ECO 737 Health Economics Fall 2014
advertisement

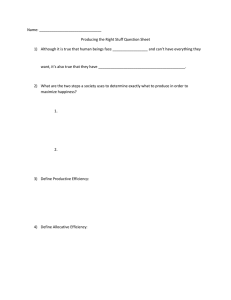
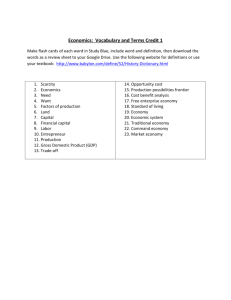
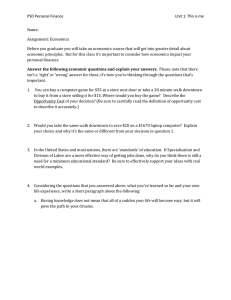
ECO 737 Health Economics Fall 2014 Mondays and Wednesdays from 2:00-3:15 PM, Bryan 456 Instructor: Martin Andersen Office: Bryan 448 Office Hours: Mondays and Wednesdays from 10AM to 11:30 AM E-mail: msander4@uncg.edu Overview This course provides an overview of health economics, with an emphasis on the United States. We will cover a broad range of topics and, in most cases, we will be unable to do them justice. We will also be omitting several important areas of health economics—I will provide a supplemental reading list by the end of the semester that brings in additional readings and topics (but this list is SOLELY for your own interest). However, you will have the opportunity to write on and discuss a topic of your choosing as part of the final project for the course. Please take this as an opportunity to explore an area of health economics that interests you. Student Learning Objectives At the end of this course, students should achieve the following capabilities: 1. Describe the major theoretical models in health economics and the key empirical tests of those models; 2. Apply these models to problems in health economics and health policy; and 3. Assess if new medical or other interventions are cost-effective. Prerequisites Students should have a firm grasp of microeconomic theory and applied econometrics. Grading and Evaluation The overall grade for the course will be based on five items: 1. In-class midterm (20%); 2. Referee report (20%); 3. Class participation (20%); 4. Final research project: a. Project presentation (20%); b. Written report (20%). The in-class midterm will be on September 22nd and will consist of two to four long answer questions, drawn from a list of eight to ten questions that I will give you on September 12th (via email). The referee report assignment will be distributed on September 24th and will be due at NOON on October 15th (note: the due time is before the start of class—assignments handed in during class will be considered late and penalized accordingly). Class participation will be based on an in-class paper presentation and comments submitted, by e-mail, the night before each lecture on the starred readings in the list below. The final research project will be described in more detail on the first day of class. Structure of the Course The first five weeks of the course will consist mostly of lectures in which I will cover the essentials of health economics. After these five weeks have concluded, each of you will be able to discuss health economics in broad strokes. At the end of this period, there will be an in-class midterm before we shift gears to discussing special topics or applications in health economics. These lectures will be in a modified seminar format, in which each of you will be responsible for one or two papers during the remainder of the semester and will present and lead a discussion about the paper. The semester will conclude with a short segment on cost-effectiveness analysis and then final project presentations. Two lectures will be canceled during the semester and I plan on rescheduling these lectures to a single two and half hour session to discuss some recent developments in hospital-insurer bargaining. I will circulate a Doodle poll early in the semester to identify a time and date for this lecture and I will provide breakfast/lunch/snacks/dinner as appropriate. Note: I reserve the right to change readings, order of topics, assignments, etc., as needed. Textbook There is no assigned textbook for this class, rather we will be using journal articles and, occasionally, chapters from the Handbook of Health Economics. However, the following books may well be useful during the semester: Culyer, A. J., & Newhouse, J. P. (Eds.). (2000). Handbook of Health Economics, Volumes 1A & 1B. Amsterdam ; New York: North Holland. Fuchs, V. R. (1998). Who Shall Live? (Expanded.). World Scientific Publishing Company. Newhouse, J. P. (1993). Free for All?: Lessons from the RAND Health Insurance Experiment. Cambridge, MA: Harvard University Press. Pauly, M. V., McGuire, T. G., & Barros, P. P. (Eds.). (2012). Handbook of Health Economics, Volume 2 (1 edition.). Amsterdam: North Holland. Sloan, F. A., & Kasper, H. (Eds.). (2008). Incentives and Choice in Health Care (1 edition.). Cambridge, MA: The MIT Press. Schedule Date Monday, 8/18 Wednesday, 8/20 Monday, 8/25 Wednesday, 8/27 Monday, 9/01 Wednesday, 9/03 Monday, 9/08 Wednesday, 9/10 Monday, 9/15 Wednesday, 9/17 Monday, 9/22 Wednesday, 9/24 Monday, 9/29 Wednesday, 10/01 Monday, 10/06 Wednesday, 10/08 Monday, 10/13 Wednesday, 10/15 Monday, 10/20 Wednesday, 10/22 Monday, 10/27 Wednesday, 10/29 Monday, 11/03 Wednesday, 11/05 Monday, 11/10 Wednesday, 11/12 Monday, 11/17 Wednesday, 11/19 Monday, 11/24 Wednesday, 11/26 Monday, 12/01 Topic Introduction Demand for Health and Health Capital Demand for Health Care Services Demand for Private Health Insurance UNIVERSITY HOLIDAY, NO CLASS Selection in Insurance Markets—Theory Selection in Insurance Markets—Empirics Public Programs and Insurance Coverage RESCHEDULED (DATE TBD) Insurer-Provider Bargaining In-Class Midterm Exam Physician Behavior Hospital Behavior Competition Prescription Drugs Productivity UNIVERSITY HOLIDAY, NO CLASS Managed Care Medical Malpractice Socio-economic Status and Health Mental Health Risky Behaviors Obesity Business Cycle Effects Environment and Health Guest Lecture (Prof. J. Bray) Cost Effectiveness/Cost Benefit—1 Cost Effectiveness/Cost Benefit—2 Labor Markets and Health Insurance UNIVERSITY HOLIDAY, NO CLASS Final Project Presentations Readings Lecture 1—Introduction Fuchs, V. R. (1998). Who Shall Live? (Expanded.). World Scientific Publishing Company. A real classic—should be on every health economist’s shelf. Fuchs, V. R. (2012). Major Trends in the U.S. Health Economy since 1950. N Engl J Med, 366(11), 973–977. doi:10.1056/NEJMp1200478 Fuchs, V. R. (2008). Three “Inconvenient Truths” about Health Care. N Engl J Med, 359(17), 1749–1751. doi:10.1056/NEJMp0807432 Cutler, D. M. (2002). Equality, Efficiency, and Market Fundamentals: The Dynamics of International Medical-Care Reform. Journal of Economic Literature, 40(3), 881– 906. Lecture 2—Demand for Health and Health Capital *Case, A., and A. Deaton. “Broken down by Work and Sex: How Our Health Declines.” Analyses in the Economics of Aging, 2005, 185–205. Grossman, Michael. “On the Concept of Health Capital and the Demand for Health.” The Journal of Political Economy 80, no. 2 (April 1972): 223–55. *Grossman, Michael. “The Human Capital Model,” Volume 1:, Part 1:347–408. Elsevier, 2000. Lecture 3—Demand for Health Care Services Acemoglu, Daron, Amy Finkelstein, and Matthew J. Notowidigdo. “Income and Health Spending: Evidence from Oil Price Shocks.” Review of Economics and Statistics 95, no. 4 (October 2013): 1079–95. doi:10.1162/REST_a_00306. Arrow, Kenneth J. “The Economics of Moral Hazard: Further Comment.” The American Economic Review 58, no. 3 (June 1968): 537–39. * Arrow, Kenneth J. “Uncertainty and the Welfare Economics of Medical Care.” The American Economic Review 53, no. 5 (December 1963): 941–73. Chandra, Amitabh, Jonathan Gruber, and Robin McKnight. “Patient Cost-Sharing and Hospitalization Offsets in the Elderly.” American Economic Review 100, no. 1 (March 2010): 193–213. doi:10.1257/aer.100.1.193. *Finkelstein, Amy. “The Aggregate Effects of Health Insurance: Evidence from the Introduction of Medicare*.” Quarterly Journal of Economics 122, no. 1 (February 1, 2007): 1–37. doi:10.1162/qjec.122.1.1. *Manning, Willard G, Joseph P Newhouse, Naihua Duan, Emmett B Keeler, and Arleen Leibowitz. “Health Insurance and the Demand for Medical Care: Evidence from a Randomized Experiment.” The American Economic Review 77, no. 3 (June 1987): 251–77. *Pauly, Mark V. “The Economics of Moral Hazard: Comment.” The American Economic Review 58, no. 3 (June 1968): 531–37. Lecture 4—Demand for Private Health Insurance *Ehrlich, Isaac, and Gary S. Becker. “Market Insurance, Self-Insurance, and SelfProtection.” The Journal of Political Economy 80, no. 4 (August 1972): 623–48. Feldstein, Martin, and Jonathan Gruber. “A Major Risk Approach to Health Insurance Reform.” Tax Policy and the Economy 9 (January 1, 1995): 103–30. Feldstein, Martin S. “The Welfare Loss of Excess Health Insurance.” The Journal of Political Economy 81, no. 2 (April 1973): 251–80. *Gruber, Jonathan, and James Poterba. “Tax Incentives and the Decision to Purchase Health Insurance: Evidence from the Self-Employed.” The Quarterly Journal of Economics 109, no. 3 (August 1994): 701–33. Manning, Willard G., and M. Susan Marquis. “Health Insurance: The Tradeoff between Risk Pooling and Moral Hazard.” Journal of Health Economics 15, no. 5 (October 1996): 609–39. doi:10.1016/S0167-6296(96)00497-3. *Zeckhauser, R. (1970). Medical insurance: A case study of the tradeoff between risk spreading and appropriate incentives. Journal of Economic Theory, 2(1), 10–26. doi:10.1016/0022-0531(70)90010-4 Lecture 5—Selection in Insurance Markets—Theory *Akerlof, George A. “The Market for ‘Lemons’: Quality Uncertainty and the Market Mechanism.” The Quarterly Journal of Economics 84, no. 3 (August 1970): 488– 500. doi:10.2307/1879431. *Rothschild, Michael, and Joseph Stiglitz. “Equilibrium in Competitive Insurance Markets: An Essay on the Economics of Imperfect Information.” The Quarterly Journal of Economics 90, no. 4 (November 1976): 629–49. Einav, Liran, and Amy Finkelstein. “Selection in Insurance Markets: Theory and Empirics in Pictures.” Journal of Economic Perspectives 25, no. 1 (February 2011): 115–38. doi:10.1257/jep.25.1.115. *Einav, Liran, Amy Finkelstein, and Mark R. Cullen. “Estimating Welfare in Insurance Markets Using Variation in Prices*.” Quarterly Journal of Economics 125, no. 3 (2010): 877–921. doi:10.1162/qjec.2010.125.3.877. (Focus on theoretical section) *Hemenway, David. “Propitious Selection.” The Quarterly Journal of Economics 105, no. 4 (November 1990): 1063–69. Lecture 6— Selection in Insurance Markets —Empirics *Cutler, David M, and Sarah J Reber. “Paying for Health Insurance: The Trade-Off between Competition and Adverse Selection.” The Quarterly Journal of Economics 113, no. 2 (May 1998): 433–66. *Einav, Liran, Amy Finkelstein, and Mark R. Cullen. “Estimating Welfare in Insurance Markets Using Variation in Prices*.” Quarterly Journal of Economics 125, no. 3 (2010): 877–921. doi:10.1162/qjec.2010.125.3.877. (Focus on empirical section) *Fang, Hanming, Michael P. Keane, and Dan Silverman. “Sources of Advantageous Selection: Evidence from the Medigap Insurance Market.” Journal of Political Economy 116, no. 2 (April 1, 2008): 303–50. doi:10.1086/587623. Handel, Benjamin R. “Adverse Selection and Inertia in Health Insurance Markets: When Nudging Hurts.” American Economic Review 103, no. 7 (December 2013): 2643– 82. doi:10.1257/aer.103.7.2643. Lecture 8—Public Programs and Insurance Coverage *Card, David, and Lara D. Shore-Sheppard. “Using Discontinuous Eligibility Rules to Identify the Effects of the Federal Medicaid Expansions on Low-Income Children.” The Review of Economics and Statistics 86, no. 3 (March 13, 2006): 752–66. *Cutler, David M, and Jonathan Gruber. “Does Public Insurance Crowd Out Private Insurance.” The Quarterly Journal of Economics 111, no. 2 (May 1996): 391–430. Gruber, Jonathan, and Kosali Simon. “Crowd-out 10 Years Later: Have Recent Public Insurance Expansions Crowded out Private Health Insurance?” Journal of Health Economics 27, no. 2 (March 2008): 201–17. doi:10.1016/j.jhealeco.2007.11.004. Lecture 9—Physician Behavior Chandra, Amitabh, David Cutler, and Zirui Song. “Chapter Six - Who Ordered That? The Economics of Treatment Choices in Medical Care.” In Handbook of Health Economics, Volume 2:397–432. Elsevier, 2011. http://www.sciencedirect.com/science/article/pii/B9780444535924000062. *Clemens, Jeffrey, and Joshua D. Gottlieb. “Do Physicians’ Financial Incentives Affect Medical Treatment and Patient Health? †.” American Economic Review 104, no. 4 (April 2014): 1320–49. doi:10.1257/aer.104.4.1320. Gruber, Jonathan, and Maria Owings. “Physician Financial Incentives and Cesarean Section Delivery.” The RAND Journal of Economics 27, no. 1 (Spring 1996): 99– 123. Kolstad, Jonathan T. “Information and Quality When Motivation Is Intrinsic: Evidence from Surgeon Report Cards.” American Economic Review 103, no. 7 (December 2013): 2875–2910. doi:10.1257/aer.103.7.2875. *McGuire, Thomas G. “Physician Agency.” In Handbook of Health Economics, 1:461–536. Elsevier, 2000. http://www.sciencedirect.com/science/article/pii/S1574006400801687. (This chapter is very long, skim it.) *McGuire, Thomas G., and Mark V. Pauly. “Physician Response to Fee Changes with Multiple Payers.” Journal of Health Economics 10, no. 4 (1991): 385–410. doi:10.1016/0167-6296(91)90022-F. *Yip, Winnie C. “Physician Response to Medicare Fee Reductions: Changes in the Volume of Coronary Artery Bypass Graft (CABG) Surgeries in the Medicare and Private Sectors.” Journal of Health Economics 17, no. 6 (December 1998): 675–99. doi:10.1016/S0167-6296(98)00024-1. Lecture 10—Hospital Behavior *Cutler, David M. “The Incidence of Adverse Medical Outcomes Under Prospective Payment.” Econometrica 63, no. 1 (January 1995): 29–50. *Dafny, Leemore S. “How Do Hospitals Respond to Price Changes?” The American Economic Review 95, no. 5 (December 2005): 1525–47. Dranove, David. “Pricing by Non-Profit Institutions : The Case of Hospital Cost-Shifting.” Journal of Health Economics 7, no. 1 (March 1988): 47–57. doi:10.1016/01676296(88)90004-5. Baicker, K., & Staiger, D. (2005). Fiscal Shenanigans, Targeted Federal Health Care Funds, and Patient Mortality*. Quarterly Journal of Economics, 120(1), 345–386. doi:10.1162/qjec.2005.120.1.345 *Ellis, Randall P., and Thomas G. McGuire. “Hospital Response to Prospective Payment: Moral Hazard, Selection, and Practice-Style Effects.” Journal of Health Economics 15, no. 3 (June 1996): 257–77. doi:10.1016/0167-6296(96)00002-1. *———. “Provider Behavior under Prospective Reimbursement : Cost Sharing and Supply.” Journal of Health Economics 5, no. 2 (June 1986): 129–51. doi:10.1016/0167-6296(86)90002-0. Frakt, Austin B. “How Much Do Hospitals Cost Shift? A Review of the Evidence.” Milbank Quarterly 89, no. 1 (March 2011): 90–130. doi:10.1111/j.14680009.2011.00621.x. Newhouse, Joseph P. “Toward a Theory of Nonprofit Institutions: An Economic Model of a Hospital.” The American Economic Review 60, no. 1 (1970): 64–74. Pauly, Mark, and Michael Redisch. “The Not-For-Profit Hospital as a Physicians’ Cooperative.” The American Economic Review 63, no. 1 (March 1973): 87–99. Lecture 11—Competition in Health Care Markets Gaynor, Martin, and Robert J. Town. “Chapter Nine - Competition in Health Care Markets.” In Handbook of Health Economics, Volume 2:499–637. Elsevier, 2011. Gaynor, Martin, and William B. Vogt. “Antitrust and Competition in Health Care Markets,” Volume 1:, Part 2:1405–87. Elsevier, 2000. *Kessler, Daniel P., and Mark B. McClellan. “Is Hospital Competition Socially Wasteful?” The Quarterly Journal of Economics 115, no. 2 (May 2000): 577–615. Dafny, L., Gruber, J., & Ody, C. (2014). More Insurers Lower Premiums: Evidence from Initial Pricing in the Health Insurance Marketplaces (Working Paper No. 20140). National Bureau of Economic Research. Retrieved from http://www.nber.org/papers/w20140 *Dafny, L. S. (2010). Are Health Insurance Markets Competitive? American Economic Review, 100(4), 1399–1431. doi:10.1257/aer.100.4.1399 Melnick, Glenn A., Jack Zwanziger, Anil Bamezai, and Robert Pattison. “The Effects of Market Structure and Bargaining Position on Hospital Prices.” Journal of Health Economics 11, no. 3 (October 1992): 217–33. doi:10.1016/0167-6296(92)90001H. Meltzer, David, Jeanette Chung, and Anirban Basu. “Does Competition under Medicare Prospective Payment Selectively Reduce Expenditures on High-Cost Patients?” The RAND Journal of Economics 33, no. 3 (October 1, 2002): 447–68. doi:10.2307/3087467. Robinson, James C., and Harold S. Luft. “The Impact of Hospital Market Structure on Patient Volume, Average Length of Stay, and the Cost of Care.” Journal of Health Economics 4, no. 4 (December 1985): 333–56. doi:10.1016/0167-6296(85)900128. Lecture 12—Prescription Drugs Duggan, Mark, and Fiona Scott Morton. “The Effect of Medicare Part D on Pharmaceutical Prices and Utilization.” American Economic Review 100, no. 1 (March 2010): 590–607. doi:10.1257/aer.100.1.590. *Duggan, Mark, and Fiona M. Scott Morton. “The Distortionary Effects of Government Procurement: Evidence from Medicaid Prescription Drug Purchasing*.” Quarterly Journal of Economics 121, no. 1 (February 1, 2006): 1–30. doi:10.1162/qjec.2006.121.1.1. Frank, Richard G., and David S. Salkever. “Pricing, Patent Loss and the Market for Pharmaceuticals.” Southern Economic Journal 59, no. 2 (October 1992): 165–79. Huskamp, Haiden A., Richard G. Frank, Kimberly A. McGuigan, and Yuting Zhang. “The Impact of a Three-Tier Formulary on Demand Response for Prescription Drugs.” Journal of Economics & Management Strategy 14, no. 3 (September 1, 2005): 729–53. doi:10.1111/j.1530-9134.2005.00080.x. Moran, John R., and Kosali Ilayperuma Simon. “Income and the Use of Prescription Drugs by the Elderly: Evidence from the Notch Cohorts.” J. Human Resources XLI, no. 2 (April 1, 2006): 411–32. doi:10.3368/jhr.XLI.2.411. *Reiffen, David, and Michael R. Ward. “Generic Drug Industry Dynamics.” Review of Economics and Statistics 87, no. 1 (February 1, 2005): 37–49. doi:10.1162/0034653053327694. Yin, Wesley, Anirban Basu, James X. Zhang, Atonu Rabbani, David O. Meltzer, and G. Caleb Alexander. “The Effect of the Medicare Part D Prescription Benefit on Drug Utilization and Expenditures.” Annals of Internal Medicine 148, no. 3 (February 5, 2008): 169 –177. Lecture 13—Productivity *Almond, D., Doyle, J., Kowalski, A. E., & Williams, H. (2010). Estimating Marginal Returns to Medical Care: Evidence from At-Risk Newborns*. Quarterly Journal of Economics, 125(2), 591–634. doi:10.1162/qjec.2010.125.2.591 Chandra, Amitabh, and Jonathan Skinner. “Technology Growth and Expenditure Growth in Health Care.” Journal of Economic Literature 50, no. 3 (September 2012): 645– 80. doi:10.1257/jel.50.3.645. *Chandra, Amitabh, and Douglas Staiger. “Productivity Spillovers in Health Care: Evidence from the Treatment of Heart Attacks.” Journal of Political Economy 115, no. 1 (2007): 103–40. *Garber, A. M., & Skinner, J. S. (2008). Is American Health Care Uniquely Inefficient? Journal of Economic Perspectives. Hall, Robert E, and Charles I Jones. “The Value of Life and the Rise in Health Spending.” Quarterly Journal of Economics 122, no. 1 (2007): 39–72. Murphy, Kevin M., and Robert H. Topel. “The Value of Health and Longevity.” Journal of Political Economy 114, no. 5 (October 1, 2006): 871–904. doi:10.1086/508033. Lecture 14—Managed Care *Aizer, Anna, Janet Currie, and Enrico Moretti. “Does Managed Care Hurt Health? Evidence from Medicaid Mothers.” Review of Economics and Statistics 89, no. 3 (2007): 385–99. doi:10.1162/rest.89.3.385. Baker, Laurence C., and Ciaran S. Phibbs. “Managed Care, Technology Adoption, and Health Care: The Adoption of Neonatal Intensive Care.” The RAND Journal of Economics 33, no. 3 (Autumn 2002): 524–48. Chernew, Michael, Philip DeCicca, and Robert Town. “Managed Care and Medical Expenditures of Medicare Beneficiaries.” Journal of Health Economics 27, no. 6 (December 2008): 1451–61. doi:10.1016/j.jhealeco.2008.07.014. *Cutler, David M, Mark McClellan, and Joseph P Newhouse. “How Does Managed Care Do It?” The RAND Journal of Economics 31, no. 3 (Autumn 2000): 526–48. Duggan, Mark, and Tamara Hayford. “Has the Shift to Managed Care Reduced Medicaid Expenditures? Evidence from State and Local-Level Mandates.” Journal of Policy Analysis and Management, 2013, n/a–n/a. doi:10.1002/pam.21693. *Frank, R. G., Glazer, J., & McGuire, T. G. (2000). Measuring adverse selection in managed health care. Journal of Health Economics, 19(6), 829–854. doi:10.1016/S0167-6296(00)00059-X Wu, Vivian Y. “Managed Care’s Price Bargaining with Hospitals.” Journal of Health Economics 28, no. 2 (March 2009): 350–60. doi:10.1016/j.jhealeco.2008.11.001. Lecture 15—Medical Malpractice Brennan, Troyen A., Colin M. Sox, and Helen R. Burstin. “Relation between Negligent Adverse Events and the Outcomes of Medical-Malpractice Litigation.” N Engl J Med 335, no. 26 (December 26, 1996): 1963–67. doi:10.1056/NEJM199612263352606. *Currie, Janet, and W. Bentley MacLeod. “First Do No Harm? Tort Reform and Birth Outcomes*.” Quarterly Journal of Economics 123, no. 2 (May 1, 2008): 795–830. doi:10.1162/qjec.2008.123.2.795. Danzon, Patricia M. “Liability for Medical Malpractice,” Volume 1:, Part 2:1339–1404. Elsevier, 2000. http://www.sciencedirect.com /science/article/B7P5R-4FF827617/2/970336c7c654bd7ae34d8232f907e8f3. *Frakes, Michael, and Anupam B. Jena. Does Medical Malpractice Law Improve Health Care Quality? Working Paper. National Bureau of Economic Research, January 2014. http://www.nber.org/papers/w19841. *Kessler, Daniel, and Mark McClellan. “Do Doctors Practice Defensive Medicine?” The Quarterly Journal of Economics 111, no. 2 (May 1996): 353–90. Kessler, Daniel P. “Evaluating the Medical Malpractice System and Options for Reform.” Journal of Economic Perspectives 25, no. 2 (May 2011): 93–110. doi:10.1257/jep.25.2.93. Klick, Jonathan, and Thomas Stratmann. “Medical Malpractice Reform and Physicians in High‐Risk Specialties.” The Journal of Legal Studies 36, no. S2 (June 1, 2007): S121–S142. doi:10.1086/520416. Lecture 16—Socio-economic Status and Health *Glied, S., & Lleras-Muney, A. (2008). Technological innovation and inequality in health. Demography, 45(3), 741–761. doi:10.1353/dem.0.0017 Goldman, D. P., & Smith, J. P. (2002). Can patient self-management help explain the SES health gradient? Proceedings of the National Academy of Sciences of the United States of America, 99(16), 10929 –10934. doi:10.1073/pnas.162086599 *Lleras-Muney, Adriana. “The Relationship between Education and Adult Mortality in the United States.” The Review of Economic Studies 72, no. 1 (January 1, 2005): 189– 221. Lecture 17—Mental Health *Currie, Janet, and Mark Stabile. “Child Mental Health and Human Capital Accumulation: The Case of ADHD.” Journal of Health Economics 25, no. 6 (November 2006): 1094–1118. doi:10.1016/j.jhealeco.2006.03.001. Elder, Todd E. “The Importance of Relative Standards in ADHD Diagnoses: Evidence Based on Exact Birth Dates.” Journal of Health Economics 29, no. 5 (September 2010): 641–56. doi:10.1016/j.jhealeco.2010.06.003. Fletcher, Jason M. “The Effects of Childhood Adhd on Adult Labor Market Outcomes.” Health Economics, 2013, n/a–n/a. doi:10.1002/hec.2907. Fletcher, Jason, and Barbara Wolfe. “Child Mental Health and Human Capital Accumulation: The Case of ADHD Revisited.” Journal of Health Economics 27, no. 3 (May 2008): 794–800. doi:10.1016/j.jhealeco.2007.10.010. *Frank, Richard G., and Thomas G. McGuire. “Economics and Mental Health.” In Handbook of Health Economics, Volume 1:, Part 2:893–954. Elsevier, 2000. http://www.sciencedirect.com/science/article/B7P5R-4FF8276W/2/7c72e2b65c41420922471dff2034e5da. *Klick, Jonathan, and Sara Markowitz. “Are Mental Health Insurance Mandates Effective? Evidence from Suicides.” Health Economics 15, no. 1 (January 2006): 83–97. doi:10.1002/hec.1023. *Lang, Matthew. “The Impact of Mental Health Insurance Laws on State Suicide Rates.” Health Economics 22, no. 1 (2013): 73–88. doi:10.1002/hec.1816. Lecture 18—Addiction Becker, Gary S, and Kevin M Murphy. “A Theory of Rational Addiction.” The Journal of Political Economy 96, no. 4 (August 1988): 675–700. *Becker, Gary S., Michael Grossman, and Kevin M. Murphy. “An Empirical Analysis of Cigarette Addiction.” The American Economic Review 84, no. 3 (June 1994): 396– 418. doi:10.2307/2118059. Bernheim, B. Douglas, and Antonio Rangel. “Addiction and Cue-Triggered Decision Processes.” The American Economic Review 94, no. 5 (December 2004): 1558–90. doi:10.2307/3592834. Cawley, John, and Christopher J. Ruhm. “Chapter Three - The Economics of Risky Health Behaviors.” In Handbook of Health Economics, Volume 2:95–199. Elsevier, 2011. http://www.sciencedirect.com/science/article/pii/B9780444535924000037. Chaloupka, Frank J., and Kenneth E. Warner. “The Economics of Smoking,” Volume 1:, Part 2:1539–1627. Elsevier, 2000. http://www.sciencedirect.com/science/article/B7P5R-4FF82761B/2/02fc6bbcacd765074e46dd650843ef57. *Gruber, Jonathan, and Botond Köszegi. “Is Addiction ‘Rational’? Theory and Evidence.” The Quarterly Journal of Economics 116, no. 4 (November 2001): 1261–1303. doi:10.2307/2696459. Lecture 19—Obesity *Bhattacharya, Jay, and M. Kate Bundorf. “The Incidence of the Healthcare Costs of Obesity.” Journal of Health Economics 28, no. 3 (May 2009): 649–58. doi:10.1016/j.jhealeco.2009.02.009. *Cawley, John, and Chad Meyerhoefer. “The Medical Care Costs of Obesity: An Instrumental Variables Approach.” Journal of Health Economics 31, no. 1 (January 2012): 219–30. doi:10.1016/j.jhealeco.2011.10.003. Chou, Shin-Yi, Michael Grossman, and Henry Saffer. “An Economic Analysis of Adult Obesity: Results from the Behavioral Risk Factor Surveillance System.” Journal of Health Economics 23, no. 3 (May 2004): 565–87. *Cutler, David M., Edward L. Glaeser, and Jesse M. Shapiro. “Why Have Americans Become More Obese?” The Journal of Economic Perspectives 17 (August 1, 2003): 93–118. doi:doi:10.1257/089533003769204371. Finkelstein, Eric A, Christopher J Ruhm, and Katherine M Kosa. “Economic Causes and Consequences of Obesity.” Annual Review of Public Health 26 (2005): 239–57. Flegal, Katherine M., Margaret D. Carroll, Cynthia L. Ogden, and Clifford L. Johnson. “Prevalence and Trends in Obesity Among US Adults, 1999-2000.” JAMA 288, no. 14 (October 9, 2002): 1723–27. doi:10.1001/jama.288.14.1723. Flegal, Katherine M., Barry I. Graubard, David F. Williamson, and Mitchell H. Gail. “Excess Deaths Associated With Underweight, Overweight, and Obesity.” JAMA 293, no. 15 (April 20, 2005): 1861–67. doi:10.1001/jama.293.15.1861. Gruber, Jonathan, and Michael Frakes. “Does Falling Smoking Lead to Rising Obesity?” Journal of Health Economics 25, no. 2 (March 2006): 183–97. Philipson, Tomas J., and Richard A. Posner. “The Long-Run Growth in Obesity as a Function of Technological Change.” Perspectives in Biology and Medicine 46, no. 3 (2003): S87–S107. Lecture 20—Business Cycle Effects Currie, Janet, and Erdal Tekin. “Is the Foreclosure Crisis Making Us Sick?” National Bureau of Economic Research Working Paper Series No. 17310 (August 2011). http://www.nber.org/papers/w17310. Dehejia, Rajeev, and Adriana Lleras-Muney. “Booms, Busts, and Babies’ Health.” The Quarterly Journal of Economics 119, no. 3 (August 1, 2004): 1091–1130. Miller, Douglas L., Marianne E. Page, Ann Huff Stevens, and Mateusz Filipski. “Why Are Recessions Good for Your Health?” The American Economic Review 99, no. 2 (May 1, 2009): 122–27. *Ruhm, Christopher J. “Are Recessions Good for Your Health?” The Quarterly Journal of Economics 115, no. 2 (May 2000): 617–50. ———. “Good Times Make You Sick.” Journal of Health Economics 22, no. 4 (July 2003): 637–58. doi:10.1016/S0167-6296(03)00041-9. *Ruhm, Christopher J. Recessions, Healthy No More? Working Paper. National Bureau of Economic Research, August 2013. http://www.nber.org/papers/w19287. Xu, Xin, and Robert Kaestner. “The Business Cycle and Health Behaviors.” National Bureau of Economic Research Working Paper Series No. 15737 (February 2010). http://www.nber.org/papers/w15737. Lecture 21—Health and the Environment *Chay, Kenneth Y., and Michael Greenstone. “The Impact of Air Pollution on Infant Mortality: Evidence from Geographic Variation in Pollution Shocks Induced by a Recession.” The Quarterly Journal of Economics 118, no. 3 (August 1, 2003): 1121–67. Isen, Adam, Maya Rossin-Slater, and W. Reed Walker. Every Breath You Take – Every Dollar You’ll Make: The Long-Term Consequences of the Clean Air Act of 1970. Working Paper. National Bureau of Economic Research, January 2014. http://www.nber.org/papers/w19858. Lleras-Muney, Adriana. “The Needs of the Army Using Compulsory Relocation in the Military to Estimate the Effect of Air Pollutants on Children’s Health.” Journal of Human Resources 45, no. 3 (June 20, 2010): 549–90. *Moretti, Enrico, and Matthew Neidell. “Pollution, Health, and Avoidance Behavior Evidence from the Ports of Los Angeles.” Journal of Human Resources 46, no. 1 (January 1, 2011): 154–75. Neidell, Matthew J. “Air Pollution, Health, and Socio-Economic Status: The Effect of Outdoor Air Quality on Childhood Asthma.” Journal of Health Economics 23, no. 6 (November 2004): 1209–36. doi:10.1016/j.jhealeco.2004.05.002. Schlenker, Wolfram, and W. Reed Walker. “Airports, Air Pollution, and Contemporaneous Health.” National Bureau of Economic Research Working Paper Series No. 17684 (2011). http://www.nber.org/papers/w17684. Lecture 22—Guest Lecture by J. Bray Readings TBD Lectures 23 and 24—Cost Effectiveness Analysis *Drummond, M. F., Sculpher, M. J., Torrance, G. W., O’Brien, B. J., & Stoddart, G. L. (2005). Methods for the Economic Evaluation of Health Care Programmes (3 edition.). Oxford University Press. (Chapters 2 and 3 only). Chandra, Amitabh, Anupam B Jena, and Jonathan S Skinner. “The Pragmatist’s Guide to Comparative Effectiveness Research.” Journal of Economic Perspectives 25, no. 2 (May 2011): 27–46. doi:10.1257/jep.25.2.27. Garber, Alan M. “Advances in Cost-Effectiveness Analysis of Health Interventions,” Volume 1:, Part 1:181–221. Elsevier, 2000. http://www.sciencedirect.com /science/article/B7P5R-4FF8276-8/2/6e4802b1d5a3dab5dfd49222a9500601. *McClellan, Mark, and Joseph P. Newhouse. “The Marginal Cost-Effectiveness of Medical Technology: A Panel Instrumental-Variables Approach.” Journal of Econometrics 77, no. 1 (March 1997): 39–64. Meltzer, David O., and Peter C. Smith. “Chapter Seven - Theoretical Issues Relevant to the Economic Evaluation of Health Technologies.” In Handbook of Health Economics, Volume 2:433–69. Elsevier, 2011. http://www.sciencedirect.com/science/article/pii/B9780444535924000074. *Sanders, Gillian D., Mark A. Hlatky, and Douglas K. Owens. “Cost-Effectiveness of Implantable Cardioverter-Defibrillators.” N Engl J Med 353, no. 14 (October 6, 2005): 1471–80. doi:10.1056/NEJMsa051989. Lecture 25—Labor Markets and Health Insurance *Baicker, Katherine, and Amitabh Chandra. “The Labor Market Effects of Rising Health Insurance Premiums.” Journal of Labor Economics 24, no. 3 (July 1, 2006): 609– 34. doi:10.1086/505049. Dey, Matthew, and Christopher Flinn. “Household Search and Health Insurance Coverage.” Journal of Econometrics 145, no. 1–2 (July 2008): 43–63. doi:10.1016/j.jeconom.2008.05.013. Dey, Matthew S., and Christopher J. Flinn. “An Equilibrium Model of Health Insurance Provision and Wage Determination.” Econometrica 73, no. 2 (March 2005): 571– 627. doi:10.1111/j.1468-0262.2005.00588.x. *Gruber, Jonathan. “The Incidence of Mandated Maternity Benefits.” The American Economic Review 84, no. 3 (June 1994): 622–41. Gruber, Jonathan, and Alan B. Krueger. “The Incidence of Mandated Employer-Provided Insurance: Lessons from Workers’ Compensation Insurance.” Tax Policy and the Economy 5 (1991): 111–43. *Kolstad, Jonathan T., and Amanda E. Kowalski. Mandate-Based Health Reform and the Labor Market: Evidence from the Massachusetts Reform. Working Paper. Cambridge, MA: National Bureau of Economic Research, 2012. http://www.nber.org/papers/w17933. Olson, Craig A. “Do Workers Accept Lower Wages in Exchange for Health Benefits?” Journal of Labor Economics 20, no. 2 (April 2002): S91–S114. *Summers, Lawrence H. “Some Simple Economics of Mandated Benefits.” The American Economic Review 79, no. 2 (May 1989): 177–83. Bonus Lecture—Insurer-Hospital Bargaining Gaynor, Martin, Kate Ho, and Robert Town. The Industrial Organization of Health Care Markets. Working Paper. National Bureau of Economic Research, January 2014. http://www.nber.org/papers/w19800. Ho, Kate, and Robin S. Lee. Insurer Competition and Negotiated Hospital Prices. Working Paper. National Bureau of Economic Research, September 2013. http://www.nber.org/papers/w19401. Ho, Kate, and Ariel Pakes. Hospital Choices, Hospital Prices and Financial Incentives to Physicians. Working Paper. National Bureau of Economic Research, August 2013. http://www.nber.org/papers/w19333. Ho, Katherine. “Barriers to Entry of a Vertically Integrated Health Insurer: An Analysis of Welfare and Entry Costs.” Journal of Economics & Management Strategy 18, no. 2 (June 1, 2009): 487–545. doi:10.1111/j.1530-9134.2009.00221.x. ———. “Insurer-Provider Networks in the Medical Care Market.” American Economic Review 99, no. 1 (March 2009): 393–430. doi:10.1257/aer.99.1.393. ———. “The Welfare Effects of Restricted Hospital Choice in the US Medical Care Market.” Journal of Applied Econometrics 21, no. 7 (2006): 1039–79. doi:10.1002/jae.896.