ECO 737 HEALTH ECONOMICS Fall 2013 Instructor: Jeremy Bray
advertisement

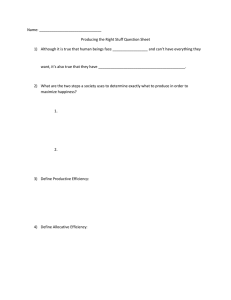
ECO 737 HEALTH ECONOMICS Fall 2013 Instructor: Office: Office Hours: Phone: E-mail Jeremy Bray Bryan 462 Tuesday 10:00 to 12:00 and by appointment 334-3910 jwbray@uncg.edu OVERVIEW This course will cover a variety of topics in health economics. Topics will be organized into three main areas: barriers to entry, health economics as a vocation, and things that interest me. “Barriers to entry” will be an overview of topics that any health economist should be familiar with. After this part of the course, you should be able to hold a conversation with an academic health economist without embarrassing the department. “Health economics as a vocation” will cover techniques of economic evaluation as applied to health care. After this section of the course you will have a basic tool set that many non-academic employers will value. “Things that interest me” will cover theoretical and empirical research on health behaviors. After this section of the course, you should have an understanding of research on people’s investments in their health. The class will use a modified seminar format. I will present at the beginning of each section to provide an overview of the coming material and students will present the rest of the material for that section. When you lead the discussion of an article (or articles), you should expect that the rest of the class has read all assigned materials, but you should still begin the discussion with a short presentation of key aspects or issues. Handouts or slides should be used to facilitate the discussion if appropriate. You will then lead and moderate the more extensive discussion that follows. When you present, it is your responsibility to ensure a quality discussion so be prepared to ask questions of the class that will prompt extended discussion around key points. Your summary presentation, choice of accompanying presentation materials (if any), and ability to promote further discussion will determine the presentation portion of your grade (see below). When you are not the presenter, you will be expected to have carefully read the materials before class and to participate extensively in the discussion of them. This will determine the class participation portion of your grade. GRADING Grading in the course will be based on general class participation (15%), applied homework assignments (15%), class presentations (20%), written assignments (25%), and the final project (25%). Applied homework assignments will be based on one or more chapters from AHE. The written assignments will consist of 3 short papers taking the form of memos, article summaries, referee reports, or brief analyses. The final project will involve the review of a specific literature, with or without an accompanying analysis of data. Specific information will be supplied at a later date. READINGS Readings will come primarily from the peer-reviewed literature, with supporting readings from the Handbook of Health Economics (HHE), Applied Health Economics, 2nd ed. (AHE), and various on-line resources. HHE is available to students electronically through the library or Science Direct. AHE should be available in the bookstore. The first edition is acceptable if you find one in a used bookstore. A copy of the first edition should also be available through the library and students may share copies if they wish. I reserve the right to change or add reading assignments as new articles are published, the class discussion takes us in a new direction, or I decide a different reading assignment would better fit the capabilities of the class. Once a particular reading is assigned to a student for presentation, it will not change. Guidance for preparing your final assignment can be found in the Cochrane Handbook of Systematic Reviews of Intervention (http://handbook.cochrane.org). Jones, Rice, d’Uva, & Balia. (2013). Applied Health Economics: Routledge, USA Handbook of Health Economics, Volumes 1 and 2. Elsevier, 2000. Barriers to Entry Background AHE Ch1, 2, 11 HHE V1a Ch2 Sec 3 http://www.kff.org/healthreform/upload/7871.pdf http://www.kff.org/healthreform/upload/8061.pdf General readings Akerlof, G. A. (1970). The market for" lemons": Quality uncertainty and the market mechanism. The quarterly journal of economics, 488-500. Anderson, G., P. Hussey, B. Frogner and H. Waters. 2005. “Health Spending in the United States and the Rest of the World” Health Affairs 24(4), 903-14. Arrow, K. 1963. “Uncertainty and the Demand for Medical Care” American Economic Review, 53(5), 941-73. Baicker, K., & Goldman, D. (2011). Patient Cost-Sharing and Healthcare Spending Growth. Journal of Economic Perspectives, 25(2), 47-68. Cutler, D. M., & Ly, D. P. (2011). The (Paper)Work of Medicine: Understanding International Medical Costs. Journal of Economic Perspectives, 25(2), 3-25. Garber A. and J. Skinner. 2008. “Is American Health Care Uniquely Inefficient?” Journal of Economic Perspectives 22(4), 27-50. (An excellent review of the US health care system that distinguishes between allocative and productive efficiency.) Getzen T., 2000. “Health care is an individual necessity and a national luxury: applying multilevel decision models to the analysis of health care expenditures.” Journal of Health Economics 19: 259–270. Grossman, M. 1972. “On the Concept of Health Capital and the Demand for Health” Journal of Political Economy 80(2), 233-55. Gruber J. and M. Owings, 1996. “Physician Financial Incentives and Cesarean Section Delivery.” RAND Journal of Economics 27(1): 99-123. Kessler, D. P. (2011). Evaluating the Medical Malpractice System and Options for Reform. Journal of Economic Perspectives, 25(2), 93-110. Kolstad J. and A. Kowalski, 2010. “The Impact of an Individual Health Insurance Mandate On Hospital and Preventive Care: Evidence from Massachusetts.” NBER Working Paper 16012. McClellan, M. (2011). Reforming Payments to Healthcare Providers: The Key to Slowing Healthcare Cost Growth While Improving Quality? Journal of Economic Perspectives, 25(2), 69-92. McGuire T. and M. Pauly, 1991. “Physician Response to Fee Changes with Multiple Payers,” Journal of Health Economics 10(4): 386-410. Pauly, M. 1968. “The Economics of Moral Hazard: Comment” American Economic Review, 58(3, part 1), 531-36. Rice, T. 1997. “Can Markets Give Us the Health System We Want?” Journal of Health Politics, Policy and Law 22(2), 383-426. Robinson, J. 2001. “The End of Asymmetric Information” Journal of Health Politics, Policy and Law 26(5), 1046-53. Thomasson M. 2002. “From Sickness to Health: The 20th Century Development of US Health Insurance” Explorations in Economic History 39(3), 233-53 White, C. 2007. “Health Care Spending Growth: How Different is the United States from the Rest of the OECD?” Health Affairs 26(1), 154-161. Yip W., 1998. “Physician response to Medicare fee reductions: changes in the volume of coronary artery bypass graft (CABG) surgeries in the Medicare and private sectors.” Journal of Health Economics 17: 675-699. Health Economics as a Vocation Background AHE Ch3, 12 HHE V1a Ch. 4 pp. 181-221 Bray, J. W., & Zarkin, G. A. (2006). Economic evaluation of alcoholism treatment. Alcohol Research and Health, 29(1), 27. Cost Basu, A., & Manning, W. G. (2009). Issues for the Next Generation of Health Care Cost Analyses. Medical Care, 47(7_Supplement_1), S109-S114 Duan. (1983). Smearing Estimate: A Nonparametric Retransformation Method. Journal of the American Statistical Association , Vol. 78, No. 383, pp. 605-610 Dunlap, L. J., Zarkin, G. A., & Cowell A.J. (2008). Examining variation in treatment costs: A cost function for outpatient methadone treatment programs. Health Services Research, 43(3), 931–950. Johns, B., Baltussen, R., & Hutubessy, R. (2003). Programme costs in the economic evaluation of health interventions. Cost Effectiveness and Resource Allocation, 1(1), 1. Manning, Joseph P. Newhouse, Naihua Duan, Emmett B. Keeler and Arleen Leibowitz. (1987) Health Insurance and the Demand for Medical Care: Evidence from a Randomized Experiment. The American Economic Review , Vol. 77, No. 3, pp. 251-277 Manning. (1998). The logged dependent variable, heteroscedasticity, and the retransformation problem. Journal of Health Economics, Volume 17, Issue 3, Pages 283-295 Manning, John Mullahy (2001). Estimating log models: to transform or not to transform? Journal of Health Economics, Volume 20, Issue 4, Pages 461-494 Smith, M.W. and P.G. Barnett (2003). Direct Measurement of Health Care Costs. Medical Care Research and Review, 60 (3) p. 74S-91S Zarkin, G. A., Dunlap, L. J., Wedehase, B., & Cowell, A. J. (2008). The effect of alternative staff time data collection methods on drug treatment service cost estimates. Evaluation and Program Planning, 31(4), 427–435. Zarkin, G. A., Dunlap L. J., & Homsi, G. (2004). The substance abuse services cost analysis program (SASCAP): A new method for estimating drug treatment services costs. Evaluation and Program Planning, 27(1), 35–43. Zarkin, G. A., Bray, J. W., Davis, K. L., Babor, T. F., & Higgins-Biddle, J. C. (2003). The costs of screening and brief intervention for risky alcohol use. Journal of Studies on Alcohol, 64(6), 849–857. CEA/CUA Bala, M.V., & Zarkin, G. A. (2004). Pharmacogenomics and the evolution of healthcare: Is it time for cost-effectiveness analysis at the individual level? PharmacoEconomics, 22(8), 495–498. Bala, M. V., & Zarkin, G. A. (2002). Application of cost-effectiveness analysis to multiple products: A practical guide. American Journal of Managed Care, 8(3), 211-220. Barbosa, C., Godfrey, C., & Parrott, S. (2010). Methodological assessment of economic evaluations of alcohol treatment. What is missing? Alcohol and Alcoholism, 45(1), 53– 63. doi:10.1093/alcalc/agp067 Barton, G. R., Briggs, A. H., & Fenwick, E. A. L. (2008). Optimal Cost‐Effectiveness Decisions: The Role of the Cost‐Effectiveness Acceptability Curve (CEAC), the Cost‐Effectiveness Acceptability Frontier (CEAF), and the Expected Value of Perfection Information (EVPI). Value in Health, 11(5), 886-897. Dunlap, L. J., Zarkin, G. A., Bray, J. W., Mills, M. J., Kivlahan, D. R., McKay, J., Latham, P., & Tonigan, J. S. (2010). Revisiting the cost-effectiveness of the COMBINE Study for alcohol dependent patients: The patient perspective. Medical Care, 48(4), 306–313. Fenwick, E., Claxton, K., & Sculpher, M. (2001). Representing uncertainty: the role of cost‐ effectiveness acceptability curves. Health Economics, 10(8), 779-787. Fenwick, E., O'Brien, B. J., & Briggs, A. (2004). Cost‐effectiveness acceptability curves–facts, fallacies and frequently asked questions. Health Economics, 13(5), 405-415. Fenwick, E., & Byford, S. (2005). A guide to cost-effectiveness acceptability curves. The British Journal of Psychiatry, 187(2), 106-108. Gafni, A., & Birch, S. (2006). Incremental cost-effectiveness ratios (ICERs): the silence of the lambda. Social Science & Medicine, 62(9), 2091-2100. Garber, A. M., & Phelps, C. E. (1997). Economic foundations of cost-effectiveness analysis. Finkelstein A., 2004. “Static and Dynamic Effects of Health Policy: Evidence from the Vaccine Industry.” Quarterly Journal of Economics 119(2): 527-564. http://www.who.int/choice/publications/p_2003_generalised_cea.pdf Harkness J., S. Newman, and D. Salkever, 2004. “The Cost-Effectiveness of Independent Housing for the Chronically Mentally Ill: Do Housing and Neighborhood Features Matter?” Health Services Research 39(5): 1341-1360 Hutubessy, R. C. W., Niessen, L. W., Dijkstra, R. F., Casparie, T. F., & Rutten, F. F. (2005). Stochastic league tables: an application to diabetes interventions in the Netherlands. Health Economics, 14(5), 445-455. Hutubessy, R. C. W., Baltussen, R. M. P. M., Evans, D. B., Barendregt, J. J., & Murray, C. J. L. (2001). Stochastic league tables: communicating cost‐effectiveness results to decision‐ makers. Health Economics, 10(5), 473-477. Mauskopf, J., Rutten, F., & Schonfeld, W. (2003). Cost-effectiveness league tables: valuable guidance for decision makers? Pharmacoeconomics, 21(14), 991-1000. Pereira, J., Barbosa, C., Mateus, C., & Standaert, B. (2008). Cost-effectiveness analysis of an HPV-16/18 prophylactic cervical cancer vaccine in a setting of existing screening in Portugal—Results from a mathematical model. Value in Health, 11, A63. Sanders G., M. Hlatky, and D. Owens, 2005. “Cost-Effectiveness of Implantable CardioverterDefibrillators.” New England Journal of Medicine 353: 1471-1480. Zarkin, G. A., Bray, J. W., Aldridge, A. P., Mitra, D., Mills, M. J., Couper, D. J., & Cisler R. A. (2008). Cost and cost-effectiveness of the COMBINE study for alcohol-dependent patients. Archives of General Psychiatry, 65(10), 1214–1221. CBA Bala, M. V., Zarkin, G. A., & Mauskopf, J. (2008). Presenting results of probabilistic sensitivity analysis: The incremental benefit curve. Health Economics, 17(3), 435–440. Bala, M., Zarkin, G. A., & Mauskopf, J. A. (2002). Conditions for the (near) equivalence of costeffectiveness and cost-benefit analyses. Value in Health, 5(4), 338–346. Bray, J. W., Zarkin, G. A., Davis, K. L., Mitra, D., Higgins-Biddle, J. C., & Babor, T. F. (2007). The health care utilization effect of screening and brief intervention for risky drinking in four managed care organizations. Medical Care, 45(2), 177–182. Stinnett, A. A., & Mullahy, J. (1998). Net health benefits. Medical Decision Making, 18(2), S68S80. Willan, A. R., & Lin, D. (2001). Incremental net benefit in randomized clinical trials. Statistics in Medicine, 20(11), 1563-1574. Zarkin, G. A., Bray, J. W., Aldridge, A. P., Mills, M. J., Cisler, R. A., Couper, D. J., et al. (2010). The effect of alcohol treatment on social costs of alcohol dependence: Results from the COMBINE study. Medical Care, 48, 396–401. Zarkin, G. A., Dunlap, L. J., Belenko, S., & Dynia, P. A. (2005). A benefit-cost analysis of the Kings County District Attorney’s Office Drug Treatment Alternative to Prison (DTAP) program. Justice Research and Policy, 7(1), 1–25. Zarkin, G. A., Dunlap L. J., Hicks, K. A., & Mamo, D. (2005). Benefits and costs of methadone treatment: Results from a lifetime simulation model. Health Economics, 14(11), 1133– 1150. Miscellaneous Methods Barbosa, C., Taylor, B., Godfrey, C., Rehm, J., Parrott, S., & Drummond, C. (2010). Modelling lifetime QALYs and health care costs from different drinking patterns over time: A modified Markov model. International Journal of Methods in Psychiatric Research, 19(2), 97–109. doi:10.1002/mpr.306 Bray, J. W., Cowell, A. J., & Hinde, J. M. (2011). A systematic review and meta-analysis of health care utilization outcomes in alcohol screening and brief intervention trials. Medical Care, 49, 287–294. Chandra, A., Jena, A. B., & Skinner, J. S. (2011). The Pragmatist's Guide to Comparative Effectiveness Research. Journal of Economic Perspectives, 25(2), 27-46. Galet and List (2003). Cigarette demand: a meta-analysis of elasticities. Health Economics Volume 12, Issue 10, pages 821–835. Lu Z. and W. Comanor, 1998. “Strategic Pricing of New Pharmaceuticals.” Review of Economics and Statistics 80(1): 108-118. Prospective Studies Collaboration, Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies, The Lancet, Volume 360, Issue 9349, 14 December 2002, Pages 1903-1913 Wagenaar, A. C., Salois, M. J., & Komro, K. A. (2009). Effects of beverage alcohol price and tax levels on drinking: a meta-analysis of 1003 estimates from 112 studies. Addiction, 104(2), 179-190. Things that Interest Me Background AHE Ch5-8 Becker, G. S. (1965). A theory of the allocation of time. The Economic Journal , 75 (299), 493517. Cook, P. and M. Moore. 2000. “Alcohol” Handbook of Health Economics, 1630-73. General Readings Auld, C. and P. Grootendorst. 2004. “An Empirical Analysis of Milk Addiction” Journal of Health Economics, 23(6), 1117-33. Becker, G. and K. Murphy. 1988. “A Theory of Rational Addiction” Journal of Political Economy, 96(4), 675-700. Becker, G., M. Grossman and K. Murphy. 1994. “An Empirical Analysis of Cigarette Addiction” American Economic Review, 84(3), 396-418. (Focus on p. 396-407.) Berger, M.C., Leigh, J.P., 1988. The effect of alcohol use on wages. Applied Economics 20, 1343-1351. Bernheim, B.D. and R. Rangel. 2004. “Addiction and Cue-Triggered Decision Processes” American Economic Review 94(5), 1558-90. Bray, J. W., Loomis, B. R., & Engelen, M. A. (2009). You save money when you buy in bulk: Does volume-based pricing cause people to buy more beer? Health Economics, 18, 607– 618. Bray, J. W. (2005). Alcohol use, human capital, and wages. Journal of Labor Economics, 23(2), 279–312. Caplan, B. (2006). Terrorism: The relevance of the rational choice model. Public Choice, 128(1), 91–107. Chaloupka, F.J., Saffer, H., Grossman, M., 1993. Alcohol-control policies and motor-vehicle fatalities. Journal of Legal Studies 22(1), 161-186. Chaloupka F. and K. Warner. 2000. “The Economics of Smoking” Handbook of Health Economics. Chatterji, P., & Markowitz, S. (2001). The impact of maternal alcohol and illicit drug use on children's behavior problems: evidence from the children of the national longitudinal survey of youth. Journal of Health Economics, 20(5), 703-731. Cook, P.J., Moore, M.J., 1993. Drinking and schooling. Journal of Health Economics 12, 411429. Gruber J. and B. Köszegi. 2001. “Is Addiction Rational? Theory and Evidence” Quarterly Journal of Economics , 161(4), 1261-1303. Gul, F., & Pesendorfer, W. (2001). Temptation and self‐control. Econometrica, 69(6), 14031435. Gul, F., & Pesendorfer, W. (2007). Harmful addiction. Review of Economic Studies, 74(1), 147172. Heien, D.M., 1996. Do drinkers earn less? Southern Economic Journal 63(1), 60-69. Kahneman, D. (2003). Maps of bounded rationality: Psychology for behavioral economics. The American economic review, 93(5), 1449-1475. Kenkel, D. 1991 “Health Behavior, Health Knowledge and Schooling” Journal of Political Economy, 99(2), 287-305. Markowitz, S., Chatterji, P., & Kaestner, R. (2003). Estimating the impact of alcohol policies on youth suicides. Journal of Mental Health Policy and Economics, 6(1), 37-46. Mullahy, J., & Sindelar, J. (1989). Life-cycle effects of alcoholism on education, earnings, and occupation. Inquiry: a journal of medical care organization, provision and financing, 26(2), 272. Mullahy, J., & Sindelar, J. L. (1994). Alcoholism, work, and income over the life cycle: National Bureau of Economic Research. Mullahy, J., & Sindelar, J. (1996). Employment, unemployment, and problem drinking. Journal of Health Economics, 15(4), 409-434. Pacula, R.L., 1998. Does increasing the beer tax reduce marijuana consumption? Journal of Health Economics 17, 557-585. Wagenaar, A. C., Maldonado-Molina, M. M., & Wagenaar, B. H. (2009). Effects of Alcohol Tax Increases on Alcohol-Related Disease Mortality in Alaska: Time-Series Analyses From 1976 to 2004. Am J Public Health, 99(8), 1464-1470. Zarkin, G. A., French, M. T., Mroz, T., & Bray, J. W. (1998). Alcohol use and wages: New results from the national household survey on drug abuse. Journal of Health Economics, 17(1), 53-68. TENTATIVE CLASS SCHEDULE 8/19/2013 8/21/2013 8/26/2013 8/28/203 9/2/2013 9/4/2013 9/9/2013 9/11/2013 9/16/2013 9/18/2013 9/23/2013 9/25/2013 9/30/2013 10/2/2013 10/7/2013 10/9/2013 Introduction Barriers to entry (background) Barriers to entry (health care financing/reform) Barriers to entry (health care financing/reform) No class – Labor Day Barriers to entry (demand for health care) No class No class Barriers to entry (demand for health care) HE as a vocation (background) HE as a vocation (cost) HE as a vocation (cost) HE as a vocation (CEA/CUA) HE as a vocation (CEA/CUA) HE as a vocation (CBA) HE as a vocation (CBA) 10/14/2013 10/16/2013 10/21/2013 10/23/2013 10/28/2013 10/30/2013 11/4/2013 11/6/2013 11/11/203 11/13/2013 11/18/2013 11/20/2013 11/25/2013 11/27/2013 12/2/2103 12/9/2013 No class – Fall break HE as a vocation (methods) HE as a vocation (methods) Things that interest me (background) Things that interest me (addiction) Things that interest me (addiction) Things that interest me (addiction) Things that interest me (policy) Things that interest me (policy) Things that interest me (policy) Things that interest me (human capital/labor market) Things that interest me (human capital/labor market) Things that interest me (human capital/labor market) No class – Thanksgiving Things that interest me (human capital); last class Final assignments due no later than 6:30 pm