxygen source with non-dominant hand. 22. Replace inner cannula with dominant hand. Hold onto outer cannula with non-dominant hand during this procedure. 23. Lock inner cannula by turning it to the right (should feel it lock) with the dominant hand. 122 Performance Comments Satisfactory Unsatisfactory 24. Replace oxygen source with non-dominant hand. 25. Using the dominant hand, moisten a sterile cotton tipped applicator with peroxide & cleanse sides of stoma. 26. Cleanse far side of the stoma using one applicator & use another applicator for the near side. 27. Repeat procedure using cotton tipped applicators moistened with normal saline to rinse. 28. Hold a 4 x 4 in the dominant hand, moisten it with normal saline & cleanse the tube’s flange. 29. Dry areas with 4 x 4’s following the same sequence. 30. Second nurse washes hands and dons clean gloves. 31. Second nurse removes oxygen source. 32. Second nurse stands at the side of the bed opposite the first nurse. Second nurse gently holds sides of tracheostomy flange to prevent tube from being coughed out. 33. First nurse cuts old tracheostomy strings at both sides of the client’s neck or unhooks Velcro straps from each side. Takes extra caution to avoid cutting cuff tubing. 34. Remove old tracheostomy string. First nurse picks ups trach string. Inserts one trach string into the flange opening nearest to him/her. Passes the string behind the client’s neck and through the back side of the opposite flange opening. Next, pass the string behind the client’s neck again and tie the two ends together in a knot on the side of the client’s neck or fasten Velcro straps. (See picture on next page.) 123 Performance Comments Satisfactory Unsatisfactory 35. Second nurse’s role in now over. Removes gloves & washes hands. 36. First nurse applies trach dressing. Holds trach dressing with hand on outside edges only. Uses forceps to pull dressing beneath strings & flange. 37. Recheck tightness of ties. 38. Replace oxygen source. 39. Discard equipment and remove gloves. 40. Assist the client to a comfortable position. 41. Lower bed height, raise side rails, and give call light to client. 42. Wash hands. 43. Chart procedure: Characteristics of drainage on soiled dressing, condition of stoma, client’s response to procedure, what area was cleansed with, and type of dressing applied. 44. Explain rationale for any step of procedure as requested by instructor. 124 Tracheostomy Suctioning Performance Comments Satisfactory Unsatisfactory Time needed: 15 minutes Supplies needed: Suction catheter (diameter not more than ½ the size of the tracheostomy opening) Sterile normal saline irrigating solution Sterile container for normal saline 1 pair sterile gloves Yankeur suction Oxygen source, flow meter, wing tip connector, oxygen connecting tubing, ambu bag with trach adaptor Waste receptacle lined with plastic bag Bath towel Cleaned and cleared overbed table Note: If the client has an artificial airway, a suction apparatus, connecting tubing & sterile normal saline should always be kept at the bedside. In addition, an ample supply of suction catheters & sterile gloves should always be kept at the bedside. 1. Wash hands for 3 minutes and applies face shield or goggles if splashing is likely. 2. Introduce self and identify the client. 3. Explain reason for procedure & tell client the steps of the procedure to doing them. Provide for privacy. 4. Raise bed to working height. Elevate the head of the bed to at least 45 degrees unless contraindicated. 5. Place cleaned & cleared overbed table perpendicular to the head of the client’s bed within reach of working area. Place equipment on table. 125 Performance Comments Satisfactory Unsatisfactory 6. Assess breath sounds for quality & rate of respirations. Assess apical pulse rate & rhythm & color of lips & nailbeds. Do not suction client routinely. Suction only when needed. 7. Attach suction connecting tubing to suction apparatus. Turn on suction, occlude tubing & test suction amount. Regulate suction between 80 and 120. Make sure end of connecting tubing is within close reach. 8. Attach ambu bag to oxygen source & turn flow meter to 12-15 liters/min. Place ambu bag on opposite side of the bed. 9. Follow principles of surgical asepsis during all movements. Ask the client to refrain from touching the suction catheter. 10. Pour normal saline into sterile container. Open sterile gloves & suction catheter packages. 11. Don sterile gloves. To lessen risk of contamination, wrap catheter around the fingers of dominant gloved hand. Grasp suction connection tubing with non-dominant hand. Insert connection part of catheter into suction tubing. NOTE: During this procedure, the gloved dominant hand should remain sterile. The nondominant hand is gloved for the nurse’s protection from the client’s secretion. Remember to refrain from contaminating the dominant gloved hand. 12. Lubricate the catheter with the normal saline by applying suction & drawing up normal saline through the catheter. 13. The second nurse now assists after washing hands & donning clean gloves. 126 Performance Comments Satisfactory Unsatisfactory 14. The second nurse stands on the opposite side of the bed from the first nurse, removes the oxygen source & connects the ambu bag to the tracheostomy. 15. Using two hands to deflate the bag, the second nurse oxygenates the client with 3 to 5 deep lung inflations to help compensate for the oxygen removed during the suctioning process. 16. The second nurse removes the ambu bag. The first nurse inserts the catheter into the trach opening as far as it will go, withdraws the catheter 1-2 cm to prevent damaging the area. 17. Rotate catheter between dominant thumb & forefinger, gradually withdraw the catheter while applying intermittent suction (move non-dominent thumb up & down on suction port to apply intermittent suction). 18. Minimize hypoxemia by not suctioning for longer than 10-15 seconds during each suction attempt. After each suction pass, the first nurse rinses the catheter by suctioning up normal saline and clearing the tubing of secretions. 19. Immediately after the first nurse removes the catheter, the second nurse gives the client 3 to 5 deep ventilations with the ambu bag. 20. Repeat the procedure as necessary -- usually only one to two suction passes at one given time are needed. 21. After the last suction pass, the second nurse oxygenates the client with the ambu bag and replaces the oxygen source. The second nurse’s role is completed. 22. The first nurse discards the catheter. 23. Suction the client’s mouth with the Yankeur suction (clean), rinse the catheter & provide oral hygiene. 24. Assess the client’s breath sounds, heart rate, and skin color. 127 Performance Comments Satisfactory Unsatisfactory 25. Turn off the suction machine and the secondary oxygen source. 26. Discard the equipment & removes gloves properly. 27. Assist the client to a comfortable position. 28. Lower bed height, raise side rails, and give call light to client. 29. Document procedure. Include: Size of catheter, oxygenation with manual resuscitator before & after each suction pass, characteristics of secretions, quality of cough, lung sounds, respiratory rate, & that oral hygiene was given. 30. Explain rationale for any step of procedure as requested by instructor.